Back to Journals » Clinical Ophthalmology » Volume 16
OC-01 (Varenicline Solution) Nasal Spray Demonstrates Consistency of Effect Regardless of Age, Race, Ethnicity, and Artificial Tear Use
Authors Epitropoulos AT , Daya SM , Matossian C , Kabat AG , Blemker G, Striffler K, Hendrix L, Macsai M, Gibson A
Received 28 July 2022
Accepted for publication 6 October 2022
Published 13 October 2022 Volume 2022:16 Pages 3405—3413
DOI https://doi.org/10.2147/OPTH.S383091
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Alice T Epitropoulos,1,2 Sheraz M Daya,3 Cynthia Matossian,4 Alan G Kabat,5,6 Gretchen Blemker,5 Kristen Striffler,5 Laura Hendrix,5 Marian Macsai,5 Andrea Gibson5
1Ophthalmic Surgeons & Consultants of Ohio, the Eye Center of Columbus, Columbus, OH, USA; 2Department of Ophthalmology, the Ohio State University Wexner Medical Center, Columbus, OH, USA; 3Centre for Sight, London, UK; 4Matossian Eye Associates, Pennington, NJ, USA; 5Oyster Point Pharma, Inc, Princeton, NJ, USA; 6Salus University, Elkins Park, PA, USA
Correspondence: Andrea Gibson, Oyster Point Pharma, Inc, 202 Carnegie Center, Suite 109, Princeton, NJ, 08540, USA, Tel +1-860-227-1034, Fax +1-856-433-8439, Email [email protected]
Purpose: To evaluate OC-01 [varenicline solution nasal spray (VNS)] tear production and symptom outcomes in patients with dry eye disease by age, gender, race, ethnicity, and artificial tear use status.
Patients and Methods: Adults ≥ 22 years of age diagnosed with dry eye disease, with Ocular Surface Disease Index score ≥ 23, corneal fluorescein staining score ≥ 2 in ≥ 1 region or ≥ 4 for all regions, and baseline Schirmer Test Score (STS) ≤ 10 mm, with no restrictions on eye dryness score (EDS). Efficacy was assessed using integrated data from ONSET-1 and ONSET-2 [vehicle control (VC), n=294; OC-01 VNS 0.03 mg, n=308]. Subgroups included age (≤ 55, 56− 65, > 65 years), gender (male, female), race (White, Black or African American), ethnicity (Hispanic or Latino, Not Hispanic or Latino), and artificial tear use (yes, no). Analysis of covariance models, with the covariates treatment, study site, and baseline severity measures, were used to calculate treatment−VC differences. Consistency of effect among subgroups was evaluated by conducting interaction tests.
Results: Consistency of treatment effect across subgroups was observed for all endpoints, with P value for all treatment−subgroup interaction terms > 0.05. For % of patients with ≥ 10mm improvement in STS and least squares (LS) mean change from baseline in STS and EDS, there was improvement in tear production across demographic group categories. Artificial tear use did not change STS or EDS outcomes with OC-01 VNS.
Conclusion: OC-01 VNS improved tear production and patient-reported symptom outcomes across a broad range of patients by age, gender, race, and ethnicity, and regardless of artificial tear use status at baseline. OC-01 VNS demonstrated a consistent benefit across an extensive range of patients with dry eye disease.
Keywords: bioactivation, dry eye disease, nicotinic acetylcholine receptor, tear production, varenicline nasal spray
Introduction
Dry eye disease is a multifactorial disease of the ocular surface and tear film that affects tens of millions of people worldwide.1 The prevalence of dry eye disease is growing, and is known to vary across several demographic subgroups.2 For example, dry eye disease is more prevalent in older individuals, with an approximate 2% to 11% increase per decade;2,3 women are disproportionately affected more than men,2–4 with significantly higher rates of disease in older women;2 and Asian populations frequently report higher rates of dry eye disease than Caucasian populations because Asian race is a significant risk factor for the disease.2 Despite these observed demographic differences, there is a universal need for more efficacious treatments for dry eye disease.
