Back to Journals » International Medical Case Reports Journal » Volume 12
Orbital cellulitis clinically mimicking rhabdomyosarcoma
Authors Amir SP, Kamaruddin MI , Akib MNR, Sirajuddin J
Received 15 January 2019
Accepted for publication 8 July 2019
Published 26 August 2019 Volume 2019:12 Pages 285—289
DOI https://doi.org/10.2147/IMCRJ.S201678
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Suliati P Amir,1,2 Muhammad Irfan Kamaruddin,1 Marliyanti Nur Rahmah Akib,1,2 Junaedi Sirajuddin1
1Department of Ophthalmology, Hasanuddin University, Makassar, South Sulawesi, Indonesia; 2Department of Ophthalmology, Muslim University of Indonesia, Makassar, South Sulawesi, Indonesia
Correspondence: Muhammad Irfan Kamaruddin
Department of Ophthalmology, Hasanuddin University, Jalan Antang Raya, Kompleks Beverly Hills Blok B 21, RT 009/RW 001, Kelurahan Antang, Kecamatan Manggala, Makassar 90234, South Sulawesi, Indonesia
Tel +62 8 524 015 9116
Email [email protected]
Introduction: Proptosis in children with acute-onset accompanied by signs of inflammation is commonly caused by orbital cellulitis, however, the possibility of rhabdomyosarcoma should always be considered by the clinician. This is a case report of a five-year-old boy presenting with an acute-onset of proptosis without a history of trauma and systemic infection. Our clinical differential diagnosis included orbital cellulitis and orbital rhabdomyosarcoma.
Purpose: To report a case of orbital cellulitis that clinically and radiologically mimics rhabdomyosarcoma.
Case presentation: A five-year-old boy presented with rapid-onset proptosis, periorbital edema, pain and visual loss in the left eye for two weeks without a history of trauma, upper respiratory tract infection, sinusitis or immunosuppression. Our clinical differential diagnosis includes rhabdomyosarcoma and orbital cellulitis. Complete blood count reveals a leukocytosis. Multislice computed tomography (MSCT) scan shows lesions involving the lateral orbit and the retro bulbar space. Antibiotics combination and adjunct anti-inflammatory intravenously shows excellent clinical resolution.
Conclusions: The study demonstrates difficulty in differentiating acute orbital cellulitis from rhabdomyosarcoma based on clinical findings. In addition, the case highlights that antibiotic combination of cephalosporin and aminoglycosides together with an adjuvant corticosteroid as an anti-inflammatory was effective in the case of acute orbital cellulitis.
Keywords: proptosis, corticosteroid, cellulitis, rhabdomyosarcoma
Introduction
Orbital cellulitis is the most common serious eye infection in children.1 Classic clinical findings include fever, leukocytosis, erythema, proptosis, chemosis, ptosis, restriction of and pain with ocular movement, loss of visual acuity and an afferent pupillary defect.2–5 Orbital cellulitis usually appears as acute-onset proptosis with signs of inflammation. However, in thosecircumstances, rhabdomyosarcoma should also be considered because it is also well known for its rapid unilateral proptosis.6,7 Orbital rhabdomyosarcoma is an orbital malignancy that is also common in children and has been reported to be responsible for 4% of all orbital masses in children.6–9 We report a case of orbital cellulitis that mimics rhabdomyosarcoma in a five-year-old boy with rapid-onset unilateral proptosis.
Case presentation
A five-year-old boy presented with rapid-onset proptosis and inferior displacement of the left globe for two weeks with associated with pain and discharge. There is history of the same condition in contralateral eyes that spontaneously heal without any treatment. It was previously treated with intravenous antibiotic for three days without any improvement. There was no history of trauma, upper respiratory tract infection, sinusitis or immunosuppression. The vital signs were within normal limit. The left eye showed proptosis, periorbital edema, chemosis in all quadrants of the conjunctiva and severe exposure keratopathy (Figure 1). The swelling was tender and soft in consistency. Proptosis and displacement of the left globe to inferior were present. There was limitation of all movement of the globe. Examination of right eye was within normal limit. Based on history and clinical examination, clinical diagnosis of rhabdomyosarcoma was made with orbital cellulitis as differential diagnosis.
