Back to Journals » Open Access Emergency Medicine » Volume 13
Normal Saline Solution or Lactated Ringer’s Solution to Enhance Lactate Clearance in Septic Patients After Initial Resuscitation in the ED: A Retrospective Cohort Trial
Authors Limapichat T , Pattanapong K
Received 22 September 2021
Accepted for publication 22 November 2021
Published 1 December 2021 Volume 2021:13 Pages 511—519
DOI https://doi.org/10.2147/OAEM.S340691
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Thanya Limapichat, Krittapat Pattanapong
Department of Emergency Medicine, Songklanagarind Hospital, Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, Thailand
Correspondence: Thanya Limapichat
Department of Emergency Medicine, Songklanagarind Hospital, Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, 90110, Thailand
Tel +66 74-451705
Fax +66 74-451704
Email [email protected]
Objective: To compare the effect of isotonic crystalloid solutions between lactated Ringer’s solution (LRS) and normal saline solution (NSS) on lactate clearance in septic patients at the emergency department (ED).
Materials and Methods: This study is a single-center retrospective chart review. The study enrolled patients older than 18 years with sepsis and initial serum lactate level > 2 mg/dL in the ED. The primary outcome was to determine which isotonic solution was better for serum lactate clearance in septic patients. The secondary outcomes were serum creatinine change within 24 h and the 48-h survival rate after admission.
Results: A total of 120 patients were enrolled with a median crystalloid volume administered in the ED of 1000 mL. Within 2 h of resuscitation, there was no difference in lactate clearance between the LRS and NSS groups with median values of 29.2% and 25%, respectively (P=0.839). The 48-h survival rate after admission did not differ between the LRS and NSS groups with median values of 90% and 86%, respectively. Both isotonic solutions increased serum creatinine levels within 24 h of treatment with median values of 0.3 for each group (P=0.647).
Conclusion: Among septic patients in the ED treated with NSS or LRS, there was no difference in lactate clearance, serum creatinine change within 24 h, or 48-h survival. However, several factors were associated with increased lactate levels, such as older age and use of vasopressors and immunosuppressive agents.
Keywords: lactate clearance, balance crystalloid, sepsis, NEWS
Plain Language Summary
What is Already Known on This Topic
Isotonic crystalloid solution is the first choice for intravenous fluid resuscitation in septic patients.
What This Study Adds
The study shows no difference in lactate clearance for either of the crystalloid fluid solutions in septic patients at the emergency department. These factors were associated with poor lactate clearance; older age, vasopressor usage, and the immunosuppressive agents used.
Background
Sepsis is an emergency medical condition in which our immune system reacts to infection; resulting in organ dysfunction.1 According to the Third International Consensus Definition for Sepsis and Septic Shock (Sepsis-3), sepsis is defined as a “life-threatening organ dysfunction caused by a dysregulated host response to infection” and organ dysfunction as being “an increase in the Sequential (Sepsis-related) Organ Failure Assessment (SOFA) score of 2 points or more.”1
The SOFA score is calculated based on many factors, including laboratory results. Using this score for triaging septic patients before entering the emergency department (ED) is not appropriate and resulting in delayed treatment.2 Even though the quick (q) SOFA is the standard tool for triaging septic patients; according to the Sepsis-3 guideline, the National Early Warning Score (NEWS) is more prompt and efficient than the modified Early Warning Score, qSOFA, and the systemic inflammatory response syndrome score because the AUROC is high.3
Lactate is an end-product from many types of cells which is released into the blood and metabolized by the liver and kidneys by direct oxidation or as a source of glucose. Sepsis associated hyperlactatemia can be explained by many theories, such as tissue hypoxia. Meanwhile, sepsis can accelerate the glycolysis process by activation of the β2-adrenergic receptor.4 Many studies have stated that a serum lactate level above 4 mmol/L in patients with septic shock is associated with a poor prognosis and the mortality at 28 days is 4.29 times higher than the group with a lactate level <4 mmol/L.5 Moreover, lactate production has been associated with increased sympathetic activity (HR ≥ 90) and hypotension (MAP < 65 mmHg) and is a significant predictor of mortality.6
If the initial serum lactate is higher than 2 mmol/L, effectively decreasing the lactate level can decrease mortality at 28 days.7 One study showed lactate clearance of over 10% after 2 h of fluid resuscitation, which can be used as a goal of treatment within the early phase of managing a septic patient, or in the least it implies a good response from the treatment.8 According to a meta-analysis, using lactate clearance as a target to guide early therapy is linked to a lower risk of death in adult sepsis patients.9
