Back to Journals » Research and Reports in Urology » Volume 11
Orthotopic Neobladder Reconstruction: Patient Selection And Perspectives
Authors Qu LG , Lawrentschuk N
Received 4 August 2019
Accepted for publication 26 September 2019
Published 11 December 2019 Volume 2019:11 Pages 333—341
DOI https://doi.org/10.2147/RRU.S181473
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jan Colli
Liang G Qu,1 Nathan Lawrentschuk1–4
1Department of Urology, Austin Health, Heidelberg, VIC, Australia; 2Department of Surgery, University of Melbourne, Heidelberg, VIC, Australia; 3Department of Surgical Oncology, Peter MacCallum Cancer Centre, Melbourne, VIC, Australia; 4EJ Whitten Prostate Cancer Research Centre, Epworth Healthcare, Melbourne, VIC, Australia
Correspondence: Nathan Lawrentschuk
Department of Surgery, University of Melbourne, Austin Hospital Suite 5, 210 Burgundy Street, Heidelberg, VIC 3084, Australia
Tel +61 3 9496 5000 Email [email protected]
Abstract: Orthotopic neobladder (ONB) reconstruction is a continent urinary diversion procedure that may be performed in a patient with bladder cancer following a radical cystectomy. The selection of a patient for an ONB reconstruction is strict as not everyone may be suitable to undergo this complex surgery. Patients must be not only mentally competent but also physically dexterous enough to allow for appropriate neobladder training post-procedure, to achieve best urinary function. However, even with a carefully chosen patient population, various complications specific to ONB reconstruction may result. Metabolic acidosis may result from electrolyte shifts, resulting in secondary complications such as bone demineralization and urinary calculi. In addition, nutritional deficiencies may result from the use of a transposed intestinal segment for the fashioning of the reservoir. A widely used outcome measure when assessing for ONB reconstruction is continence. With a strict neobladder training regimen, daytime continence may be achieved in roughly 70% of patients post-ONB procedure. This number may increase over the course of several years, although may decrease in up to 20 years of follow-up. Similarly, quality of life (QoL) measures have been widely studied, and current literature suggests slightly better QoL achieved with ONB compared to other urinary diversion procedures. Of note, the tools used to assess continence and QoL vary between studies, limiting the interpretability of the summarized data. Nevertheless, ONB reconstruction is a procedure that is still evolving, with ongoing modifications that can reduce complications and improve patient urinary function.
Keywords: neobladder, urinary diversion, bladder cancer
Introduction
Orthotopic neobladder (ONB) reconstruction procedures have been performed across the world, primarily for the surgical treatment of bladder cancer. Its technique has varied and evolved over time, with modifications to approaches, including the adoption of robot-assisted techniques. The use of ONB reconstruction usually follows a radical cystectomy (RC), therefore requiring the fashioning of a urinary reservoir to allow for a diverted lower urinary tract.
Although various urinary diversion procedures exist, ONB reconstruction may be the preferred option for a number of reasons. ONB reconstruction allows for the patient to be continent, allowing them to be able to control their urinary function and allowing for better quality of life (QoL) in comparison to other non-continent procedures, such as ileal conduit (IC) formation. Importantly, ONB reconstruction avoids the need for stoma formation - more than 60% of patients undergoing IC may be affected psychosocially.1
However, not all patients may be suitable for ONB reconstruction, as there are several considerations and contraindications that may prevent a patient from being a suitable candidate. In addition, several specific complications may result, both in relation to the intestinal and urinary systems. These are largely influenced by the patient’s baseline characteristics, including comorbidities and baseline continence. In addition, strict adherence to a voiding regime to prepare the neobladder is required to ensure the best outcomes for adequate continence and urinary function.
This review explores the various aspects of ONB reconstructions, including patient selection, overview of the procedure, the expected complications, and functional outcomes.
Patient Selection For Neobladder Reconstruction
ONB reconstructions are most commonly performed for patients with bladder cancer. The indications, considerations, and contraindications will be discussed. Although ONBs are mainly performed for patients with bladder cancer, there have been case reports of ONBs being utilized in various other benign conditions (e.g. interstitial cystitis) refractory to conservative measures, as well as in patients with neurogenic bladder.2,3 Nevertheless, this section will focus on the management and selection of patients who have undergone RC secondary to bladder cancer.