Maintenance of the natural tear film is critical to ocular surface homeostasis,5–7 and tear film instability is a key feature of dry eye disease.1,7 The most common first-line therapy for dry eye disease is over-the-counter artificial tear eye drops, which are intended to supplement insufficient tear production and potentially help protect the ocular surface.8 At least 60 million people worldwide use artificial tears to treat dry eye symptoms;8 however, artificial tears provide only temporary relief9 and may exacerbate the condition by washing away natural tears on the ocular surface or causing irritation from preservatives. Further, artificial tears do not contain the complex biologically active, endogenously expressed components of natural tears, such as lipids, mucins, and proteins,10 which contribute not only to producing high-quality vision, but also support protection from infection, suppression of inflammation, and healing of injuries.11
OC-01 (varenicline solution) nasal spray (TYRVAYA® [varenicline solution] 0.03 mg; Oyster Point Pharma, Inc., Princeton, NJ),12 is a recently approved treatment for the signs and symptoms of dry eye disease that stimulates basal tear production. The active component of OC-01 nasal spray, varenicline, is believed to bind to nicotinic acetylcholine receptors on the terminal branches of the trigeminal nerve in the nasal cavity,13,14 thereby activating the lacrimal functional unit to produce endogenous tears in all their complexity via efferent parasympathetic innervation.15,16
Approval for OC-01 (varenicline solution) nasal spray was based on evidence from pivotal clinical trials, including the ONSET-117 and ONSET-218 trials. These randomized, prospective, vehicle-controlled trials investigated the efficacy and safety of OC-01 (varenicline solution) nasal spray in over 600 patients with dry eye disease. However, it is important to understand the response to OC-01 (varenicline solution) nasal spray based on various baseline demographic factors and whether concomitant use or absence of artificial tears during therapy affects treatment outcomes. To assess any possible heterogeneity in treatment response in different populations of patients with dry eye disease, we evaluated integrated data from the ONSET-1 and ONSET-2 trials by baseline demographic subgroups of age, gender, race, and ethnicity and by patients using and not using artificial tears.
Materials and Methods
Study Designs
Data for this planned post hoc integrated analysis were obtained from 2 randomized clinical trials, ONSET-1 (ClinicalTrials.gov, NCT03636061)17 and ONSET-2 (ClinicalTrials.gov, NCT04036292).18 For both studies, institutional review board (Alpha IRB, San Clemente, CA) approval was obtained and the study was conducted in compliance with the ethical principles of the Declaration of Helsinki and International Council for Harmonisation Good Clinical Practice. All patients provided written informed consent before participation.
Methods and safety and efficacy results have been previously reported.17,18 Briefly, the ONSET-1 (Phase 2b) and ONSET-2 (Phase 3) trials were both 4-week, multicenter, randomized, prospective, vehicle-controlled trials in adults within the United States to evaluate the efficacy and safety of OC-01 (varenicline solution) nasal spray. Patients were eligible if they had a physician’s diagnosis of dry eye disease; an Ocular Surface Disease Index score of at least 23, with up to 3 responses of “Not Applicable”; a corneal fluorescein staining score of at least 2 in at least 1 corneal region or at least 4 for all corneal regions; a baseline, anesthetized Schirmer Test Score (STS) of 10 mm/5 min or lower; and an anesthetized STS at least 7 mm greater in the same eye after mechanical nasal stimulation with a cotton swab. The study eye was defined as the eye that met all inclusion criteria. Eligibility was not restricted by Eye Dryness Score (EDS).
Statistical Analysis
Efficacy assessments were conducted on integrated data from the ONSET-1 and ONSET-2 trials comparing vehicle control and OC-01 (varenicline solution) nasal spray 0.03 mg, administered twice daily. Planned post hoc analyses of prespecified baseline demographics and concomitant artificial tear use evaluated the following endpoints: (1) the percentage of patients who achieved an at least 10-mm improvement in the study eye in anesthetized STS from baseline to week 4, (2) the mean change in STS from baseline to week 4, and (3) the mean change in patient-reported EDS from baseline to week 4. Categories for baseline demographics and concomitant artificial tear use included the following subgroups: age (≤55, 56–65, >65 years), gender (male, female), race (White, Black or African American, Asian or Native Hawaiian or Other Pacific Islander, American Indian or Alaskan Native or Other); ethnicity (Hispanic or Latino, Not Hispanic or Latino); and artificial tear use (yes, no). Summary statistics and analysis included observed measurements and a last-observation-carried-forward approach for missing data.