According to the surviving sepsis campaign bundle 2018, intravenous fluid is one of the resuscitation strategies to treat sepsis as it can decrease the serum lactate level. If the initial serum lactate level is above 2 mmol/L before intravenous fluid infusion, it is recommended to follow the serum lactate level within 2–4 h.10 The recommend fluid is an isotonic solution which includes a normal saline solution (NSS) and balanced crystalloid solutions. NSS is composed of 154 mmol/L each of sodium and chloride ions. A balanced crystalloid solution replaces the chloride ions with bicarbonate or another buffer such as lactated Ringer’s solution (LRS) which can balance the pH of the patient’s blood.11
In non-critically ill adult patients who received at least 500 mL of isotonic crystalloid solution of either NSS or balanced crystalloid solutions such as LRS, Plasma-Lyte, or Acetar, there was no difference in 48-hour survival.12 Meanwhile, in critically ill patients who were admitted to the intensive care unit and received the median amount of 1000 mL of isotonic crystalloid solution, there were lower rates of composite outcome of death from any cause, new renal-replacement therapy, or persistent renal dysfunction compared to the use of NSS.13
Since 2018, Songklanagarind Hospital at the Prince of Songkla University has applied NEWS triaging for septic patients within the ED. A NEWS score equal to 5, 6, or 7 is defined as sepsis and scores 8–20 are defined as severe sepsis. For initial resuscitation, we routinely use NSS and LRS. Nevertheless, few studies have focused on the type of fluid resuscitation utilized in septic patients with the goal of lowering serum lactate levels. We focused on these two types of fluids, because we wanted to compare the results as well as to provide additional information to help clinicians make better decisions.
Materials and Methods
Study Design and Setting
A retrospective study was conducted at the ED of Songklanagarind Hospital which is a tertiary university hospital in Southern Thailand. The data were collected from January 2018 to October 2019. The inclusion criteria for the study were (1) aged >18 years of age, (2) visited the ED with initial NEWS ≥5 and were diagnosed with sepsis, (3) patients with sepsis were given ≥500 mL of only one type of isotonic crystalloid solution, (4) patients with sepsis were admitted to the ward, and (5) the initial serum lactate level was >2 mmol/L; which was measured before intravenous fluid initiation and a repeat serum lactate level was measured within 6 h. The exclusion criteria were (1) pregnancy or lactation, (2) end-stage renal disease with regular hemodialysis, (3) heart failure or pulmonary edema that was diagnosed at the same visit with sepsis, and (4) incomplete information.
A suspected septic patient is usually triaged to the ED. Diagnosis of sepsis does not depend only on NEWS at a triage zone. The emergency physician needs to complete history taking and a physical examination of the patient. The investigations are requested based on the suspected disease and patient profile. Intravenous fluid is started after the serum lactate results are known, and the results are usually followed within 6 h. The total amount of intravenous fluid, type of intravenous fluid, and the time to follow-up the serum lactate level depends on the clinical signs and symptoms as well as the doctor’s judgment.
Data Collection
The collected data from the medical records included: patient baseline characteristics, initial NEWS score, mechanical ventilation usage, vasopressor usage and concentration, underlying diseases, and medications related to immunocompromised status, drugs which increased serum lactate level such as β2-agonist, baseline serum creatinine, initial serum creatinine and electrolytes, chronic kidney stage, type of intravenous fluid, total intravenous fluid volume, serum lactate level within 2 h, 4 h, and 6 h, disposition, serum creatinine change within 24 h, and 48-h survival. The patients were categorized into two groups: NSS group or LRS group.
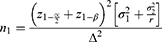
Sample size was calculated based on the Zitek et al study.14
We calculated sample size (n) from this formula. We used hypothesis testing two independent means.
 = Mean of lactate level difference in the LRS group = 0.93
= Mean of lactate level difference in the LRS group = 0.93
 = Mean of lactate level difference in the NSS group = 0.37
= Mean of lactate level difference in the NSS group = 0.37
 = Standard deviation of lactate level difference in the LRS group = 1.00
= Standard deviation of lactate level difference in the LRS group = 1.00
 = Standard deviation of lactate level difference in the NSS group = 1.24
= Standard deviation of lactate level difference in the NSS group = 1.24
Ratio (r) = N2/N1 = 1
N1 = 64: N2 = 64
To increase the statistical power of the analysis, we decided to increase the sample size by an additional 20%. Therefore, each group sample should be 64+13 people and a total sample of 154 people.
** 95% CI = mean ± 1.96 (SD/square root of n).
Outcome Measurements
The primary outcome was serum lactate change in septic patients within 24 h after intravenous fluids were given at the ED. The secondary outcomes were 48-h survival after admission and serum creatinine change within 24 h after intravenous fluids were given.
