Back to Journals » Clinical Ophthalmology » Volume 14
Oculocardiac Reflex During ROP Exams
Authors Schumacher AC, Ball ML, Arnold AW , Grendahl RL, Winkle RK, Arnold RW
Received 21 October 2020
Accepted for publication 23 November 2020
Published 4 December 2020 Volume 2020:14 Pages 4263—4269
DOI https://doi.org/10.2147/OPTH.S288043
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Video abstract presented by Robert Arnold.
Views: 2542
August C Schumacher,1 Michelle L Ball,2 Andrew W Arnold,3 Robin L Grendahl,4 R Kevin Winkle,4 Robert W Arnold5
1US Ski Team, Alaska Winter Stars, Anchorage, AK, USA; 2Pediatric Department, Alaska Native Medical Center, Anchorage, AK, USA; 3College of Osteopathic Medicine, Pacific Northwest Universit, Yakima, WA, USA; 4Alaska Children’s EYE & Strabismus, Anchorage, AK, USA; 5Alaska Blind Child Discovery, Alaska Children’s EYE & Strabismus, Anchorage, AK, USA
Correspondence: Robert W Arnold
Alaska Blind Child Discovery, Alaska Children’s EYE & Strabismus, 3500 Latouche #280, Anchorage, AK 99508, 99508 Tel +1 907 561-1917
Fax +1 907 563-5373
Email [email protected]
Purpose: Reducing physiologic stress including bradycardia during staging eye exams for retinopathy of prematurity (ROP) is desirable. We observed heart rate change during routine retinopathy of prematurity eye examinations and compared the response with our ongoing study of oculocardiac reflex (OCR) elicited by uniform EOM tension during strabismus surgery.
Patients and Methods: Electrocardiograph was prospectively monitored during ROP exams featuring indirect ophthalmoscopy with Alfonso lid speculum and see-through scleral depressor without topical anesthesia. Clinical data were retrieved from ROP-Check software. OCR was defined as maximally changed heart rate (HR) as a percent of baseline. Strabismus surgery patients under general anesthesia served as controls.
Results: From 10/2017 to 9/2020, 281 infants had ROP exams, and the median OCR was 55.9% of baseline HR (IQR 41.4% to 72.6%), the kurtosis 0.93 and skewness 1.01 representing a drop from HR 169 ± 16 bpm to 102 ± 39 bpm. In comparison, 1493 adult and pediatric strabismus surgery patients had less OCR median bradycardia 87.8% (IQR 72– 98%), kurtosis 1.60 and skewness − 1.18. ROP %OCR correlated with birth gestational age (%OCR = 2.5 (GA) – 11, r(279)=0.33, p< 0.01) and with birthweight (%OCR = 0.02 (BW) + 38, r(279) =0.35, p< 0.01). The duration of bradycardia induced by ROP exam averaged 92 ± 34 seconds (range 34– 240 seconds).
Conclusion: Bradycardia is common during eye exams in the smallest premature infants with greater degree, more rapid onset and longer duration than OCR during strabismus surgery.
Keywords: bradycardia, retinopathy of prematurity, strabismus
Plain Language Summary
The heart rate change for premature infants during lid speculum, scleral depressed eye exams is more profound than oculocardiac reflex during strabismus surgery.
Introduction
The oculocardiac reflex (OCR) is typically a trigemino-vagal transient bradycardia elicited by manipulation of tissues of the eye and orbit.1 Though classically recognized during extraocular muscle (EOM) traction during strabismus or retinal surgery, OCR can accompany different types of eye surgery or eye examination.2
Retinopathy of Prematurity (ROP) Examination: OCR has been noted in premature infants.3 The heart rate change in 31% of infants can range from 10%-59% of baseline with various phases of the exam.4 In another study, three of 80 premature infants undergoing ROP cryotherapy had respiratory arrest and one had cardiac arrest.5 Healthy premature babies monitored all night, and then subjected to globe pressure had mean lowest HR corresponding to 1049 ± 540 ms with lowest HR (1894 ms R-R interval) being 32 bpm.6
Lid speculum with scleral depression affords far better assessment of peripheral retina than direct ophthalmoscope even with contact lens.7 Retinal digital contact photography may have longer duration, but also may be less stressful than indirect ophthalmoscopy in neonatal intensive care unit (NICU) infants.8 We observed heart rate change during routine retinopathy of prematurity and consult eye examinations in the NICU and compared the response with our ongoing study of OCR elicited by uniform EOM tension during strabismus surgery with general anesthesia.