Bladder cancer ranks as the world’s tenth most common cancer. Its incidence worldwide was approximately 500,000 in 2018 with almost 200,000 deaths.4 Bladder cancer control remains a challenging field, with limited early detection methods and modest systemic therapies.5 Various guidelines published by urological and oncological authority bodies have outlined indications for undergoing RC and subsequent urinary diversion. The general indications for performing RC with urinary diversion are primarily: residual high-grade T1 disease in non-muscle invasive cancer; muscle invasive disease at re-resection; primary treatment for cT2-4a disease, along with neoadjuvant chemotherapy and a pelvic lymphadenectomy.6 Staging of bladder cancer should incorporate either magnetic resonance imaging or positron emission tomography, for their superior sensitivity to detect lymph node metastases, compared to computed tomography.7 The choices of open or robotic-assisted RC have comparable oncologic and QoL outcomes, and either surgical approach may be utilized.8
The decision regarding choice of urinary diversion, however, depends on several factors (Table 1). The choice of performing ONB post-RC depends on variables relating to both the patient and the surgeon. Of note, patients may have baseline characteristics that prevent them from being suitable candidates for ONB reconstruction. Patients who undergo ONBs are often younger compared to patients undergoing ICs, with the mean and median age of these patients reported frequently under 65-years old.9 However, older age is not a contraindication - older patients who still have good physical and cognitive capacity may be able to adequately manage the care required post-operation.10 In addition, patients often have better baseline health in comparison to patients who undergo ICs, with lower body mass index (BMI), lower American Society of Anesthesiology (ASA) score, and fewer general medical comorbidities.9 After the procedure, surgeons must also consider the patient’s ability to adapt to the requirements of caring and managing the ONB. A strict compliance to a neobladder training programme is required to help patients achieve best QoL. An adequate level of physical dexterity and mental cognition is required to ensure patients are able to understand the demands of self-care.11 To aid the complex patient selection process, formally studied frailty indices have been reported and may be used to identify patients suitable for ONB reconstruction.12 Although definitions for frailty may vary between studies, a frailty index may better predict risk of post-operative complications compared to age, BMI or ASA score. These indices should be further studied for their role in patient selection.13
 |
Table 1 Advantages And Disadvantages Of Performing An Orthotopic Neobladder |
Surgeon factors are also important in the decision to undergo ONB. With several decades of use and multiple variations that may be performed, surgeon experience is necessary to ensure minimal complications result. The experience of surgeons has been demonstrated to be a prognostic predictor for QoL post-procedure, as less experience may result in higher prevalence of post-operative incontinence.14 This may also explain the diminishing number of ONB procedures being performed across the world - a vicious cycle is created from: decreasing frequency of procedures being performed, leading to less opportunity to train for the procedure to maintain surgical experience.15 There is therefore a push to ensure ONBs are performed in high-volume centres, allowing for maintained surgical exposure and high-volume follow-up to monitor and minimize rates of complications and improve patient outcomes.16
Contraindications
Despite the various considerations above however, there are contraindications to performing ONB reconstructions on patients (Table 2). Patients who have pre-existing renal or liver impairment should not undergo ONB reconstruction.17,18 Due to the intestinal segment transposed and utilized for the ONB, urinary wastes including creatinine, urea and ammonia may be reabsorbed into systemic circulation, increasing the burden of waste excretion mechanisms and potentially worsening pre-existing impairment.3
 |
Table 2 Contraindications And Considerations For ONB Reconstruction |
Extensive cancer disease may limit the ability to construct an ONB with adequate oncological and QoL outcomes. In particular, cancer to the prostatic apex or bladder neck prohibits the urethral anastomosis stage during the procedure.17,18 Cancer affecting the distal urethra should also be ruled out prior to considering ONB reconstruction.11
Finally, any pre-existing incontinence secondary to urethral rhabdosphincter insufficiency will impair post-procedure continence.11 An alternative urinary diversion route should be considered if this is the case.
Overview Of Procedure And Perioperative Management
As ONB reconstructions are complex oncological procedures, there should be a strong emphasis on adequate preoperative counselling and patient education, with a comprehensive multidisciplinary approach involving both face-to-face discussions and accessible, reliable, online health information.3,19 The team would often consist of physicians, urology nurses, stoma nurses, as well as other allied health input including physiotherapists. Patients should be informed of not only the peri-operative management, but also the ongoing need and expectations for neobladders training, as well as expected oncological and QoL outcomes.
Performing ONB reconstructions may rely on any one of the many reported techniques. These include: Kock, T-pouch, Studer, Hautmann, Abol-Enein, Ghoneim and vescica ileale Padovana. ONBs relying on different intestinal segments include ileocolonic neobladders, such as the Mainz pouch, or sigmoid neobladder, such as the Reddy pouch.20 The main considerations that have resulted in a range of accepted techniques include: the type of intestinal segment used, and the folding construction of the reservoir. Different portions of the bowel may be preferred to others and may result in differing quality and function. In particular, terminal ileum is commonly used due to its ability to distend more and hold more volume. In addition, once used for ONB reconstruction, its mucosa may undergo atrophy over time, decreasing electrolyte exchange and subsequent systemic metabolic disturbances.20 The folding construction of the reservoir may also be performed in different ways to achieve a spherical reservoir. Due to the tubular shape of the intestine, different techniques may be used to re-fashion and create a reservoir with lower wall pressure on distension.21 In addition, a spherical reservoir ensures a low surface area-to-volume ratio, decreasing risk of metabolic consequences resulting from electrolyte shifts.