Definitions of Variables
Initial vital signs were defined as body temperature, pulse rate, respiratory rate, blood pressure, oxygen saturation, and Glasgow Coma Scale score from initial presentation in the triage zone. The NEWS cut point, identified as the summation of NEWS >4 (5 or more), is a medium score according to The United Kingdom, Royal College of Physicians 2012. Immunocompromised patients were defined as immunodeficiency from underlying diseases such as human immunodeficiency virus infection, diabetes mellitus, hematologic malignancy, malignancy diseases with previous chemotherapy within 1 month, and cirrhosis or the use of immunosuppressive drugs; such as, methotrexate, azathioprine, or cyclosporine. Sepsis in our study was defined as patients who were clinically suspected of infection with a NEWS score ≥5 and serum lactate >2 mmol/L. Lactate clearance was defined by the equation (initial serum lactate level – serum lactate level within 2 or 4 h) x 100/initial serum lactate level.
Statistical Analysis
All data were entered into Epidata software version 3.1 and the statistical analysis used R Software version 3.6.1. The continuous variables were mostly analyzed and reported as median or mean while categorical variables are reported as percentage. All data were based on non-parametric frequency distributions. The univariate model analyzed the baseline characteristics, medications, and comorbidities. The data were compared in subjects with NSS and LRS. Continuous variables were compared using the Mann–Whitney U-test. Categorical variables were compared using the χ2 or Fisher’s exact test as indicated. Significant predictive factors associated with increased serum lactate level (P<0.20) identified during multivariate analysis were introduced into a logistic regression model with backward stepwise selection. Generalized estimating equations were conducted for analysis of the serum lactate level between the groups at different time points. A P-value <0.05 was considered statistically significant.
Results
During the 22-month trial, 220 patients with NEWS ≥5 and serum lactate >2 mmol/L were treated with isotonic crystalloid solutions in the ED, and were hospitalized. The number of excluded patients was 100; exclusion reasons are shown in Figure 1. The final sample size was 120 patients who met the inclusion criteria. One hundred patients (83%) were in the NSS group and 20 patients (17%) were in the LRS group. The baseline characteristics were similar between the two groups; including, the demographic characteristics, burden of coexisting conditions, and renal function (Table 1).
 |
Table 1 Baseline Characteristics of the Patients |
 |
Figure 1 Consort flow diagram of trial. Notes: Adapted from: Schulz KF, Altman DG, Moher D; CONSORT Group. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. PLoS Med. 2010;7(3):e1000251.22 Copyright: © 2010 Schulz et al. Creative Commons Attribution License. |
The median crystalloid resuscitation volumes for septic patients were 1000 mL and 750 mL for the NSS and LRS groups, respectively. The total median crystalloid resuscitation volume for septic patients was 1000 mL in both groups.
Within 2 h of resuscitation, the LRS group had higher median lactate clearance (29.2%) compared with the NSS group (25%) without statistical significance (P=0.839). Within 4 h of resuscitation, the NSS group had higher median lactate clearance (27.1%) compared with the LRS group (0.8%) (P=0.515) (Figure 2). Both crystalloid isotonic solution resuscitation groups experienced a serum creatinine increase of 0.3 mg/dL (P=0.838). The LRS group had a higher 48-h survival rate of 90% compared with 86% in the NSS group without statistical significance (P=1.00). The median baseline creatinine level in the NSS group was 0.904 mg/dL (95% Cl 0.826, 0.941). Within 24 h of resuscitation, the median serum creatinine level increased by 0.4883 mg/dL (P<0.001). Meanwhile, the LRS group had a median baseline creatinine level of 0.885 mg/dL (95% Cl 0.716, 1.054) which increased by 0.1853 mg/dL within 24 h of resuscitations (P=0.34) (Table 2 and Figure 3).
 |
Table 2 Comparison of Isotonic Crystalloid Fluids in Septic Patients in the Emergency Department |
 |
Figure 2 Percentage of serum lactate change after intravenous fluid resuscitation in septic patients. |
 |
Figure 3 Serum creatinine level after fluid resuscitation in septic patients. *P<0.05. |
The increased group was defined as a serum lactate level that increased at any time within 24 h of resuscitation compared with the lowest level measured. Some factors were statistically significantly different between the decreased and increased groups. These factors were age, vasopressor usage, the immunosuppressive agent used, and serum creatinine (Table 3).
 |
Table 3 Comparison of the Increased and Decreased Lactate Groups |
Multivariate analysis with logistic regression revealed that the significant risk factors for increased lactate level in septic patients were older age, vasopressor usage, and the immunosuppressive agents used (Table 4).
