Back to Journals » Open Access Emergency Medicine » Volume 15
Outcomes of Ultrasound Guided Peripheral Intravenous Catheters Placed in the Emergency Department and Factors Associated with Survival
Authors Malik A, Dewald O , Gallien J, Favot M, Kasten A, Reed B, Wells R , Ehrman RR
Received 10 February 2023
Accepted for publication 29 April 2023
Published 19 May 2023 Volume 2023:15 Pages 177—187
DOI https://doi.org/10.2147/OAEM.S405692
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Adrienne Malik,1 Olga Dewald,2 John Gallien,3 Mark Favot,3 Adam Kasten,5 Brian Reed,6 Robert Wells,5 Robert R Ehrman4
1Department of Emergency Medicine, University of Kansas Medical Center, Kansas City, MO, 66160, USA; 2Department of Emergency Medicine, Sparrow Hospital, Lansing, MI, 48912, USA; 3Department of Emergency Medicine, DMC Detroit Receiving Hospital, Detroit, MI, 48201, USA; 4Department of Emergency Medicine, DMC Sinai Grace Hospital, Detroit, MI, 48235, USA; 5Department of Emergency Medicine, DMC Harper Hospital, Detroit, MI, 48201, USA; 6Department of Emergency Medicine, Wayne State University, Detroit, MI, 48201, USA
Correspondence: Adrienne Malik, Department of Emergency Medicine, University of Kansas Medical Center, 4000 Cambridge St, Kansas City, MO, 66160, USA, Email [email protected]; [email protected]
Background: Patients with difficult peripheral intravenous (IV) access are common in emergency departments (EDs). Ultrasound-guided peripheral intravenous catheters (USIVs) are frequently used in this population; however, information regarding the effect of patient and IV characteristics on the dwell time (DT) and survival probability (SP) of USIVs is limited.
Objective: Our study aimed to evaluate for associations between patient or IV characteristics and the DT and SP of USIVs.
Methods: Retrospective analysis was performed on a database from an ED nurse (RN) USIV training program at an urban, academic hospital. Patients over 18 years with an USIV placed during the study period were included. Subject demographics, history, IV characteristics, insertion, and removal times were collected. Data were analyzed using descriptive statistics and univariable and multivariable Cox regression. USIV survival times for variates of interest were estimated using Kaplan–Meier curves for three censoring points.
Results: The final analysis cohort was 388 patients. Mean age was 56.6 years, 66.5% were female, mean BMI was 29.9 kg/m2, and 42.5% were obese (BMI ≥ 30). Median DT was 40.3 hours in admitted patients (N=340). SP for USIVs at 96 hours was 87.8%. A total of 21 of 340 (6.2%) USIVs failed. USIV location conferred a difference on DT in obese patients when dichotomized into upper arm versus antecubital fossa and forearm together (38.6 hours vs 44.6 hours, p=0.03). No factors were associated with a difference in USIV SP.
Conclusion: Median USIV DT of 40.3 hours for admitted patients was higher than in previous studies. Only 7% of USIVs in our study failed. Overall, catheters survived longer than expected.