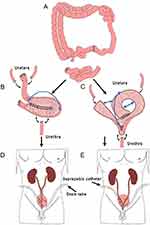
Ongoing modifications and novel techniques are still being reported, for not only varied ways of folding the segments but also utility of different segments, segment lengths, and surgical approaches.22–24 The general principles for an ONB reconstruction are still preserved throughout the different techniques (Figure 1). To use the Studer pouch as an example, an ileal segment is isolated, with bowel continuity restored. Ureters are spatulated and anastomosed end-to-side to the ileal segment. The fashioning of the reservoir into a spherical shape is performed, known as detubularization. A caudal reservoir outlet is fashioned and anastomosed to the membranous urethra, with the urethral sphincter mechanism preserved for continence. Cystostomy tube and ureteric stents should be placed during the procedure and left in.11 A large capacity reservoir of up to 4–500 mL should result using this procedure.25
In addition to the open ONB reconstruction, there is also a growing number of centres performing robotic-assisted procedures for neobladder construction.24,26–29 These may be done similarly to open approaches, with the ability to fashion the neobladder within the body, i.e. intracorporeally. However, the same principles apply, where a similar length of intestine is isolated, detubularized, and adequately anastomosed. These techniques are being evolved over time to improve efficiency, reduce complications, as well as achieve comparable oncologic outcomes compared to open ONB reconstruction.30,31
Neobladder Training
After completion of the procedure, an indwelling catheter and a suprapubic catheter should remain in situ to allow for post-operative neobladder healing.25 Routine practices have previously been described, where regular flushing of the catheter with normal saline post-operatively prevents catheter blockage. The indwelling catheter may be removed at day 10 post-procedure, however anastomotic leaks must first be ruled out. Leaks may result from breakdown of any of the anastomoses completed, including the ureters or the neobladder itself. Leaks may be identified from an increase in pelvic drain output and a decrease in monitored urine output. A leak may be confirmed by assessing the fluid creatinine concentration. In addition, a cystogram may also be performed to ensure neobladder healing is adequate.25 The suprapubic catheter may be subsequently removed if there are no issues after the removal of the indwelling catheter.
Beyond the immediate post-operative period, there is ongoing neobladder rehabilitation required to attain the best results in function. Patients must learn neobladder emptying techniques, as well as intermittent self-catheterization as this may potentially be needed. As neobladders are unable to contract like a native bladder, voiding may be achieved by performing a Valsalva manoeuvre accompanied by pelvic floor relaxation.25 Additional intra-abdominal pressure to assist voiding may also be achieved by gentle manual pressure over the suprapubic area, or by positioning (e.g. sitting or leaning forward).
Post-procedure neobladder training also involves training the bladder to slowly increase in the amount of distension it can withstand to increase reservoir capacity. This may be achieved by slowly decreasing the frequency of voids, which initially may be as regular as 2 to 3 hourly daily, to 5 to 6 hourly after a demonstrated 2–3 weeks of successful voiding.25,32 Monitoring of bladder volumes and post-void residual volumes should be done to identify patients who may be recommended more frequent voids to avoid overflow incontinence. High residual volumes that do not improve over time may require patients to undergo intermittent self-catheterization. Comorbidities (OR: 9.0) and BMI (OR 1.5) have both been reported as predictors of patients who may need intermittent self-catheterization.33
In addition to the above neobladder-specific points, general post-operative measures should also be taken. Patients should be advised to avoid driving, heavy lifting, as well as any sexual activity for 2 to 3 months.25
Complications And Patient Outcomes
More than half of all patients undergoing orthotopic reconstruction will experience complications within 90 days of surgery.34 Various specific complications may result after ONB reconstruction and account for the majority of reported complications. These are mostly sequelae secondary to disturbances of the intestinal and urinary tracts. Rare complications may also result, including ureteroileal strictures, neobladder fistulas, and spontaneous neobladder rupture.16 In addition, general post-operative complications may also be present and account for roughly 20% of the reported complications.25,34 Within the immediate post-operative period, infectious sequelae such as intraabdominal abscesses or urinary tract infections have been most commonly reported complications. Genitourinary (hydronephrosis), gastrointestinal (ileus, bowel obstruction), and wound-related complications (infection, dehiscence) may also be expected in these patients. Other complications may also manifest post-surgery, from bladder cancer treatments such as previous radiotherapy.35 The overall long-term complication rate has been reported to be 40.8%, with overall survival rates of 65.5%, 49.8%, and 28.3% at 5, 10, and 20 years, respectively.16
Electrolyte Balance