The differences in the means in the study eye in vehicle control and OC-01 (varenicline solution) nasal spray were analyzed using an analysis of covariance model, with treatment, site, baseline STS, and baseline EDS as covariates. Data were presented as least squares (LS) mean changes with 95% confidence intervals (CIs). Consistency of effect within subgroups was evaluated by including treatment–subgroup interaction terms in models and tests. Interaction was considered statistically significant at a P value of 0.05. For purposes of interpretation, subsequent use of the term “no interaction” may be defined as follows: no statistically significant (p>0.05) difference in the treatment effect, ie, OC-01 (varenicline solution) nasal spray 0.03 mg treatment outcome minus vehicle control outcome, between the respective subgroups (eg, males vs females, White vs Black or African American subjects, use of artificial tears vs non-use of artificial tears at baseline). Exploratory post hoc subgroup analyses are not evaluated for statistical significance testing.
Results
Demographic and Baseline Clinical Characteristics
A total of 602 patients were included in the integrated population for efficacy assessments; 294 were assigned to vehicle control and 308 were assigned to OC-01 (varenicline solution) nasal spray 0.03 mg (Table 1). Overall, the treatment groups were generally balanced for all demographic categories. Mean age was 59 to 61 years; most patients were female (>76%), White (>84%), and not Hispanic or Latino (>88%); and most patients did not use artificial tears (>74%).
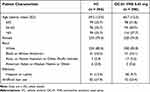 |
Table 1 Baseline Demographic Characteristics and Artificial Tear Use |
Improvements in Schirmer Test Score After OC-01 (Varenicline Solution) Nasal Spray Administration
There were no statistically significant treatment–subgroup interactions for any of the baseline demographic groups (all P > 0.05) and therefore, consistency of treatment effect was demonstrated for all endpoints assessed across all analyzed subgroups.
Improvements in tear production were demonstrated for OC-01 (varenicline solution) nasal spray versus vehicle in most demographic categories. The odds of achieving at least 10-mm improvement in STS for OC-01 (varenicline solution) nasal spray versus vehicle control for age categories ≤55, 56–65, and >65 years were 2.3 (95% CI, 1.1–4.4), 2.9 (1.3–6.5), and 5.5 (2.3–13.2), respectively (Figure 1A); for males and females were 2.3 (0.9–6.3) and 3.5 (2.2–5.5), respectively (Figure 1B); for the White and Black or African American groups were 3.3 (2.2–5.0) and 0.6 (0.1–2.5), respectively (odds ratios for the other race groups could not be calculated because of low patient numbers) (Figure 1C); and for the Hispanic or Latino and not Hispanic or Latino groups were 3.9 (1.0–16.0) and 3.1 (92.0–4.6), respectively (Figure 1D). The LS mean change from baseline in STS for OC-1 (varenicline solution) nasal spray versus vehicle control for age categories ≤55, 56–65, and >65 years was 5.9 mm (95% CI, 3.1–8.8), 6.3 mm (3.7–9.0), and 5.7 mm (3.4–8.1), respectively; for males and females was 3.6 mm (0.3–7.0) and 6.3 mm (4.6–8.0), respectively; for the White, Black or African American, and Asian groups was 5.7 mm (4.1–7.2), 3.4 mm (–2.2 to 8.9), and 5.3 mm (–9.1 to 19.6), respectively (odds ratios for American Indians could not be calculated because of low patient numbers); and for the Hispanic or Latino and not Hispanic or Latino groups was 7.2 mm (2.5–11.9) and 5.7 mm (4.1–7.2), respectively (Figure 2).