Keywords: ultrasound, peripheral IV, retrospective, emergency medicine, vascular access
Introduction
Patients with difficult peripheral intravenous (IV) access are common, with 11.8% of emergency department (ED) patients and up to 25% of hospitalized patients meeting this designation.1,2 Two failed attempts to place an IV by palpation is commonly used to define a patient as “difficult to access”.1 Ultrasound-guided peripheral intravenous lines (USIVs) are frequently utilized to obtain IV access in these patients, resulting in reduced need for central venous catheter placement, fewer skin punctures, and increased patient satisfaction.3–6 While initially USIVs were preferentially placed by physicians, multiple studies now demonstrate that ED technicians and registered nurses (RNs) perform this procedure as reliably as physicians.7–10
Though the rate of successful initial placement is high, USIVs historically have a greater reported incidence of premature failure (lower survival) and decreased dwell time (amount of time catheter documented as usable) when compared to IVs placed using standard techniques.11–14 However, newer literature reports similar survivorship between USIVs and those placed by standard methods.15 Previous research efforts sought to better understand what modifiable and non-modifiable factors affect the longevity of USIVs. As a result of these studies, it is now established that initial USIV placement success is greater and dwell time (DT) longer when target vessels are larger (≥0.4 cm), more superficial (≤1.2cm deep), located at or distal to the antecubital fossa (AC), and when at least 65% of the catheter is placed in the vein.16–19 While several previous studies investigated patient characteristics associated with difficult IV access, much remains unknown about how these patient characteristics affect the survival probability and DT of USIVs.1,20 Prior research found no relationship between survival or DT and end-stage renal disease (ESRD), history of IV drug abuse (IVDA), or obesity; all are factors commonly associated with patients characterized as having difficult IV access.13 A multivariate analysis by Wallis et al found that PIV placement in the hand, AC, or upper arm was an independent risk factor for IV occlusion or accidental dislodgement; however, their cohort included only PIVs placed by traditional palpation method.19
Further data are needed to assess the possible influence of patient and IV catheter factors on the survival and durability of USIVs, as this information could assist clinicians in making choices about IV placement for patients with difficult PIV access. The goal of this study was to evaluate for associations between specific patient characteristics (sex, BMI, history of ESRD, or IVDA) or IV characteristics (IV placement location) and the DT and SP of USIVs.
Materials and Methods
Study Design and Setting
This was a retrospective chart review of all entries in a quality-assurance database started in conjunction with an institutional program training ED RNs to place USIVs. The study was conducted at an urban, academic tertiary-care hospital with 50,000 annual adult ED visits. All database entries from July 2015 through October 2016 for ED patients older than 18 years who received a nursing-placed USIV were included. No database entries were initially excluded. Patient eligibility for RN placement of an USIV was determined by the treating clinician and availability of certified personnel per hospital guidelines. In accordance with standard practice at our institution, patients were deemed to need an USIV after two failed attempts at placement by palpation/landmark technique by an experienced RN. IV catheter gauge and placement location were chosen by the nurse operator per hospital protocol and placed employing standard infection control methods. This study was approved by the Wayne State University Institutional Review Board (IRB) and was executed in compliance with our hospital’s patient data protection and HIPPA-related privacy regulations. As this study was performed on a previously obtained quality-assurance database, no sample size calculations were performed and consent was waived as approved by the IRB. A secure log of each RN-placed USIV was maintained to document training and compliance with ongoing certification requirements.
Study Protocol
Placement of Ultrasound-Guided IVs
USIVs were placed using a standard short-axis technique, utilizing a high-frequency (L10-8) linear-array transducer (Mindray Bio-medical Electronics, Shenzen, China). All catheters included in this study were BD Insyte™ Autoguard™ shielded IV catheters, standard in our ED. Placements were performed employing standard USIV hygiene practices, and following successful cannulation all USIVs were secured with a 3M Tegaderm IV securement film. Participant RNs attended a two-hour didactic session led by US-trained faculty or two RN superusers, each of whom had placed >350 USIVs. Participants then completed 10 USIV insertions supervised by RN superusers or appropriately credentialed emergency physicians. After 10 USIV starts, participants were considered “certified” and able to place USIVs unsupervised.
Chart Review Protocol
Non-blinded data abstractors were trained by the primary investigator. For each subject, demographic variables, past medical history, IV characteristics, and IV insertion and removal times were collected from the electronic medical record (EMR) and entered in a REDCap form. Per hospital protocol, all IVs were assessed at least once every 8 hours with documentation of time and reason for removal made in the EMR. This documentation system is universal to all floor units and the ED. When a documented removal time was unavailable, the last documented time of IV functionality (“last assessed time”) was recorded. Failure of a PIV was defined as any unplanned removal; IVs that were removed prior to failure (eg, at the time of discharge) were documented as such.
In accordance with published methods for chart review studies, the primary investigator reviewed the first 5 charts from each abstractor and a random sample of 10 charts at approximately 50% completion.21 At the conclusion of chart review, the primary investigator and abstractors reviewed all records with missing entries or those flagged as ambiguous. Any patients with missing data, or those in whom consensus amongst study team members could not be reached, were excluded from the final analysis.