Patients and Methods
The primary purpose of this study is to characterize the cardiac rhythm response to retinal exam with lid speculum and scleral depression during routine, scheduled staging exams for retinopathy of prematurity. Patients are dilated with cyclopentolate 0.2%, neosynephrine 1% one drop repeated twice at least 30 minutes before the examination with Alfonso lid speculum and Arnold See-Through scleral depressor (Storz sp7-38098).9 The infants are comforted by the child life specialist and, though supine, some, at the request of the nurse, are given a drop of stored, maternal breast milk, or concentrated sucrose solution,10 however, topical anesthetics are not used. The cardiac response is a type of oculocardiac reflex that is typically a bradycardia but sometimes no change or even a tachycardia. A secondary purpose of this study is to compare oculocardiac reflex during awake ROP exams with uniform oculocardiac reflex in children and adults during strabismus surgery under general anesthesia. In each strabismus case, the rectus muscle is gently hooked with a Jameson hook with a hole into which a small, sterile tension gauge is inserted to apply a uniform 200 gram, 10-second square-wave tension while observing the initial stable baseline heart rate and the maximally tension-altered heart rate. Examples of the cardiac rate changes during ROP exam can be viewed: https://youtu.be/_KO-qdhSMO8 and oculocardiac reflex during strabismus surgery: https://youtu.be/HtyMI7pqTvE.
This study of the oculocardiac reflex has been reviewed by the institutional review board of Providence Hospital and complies with the Declaration of Helsinki and the Health Insurance Portability and Accessibility Act (HIPAA). The study is prospective and observational concerning routine vital sign documentation during routine staging examinations for retinopathy of prematurity in the neonatal intensive care unit and the operating rooms. Since data were collected during routine ocular manipulation and routine monitoring, the requirement for written informed consent was waived. The study is registered: NCT04353960. De-identified data are available from http://www.abcd-vision.org/OCR/OCR%20ROP%20Strab%20De-Id.pdf
Electrocardiograph was monitored during routine staging examinations for retinopathy of prematurity. Stable baseline heart rate, maximally changed heart rate during the exam and duration of changed heart rate were recorded. No topical anesthetic drops were administered. Oculocardiac reflex was defined as the maximally changed heart rate as a percent of stable baseline heart rate: bradycardia ranged from 26% to 99%, tachycardia was greater than 100% up to 138%. For example, from a stable heart rate of 160 b.p.m, a 25% drop during scleral depressed eye exam to a low heart rate of 120 bpm would be classified as an OCR of 75%. Additional demographic and medical record data were retrieved from ROP Check software.11 The Providence NICU utilizes American Academy of Pediatrics (AAP) ROP scheduling guidelines.12
The smaller and least stable premature infants had additional nursing and respiratory therapy support during exams. Substantial bradycardia or apnea and desaturation prompted an interruption of scleral depression and/or exam with temporary removal of the Alfonso lid speculum.
Statistical Methods
The frequency distributions for heart rate change were tested for normality using kurtosis and skewness. Non-parametric analysis for two-sample comparison utilized the Mann–Whitney test and multiple comparison groups the Kruskal–Wallis test. Paired continuous data were analyzed with linear regression with Pearson Product Moment. A p of less than 0.05 was considered significant.
Given the mean 83% and standard deviation 20% for oculocardiac reflex during strabismus surgery in children and adults, the sample size needed to detect a 5% difference in means with alpha 0.05 and power 0.80 would be 252.