 |
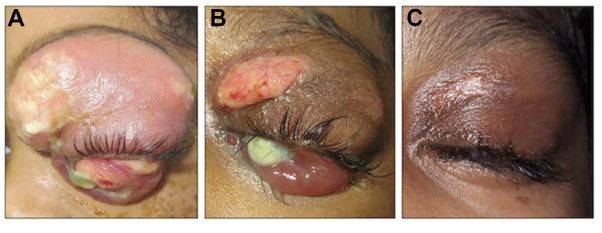
Figure 1 Baseline clinical presentation of left eye shows uniaxial proptosis with marked palpebral edema and conjunctival chemosis. Note the corneal ulcers. |
A multislice computed tomography (MSCT) scan showed lesions involving the lateral orbit (Figure 2A) and the retro bulbar space (Figure 2B). Complete blood count showed leukocytosis with signs of infection. Systemic screening results for metastasis were negative. Consultation with ear, nose and throat (ENT) specialist confirm no clinical and radiological signs of sinusitis. A dental consultation also showed no odontogenic infection. Community acquired pneumonia (CAP) was confirmed by a pediatrician from clinical and thorax radiologic findings. A biopsy was not performed due to suboptimal condition for anesthetic procedure.
On three days' administration of broad-spectrum cephalosporin antibiotic 750 mg twice a day, there is slight improvement of the patient's condition (Figure 3A). Patient shows resolution of clinical presentation after an additional intravenous administration of anti-inflammatory dexamethasone 5 mg twice a day for three days (Figure 3B). The patient made a good response after additional intravenous administration of broad-spectrum aminoglycoside antibiotic 40 mg twice a day for one week (Figure 3C). Simultaneously with intravenous therapy, an alpha receptor antagonist sympathomimetic and antibiotic were given topically to prevent further damage to the anterior segment of eyeball. After three weeks' therapy, the globe recovered, proptosis and displacement disappeared and ocular motility became normal. The visual prognosis was poor but with topical treatment, the ocular surface began to show better results. The patient’s legal guardian signed the written informed consent for publication of the case details and accompanying images. Institutional approval was not necessary.
Discussion and conclusion
Proptosis is an anterior displacement of the globes due to a space-occupying lesion in the orbit.10 The causes in children were different from adults. Orbital cellulitis is known to be the most common cause of proptosis among children.11 Other causes of proptosis in children include: developmental, vascular malformations, inflammations, and neoplasms.12 Even though orbital cellulitis is the most common cause, childhood proptosis needs special attention as it is commonly caused by malignant lesion and at least threatens vision. In children presenting with acute rapid-onset unilateral proptosis with signs of inflammation, the possibility of rhabdomyosarcoma should always beconsider.
Rhabdomyosarcoma is the most common primary orbital malignancies in children. The onset is five to seven years. The classic clinical picture is sudden onset and rapid progression of unilateral proptosis with inferior or inferior temporal displacement of the globe.13 Moreover, early signs and symptoms of orbital cellulitis include fever, lethargy, headache, rhinorrhea, eyelid edema, orbital pain and tenderness on palpation. Proptosis, chemosis and limited ocular movement suggest orbital involvement.14
Acute, rapidly progressive proptosis that presents in this case, raises a high suspicion of orbital rhabdomyosarcoma; notwithstanding, associated pain does not eliminate orbital cellulitis as a differential diagnosis. Based on complete blood count, leukocytosis with signs of infection occured. It is known that sinusitis is the most common cause of bacterial cellulitis, consequently once it is suspected, orbital imaging is indicated to confirm orbital involvement, to document the presence and extent of sinusitis and subperiosteal abscess and also to rule out a foreign body in the patient with a history of trauma.14 Some examinations should be done to rule out causes of infection, such as nasopharyngeal, conjunctival and blood culture. These procedures were not performed in this case considering the history of intravenous antibiotic. Accordingly, the result must be masked. The typical pathogens associated with acute sinusitis, including Streptococcus pneumoniae, Streptococcus pyogenes, Staphylococcus aureus, Haemophilus influenza, Moraxella catarrhalis, and nonhemolytic streptococci (including the Streptococcus milleri group) were common causes of orbital cellulitis.5 Etiology varies with age, in children younger than nine years old it is generally caused by single aerobic pathogen. In older children and adults, S. pneumoniae, S. pyogenes, S. aureus, and various anaerobic species are common. Gram-negative organisms are found primarily in immunosuppressed patients.14