Study Outcomes
Catheter survival was the primary outcome of interest. The amount of time a catheter was usable was recorded as a DT and calculated as the recorded time in hours from USIV catheter insertion to catheter removal. If no documented catheter removal time was available, the last recorded catheter assessment time was used as a surrogate. DTs less than 1 hour were considered unsuccessful placements and not considered in the overall survival analysis. This was done to remove the influence of immediately unusable IV placements since the aim of this study was to evaluate the survival of successfully placed IVs. The records for dwell times less than 1 hour were included in secondary outcome analysis which evaluated number of IV attempts and binary classification of successful versus unsuccessful IV placement. A similar approach was used by Fung et al.22 Patients with multiple documented USIV placement records during a single encounter were removed from the final cohort used in DT and survival analysis to establish a more clinically homogeneous sample. To identify potential covariates associated with USIV catheter survival, demographic variables (age, sex, height, weight), past medical history (ESRD, IVDA), and IV characteristics (length, gauge, location, operator) were extracted from the dataset and included in our analysis. To understand the association between obesity and DT, we examined survival patterns based on a BMI cut-point of 30 kg/m2, chosen based on World Health Organization guidelines that define obesity as a BMI ≥30 kg/m2. We relied on a binary classification of obesity as either non-obese (<30 kg/m2) or obese (≥30 kg/m2).
Statistical Analysis
Descriptive data are presented as mean, median value with interquartile range (IQR), or counts and percentages. Bivariable comparisons were made using t-test, Wilcoxon rank sum test, or chi-square/Fisher’s exact test, as appropriate.
The Kaplan–Meier product limit method was used to estimate the probability of catheter survival. Survival time endpoint was reached when the event of interest (IV failure) or a censoring event occurred. IVs that were removed at time of hospital discharge or requested to be removed were treated as censoring events. Survival curves of each covariate of interest were generated for three different fixed time points: 400 hours (considered non-failure), 96 hours, and 24 hours. Cox proportional hazard models were used to determine whether any of the predictors of interest were independently related to catheter survival over time. Covariates significant in the univariable analyses were then included in the multivariable Cox model. Interaction between IV location and obesity status was also assessed. The proportional hazard assumption of compared survival curves was assessed visually. When the proportionality assumption was violated, time-varying hazard ratios (HRs) were calculated. CDC guidelines recommend removal of PIVs at 96 hours for infection control purposes.23 As such, we calculated survival probability (SP) and restricted mean survival time (RMST) at this time point. RMST represents the area under the Kaplan–Meier survival curve up to this time point and can be interpreted as mean survival time for all USIVs followed until this time, accounting for failures and censored events.24,25 The level of statistical significance used for all tests was 0.05. All statistical analyses were conducted using SAS version 9.4 [SAS Institute, Cary, NC].
Results
Demographic and Clinical Characteristics
A total of 1475 IV placement records from patients who underwent nursing-placed USIVs during the study period were identified. The final analysis cohort of 388 patients consisted of those with a single USIV placed successfully during their hospital encounter and a known outcome of IV failure or removal (Figure 1). Table 1 shows the clinical characteristics of the final cohort of 388 patients.
 |
Table 1 Patient Demographics and USIV Characteristics of the Analysis Cohort of Patients with a Single Successful Ultrasound IV During Their Hospital Encounter with a Known Outcome |
 |
Figure 1 Study flow diagram of the USIV placements included in the study. Diagram illustrates the flow to determine the final analysis cohort. |
The mean age of the 388 patients in the final cohort was 56.6 years, 66.5% were female, mean BMI was 29.9 kg/m2, and 42.5% were obese (BMI ≥30). Overall, 21.9% had ESRD, and 11.6% had a history of IVDA. The distribution of IV gauges in the final cohort was 73.4% 18G (6.35 cm), 25.6% 20G (4.45 cm), and 1.0% other sizes. Placement location was 51.8% in the upper arm, 22.7% in the forearm, and 25.5% in the AC.