Results
Trigeminovagal reflexes were monitored for two groups of patients undergoing different forms of ocular manipulation. From October 2017 through September 2020, 281 infants and 691 exams were recorded. One hundred and seven infants had only one exam recorded while 174 had between 2 and 10 serial exams recorded. From September 1992 through September 2020, 1493 pediatric and adult strabismus surgery patients had oculocardiac reflex monitored as elicited by a 200 gram, 10-second, square-wave tension on a gently isolated extraocular rectus muscle with no anticholinergic or opioid medications. The impact on heart rate for premature infants undergoing ROP exam, separated by age, multiparity and whether ROP-treated plus strabismus surgical patients separated by age groups are presented in Table 1.
The duration of OCR induced by scleral depressed indirect ophthalmoscopy of both eyes was 92±34 seconds ranging from 15 seconds to 240 seconds. The proportion brief (<20 seconds to recover) was 38%, moderate 20–60 second duration was 40% and prolonged over one 60 seconds was 22%.
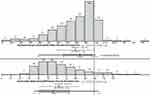
The median heart rate change during ROP exams of 55.9% (interquartile range IQR 41.4 to 72.6%) represented more bradycardia than strabismus surgical OCR 87.8% (IQR 72.0% to 98.0%; Mann–Whitney z=21, p<0.01, Table 1). The distribution of heart rate change in infants during lid-speculum, scleral depressed exams and of general anesthesia extraocular muscle controlled tension differ substantially (Figure 1). For ROP exam oculocardiac reflex, kurtosis was 0.93 and skewness 1.01 (n=691) while for strabismus surgical oculocardiac reflex kurtosis was 1.60 and skewness −1.18 (n=1493). During ROP exams, 64% had rapid onset bradycardia dropping at least 20% within the first two seconds while 36% had gradual onset. During strabismus surgery, 17% had rapid onset while 83% had gradual onset. Less than 10% of exams required interruption of lid speculum scleral depression due to temporary oxygen desaturation and prolonged bradycardia.
Using a definition of bradycardia as HR less than 100 bpm for >15 seconds, and tachycardia as HR 200 bpm or more for >15 seconds,13 during ROP scleral depressed exams, 57.3% of our patients had “bradycardia” and 2.2% had tachycardia.
Influences on oculocardiac reflex during ROP exams by parametric statistics and regressions are shown in Table 2. OCR during initial ROP exam correlated with birthweight (%OCR = 0.02 (BW) + 38, r(279) =0.35, p<0.01, Figure 2) and also correlated with birth gestational age (%OCR = 2.5 (GA) – 11, r(279)=0.33, p<0.01, Figure 3). Worse stages of ROP were related to more bradycardia during exams (Kruskal–Wallis X2 (2) = 15.6, p<0.01) however whether or not the infant reached threshold for ROP treatment did not influence OCR (Mann–Whitney z = 1.4, p=0.16). Twin and triplet infants were not more likely to have OCR (Mann–Whitney z = 1.3, p=0.20).
Discussion
The heart rate change induced by scleral-depressed, lid speculum ophthalmic exam in premature infants is of greater bradycardia, more rapid onset and more prolonged duration than the type of oculocardiac reflex elicited by 10-seconds moderate tension on and extraocular rectus muscle. The bradycardia during ROP exams was greater with lower birthweights and younger gestational ages. Propensity toward OCR during prior examinations was not predictive of progression to threshold for ROP treatment.