Due to the greater permeability of the intestinal mucosa to electrolytes, a neobladder allows for increased metabolic shifts of electrolytes in urine that may be systemically absorbed. The absorption of potassium, hydrogen and chloride ions may result in a hyperchloraemic hyperkalaemic metabolic acidosis. A salt-loss syndrome may also result from fluid being osmotically shifted into the electrolyte-rich urine, manifesting as general malaise and dehydration.17,18,25 Metabolic acidosis should be monitored throughout the post-operation follow-up period, as up to roughly half of patients may have confirmed metabolic acidosis 1-month post-procedure.36 In particular, patients with pre-existing renal impairment, as well as diabetes, are both more prone to developing metabolic acidosis in the post-operative period.36 A chronic metabolic acidosis may include calcium resorption and decreased circulating phosphate levels, leading to osteomalacia and osteoporosis.17
High urinary calcium secondary to the metabolic acidosis may also predispose patients with ONBs to a higher risk of urinary calculi.17,18 Of note, rates of bladder calculi can be up to 10–20% of individuals and are often composed of struvite, secondary to urease-splitting organisms such as Proteus and Klebsiella species.37 This risk is increased especially with the risk of urinary tract infections (UTIs) and bacterial colonization associated with ONB formation.38
Regular serum electrolyte monitoring should be performed throughout the follow-up period.39 Identifying metabolic acidosis should be done as early as possible, followed by prompt management to avoid complications. Treatment options used primarily address correcting the electrolyte abnormalities. Daily oral sodium bicarbonate supplementation may be used to correct the acidosis, as well as increasing salt intake, and a review of the electrolyte-altering medications a patient may be taking.25 Up to 33% of patients may be expected to take long-term bicarbonate supplementation.16 In addition, re-catheterizing the ONB in the acute post-operative setting may decrease the amount of urine residing in the neobladder that is responsible for electrolyte shifts. Treating any existing UTI may also help prevent the development of urinary calculi.
Nutrition
Patients undergoing ONB reconstructions are subject to standard perioperative complications such as post-operative ileus. A greater risk of ileus is present for ONB reconstruction compared to other urinary diversion techniques such as IC formation, with an incidence of up to 14.8%.18,40 However, specific nutrition-related complications may result from transposition of the intestinal segment for ONB reconstruction. In particular, the shortening of remaining terminal ileum will lead to decreased bile acid reabsorption, resulting in fatty diarrhoea and dehydration. The decreased ability to absorb vitamin B and folic acid means appropriate nutritional supplementation must also be taken to avoid consequences of micronutrient deficiencies.18,40
Continence
Continence remains one of the most important outcomes for patients after ONB reconstruction. The ability to gain continence majorly influences a patient’s perspective on their QoL - affecting their sleep, mood, personal wellbeing, and social life. Although it has been widely reported across different countries and different reconstruction techniques, the data are difficult to interpret largely due to the difference in definitions utilized among studies reporting this measure. Various standardized methods of evaluation have been proposed in other reports and should be used to improve generalizability and interpretability of ONB reconstruction techniques.20
The prevalence of continence can vary greatly, and different rates have been reported for daytime as well as at night-time. Daytime continence has been reported to range from 21−70% at 12 months post-procedure.41–43 Continence may improve over the course of several years, where up to 92% of patients were continent at 4 years, compared to only 70% at 12 months.43 In the long term, continence prevalence largely improves in most patients, with daytime continence rates of up to 92%, 90% and 79% at 10, 15 and 20 years post-procedure, respectively.44 At 12 months, prevalence of night-time continence has also been reported to vary greatly, from 19% to 79% of patients.33,42–46 Similar to the daytime continence rates, night-time continence may improve over years following the procedure, with 73% of patients being continent versus 90% at 4 years post-procedure.43 Rates of night-time incontinence at 10, 15 and 20 years have been reported to be 70%, 65% and 55%, respectively.44
As expected, incontinence rates are widely reported as being higher than the healthy population. One study comparing patients with modified S-pouch ONB with healthy controls demonstrated nocturnal incontinence rate of up to 28% compared to 3.7% in healthy individuals (p=0.003).43 However, some pre-operative characteristics predict better continence outcomes, such as performance status, and fewer comorbidities such as ischaemic heart disease.47 In addition, a retained sensation of a filling ONB post-procedure is a predictor for better overall daytime continence.47 Patients with large post-void residual volumes and frequent uninhibited contractions identified on urodynamic studies are more likely to develop night-time incontinence.48 Trials are ongoing, examining the efficacy of oxybutynin as well as verapamil, where a small cohort had up to 70% and 55% response respectively, improving night-time incontinence.49