Twenty-one RNs performed the USIV placements during our study period. Of these, three RNs were responsible for 72.9% (906/1357) of the total catheter placement attempts and 73.1% (674/980) of the successful placements. In the sub-sample of admitted patients (340/388), the proportion of USIVs placed by these three operators was 77.6% (260/340).
Catheter Dwell Time and Survival
Dwell Time Analysis
Median DT for the initial cohort of 1190 unique IV placements was 26.3 hours (IQR 3.7–61.1). Among successful USIV placements (N=980) the median was 37.2 hours (IQR 15.1–69.2). The final analysis cohort of single USIV placements in unique patients with known outcomes and any admission status (N=388) had a median DT of 35.2 hours (IQR 15.0–65.4). A total of 48 patients from this cohort of 388 were ultimately discharged from the ED causing their median DTs to be limited by their length of stay. This resulted in a small depression of the overall median DT in the final cohort (N=388). When these 48 discharged patients were excluded from the DT analysis, the sub-sample of only admitted patients (N=340) had a median DT of 40.3 hours (IQR 18.8–69.5). There was no significant difference in catheter DT based on RN operator.
In the sub-group of admitted patients, no significant differences in mean DT were found for females versus males, BMI ≥30 kg/m2, history of IVDA, or ESRD. There was no difference in DT with respect to IV catheter size or location in the full admitted cohort. In the subset of admitted obese patients, mean DT was noted to be shorter for IVs placed in the upper arm when compared to AC and forearm placements considered together (27.4 versus 42.2 hours, p=0.03). All covariates are listed in Table 2.
 |
Table 2 Variables of the Cohort of 340 Admitted Patients with a Single Successful USIV Placement Encounter with a Known Outcome |
Overall Survival Analysis
The USIV survival curve for the cohort of 340 admitted patients using a time-to-event analysis is graphically depicted in Figure 2. Median survival time could not be reported based on our data since only 21 of the 340 admitted subjects experienced IV failure prior to the final time point of survival data collection. At 96 hours the point estimate SP of an USIV in this cohort was 87.8%; however, since no event occurred at 96 hours, no confidence interval (CI) could be generated. Therefore, we calculated the CI for survival probability at the closest times surrounding 96 hours with documented events. At 84 hours the point estimate SP was 87.8% (95% CI 0.80–0.92), and at 102 hours it was 85.2% (95% CI 0.75–0.91).
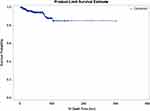 |
Figure 2 Kaplan–Meier curve for overall USIV catheter survival probability in admitted patients with a single successful USIV placement and known placement outcome (N=340). |
To account for the fact that only 32 at-risk catheters remained at 102 hours, and the left skew of censoring events in our cohort, we calculated the point estimate of SP at 40.3 hours which was our cohort’s median DT. As there was no event at exactly 40.3 hours to allow for the generation of a CI, we calculated the CI for SP at the closest times surrounding 40.3 hours with documented events, which were at 38.05 hours and 42.85 hours. The point estimates of SP for these times were 94.7% (95% CI 91.3–96.9) with 179/340 IVs still remaining, and 94.2% (95% CI 90.5–96.5) with 162/340 IVs still remaining, respectively. The 96-hour RMST of admitted patients was 88.7 hours (standard error 1.6 hours). When restricted at the last known event time (102.2 hours), the RMST was 95.9 hours (standard error 1.4 hours).
Survival Analysis by Sex, BMI, and IV Location
There were no statistically significant differences in SP between sex, BMI, or IV location groups at any fixed time point (24, 96, and 400 hours). Survival curves are shown in Figure 3.
Survival Analysis by Dichotomized IV Location in Obese Subjects
There was an observed significant difference in mean DT among obese patients with respect to an upper-arm IV placement location versus forearm and AC locations, collectively (Table 2). Thus, a SP analysis was performed which only included obese patients and a dichotomous location indicator (upper arm, yes or no). Despite the observed difference in median DTs in obese patients with respect to upper arm placements, no significant differences in SP were realized at any of the three time points examined.