 |
Table 4 Multivariate Analysis by Logistic Regression; if Isotonic Crystalloid Solution Results in Increasing versus Decreasing Serum Lactate Levels |
Discussion
Our study revealed that septic patients treated with LRS resulted in a higher serum lactate clearance within 2 h compared to NSS without statistical significance. Even though, a previous study reported that the serum lactate level rose after a 30 cc/kg bolus of LRS was given to healthy subjects.14 The mechanism of hyperlactatemia in septic patients is different from healthy patients. Lactate is metabolized by direct oxidation or as a source of glucose using both the liver and kidney. Meanwhile, during the sepsis process, lactate has increased removal, decreased production, and dilution; either, because of fluid administration during resuscitation or all of the above in variable combinations.4 According to the SALT-ED trial,12 serum creatinine in an ED patient treated with at least 500 mL of crystalloid fluid resuscitation within 24 h tended to increase and then return to baseline serum creatinine, which was consistent with the results of our study. Moreover, our study shared some common results with the Self et al study. Wherein, the 48-h survival rate demonstrated no difference between the NSS and LRS groups.12
In our practice, we usually use NSS for resuscitation; however, previous studies have shown that rapid NSS infusion led to hyperchloremic metabolic acidosis and a higher rate of AKI.15,16 The results of our study provide important information suggesting that LRS is a good choice for resuscitation instead of NSS as well.
Twenty-two of 120 (18.3%) patients were classified as being in the increased lactate group. We found that older age was associated with an increased lactate level, which differed from the Cheng et al study. This was possibly due to no subgroup analysis of the elderly and non-elderly in our study.17 Our study found that vasopressor and immunosuppressive agents usage had higher lactate levels compared with the no vasopressor and immunosuppressive agent groups; it is possible that this is due to the severity of these groups. In one trial, those who received vasoactive drugs had a higher lactate level18 and a higher APACHEII score. The APACHEII score is a predictor of in-hospital and 30-day mortality in septic patients.19
Immunocompromised patients are thought to be more vulnerable to severe infection and are often seen as a poor prognostic grouping in the case of septic shock. According to a previous study; immunocompromised patients, including those treated with corticosteroids and other immunosuppressive drugs, had a greater rate of bacteremia and were more likely to be infected with multiresistant bacteria. It also leads to a higher rate of mortality,20 which is also shown in the group with inadequate lactate clearance.21
A strength of our trial was the hypothesis test, for which no previous study had performed. However, our study has several limitations. First, we aimed for 154 participants but only 120 (78%) patients were enrolled into the study. A larger sample and extended duration would improve any future studies. Second, most of the intravenous fluid resuscitations (83%) in our study used NSS. Therefore, we would suggest changing the study design to a prospective study which could conduct randomization or allocation that would make the two groups of population more similar. Finally, this study was conducted in a single tertiary center hospital. Hence, a multicenter study may increase the generalizability of the study.
Conclusions
Among septic patients in the ED treated with either NSS or LRS, there was no difference in lactate clearance, serum creatinine change within 24 h, or 48-h survival. However, some factors were associated with an increased lactate level. These being; older age, vasopressor usage, and the immunosuppressive agents used.
Compliance with Ethical Requirements
The ethics committee of Prince of Songkla University approved this study. The institutional review board of Prince of Songkla University is affiliated with the International Conference on Harmonization in Good Clinical Practice. According to our institutional review board protocol for waiver of informed consent, and the requirement for consent was waived, because the participants had no more than minimal risk and standard treatment procedures were provided. All research information was kept as confidential data in an encrypted file with password and limited data access by only the researcher and assistant. The ethical registration number was REC.62-294-20-4. This study was conducted in accordance with the Declaration of Helsinki.
Acknowledgments
The authors thank Kingkarn Waiyanak for article searches and retrieval, Miss Kuson Phibun for assistance with the data collection, Dr. Pasuree Sangsupawanich, PhD and Miss Nannapat Pruphetkaew for assistance with the statistics, the Epidemiology Unit and the Faculty of Medicine for funding this research.