A study by Ferguson and McNabb shows that in 56% of their patients that had blood cultures none had positive results. Based on their study, positive results more likely come from cultures taken from abscesses. They also noted that there was no correlation between etiology of orbital abscesses and cultures from conjunctiva.15
MSCT scan imaging shows a well-defined, irregular, homogenous lesion in the left supero-temporal orbit and the retro bulbar space. Consultation with an ENT specialist confirmed no clinical and imaging signs of sinusitis. These findings lead to high possibilities of rhabdomyosarcoma. In CT scan, orbital RMS appears as a well-defined, homogenous, soft tissue mass that is isodense to muscles without bone destruction in earlier stages, but in advanced cases with bone destruction, there is invasion of surrounding structures and calcification. Focal hemorrhage or necrosis could give a heterogeneous appearance and moderate to marked general enhancement with contrast.16
A consultation with a pediatrician was made before planning a biopsy. Pediatrician revealed an inadequate condition for anesthetic procedure due to CAP. Intravenous antibiotic of cephalosporin was administered. There is slight improvement after three days. The possibilities of orbital cellulitis reappeared. The most common cause of orbital cellulitis is bacterial infection. Bacterial infections of the orbit, originate from three primary sources: direct spread from adjacent sinusitis, dacryocystitis or dacryoadenitis, direct inoculation after trauma or skin infection, and hematologic spread from distant focus (eg, otitis media and pneumonia).17
Garcia and Harris, in their prospective study, established that patients younger than nine years of age with small, medial subperiosteal abscesses of nondental origin who did not have evidence of optic nerve compression, gas within the abscess space, frontal sinusitis, or chronic sinusitis were successfully managed with medical therapy alone.18
Adjuvant corticosteroid intravenously showed good response in one week for this case. The use of corticosteroid is still controversial in the treatment of orbital cellulitis. However, the use of systemic steroids under the coverage of appropriate antibiotics could decrease inflammatory response and does not have adverse effects. A prospective, randomized, comparative clinical study by Pushkar et al supports the beneficial effect of corticosteroids as an adjunct to antibiotics in acute bacterial orbital cellulitis. Addition of steroids helped in early resolution of inflammation and improved the overall outcome.19
In addition to routine antibiotic, gentamycin was used. Intravenous combination antibiotics showed good clinical resolution. Surgical intervention was not performed; not only because of patient's suboptimal condition for anesthetic procedures, but also because of antibiotic clinical response.
A study by Chang et al showed that the most therapeutic antibiotic regimens for orbital cellulitis were a combination of aminoglycosides and penicillin and/or cephalosporin.20 Bactericidal of these two antibiotic groups are different. Bacterial action of aminoglycosides is inhibition of protein biosynthesis, alternatively, penicillin and cephalosporin inhibit bacterial cell wall synthesis. Smith et al found that in patients older than nine years, proptosis, extra ocular movement (EOM) restriction, or elevated IOP at the time of presentation are significantly more likely to require surgical intervention during their hospitalization.21
Complications of orbital cellulitis were varied. Cavernous sinus thrombosis and intracranial extension may result in death. Other complications include corneal exposure with secondary ulcerative keratitis as shown in this case, as well as panopthalmitis. Secondary glaucoma, neurotrophic keratitis, septic uveitis or retinitis, infectious neuritis, inflammatory neuritis, optic nerve edema, exudative retinal detachment and central retinal artery occlusion could also happen.14
This case shows that an acute rapid-onset progressive proptosis may have special attention for diagnosis and management. Orbital cellulitis may mimic rhabdomyosarcoma in baseline clinical presentation. Antibiotic combinations of cephalosporin with aminoglycosides along with corticosteroid, show very good clinical resolution.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Jain A, Rubin PA. Orbital cellulitis in children. Int J Ophthalmol Clin. 2001;41(4):71–86. doi:10.1097/00004397-200110000-00009
2. Foster JA, Carter KD, Durairaj VD, et al. Section 07: orbit, eyelids and lacrimal system. In: Cantor LB, Rapuano CJ, Cioffi GA, editors. 2016–2017 Basic and Clinical Science Course. San fransisco: American Academy of Opthalmology; 2016:70–72.