Proportional Hazard Analysis
On univariable analysis, both obesity and female sex independently predicted a decreased catheter survival time (Table 3), with obesity significant at all time points and female gender significant only at 96 hours. However, on multivariable analysis, no statistically significant associations were seen for any covariates. Lack of significance persisted regardless of whether the obesity variable was treated as categorical or continuous, or considered to have an interaction with IV location (Supplement Tables 1–4). The proportionality assumption was violated for the multivariable model so time-varying HRs were calculated for intervals between 1 and 96 hours. None of the time-varying HRs were statistically significant either.
Discussion
Our large, retrospective observational study evaluated for associations of patient and IV characteristics on USIV DT and survival. Although we found no significant association between any patient or IV factor and survival, we did find a surprisingly high overall SP for USIVs in our study population at multiple time points, with only 21 explicitly documented failures in the cohort of 340 admitted patients. This cohort best represents USIVs with true potential for survival since patients discharged from the ED have their IVs removed after only a few hours. We also found a greater than anticipated median DT of 40.3 hours in this cohort when patients discharged from the ED were excluded.
Until recently, general consensus has been that USIVs do not last as long as those placed by the landmark method. Prior studies report overall decreased DTs and increased failure rates for USIVs when compared with traditional PIVs.12,26,27 In 2010, Dargin et al found a median DT for USIVs of 26 hours in their study evaluating USIV placement in ED patients with difficult IV access.13 Pandurangadu et al’s 2018 prospective study reported a median time to USIV failure of 15.6 hours.18 A retrospective study evaluating the difference in DT between USIVs and traditional IVs reported an average DT of 27.91 hours for USIVs.27 Even a prospective study of long IV catheters (4.78 cm, 20G) placed using ultrasound only reported a median DT of 30 hours.12 Another publication reported the failure rate of USIVs at 45–56% after initial successful placement compared to only 19–25% for traditionally placed PIVs.12 Given these previous findings, our results at first appear to be an outlier. Our reported median DT of 26.3 hours in the initial analysis cohort (N=1190) is thus consistent with previously reported DTs in the literature, but our median DT of 40.3 hours in the admitted patient cohort was greater than expected based on DT reports from previous studies.12,13,26,27
In contrast, a large RCT by Shokoohi et al in 2019 found similar DTs for ED USIVs and IVs placed by traditional methods in both an ED setting and an inpatient setting. They reported no difference in the relative risk for premature removal in the USIV group before 72 hours, with only 27% (50/182) failing by 72 hours.15 In our admitted cohort only 4.7% (16/340) of USIVs had a documented failure by 72.7 hours. In a 2021 retrospective study comparing extended dwell IV catheters to standard catheters placed using ultrasound in admitted patients, Fung et al reported a median DT of 3.8 days (95% CI 3.6–4.0) for standard USIVs.22 In comparison to our results, their unusually long DT is confounded by the heterogeneity of what the investigators categorized as a standard IV (length 2–4.5 cm, gauges 14–24) as well as the use of a dedicated IV access care team that is responsible for IV insertion and maintenance.22 They used a longer time point to define early failure (DT <4 hours compared to a much stricter, 1-hour cutoff in our study), and they also appear to have excluded—rather than censored—patients with ambiguous removal times. Both of these approaches would likely prolong observed DTs.
Still, the findings from these studies, in conjunction with our data, call into question the tacit belief that USIVs fail quickly. The studies reporting longer USIV survival are more recent, and there are multiple factors that may contribute to this noted increased longevity. Improved ultrasound technology, greater operator familiarity with USIV placement techniques, and knowledge gained from the body of literature identifying factors that increase the likelihood of USIV survival (for example: the percentage of the catheter that should reside in the vein) are a few such possible influences leading to longer USIV DTs.18,20
With several contemporary USGIV studies demonstrating notably longer dwell times, consideration over exactly how long an USIV needs to last is warranted. Shokoohi et al designed their prospective study to evaluate USIV survival up to 72 hours, based on a hospital policy to remove any existing PIV at that time point.15 That policy is based on the low bound of a category 1B guideline for the prevention of catheter-related infections which states PIVs (regardless of placement methods) do not require removal before 72–96 hours as a means of infection prevention.23 Extrapolating from this guideline, it stands to reason that an USIV need only achieve a maximum DT of 96 hours before infection control recommendations will mandate its removal. The SP for USIVs in our study at 96 hours was 87.8% and our RMST at 96 hours was 88.7 hours, well within this recommended removal timeframe. If overall survival in fact approaches 96 hours as indicated by our results, then the belief that USIVs are inferior to traditional placements because they fail sooner is challenged. Further research is needed to confirm our findings prospectively.