The increase in tear production favored OC-01 (varenicline solution) nasal spray over vehicle control, regardless of artificial tear use status at baseline. The odds of achieving at least 10-mm improvement in STS for OC-01 (varenicline solution) nasal spray versus vehicle control for artificial tear users and nonusers were 2.5 (95% CI, 1.0–6.3) and 3.2 (2.0–5.0), respectively (Figure 1E). The LS mean change from baseline in STS for OC-1 (varenicline solution) nasal spray versus vehicle control for artificial tear users and nonusers was 3.7 mm (95% CI, 0.5–6.9) and 6.0 mm (4.3–7.7), respectively (Figure 2).
Improvements in Eye Dryness Score After OC-01 (Varenicline Solution) Nasal Spray Administration
Improvements in LS mean change from baseline in EDS were also shown across all subgroups. The LS mean change from baseline in EDS for OC-1 (varenicline solution) nasal spray versus vehicle control for age categories ≤55, 56–65, and >65 years was –7.0 (95% CI, –13.9 to –0.2), –6.4 (–13.6 to 0.8), and –4.4 (–10.7 to 1.9), respectively; for males and females was –5.4 (–14.5 to 3.7) and –6.3 (–10.7 to –2.0), respectively; for the White, Black or African American, and Asian groups was –5.4 (–9.6 to –1.3), –10.5 (–23.6 to 2.6), and –11.9 (–53.7 to 29.9), respectively (odds ratios for American Indians could not be calculated because of low patient numbers); and for the Hispanic or Latino and not Hispanic or Latino groups was –4.9 (–17.5 to 7.7) and –6.1 (–10.2 to –2.1), respectively (Figure 3).
The decrease in EDS favored OC-01 VNS over VC, regardless of artificial tear use at baseline. The LS mean change from baseline in EDS for OC-1 (varenicline solution) nasal spray versus vehicle control for artificial tear users and nonusers was –6.5 (95% CI, –14.0 to 1.0) and –6.1 (–10.7 to –1.6), respectively (Figure 3).
Discussion
Dry eye disease is more prevalent in women and older patients2,3 and assessing treatment outcomes in these and other demographic subgroups in clinical trials is important for real-world applicability of new therapeutic modalities. In this planned post hoc integrated analysis, OC-01 (varenicline solution) nasal spray improved the signs and symptoms of dry eye disease, by assessment of tear production with STS and assessment of patient-reported symptoms via EDS, across a broad range of patients by age, gender, race, and ethnicity. Unfortunately, based on the location of the investigational centres, a low number of Asian and Native American patients enrolled in the studies, limiting assessment in these populations (future studies are being planned in China that will provide additional information in the Asian population). Further, OC-01 (varenicline solution) nasal spray was efficacious, regardless of artificial tear use status at baseline, which is important given the real-world use of artificial tears by patients, as a monotherapy or in conjunction with other treatments, for the management of dry eye disease. Safety findings for the current integrated analyses were consistent with the previously reported primary studies17,18 and were unremarkable, with very few differences among the subgroups (data not shown). Overall, we followed the appropriate methodology to explore the consistency of effect (interaction testing) across post hoc subgroups from our clinical trials19 and our analysis results further support OC-01 (varenicline solution) nasal spray is an effective and well-tolerated treatment across many different patients with dry eye disease.
Thorough assessments of available treatments for dry eye disease by demographic subgroups are lacking in the literature. For example, Farrand et al (2017)3 reported that patients with dry eye disease noted use of treatments, including artificial tears, ophthalmic cyclosporine, topical steroids, topical allergy medications, and topical antibiotics, but did not classify treatments by patient group. Interestingly, although the prescribing information for the most common topical prescription medications, cyclosporine A and lifitegrast, suggests these drugs are effective in both younger and older patients,20,21 a recently published meta-analysis suggests that cyclosporine A may be more effective in a relatively older population.22 Given the multifactorial and heterogenous nature of dry eye disease, there is a need to better characterize whether a treatment response to therapy is assessed across specific groups of patients and determine if the data demonstrate consistency of treatment effect outcomes across diverse patient subgroups.