Reducing physical stress during ROP exam is warranted.14 Cardiac monitoring is helpful for inpatient retinal exams and should be considered in premature infants during outpatient examinations or during ROP treatment. Some clinicians advocate topical anesthesia and close monitoring during exams.15 Others find breast milk, sucrose and/or local anesthetic insufficient to curb the heart rate change (tachycardia) associated with lid speculum NICU eye exams.16 We recognize that topical anesthetics can quickly numb the cornea which is not touched during our exams, but that the deep pressure of lid speculum and scleral depression are not blunted by a topical anesthetic drop just before the exam. We also have documented that topical anesthetic do not enhance recovery from strabismus surgery, but maybe actually worsen recovery in young patients.17 Not every effort to reduce exam pain is benign.13 Ongoing close monitoring is also indicated due to an increased frequency of cardiorespiratory events in the hours after the exam.18 Infants receiving supplemental oxygen may be at particular risk of cardiac disturbance during exams.19 Heart rate variability as an indicator of autonomic nervous system function may be an independent risk factor for Type 1 ROP.20
General anesthesia utilized with strabismus surgery is a substantial difference when compared to awake ROP Exams. Oculocardiac reflex has been documented in awake strabismus patients, also.21 Certain substances can augment oculocardiac reflex during strabismus surgery such as fast-acting opioids22,23 and dexmedetomidine.24 For this reason, we excluded cases treated with those and with anticholinergics for our comparison group. Additional care should be considered for infants undergoing inpatient or outpatient retinal exams and/or retinopathy of prematurity treatment when opioids or this alpha-2 adrenergic agonist sedative have been administered.
Abbreviations
AAP, American Academy of Pediatrics; BW, birth weight; b.p.m., beats per minute; EOM, extraocular muscle; GA, gestational age; HIPAA, Health Insurance Portability and Accessibility; NICU, neonatal intensive care unit; OCR, oculocardiac reflex; ROP, retinopathy of prematurity.
Data Sharing Statement
Data Access: http://www.abcd-vision.org/OCR/OCR%20ROP%20Strab%20De-Id.pdf.
Trial Registration
Clinical Trials Registry: NCT04353960.
Disclosure
Dr. Robert Arnold is President and board member of Glacier Medical Software that markets cloud-based NICU monitoring software ROP Check. He is also President and board member of PDI Check that markets autostereoscopic vision screening games for Nintendo 3DS. He coordinates the Alaska Blind Child Discovery that has received discounted vision screen technology from several vendors. He is the inventor of the Storz Arnold See-Through Scleral Depressor (sp7-38098) but receives no royalties and was an investigator and protocol developer for Pediatric Eye Disease Investigator Group, during the conduct of the study; and non-paid advisory board for GoCheck Kids, Adaptica and PlusoptiX, outside the submitted work; in addition, Dr Robert W Arnold has a patent pending for PDI Check to Robert Arnold and Alex Damarjian. The authors report no other potential conflicts of interest for this work.
References
1. Dunville LM, Sood G, Kramer J. Oculocardiac Reflex. StatPearls Web site. 2020. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29763007.
2. Ha SG, Huh J, Lee BR, Kim SH. Surgical factors affecting oculocardiac reflex during strabismus surgery. BMC Ophthalmol. 2018;18(1):103. doi:10.1186/s12886-018-0771-9
3. Javorka K, Zavarska L. [Oculocardiac reflex in premature infants]. Cesk Pediatr. 1978;33(3):138–140.
4. Clarke WN, Hodges E, Noel LP, Roberts D, Coneys M. The oculocardiac reflex during ophthalmoscopy in premature infants. Am J Ophthalmol. 1985;99(6):649–651. doi:10.1016/S0002-9394(14)76029-5
5. Brown GC, Tasman WS, Naidoff M, Schaffer DB, Quinn G, Bhutani VK. Systemic complications associated with retinal cryoablation for retinopathy of prematurity. Ophthalmology. 1990;97(7):855–858. doi:10.1016/S0161-6420(90)32491-0
6. de Montgolfier-aubron I, de Broca A, Kabeya B, Lego-Popesco S, Chavet MS, Gold F. [Standardized oculocardiac reflex in ex-premature near full term (93 cases)]. Arch Pediatr. 2002;9(5):456–462. doi:10.1016/S0929-693X(01)00826-0.French.
7. Dhillon B, Wright E, Fleck BW. Screening for retinopathy of prematurity: are a lid speculum and scleral indentation necessary? J Pediatr Ophthalmol Strabismus. 1993;30(6):377–381.