Overall, we found no patient or IV factors associated with SP or exerting a significant survival hazard on our cohort. Existing literature focused on factors influencing USIV catheter DT after initial placement is still somewhat limited with contradictory findings. A prospective observational study of the survival characteristics of USIVs placed in difficult-to-access patients who were followed throughout hospitalization identified several covariates of interest. These covariates included age, sex, BMI, and IVDA; but, as in our study, none were associated with overall catheter survival.13 In contrast, a retrospective study comparing the catheter DTs for patients with nursing-placed IVs or USIVs found that sex, age, and BMI were all significant predictors of catheter DT.27 In a more recent study by Fung et al, the researchers found no association between history of ESRD or BMI and catheter SP but did find advanced age and male gender slightly protective against failure.22 Another study by Fields et al found significantly increased SP for USIVs placed in the forearm or AC as compared to the upper arm after 18 hours, but we failed to find a significant difference in SP based on IV location in our cohort.16 It is possible that we failed to identify a significant patient or IV factor association with SP due to the overall low number of IV failures in our cohort.
We did observe that obesity (BMI ≥30 kg/m2) was associated with decreased median DT when IV location was dichotomized into upper or lower arm (p=0.03), but there was no statistically significant effect on the hazard of failure in our multivariable analysis. Previous studies postulated that obesity adversely affects catheter survival due to increased subcutaneous tissue and subsequent distance from the skin insertion site to the target vein.16 This is theorized to lead to inadvertent catheter dislodgement, especially when using a shorter length catheter.16 We did not collect data on target vessel depth, so this question remains unanswered in our cohort. Future studies evaluating the relationship between target vessel depth, catheter length, and catheter survival in an obese patient population are needed. While future studies may provide more clarity, our study does seem to suggest that preferential USIV placement in the lower arm may confer a greater DT in obese patients.
Limitations
This study is a retrospective, observational analysis of a quality assurance database conducted at a single institution and thus subject to limitations inherent to the study design. While the retrospective nature of our cohort allowed for a large sample size, our dataset is hindered by missing data points from some patient records, necessitating exclusion as described in our methods section. While residual confounding may exist (see below), our study methodology, analysis cohort selection process, criteria for exclusion, and covariate adjustments are similar to other studies on this topic.15,22
One such possible confounder is that RNs who placed USIVs in our study chose catheter gauge and placement location independently, possibly resulting in selection bias for catheter sizes or IV locations. Another potential source of confounding is the variability in operator experience. The majority of RNs had little to no prior exposure to USIV catheter placement. Nine of 21 operators (42.9%) placed fewer than 10 USIVs during the observed study period, possibly affecting the initial success of attempted placements. A substantial proportion of USIVs were placed by a small number of RNs, and while USIVs placed by these RNs may have lasted longer this would support the idea that it is operator experience, rather than a patient or IV characteristic, that most influences SP. Also, our data analysis included operators’ initial catheter attempts and placements during their training period, which may have contributed to our greater than expected catheter failure rate within an hour of initial placement (16.1%). Additionally, our study only evaluated USIVs placed by RNs and did not include any placed by ED physicians or medical trainees.
Other chronic disease states (eg, peripheral arterial disease, heart failure, diabetes) were not evaluated and may have altered USIV survival. Finally, we did not assess for competing risks, such as death, accidental dislodgement, or removal at patient request. Additionally, as we had so few IV failures in our cohort, it is possible that a patient or IV characteristic does in fact influence survival, but our study was not able to detect the signal.
