Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 14
No impact of exacerbation frequency and severity on the physical activity decline in COPD: a long-term observation
Authors Sievi NA , Kohler M, Thurnheer R , Leuppi JD , Irani S, Frey M , Brutsche M , Brack T , Clarenbach CF
Received 25 September 2018
Accepted for publication 18 January 2019
Published 15 February 2019 Volume 2019:14 Pages 431—437
DOI https://doi.org/10.2147/COPD.S188710
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Noriane A Sievi,1 Malcolm Kohler,1 Robert Thurnheer,2 Joerg D Leuppi,3 Sarosh Irani,4 Martin Frey,5 Martin Brutsche,6 Thomas Brack,7 Christian F Clarenbach1
1Pulmonary Division, University Hospital of Zurich, Zurich, Switzerland; 2Pulmonary Division, Cantonal Hospital of Münsterlingen, Münsterlingen, Switzerland; 3University Clinic of Medicine, Cantonal Hospital Baselland and University of Basel, Basel, Switzerland; 4Pulmonary Division, Cantonal Hospital of Aarau, Aarau, Switzerland; 5Pulmonary Division, Clinic Barmelweid, Barmelweid, Switzerland; 6Pulmonary Division, Cantonal Hospital of St Gallen, St Gallen, Switzerland; 7Pulmonary Division, Cantonal Hospital of Glarus, Glarus, Switzerland
Introduction: COPD exacerbations are associated with a concomitant profound reduction in daily physical activity (PA). Thereby, exacerbation frequency and severity may have an amplifying effect. Whether the reduced level of PA returns to the level prior to exacerbation or has a sustained negative impact on activity behavior over time is unclear.
Methods: The number of steps per day over 1 week, as a measure of daily PA, was assessed annually in a cohort of patients with COPD. Exacerbation frequency and severity were documented. Uni- and multivariate mixed effect models were used to investigate associations between change in number of steps per day (dependent variable) and exacerbations. Stratification by possible confounders was performed.
Results: One hundred and eighty one COPD patients (median [quartile] age 64 [59/69] years, 65% male, median [quartiles] FEV1 % pred. 46 [33/65]) suffered a total of 273 exacerbations during the observation period (median [quartiles] follow-up time of 2.1 [1.6/3.1] years). Neither the frequency nor the severity of exacerbations was significantly related to the overall decline in PA over time. Stratification by different possible confounders such as age, sex and disease severity did not yield a subgroup in which exacerbations enhance the decrease in PA over time.
Conclusion: The drop in PA during the phase of an acute exacerbation seems not to be a lasting phenomenon leading to a fundamental change in activity behavior.
Trial registration: www.ClinicalTrials.gov, NCT01527773
Keywords: COPD, daily physical activity, exacerbation
Introduction
Acute exacerbations (AEs) of COPD are clinically characterized by a sustained worsening of patients’ condition (increase of dyspnea, cough and/or sputum) beyond normal day-to-day variation.1 Previous studies have shown a negative impact of AE on various health-related outcomes in patients with COPD. These include a reduced pulmonary function, an impaired quality of life and a worse survival.2–4 Therefore, AEs are recognized as an important factor predicting poor outcome in COPD patients.
Daily physical activity (PA) is acutely reduced in patients suffering from severe exacerbations requiring hospitalization5 as well as in patients treated for exacerbations in an ambulatory setting.6,7 Epidemiological studies have shown that a low level of PA is an important prognostic marker in COPD. Some of these studies suggest that patients practicing regular PA reduce their risk of hospital admission due to AE.8–10 Esteban et al11 demonstrated that exacerbation-related decrease in PA is the best predictor of 1-year risk of mortality in over 1,800 COPD patients enrolled in a prospective observational cohort study.
A previous study by our group investigated the natural course of daily PA over time and possible predictors.12 There was no significant difference in PA decline between patients with frequent exacerbations (≥2 exacerbations/year) and nonfrequent exacerbations (0–1 exacerbations/year). Recently published data on the effect of COPD exacerbations, especially the severity of exacerbations, on the decline in daily PA within 1 year revealed a possible acceleration by moderate and severe exacerbations.13 To verify these findings, the objective of the present analysis was to investigate the association between frequency and severity of exacerbations and changes in PA over time in our COPD cohort.
Methods
Study design and subjects
In the longitudinal, prospective cohort study “The Obstructive Pulmonary Disease Outcomes Cohort Study” patients with mild to very severe COPD were included from seven Swiss pulmonary outpatient clinics. Recruitment period was between October 2010 and December 2015. Patients were asked to participate during outpatient visits or during hospital stays for initially three annual study visits (some patients agreed to participate up to 7 years). The study was finished in December 2016 after the last recruited patients performed at least one follow-up visit. This manuscript analyses data out of this cohort and only patients with at least one follow-up measurement were included. Inclusion criteria were defined as 1) 40 to 75 years old at inclusion and 2) confirmed COPD according to GOLD guidelines.14 Patients who suffered from mental or physical disability precluding informed consent or compliance with the protocol were excluded. In case of an acute COPD exacerbation at time of screening or yearly follow-up, visits were performed with a delay of at least 6 weeks in an exacerbation-free interval.