3. Bergin DJ, Wright JE. Orbital cellulitis. Br J Ophthalmol. 1986;70(3):174–178. doi:10.1136/bjo.70.3.174
4. Chandler JR, Langenbrunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope. 1970;80(9):1414–1428. doi:10.1288/00005537-197009000-00007
5. Nageswaran S, Woods CR, Benjamin DK
6. Bajaj MS, Pushker N, Chaturvedi A, et al. Orbital space occupying lesion in Indian children. J Pediatr Ophthalmol Strabismus. 2007;44:106–111.
7. Boparai MS, Dash RG. Clinical, ultrasonographic and CT evaluation of orbital rhabdomyosarcoma with management. Indian J Ophthalmol. 1991;39:129–131.
8. Volpe NJ, Jacobeic FA. Paediatric orbital tumours.. Int Ophthalmol Clin. 1992;32:201–221.
9. McDonough RL, Leib ML. Atypical presentation of orbital rhabdomyosarcoma: a report of two cases. J Pediatric Ophthalmol Strabismus. 1995;32:262–265.
10. Ganessan K, Bakhshi S. Proptosis in children: approach. Indian J Med Pediatr Onc. 2004;25(Suppl 2):S33–S34.
11. Char DH. Tumors of the Eye and Ocular Adnexia. Hamilton: BC. Decker, Inc; 2001.
12. Rao AA, Naheedy JH, Chen JYY, Robbins SL, Ramkumar HL. A clinical update and radiologic review of pediatric orbital and ocular tumors. J Oncol. 2013;2013:1–22. doi:10.1155/2013/975908
13. Lueder GT, Archer SM, Hered RW, et al. Section 06: pediatric ophthalmology and strabismus. In: Cantor LB, Rapuano CJ, Cioffi GA, editors. 2016–2017 Basic and Clinical Science Course. San fransisco: American Academy of Ophthalmology; 2016:313–314.
14. Lueder GT, Archer SM, Hered RW, et al. Section 06: pediatric ophthalmology and strabismus. In: Cantor LB, Rapuano CJ, Cioffi GA, editors. 2016–2017 Basic and Clinical Science Course. San fransisco: American Academy of Ophthalmology; 2016:306–308.
15. Ferguson MP, McNabb AA. Current treatment and outcome in orbital cellulitis. Aust N Z J Ophthalmol. 1999;27(6):375–379.
16. Jurdy L, Merks JHM, Pieters BR, et al. Orbital rhabdomyosarcomas: a review. Saudi J Ophthalmol. 2013;27:167–175. doi:10.1016/j.sjopt.2013.06.004
17. Pelton RW, Klapper SR. Preseptal and Orbital Cellulitis. Focal Points: Clinical Modules for Ophthalmologists. San fransisco: American Academy of Opthalmoloy; 2008, module 11.
18. Garcia GH, Harris GJ. Criteria for nonsurgical management of subperiosteal abscess of the orbit: analysis of outcomes 1988–1998. Ophthalmology. 2000;107(8):1454–1456; discussion 1457–1458.
19. Pushkar N, Tejwani LK, Bajaj MS, Khurana S, Velpandian T, Chandra M. Role of oral corticosteroids in orbital cellulitis. Am J Ophthalmol. 2013;156:178–183. doi:10.1016/j.ajo.2013.01.031
20. Chang CH, Lai YH, Wang HZ, Su MY, Chang CW, Peng CF. Antibiotic treatment of orbital cellulitis: an analysis of pathogenic bacteria and bacterial susceptibility. J Ocul Pharmacol Ther. 2000;16(1):75–79. doi:10.1089/jop.2000.16.75
21. Smith JM, Bratton EM, DeWitt P, Davies BW, Hink EM, Durairaj VD. Predicting the need for surgical intervention in pediatric orbital cellulitis. Am J Ophthalmol. 2014;58(2):387–394. doi:10.1016/j.ajo.2014.04.022
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