Sexual Function
The majority of studies examining sexual function have focused on male patients and predictors and prevalence of sexual function post-RC and ONB reconstruction. Traditionally, erectile function has been reported to be retained in between 24% and 36% of patients post-ONB reconstruction.33,50,51 However, RC approaches with neurovascular bundle preservation may help preserve erectile function. Potency rates of up to 60% have been achieved in patients up to 2 years post-procedure.52 The use of a prostate-sparing cystectomy may also be considered, where patients may experience improved sexual function as well as overall better physical function without affecting oncological outcomes.53 Compared to healthy controls, patients undergoing ONB are still significantly more likely to have less erectile function.51 One study demonstrated approximately 36% of patients as being potent, compared to 83% in healthy controls (p=0.003).50
In terms of preserving sexual desire, there are conflicting reports regarding whether ONB are superior to other forms of urinary diversion. The evidence is directed towards better sexuality preservation with ONB reconstruction, where in one study, up to 17.5% of patients undergoing ONB reconstruction reported unaltered sexual desire.54
There is limited evidence examining sexual outcomes for females post-ONBs. A recent study by Veskimae et al, however, reported improved sexual and urinary function outcomes, using a pelvic organ preserving technique when performing RC and ONB reconstruction.55
Quality Of Life
The measure of QoL is a widely studied measure for patients with ONB reconstruction. QoL measures commonly evaluate a range of domains affecting a patient’s physical and mental health after undergoing RC with ONB formation. For patients with ONBs, the measure of QoL has unfortunately been measured using a range of tools, making inter-study comparisons challenging. Nevertheless, a number of variables have demonstrated associations for patients who undergo ONB reconstruction. Patients with pre-operative better Eastern Cooperative Oncology Group (ECOG) performance status and daytime continence are likely to have better post-procedure QoL.14 In addition, the amount of surgeon experience in performing ONB procedures may also affect subsequent QoL, highlighting the need for ongoing training and skill required to maintain ONB as an effective procedure with good functional outcomes.14
Several reviews have collated and summarized the range of evidence produced by QoL studies for patients with ONB reconstruction. Across the range of studies, the main measures used for QoL were:
European Organization for Research and Treatment of Cancer Quality of Life Core 30, 36-item Short Form Health Survey score, The Functional Assessment of Cancer Therapy for Bladder Cancer, and the Bladder Cancer Index.
One review examined post-RC QoL, and demonstrated ONBs had superior emotional function and body image compared to other urinary diversion methods.56 A systematic review by Cerruto et al examined combined QoL outcomes for ONBs versus ICs, and demonstrated better QoL in patients with ONB although being non-significant (Heades’ g=0.150; p=0.066).57 Another review, by Ghosh et al in 2016, examining QoL post-urinary diversion also suggested ONBs produced better QoL than other methods of urinary diversion.58 Despite these summarized reviews suggesting overall better QoL with ONBs, there have been some studies that demonstrate no difference in outcomes with ONB reconstruction, however the scores utilized vary from study to study, limiting their generalizability.1,59–62 One study has conversely demonstrated significantly worse urinary symptoms in the neobladder population.63 Studies have however widely demonstrated that patients with ONB reconstruction are likely to have significantly worse QoL than the general population, as demonstrated in the United States, as well as in Italy.59,61
Conclusion
ONB reconstructions have been widely performed and described throughout literature. Its use is largely for the treatment of bladder cancer, where adequate surgical control is required. Patients must be able to tolerate the post-procedure neobladder rehabilitation as well as be vigilant of the possible complications that may result in both the short and long term. Even then, patients may not all be able to experience a full return to pre-operative functional status, and some incontinence and general decrease in QoL should be expected. Nevertheless, ONB reconstruction remains an important procedure that is still evolving, with improvements to both oncological control and patient functional status.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Philip J, Manikandan R, Venugopal S, Desouza J, Javle PM. Orthotopic neobladder versus ileal conduit urinary diversion after cystectomy – a quality-of-life based comparison. Ann R Coll Surg Engl. 2009;91(7):565–569. doi:10.1308/003588409X432293
2. Maurice MJ, Meeks JJ, Smith ND. Orthotopic neobladder for bladder cancer and neurogenic bladder dysfunction. Can J Urol. 2008;15(4):4194–4195.
3. Ong K, Herdiman O, Johnson L, Lawrentschuk N. Orthotopic bladder substitution (neobladder): part I: indications, patient selection, preoperative education, and counseling. J Wound Ostomy Continence Nurs. 2013;40(1):73–82. doi:10.1097/WON.0b013e31827759ea
4. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
5. Lawrentschuk N. Bladder cancer: working towards better outcomes. Minerva Urol Nefrol. 2016;68(2):105.
6. Spiess PE, Agarwal N, Bangs R, et al. Bladder cancer, version 5.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2017;15(10):1240–1267. doi:10.6004/jnccn.2017.0156
7. Crozier J, Papa N, Perera M, et al. Comparative sensitivity and specificity of imaging modalities in staging bladder cancer prior to radical cystectomy: a systematic review and meta-analysis. World J Urol. 2019;37(4):667–690. doi:10.1007/s00345-018-2439-8
8. Sathianathen NJ, Kalapara A, Frydenberg M, et al. Robotic assisted radical cystectomy vs open radical cystectomy: systematic review and meta-analysis. J Urol. 2019;201(4):715–720. doi:10.1016/j.juro.2018.10.006
9. Crozier J, Hennessey D, Sengupta S, Bolton D, Lawrentschuk N. A systematic review of Ileal conduit and neobladder outcomes in primary bladder cancer. Urology. 2016;96:74–79. doi:10.1016/j.urology.2016.06.034
10. Saika T, Suyama B, Murata T, et al. Orthotopic neobladder reconstruction in elderly bladder cancer patients. Int J Urol. 2001;8(10):533–538. doi:10.1046/j.1442-2042.2001.00367.x
11. Studer UE, Varol C, Danuser H. Orthotopic ileal neobladder. BJU Int. 2004;93(1):183–193. doi:10.1111/j.1464-410x.2004.04641.x
12. Sathianathen NJ, Jarosek S, Lawrentschuk N, Bolton D, Konety BR. A simplified frailty index to predict outcomes after radical cystectomy. Eur Urol Focus. 2018;5:658–663.
13. De Nunzio C, Cicione A, Izquierdo L, et al. Multicenter analysis of postoperative complications in octogenarians after radical cystectomy and ureterocutaneostomy: the role of the Frailty index. Clin Genitourin Cancer. 2019. doi:10.1016/j.clgc.2019.07.002
14. Kretschmer A, Grimm T, Buchner A, Stief CG, Karl A. Prognostic features for quality of life after radical cystectomy and orthotopic neobladder. Int Braz J Urol. 2016;42(6):1109–1120. doi:10.1590/S1677-5538.IBJU.2015.0491
15. Hautmann RE. Declining use of orthotopic reconstruction worldwide – what went wrong? J Urol. 2018;199(4):900–903. doi:10.1016/j.juro.2017.10.031
16. Hautmann RE, de Petriconi RC, Volkmer BG. 25 years of experience with 1,000 neobladders: long-term complications. J Urol. 2011;185(6):2207–2212. doi:10.1016/j.juro.2011.02.006
17. Wiederkehr M, Krapf R. Metabolic and endocrine effects of metabolic acidosis in humans. Swiss Med Wkly. 2001;131(9–10):127–132.
18. Stein R, Schroder A, Thuroff JW. Bladder augmentation and urinary diversion in patients with neurogenic bladder: non-surgical considerations. J Pediatr Urol. 2012;8(2):145–152. doi:10.1016/j.jpurol.2011.03.015
19. Corfield JM, Abouassaly R, Lawrentschuk N. Health information quality on the internet for bladder cancer and urinary diversion: a multi-lingual analysis. Minerva Urol Nefrol. 2018;70(2):137–143. doi:10.23736/S0393-2249.17.02952-6
20. Chang DT, Lawrentschuk N. Orthotopic neobladder reconstruction. Urol Ann. 2015;7(1):1–7. doi:10.4103/0974-7796.148553
21. Basford JR. The law of Laplace and its relevance to contemporary medicine and rehabilitation. Arch Phys Med Rehabil. 2002;83(8):1165–1170. doi:10.1053/apmr.2002.33985
22. Bianchi G, Sighinolfi MC, Pirola GM, Micali S. Studer orthotopic neobladder: a modified surgical technique. Urology. 2016;88:222–225. doi:10.1016/j.urology.2015.11.020
23. Yadav SS, Gangkak G, Mathur R, Yadav RG, Tomar V. Long-term functional, urodynamic, and metabolic outcome of a modified orthotopic neobladder created with a short ileal segment: our 5-year experience. Urology. 2016;94:167–172. doi:10.1016/j.urology.2016.04.013
24. Chopra S, de Castro Abreu AL, Berger AK, et al. Evolution of robot-assisted orthotopic ileal neobladder formation: a step-by-step update to the University of Southern California (USC) technique. BJU Int. 2017;119(1):185–191. doi:10.1111/bju.13611
25. Herdiman O, Ong K, Johnson L, Lawrentschuk N. Orthotopic bladder substitution (Neobladder): part II: postoperative complications, management, and long-term follow-up. J Wound Ostomy Continence Nurs. 2013;40(2):171–180. quiz E1-2. doi:10.1097/WON.0b013e31827e8499
26. Ginot R, Rouget B, Bensadoun H, et al. [Radical cystectomy with orthotopic neobladder replacement: comparison of robotic assisted and open surgical route]. Prog Urol. 2016;26(8):457–463. doi:10.1016/j.purol.2016.06.009
27. Satkunasivam R, Santomauro M, Chopra S, et al. Robotic intracorporeal orthotopic neobladder: urodynamic outcomes, urinary function, and health-related quality of life. Eur Urol. 2016;69(2):247–253. doi:10.1016/j.eururo.2015.06.041
28. Dal Moro F, Ves.Pa ZF. Designing a novel robotic intracorporeal orthotopic ileal neobladder. Urology. 2016;91:99–103.