Because artificial tears may be used by patients throughout their treatment journey with dry eye disease, it is important to assess any potential interaction with prescription medications. We found improvements in tear production and patient-reported symptoms with OC-01 (varenicline solution) nasal spray treatment, regardless of artificial tear use at baseline, but a limitation of our study is that artificial tear use was assessed at baseline only (patients reported as either yes or no) and any change in use throughout the study was not assessed. Although less than 26% of subjects in the present study utilized artificial tears at baseline, we do not have definitive reasons for such low use within this more “real world” study design that allowed subjects to utilize artificial tears if needed. It is possible the rapid onset of action with OC-01 (varenicline solution) nasal spray and subsequent tear production improvements were experienced by subjects and additional artificial tear therapy was not needed, or perhaps subjects were potentially motivated to evaluate their experience of the investigational therapy without confounding it with additional treatment. Future research in this may help elucidate greater insight into patient experiences and preferences. Our findings suggest that patients who already use artificial tears (who may potentially have more severe disease at baseline) may not need to interrupt treatment with artificial tears while using nasally administered OC-01 (varenicline solution) nasal spray. Other approved prescription pharmaceutical treatment options for dry eye disease that act via reducing associated inflammation have shown mixed results regarding concomitant artificial tear use. A recent systematic review and meta-analysis found that cyclosporine A had reduced treatment effects when combined with artificial tears,22 which suggests that there may be a potential washout effect. In addition, the prescribing information for cyclosporine A recommends use with artificial tears as long as there is at least 15 minutes between treatments,20 which may complicate patient treatment administration. In contrast, evidence supports the effectiveness of lifitegrast with concomitant artificial tear use in dry eye disease.23,24 Future prospective studies may address whether the increase in natural tears and important biologically active beneficial constituents within human tears in response to OC-01 (varenicline solution) nasal spray treatment are affected or potentially washed out by concomitant use of artificial tears.
Nasal spray administration to the anterior nasal mucosa may be an ideal mode of delivery to activate natural tear production for the treatment of dry eye disease. Mechanical stimulation of the anterior ethmoidal nerve in the nasal mucosa, even with the vehicle control spray, may momentarily stimulate the trigeminal parasympathetic pathway.25–27 and this was observed in the younger subgroups (ie, those aged 65 years or less) in this analysis. In the pivotal clinical trials, a significantly greater magnitude of tear production and symptomatic benefits were demonstrated with pharmacologic neuro-activation with OC-01 (varenicline solution) nasal spray compared to vehicle control,12,17,18 and by utilizing the same optimized nasal route of administration, OC-01 (varenicline solution) nasal spray may offer an efficacious and ocular surface “sparing” treatment option for patients.
This integrated analysis was limited by the constraints of post hoc analyses, the small sample size for some demographic subgroups, and post hoc analysis results should be interpreted with caution. Our analysis is strengthened by the inclusion of patients and a study design representative of treatment in the real world, and by the finding that there were no interactions between treatment and demographic groups, indicating consistency of effect of OC-01 (varenicline solution) nasal spray, regardless of age, gender, race, ethnicity, or baseline artificial tear use.
Conclusion
The findings from our integrated analysis support the benefits of OC-01 (varenicline solution) nasal spray, including a consistency of effect across a broad range of patients. OC-01 (varenicline solution) nasal spray improved the signs and symptoms of dry eye disease in patients over a range of demographic subgroups, and regardless of concomitant artificial tear use at baseline. Because clinician decision-making for the management of dry eye disease involves consideration of the heterogeneity of disease at clinical presentation, age and variable demographic backgrounds, and artificial tear use, these data may help better elucidate the benefits of OC-01 (varenicline solution) nasal spray treatment across an extensive range of presenting patients.
Data Sharing Statement
The data used to support the primary findings of this study are available at ClinicalTrials.gov (NCT03636061 and NCT04036292).
Ethics Approval and Informed Consent
This study was conducted in accordance with the principles of Declaration of Helsinki and in compliance with the ICH E6 GCP Consolidated Guideline, ISO 14155:2011, and the applicable US FDA 21 CFR Regulations. Before clinical study initiation, the protocol and all amendments, the informed consent form, any other written information given to subjects, and any advertisements planned for subject recruitment was approved by an IRB/IEC (Alpha IRB, San Clemente, CA).