Author Contributions
Both authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801–810. doi:10.1001/jama.2016.0287
2. Churpek MM, Snyder A, Han X, et al. Quick sepsis-related organ failure assessment, systemic inflammatory response syndrome, and early warning scores for detecting clinical deterioration in infected patients outside the intensive care unit. Am J Respir Crit Care Med. 2017;195:906–911. doi:10.1164/rccm.201604-0854OC
3. Worapratya P, Wuthisuthimethawee P. Septic shock in the ER: diagnostic and management challenges. Open Access Emerg Med. 2019;11:77–86. doi:10.2147/OAEM.S166086
4. Garcia-Alvarez M, Marik P, Bellomo R. Sepsis-associated hyperlactatemia. Crit Care. 2014;18:503. doi:10.1186/s13054-014-0503-3
5. Dadeh AA, Wuthisuthimethawee P. Serum lactate levels as a prognostic predictor of septic shock in emergency department patients with systemic inflammatory response syndrome (SIRS) at Songklanagarind hospital. J Med Assoc Thai. 2016;99:913–918.
6. Jagan N, Morrow LE, Walters RW, et al. Sympathetic stimulation increases serum lactate concentrations in patients admitted with sepsis: implications for resuscitation strategies. Ann Intensive Care. 2021;11(1):1–9. doi:10.1186/s13613-021-00805-9
7. Bhat SR, Swenson KE, Francis MW, Wira CR. Lactate clearance predicts survival among patients in the emergency department with severe sepsis. West J Emerg Med. 2015;16:1118–1126. doi:10.5811/westjem.2015.10.27577
8. Jones AE, Kline J. Lactate clearance for assessing response to resuscitation in severe sepsis. Acad Emerg Med. 2013;20:844–847. doi:10.1111/acem.12179
9. Gu WJ, Zhang Z, Bakker J. Early lactate clearance-guided therapy in patients with sepsis: a meta-analysis with trial sequential analysis of randomized controlled trials. Intensive Care Med. 2015;41(10):1862–1863. doi:10.1007/s00134-015-3955-2
10. Levy MM, Evans LE, Rhodes A. The surviving sepsis campaign bundle: 2018 update. Intensive Care Med. 2018;44:925–928. doi:10.1007/s00134-018-5085-0
11. Semler MW, Kellum JA. Balanced crystalloid solutions. Am J Respir Crit Care Med. 2019;199:952–960. doi:10.1164/rccm.201809-1677CI
12. Self WH, Semler MW, Wanderer JP, et al. Balanced crystalloids versus saline in noncritically ill adults. N Engl J Med. 2018;378:819–828. doi:10.1056/NEJMoa1711586
13. Semler MW, Self WH, Wanderer JP, et al. Balanced crystalloids versus saline in critically ill adults. N Engl J Med. 2018;378:829–839. doi:10.1056/NEJMoa1711584
14. Zitek T, Skaggs ZD, Rahbar A, Patel J, Khan M. Does intravenous lactated ringer’s solution raise serum lactate? J Emerg Med. 2018;55:313–318. doi:10.1016/j.jemermed.2018.05.031
15. Semler MW, Rice TW. Saline is not the first choice for crystalloid resuscitation fluids. Crit Care Med. 2016;44:1541–1544. doi:10.1097/CCM.0000000000001941
16. Chowdhury AH, Cox EF, Francis ST, Lobo DN. A randomized, controlled, double-blind crossover study on the effects of 2-L infusions of 0.9% saline and plasma-lyte® 148 on renal blood flow velocity and renal cortical tissue perfusion in healthy volunteers. Ann Surg. 2012;256:18–24. doi:10.1097/SLA.0b013e318256be72
17. Cheng HH, Chen FC, Change MW, et al. Difference between elderly and non-elderly patients in using serum lactate level to predict mortality caused by sepsis in the emergency department. Medicine (Baltimore). 2018;97:e0209. doi:10.1097/MD.0000000000010209
18. Bou Chebl R, Jamali S, Mikati N, et al. Relative hyperlactatemia in the emergency department. Front Med (Lausanne). 2020;7:561. doi:10.3389/fmed.2020.00561
19. Gao L, Shi Q, Li H, Guo Q, Yan J. Prognostic value of baseline APACHE II score combined with uric acid concentration for short-term clinical outcomes in patients with sepsis. All Life. 2020;13:416–425. doi:10.1080/26895293.2020.1796828
20. Jamme M, Daviaud F, Charpentier J, et al. Time course of septic shock in immunocompromised and nonimmunocompromised patients. Crit Care Med. 2017;45(12):2031–2039. doi:10.1097/CCM.0000000000002722
21. Reddy AJ, Lam SW, Bauer SR, Guzman JA. Lactic acidosis: clinical implications and management strategies. Cleve Clin J Med. 2015;82(9):615–624. doi:10.3949/ccjm.82a.14098
22. Schulz KF, Altman DG, Moher D; CONSORT Group. CONSORT 2010 statement: updated Guidelines for Reporting Parallel Group Randomised Trials. PLoS Med. 2010;7(3):e1000251. doi:10.1371/journal.pmed.1000251
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.