Conclusions
We found that USIV catheters appear to have a greater SP and longer median DT than previously reported. Patient characteristics (obesity, ESRD, ISDA) and IV location (upper arm) historically thought to be associated with reduced survival had no impact on outcomes in our study. These results are consistent with more contemporaneous data suggesting that survival of USIVs placed by well-trained individuals approaches that of IVs placed by standard technique.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Fields JM, Piela NE, Au AK, Ku BS. Risk factors associated with difficult venous access in adult ED patients. Am J Emerg Med. 2014;32(10):1179–1182. PMID: 25171796. doi:10.1016/j.ajem.2014.07.008
2. Elia F, Ferrari G, Molino P, et al. Standard-length catheters vs long catheters in ultrasound-guided peripheral vein cannulation. Am J Emerg Med. 2012;30(5):712–716. PMID: 21703801. doi:10.1016/j.ajem.2011.04.019
3. Au AK, Rotte MJ, Grzybowski RJ, Ku BS, Fields JM. Decrease in central venous catheter placement due to use of ultrasound guidance for peripheral intravenous catheters. Am J Emerg Med. 2012;30(9):1950–1954. PMID: 22795988. doi:10.1016/j.ajem.2012.04.016
4. Shokoohi H, Boniface K, McCarthy M, et al. Ultrasound-guided peripheral intravenous access program is associated with a marked reduction in central venous catheter use in noncritically ill emergency department patients. Ann Emerg Med. 2013;61(2):198–203. PMID: 23141920. doi:10.1016/j.annemergmed.2012.09.016
5. Costantino TG, Parikh AK, Satz WA, Fojtik JP. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann Emerg Med. 2005;46(5):456–461. PMID: 16271677. doi:10.1016/j.annemergmed.2004.12.026
6. Schoenfeld E, Shokoohi H, Boniface K. Ultrasound-guided peripheral intravenous access in the emergency department: patient-centered survey. West J Emerg Med. 2011;12(4):475–477. PMID: 22224141; PMCID: PMC3236135. doi:10.5811/westjem.2011.3.1920
7. Bauman M, Braude D, Crandall C. Ultrasound-guidance vs. standard technique in difficult vascular access patients by ED technicians. Am J Emerg Med. 2009;27(2):135–140. PMID: 19371518. doi:10.1016/j.ajem.2008.02.005
8. Carter T, Conrad C, Wilson JL, Dogbey G. Ultrasound guided intravenous access by nursing versus resident staff in a community based teaching hospital: a “noninferiority” trial. Emerg Med Int. 2015;2015:563139. doi:10.1155/2015/563139
9. Duran-Gehring P, Bryant L, Reynolds JA, Aldridge P, Kalynych CJ, Guirgis FW. Ultrasound-guided peripheral intravenous catheter training results in physician-level success for emergency department technicians. J Ultrasound Med. 2016;35(11):2343–2352. PMID: 27629755. doi:10.7863/ultra.15.11059
10. Miles G, Salcedo A, Spear D. Implementation of a successful registered nurse peripheral ultrasound-guided intravenous catheter program in an emergency department. J Emerg Nurs. 2012;38(4):353–356. PMID: 21514651. doi:10.1016/j.jen.2011.02.011
11. Bahl A, Hijazi M, Chen NW, Lachapelle-Clavette L, Price J. Ultralong versus standard long peripheral intravenous catheters: a randomized controlled trial of ultrasonographically guided catheter survival. Ann Emerg Med. 2020;76(2):134–142. PMID: 31955940. doi:10.1016/j.annemergmed.2019.11.013
12. Bahl A, Hang B, Brackney A, et al. Standard long IV catheters versus extended dwell catheters: a randomized comparison of ultrasound-guided catheter survival. Am J Emerg Med. 2019;37(4):715–721. PMID: 30037560. doi:10.1016/j.ajem.2018.07.031
13. Dargin JM, Rebholz CM, Lowenstein RA, Mitchell PM, Feldman JA. Ultrasonography-guided peripheral intravenous catheter survival in ED patients with difficult access. Am J Emerg Med. 2010;28(1):1–7. PMID: 20006193. doi:10.1016/j.ajem.2008.09.001