Acknowledgments
Statistical analysis assistance was provided by Eugenia Henry, PhD, and Kuei Hsun Chiu, MS, of Firma Clinical Research, and was funded by Oyster Point Pharma, Inc. Medical writing assistance was provided by Janelle Keys, PhD, CMPP, of Envision Pharma Group, and was funded by Oyster Point Pharma, Inc. Envision Pharma Group’s services complied with international guidelines for Good Publication Practice (GPP3).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was sponsored by Oyster Point Pharma, Inc., manufacturer/licensee of OC-01 (varenicline solution) nasal spray.
Disclosure
The authors report the following conflicts of interest:
A.T.E.: Advisor — Oyster Point Pharma, Inc.
S.M.D.: Advisor – Oyster Point Pharma, Inc
C.M.: Advisor – Oyster Point Pharma, Inc
G.B.: Employee, Shareholder — Oyster Point Pharma, Inc.
K.S.: Employee, Shareholder — Oyster Point Pharma, Inc.
L.H.: Employee, Shareholder — Oyster Point Pharma, Inc.
M.M.: Employee, Shareholder — Oyster Point Pharma, Inc.
A.G.: Employee, Shareholder — Oyster Point Pharma, Inc.
Dr A.G.K is an Employee and Shareholder for Oyster Point Pharma, Inc., during the conduct of the study; personal fees, non-financial support from MYCO Industries, personal fees from SUN Pharma, personal fees from Kala Pharmaceuticals, personal fees, non-financial support from Bruder Healthcare Company, personal fees from Thea Pharma US, personal fees, non-financial support from OCuSOFT, Inc., personal fees from Novartis, personal fees from Quidel, personal fees, non-financial support from Bio-Tissue, outside the submitted work.
Portions of these data were presented at the American Academy of Ophthalmology Annual Meeting; November 13 to 14, 2021; New Orleans, LA; and at the European Society of Cataract and Refractive Surgeons Annual Meeting; October 8, 2021; Amsterdam, the Netherlands.
References
1. Tsubota K, Pflugfelder SC, Liu Z., et al. Defining dry eye from a clinical perspective. Int J Mol Sci. 2020;21:9271. doi:10.3390/ijms21239271
2. Stapleton F, Alves M, Bunya VY, et al. TFOS DEWS II Epidemiology report. Ocul Surf. 2017;15:334–365. doi:10.1016/j.jtos.2017.05.003
3. Farrand KF, Fridman M, Stillman IO, Schaumberg DA. Prevalence of diagnosed dry eye disease in the United States among adults aged 18 years and older. Am J Ophthalmol. 2017;182:90–98. doi:10.1016/j.ajo.2017.06.033
4. Matossian C, McDonald M, Donaldson KE, et al. Dry eye disease: consideration for women’s health. J Womens Health. 2019;28:502–514. doi:10.1089/jwh.2018.7041
5. Dartt DA, Willcox MD. Complexity of the tear film: importance in homeostasis and dysfunction during disease. Exp Eye Res. 2013;117:1–3. doi:10.1016/j.exer.2013.10.008
6. Zhang X, Jeyalatha MV, Qu Y, et al. Dry eye management: targeting the ocular surface microenvironment. Int J Mol Sci. 2017;18:1398. doi:10.3390/ijms18071398
7. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II Definition and Classification report. Ocul Surf. 2017;15:276–283. doi:10.1016/j.jtos.2017.05.008
8. Kim M, Lee Y, Mehra D, et al. Dry eye: why artificial tears are not always the answer. BMJ Open Ophthalmol. 2021;6:e000697. doi:10.1136/bmjophth-2020-000697
9. Pucker AD, Ng SM, Nichols JJ. Over the counter (OTC) artificial tear drops for dry eye syndrome. Cochrane Database Syst Rev. 2016;2:CD009729. doi:10.1002/14651858.CD009729.pub2
10. Willcox MDP, Argüeso P, Georgiev GA, et al. TFOS DEWS II Tear Film report. Ocul Surf. 2017;15:366–403. doi:10.1016/j.jtos.2017.03.006
11. Pflugfelder SC, Stern ME. Biological functions of tear film. Exp Eye Res. 2020;197:108115. doi:10.1016/j.exer.2020.108115