29. Minervini A, Vanacore D, Vittori G, et al. Florence robotic intracorporeal neobladder (FloRIN): a new reconfiguration strategy developed following the IDEAL guidelines. BJU Int. 2018;121(2):313–317. doi:10.1111/bju.14077
30. Simone G, Tuderti G, Misuraca L, et al. Perioperative and mid-term oncologic outcomes of robotic assisted radical cystectomy with totally intracorporeal neobladder: results of a propensity score matched comparison with open cohort from a single-centre series. Eur J Surg Oncol. 2018;44(9):1432–1438. doi:10.1016/j.ejso.2018.04.006
31. Lawrentschuk N. Editorial comment. J Urol. 2017;198(3):573–574. doi:10.1016/j.juro.2017.02.3378
32. Steers WD. Voiding dysfunction in the orthotopic neobladder. World J Urol. 2000;18(5):330–337.
33. Novara G, Ficarra V, Minja A, De Marco V, Artibani W. Functional results following vescica ileale Padovana (VIP) neobladder: midterm follow-up analysis with validated questionnaires. Eur Urol. 2010;57(6):1045–1051. doi:10.1016/j.eururo.2010.01.007
34. Hautmann RE, de Petriconi RC, Volkmer BG. Lessons learned from 1,000 neobladders: the 90-day complication rate. J Urol. 2010;184(3):990–994. quiz 1235. doi:10.1016/j.juro.2010.05.037
35. Ma JL, Hennessey DB, Newell BP, Bolton DM, Lawrentschuk N. Radiotherapy-related complications presenting to a urology department: a more common problem than previously thought? BJU Int. 2018;121(Suppl 3):28–32. doi:10.1111/bju.14145
36. Kim KH, Yoon HS, Yoon H, et al. Risk factors for developing metabolic acidosis after radical cystectomy and ileal neobladder. PLoS One. 2016;11(7):e0158220. doi:10.1371/journal.pone.0158220
37. Turk TM, Koleski FC, Albala DM. Incidence of urolithiasis in cystectomy patients after intestinal conduit or continent urinary diversion. World J Urol. 1999;17(5):305–307.
38. Wullt B, Agace W, Mansson W. Bladder, bowel and bugs–bacteriuria in patients with intestinal urinary diversion. World J Urol. 2004;22(3):186–195. doi:10.1007/s00345-004-0432-x
39. Alberti C. Metabolic and histological complications in ileal urinary diversion. Challenges of tissue engineering technology to avoid them. Eur Rev Med Pharmacol Sci. 2007;11(4):257–264.
40. Thorstenson A, Jacobsson H, Onelov E, Holst JJ, Hellstrom PM, Kinn AC. Gastrointestinal function and metabolic control after construction of an orthotopic ileal neobladder in bladder cancer. Scand J Urol Nephrol. 2007;41(1):14–19. doi:10.1080/00365590600911217
41. Aleksic P, Bancevic V, Milovic N, et al. Short ileal segment for orthotopic neobladder: a feasibility study. Int J Urol. 2010;17(9):768–773. doi:10.1111/j.1442-2042.2010.02599.x
42. Ahmadi H, Skinner EC, Simma-Chiang V, et al. Urinary functional outcome following radical cystoprostatectomy and ileal neobladder reconstruction in male patients. J Urol. 2013;189(5):1782–1788. doi:10.1016/j.juro.2012.11.078
43. Sevin G, Soyupek S, Armagan A, Hoscan MB, Oksay T. Ileal orthotopic neobladder (modified Hautmann) via a shorter detubularized ileal segment: experience and results. BJU Int. 2004;94(3):355–359. doi:10.1111/j.1464-410X.2004.04933.x
44. Furrer MA, Roth B, Kiss B, et al. Patients with an orthotopic low pressure bladder substitute enjoy long-term good function. J Urol. 2016;196(4):1172–1180. doi:10.1016/j.juro.2016.04.072
45. Studer UE, Burkhard FC, Schumacher M, et al. Twenty years experience with an ileal orthotopic low pressure bladder substitute – lessons to be learned. J Urol. 2006;176(1):161–166. doi:10.1016/S0022-5347(06)00573-8
46. Thulin H, Kreicbergs U, Wijkstrom H, Steineck G, Henningsohn L. Sleep disturbances decrease self-assessed quality of life in individuals who have undergone cystectomy. J Urol. 2010;184(1):198–202. doi:10.1016/j.juro.2010.03.009
47. Kretschmer A, Grimm T, Buchner A, et al. Prognostic features for objectively defined urinary continence after radical cystectomy and ileal orthotopic neobladder in a contemporary cohort. J Urol. 2017;197(1):210–215. doi:10.1016/j.juro.2016.08.004