14. Mills CN, Liebmann O, Stone MB, Frazee BW. Ultrasonographically guided insertion of a 15-cm catheter into the deep brachial or basilic vein in patients with difficult intravenous access. Ann Emerg Med. 2007;50(1):68–72. PMID: 17433498. doi:10.1016/j.annemergmed.2007.02.003
15. Shokoohi H, Boniface KS, Kulie P, Long A, McCarthy M. The utility and survivorship of peripheral intravenous catheters inserted in the emergency department. Ann Emerg Med. 2019;74(3):381–390. PMID: 30926188. doi:10.1016/j.annemergmed.2019.02.003
16. Fields JM, Dean AJ, Todman RW, et al. The effect of vessel depth, diameter, and location on ultrasound-guided peripheral intravenous catheter longevity. Am J Emerg Med. 2012;30(7):1134–1140. PMID: 22078967. doi:10.1016/j.ajem.2011.07.027
17. Witting MD, Schenkel SM, Lawner BJ, Euerle BD. Effects of vein width and depth on ultrasound-guided peripheral intravenous success rates. J Emerg Med. 2010;39(1):70–75. PMID: 19272730. doi:10.1016/j.jemermed.2009.01.003
18. Pandurangadu AV, Tucker J, Brackney AR, Bahl A. Ultrasound-guided intravenous catheter survival impacted by amount of catheter residing in the vein. Emerg Med J. 2018;35(9):550–555. PMID: 30021833. doi:10.1136/emermed-2017-206803
19. Wallis MC, McGrail M, Webster J, et al. Risk factors for peripheral intravenous catheter failure: a multivariate analysis of data from a randomized controlled trial. Infect Control Hosp Epidemiol. 2014;35(1):63–68. PMID: 24334800. doi:10.1086/674398
20. Panebianco NL, Fredette JM, Szyld D, Sagalyn EB, Pines JM, Dean AJ. What you see (sonographically) is what you get: vein and patient characteristics associated with successful ultrasound-guided peripheral intravenous placement in patients with difficult access. Acad Emerg Med. 2009;16:1298–1303. PMID: 19912132. doi:10.1111/j.1553-2712.2009.00520.x
21. Gilbert EH, Lowenstein SR, Koziol-McLain J, Barta DC, Steiner J. Chart reviews in emergency medicine research: where are the methods? Ann Emerg Med. 1996;27(3):305–308. PMID: 8599488. doi:10.1016/s0196-0644(96)70264-0
22. Fung CM, Stayer DR, Terrasi JJ, et al. Extended dwell and standard ultrasound guided peripheral intravenous catheters: comparison of durability and reliability. Am J Emerg Med. 2021;47:267–273. PMID: 33989915; PMCID: PMC8364880. doi:10.1016/j.ajem.2021.05.005
23. O’Grady N, Alexander M, Burns L, et al. Guidelines for the prevention of intravascular catheter-related infections. centers for disease control and prevention; 2015. Available from: https://www.cdc.gov/infectioncontrol/guidelines/bsi/recommendations.html.
24. Zhao L, Claggett B, Tian L, et al. On the restricted mean survival time curve in survival analysis. Biometrics. 2016;72(1):215–221. PMID: 26302239; PMCID: PMC5114026. doi:10.1111/biom.12384
25. Kim DH, Uno H, Wei LJ. Restricted mean survival time as a measure to interpret clinical trial results. JAMA Cardiol. 2017;2(11):1179–1180. PMID: 28877311; PMCID: PMC6359932. doi:10.1001/jamacardio.2017.2922
26. Keyes LE, Frazee BW, Snoey ER, Simon BC, Christy D. Ultrasound-guided brachial and basilic vein cannulation in emergency department patients with difficult intravenous access. Ann Emerg Med. 1999;34(6):711–714. PMID: 10577399. doi:10.1016/s0196-0644(99)70095-8
27. Miles G, Newcomb P, Spear D. Comparison of dwell-times of two commonly placed peripheral intravenous catheters: traditional vs. ultrasound-guided. Open J Nurs. 2015;5:1082–1088. doi:10.4236/ojn.2015.512115
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