12. Oyster Point Pharma, Inc. Tyrvaya [Package Insert]. Princeton, NJ: Oyster Point Pharma, Inc; 2021.
13. Alimohammadi H, Silver WL. Evidence for nicotinic acetylcholine receptors on nasal trigeminal nerve endings of the rat. Chem Senses. 2000;25:61–66. doi:10.1093/chemse/25.1.61
14. Flores CM, DeCamp RM, Kilo S, et al. Neuronal nicotinic receptor expression in sensory neurons of the rat trigeminal ganglion: demonstration of α3β4, a novel subtype in the mammalian nervous system. J Neurosci. 1996;16(24):7892–7901. doi:10.1523/JNEUROSCI.16-24-07892.1996
15. Gumus K, Schuetzle KL, Pflugfelder SC. Randomized controlled crossover trial comparing the impact of sham or intranasal tear neurostimulation on conjunctival goblet cell degranulation. Am J Ophthalmol. 2017;177:159–168. doi:10.1016/j.ajo.2017.03.002
16. Dartt DA. Neural regulation of lacrimal gland secretory processes: relevance in dry eye diseases. Prog Retin Eye Res. 2009;28:155–177. doi:10.1016/j.preteyeres.2009.04.003
17. Wirta D, Torkildsen GL, Boehmer B, et al. ONSET-1 phase 2b Randomized Trial to Evaluate the Safety and Efficacy of OC-01 (varenicline solution) Nasal Spray on Signs and Symptoms of Dry Eye Disease. Cornea. 2022;41(10):1207–1216. doi:10.1097/ICO.0000000000002941
18. Wirta D, Vollmer P, Paauw J, et al. ONSET-2 Study Group. Efficacy and safety of OC-01 (varenicline solution) nasal spray on signs and symptoms of dry eye disease: the ONSET-2 phase 3 randomized trial. Ophthalmology. 2022;129:379–387. doi:10.1016/j.ophtha.2021.11.004
19. Wang R, Lagakos SW, Ware JH, et al. Statistics in medicine—reporting of subgroup analyses in clinical trials. N Engl J Med. 2007;357(21):2189–2194. doi:10.1056/NEJMsr077003
20. Allergan. Restasis [Package Insert]. Irvine, CA: Allergan; 2017.
21. Novartis Pharmaceuticals Corporation. Xiidra [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2020.
22. Tuan H-I, Chi S-C, Kang Y-N. An updated systematic review with meta-analysis of randomized trials on topical cyclosporin A for dry-eye disease. Drug Des Devel Ther. 2020;14:265–274. doi:10.2147/DDDT.S207743
23. Atallah RT, Castanos MV, Najac R, Donnenfeld E. Six months’ treatment with lifitegrast in patients with moderate-to-severe symptomatic dry eye: a retrospective chart review. Clin Ophthalmol. 2019;13:1033–1037. doi:10.2147/OPTH.S191635
24. Donnenfeld ED, Karpecki PM, Majmudar PA, et al. Safety of lifitegrast ophthalmic solution 5.0% in patients with dry eye disease: a 1-year, multicenter, randomized, placebo-controlled study. Cornea. 2016;35:741–748. doi:10.1097/ICO.0000000000000803
25. Friedman NJ, Butron K, Robledo N, et al. A nonrandomized, open-label study to evaluate the effect of nasal stimulation on tear production in subjects with dry eye disease. Clin Ophthalmol. 2016;10:795–804. doi:10.2147/OPTH.S101716
26. Orrick B, Watson M, Angjeli E, et al. Quantitation of tear production by tear meniscus height following acute use of the intranasal tear neurostimulator. Invest Ophthalmol Vis Sci. 2017;58(8):2692.
27. Brinton M, Kossler AL, Patel ZM, et al. Enhanced tearing by electrical stimulation of the anterior ethmoid nerve. Invest Ophthalmol Vis Sci. 2017;58(4):2341–2348. doi:10.1167/iovs.16-21362
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