8. Prakalapakorn SG, Stinnett SS, Freedman SF, Wallace DK, Riggins JW, Gallaher KJ. Non-contact retinal imaging compared to indirect ophthalmoscopy for retinopathy of prematurity screening: infant safety profile. J Perinatol. 2018;38(9):1266–1269. doi:10.1038/s41372-018-0160-5
9. Arnold RW. Posterior retinopathy of prematurity cryotherapy from a limbal reference. J Pediatr Ophthalmol Strabismus. 1994;31:303–305.
10. Slater R, Cornelissen L, Fabrizi L, et al. Oral sucrose as an analgesic drug for procedural pain in newborn infants: a randomised controlled trial. Lancet. 2010;376(9748):1225–1232. doi:10.1016/S0140-6736(10)61303-7
11. Arnold RW, Jacob J, Matrix Z. Toward achieving 100% adherence for retinopathy of prematurity screening guidelines. J Pediatr Ophthalmol Strabismus. 2017;54(6):356–362.
12. Fierson WM, American Academy Of Ophthalmology, American Association For Pediatric Ophthalmology & Strabismus, American Association Of Certified Orthoptists. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2018;142:6.
13. Hartley C, Moultrie F, Hoskin A, et al. Analgesic efficacy and safety of morphine in the Procedural Pain in Premature Infants (Poppi) study: randomised placebo-controlled trial. Lancet. 2018;392(10164):2595–2605. doi:10.1016/S0140-6736(18)31813-0
14. Szigiato AA, Speckert M, Zielonka J, et al. Effect of eye masks on neonatal stress following dilated retinal examination: the MASK-ROP randomized clinical trial. JAMA Ophthalmol. 2019;137(11):1265. doi:10.1001/jamaophthalmol.2019.3379
15. Rush R, Rush S, Nicolau J, Chapman K, Naqvi M. Systemic manifestations in response to mydriasis and physical examination during screening for retinopathy of prematurity. Retina. 2004;24(2):242–245. doi:10.1097/00006982-200404000-00009
16. Turan O, Akkoyun I, Ince DA, Doganay B, Tugcu AU, Ecevit A. Effect of breast milk and sucrose on pain and perfusion index during examination for retinopathy of prematurity. J Matern Fetal Neonatal Med. 2019;1–5.
17. Arnold RW, Bond AN. Does topical proparacaine improve postoperative comfort after strabismus surgery? Clin Ophthalmol. 2019;13:2279–2283. doi:10.2147/OPTH.S230498
18. Reid B, Wang H, Guillet R. Apnea after routine eye examinations in premature infants. Am J Perinatol. 2017;34(2):199–203. doi:10.1055/s-0036-1585412
19. Tan JBC, Dunbar J, Hopper A, Wilson CG, Angeles DM. Differential effects of the retinopathy of prematurity exam on the physiology of premature infants. J Perinatol. 2019;39(5):708–716. doi:10.1038/s41372-019-0331-z
20. Hussein MA, Deng N, Rusin C, Paysse EE, Bhatt A, Coats DK. Heart rate variability changes and its association with the development of severe retinopathy of prematurity. J AAPOS. 2018;22(5):371–375. doi:10.1016/j.jaapos.2018.03.015
21. Arnold RW, Ellis FD, Wolfe TM. Prolonged oculocardiac reflex during strabismus surgery under topical anesthesia. J Pediatr Ophthalmol Strabismus. 1997;34(4):252–254.
22. Chung CJ, Lee JM, Choi SR, Lee SC, Lee JH. Effect of remifentanil on oculocardiac reflex in paediatric strabismus surgery. Acta Anaesthesiol Scand. 2008;52(9):1273–1277. doi:10.1111/j.1399-6576.2008.01745.x
23. Arnold RW, Jensen P, Kovtoun TA, Maurer SA, Schultz J-A. The profound augmentation of the oculocardiac reflex by fast-acting opioids. Binoc Vis Strabismus Quart. 2004;19(4):215–222.
24. Arnold RW, Biggs RE, Beerle BJ. Intravenous dexmedetomidine augments the oculocardiac reflex. J AAPOS. 2018;22(3):211–213.e211. doi:10.1016/j.jaapos.2018.01.016
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.