48. El Bahnasawy MS, Osman Y, Gomha MA, Shaaban AA, Ashamallah A, Ghoneim MA. Nocturnal enuresis in men with an orthotopic ileal reservoir: urodynamic evaluation. J Urol. 2000;164(1):10–13. doi:10.1097/00005392-200007000-00003
49. El-Bahnasawy MS, Shaaban H, Gomha MA, Nabeeh A. Clinical and urodynamic efficacy of oxybutynin and verapamil in the treatment of nocturnal enuresis after formation of orthotopic ileal neobladders. A prospective, randomized, crossover study. Scand J Urol Nephrol. 2008;42(4):344–351. doi:10.1080/00365590701832726
50. Protogerou V, Moschou M, Antoniou N, Varkarakis J, Bamias A, Deliveliotis C. Modified S-pouch neobladder vs ileal conduit and a matched control population: a quality-of-life survey. BJU Int. 2004;94(3):350–354. doi:10.1111/j.1464-410X.2004.04932.x
51. Asgari MA, Safarinejad MR, Shakhssalim N, Soleimani M, Shahabi A, Amini E. Sexual function after non-nerve-sparing radical cystoprostatectomy: a comparison between ileal conduit urinary diversion and orthotopic ileal neobladder substitution. Int Braz J Urol. 2013;39(4):474–483. doi:10.1590/S1677-5538.IBJU.2013.04.04
52. Kessler TM, Burkhard FC, Perimenis P, et al. Attempted nerve sparing surgery and age have a significant effect on urinary continence and erectile function after radical cystoprostatectomy and ileal orthotopic bladder substitution. J Urol. 2004;172(4 Pt 1):1323–1327. doi:10.1097/01.ju.0000138249.31644.ec
53. Chen PY, Chiang PH. Comparisons of quality of life and functional and oncological outcomes after orthotopic neobladder reconstruction: prostate-sparing cystectomy versus conventional radical cystoprostatectomy. Biomed Res Int. 2017;2017:1983428.
54. Asgari MA, Safarinejad MR, Shakhssalim N, Soleimani M, Shahabi A, Amini E. Quality of life after radical cystectomy for bladder cancer in men with an ileal conduit or continent urinary diversion: a comparative study. Urol Ann. 2013;5(3):190–196. doi:10.4103/0974-7796.115747
55. Veskimae E, Neuzillet Y, Rouanne M, et al. Systematic review of the oncological and functional outcomes of pelvic organ-preserving radical cystectomy (RC) compared with standard RC in women who undergo curative surgery and orthotopic neobladder substitution for bladder cancer. BJU Int. 2017;120(1):12–24. doi:10.1111/bju.13819
56. Yang LS, Shan BL, Shan LL, et al. A systematic review and meta-analysis of quality of life outcomes after radical cystectomy for bladder cancer. Surg Oncol. 2016;25(3):281–297. doi:10.1016/j.suronc.2016.05.027
57. Cerruto MA, D’Elia C, Siracusano S, et al. Systematic review and meta-analysis of non RCT’s on health related quality of life after radical cystectomy using validated questionnaires: better results with orthotopic neobladder versus ileal conduit. Eur J Surg Oncol. 2016;42(3):343–360. doi:10.1016/j.ejso.2015.10.001
58. Ghosh A, Somani BK. Recent trends in postcystectomy health-related Quality of Life (QoL) favors neobladder diversion: systematic review of the literature. Urology. 2016;93:22–26. doi:10.1016/j.urology.2015.12.079
59. Autorino R, Quarto G, Di Lorenzo G, et al. Health related quality of life after radical cystectomy: comparison of ileal conduit to continent orthotopic neobladder. Eur J Surg Oncol. 2009;35(8):858–864. doi:10.1016/j.ejso.2008.08.002
60. Hedgepeth RC, Gilbert SM, He C, Lee CT, Wood DP
61. Fujisawa M, Isotani S, Gotoh A, Okada H, Arakawa S, Kamidono S. Health-related quality of life with orthotopic neobladder versus ileal conduit according to the SF-36 survey. Urology. 2000;55(6):862–865. doi:10.1016/s0090-4295(00)00483-0
62. Sogni F, Brausi M, Frea B, et al. Morbidity and quality of life in elderly patients receiving ileal conduit or orthotopic neobladder after radical cystectomy for invasive bladder cancer. Urology. 2008;71(5):919–923. doi:10.1016/j.urology.2007.11.125
63. Gilbert SM, Wood DP, Dunn RL, et al. Measuring health-related quality of life outcomes in bladder cancer patients using the Bladder Cancer Index (BCI). Cancer. 2007;109(9):1756–1762. doi:10.1002/cncr.22556
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.