The study was conducted in accordance with the Declaration of Helsinki, and all subjects gave written informed consent to participate. The Ethics Committee of the Canton of Zurich approved the study (EK-ZH-NR: 1734 and 2011-0106). The study registration number at www.ClinicalTrials.gov is NCT01527773.
Measurements
Assessment of daily PA
The number of steps per day was assessed by a triaxial accelerometer of a multisensory armband (SenseWear Pro™; Bodymedia Inc., Pittsburgh, PA, USA). The sensor had to be worn on the upper left arm over the triceps muscle.15
The number of steps per day was annually recorded over 7 consecutive days. A minimum of 4 days with at least 22.5 hours/day was demanded to be included in the analysis.16 Due to the longitudinal setting of this study, intensity of PA (eg, time spent at moderate activity) was not included in this analysis since disease progression over time possibly increases energy expenditure for same activity tasks and therefore could overestimate intensity of PA. Fifteen patients were excluded from the analysis due to missing PA values (technical reasons, armband not worn), six patients failed to reach the demanded wearing time and two patients performed an allergic reaction to the armband. Seasonality was considered in the analysis.
Exacerbations
The number and severity of AE during the preceding year were assessed by medical reports and asking patients themselves. If exacerbation history did not match between patient and medical records, we contacted the general practitioner and/or external pulmonologist for clarification. AE was defined as an event which led to prescription of antibiotics and/or corticosteroids.17 Severity of AE was defined as follows: moderate exacerbation (treated in an ambulatory setting) and severe exacerbation (AE led to hospitalization). For exacerbation categories, patients with moderate and severe exacerbations within the same year were categorized as severe. Patients with infrequent exacerbations were considered to have 0–1 AE per year, whereas patients with ≥2 AE per year were defined as frequent exacerbators.18
Lung function
Standard pulmonary function testing was performed to measure FEV1 and FVC according to ATS guidelines.19,20 Only values after bronchodilation were analyzed. Disease severity was categorized by spirometric GOLD stages (1–4) and COPD risk groups (A [low risk, less symptoms] to D [high risk, more symptoms]).21 The modified medical research council (mMRC) scale22 was used to assess dyspnea and the COPD Assessment Test (CAT)23 to assess disease specific symptoms.
Data analysis and statistics
Results are shown as mean values (SD) or median (Q1-quartiles/Q3-quartile) unless otherwise stated. Statistical analysis was performed with STATA 15.0 (StataCorp, College Station, TX, USA).
Uni- and multivariate mixed effect models were used to investigate the association between annual change in number of steps per day (dependent variable) and exacerbation parameters, accounting for possible confounders (e.g., sex, disease severity). To investigate the possibility that exacerbations may influence the course in daily PA at about the same time or with a delay, all analyses were performed with exacerbations parameters from 1) the corresponding follow-up period and 2) from the year prior to examination.
To check the regression assumptions, residual analysis of the model was performed.
A two-sided P-value of <0.05 was considered to be statistically significant.
Results
Study participants
Three hundred thirteen patients were included at baseline, whereof 181 COPD patients (45% spirometric GOLD stage 1/2, 38% GOLD 3 and 16% GOLD 4) entered this analysis (Figure 1). Follow-up time was median (quartiles) 2.1 (1.6/3.1) years with a minimum of one follow-up visit and a maximum of seven annual follow-up visits. During follow-up, 127 patients were analyzed at year 3 and 48 at year 4. Sixty-five percent of the COPD patients were male, median (quartiles) age was 64 (59.0/69.0) years. Further patient characteristics are presented in Table 1. Reasons for missing first or second follow-up visit were withdrawal, not able to participate anymore due to worsening health status, lung transplantation, moving abroad, lost to follow-up and death.
  | Figure 1 Study flow. |
At baseline, 67 out of 181 patients (37%) suffered from at least one exacerbation in the previous year, 14% of patients were classified as frequent exacerbators. In total, there were 273 exacerbations during the observation period, 55 of them led to hospital admissions.
In this cohort, the mean (95% CI) number of steps per day significantly decreased by annually −479.1 (−634.2/−324.1) steps, P<0.001. Patients who were followed-up did not show any differences in exacerbation frequency and daily PA compared to patients who failed to follow-up.
Exacerbations within the particular year of observation
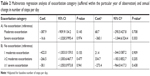
The number of exacerbations during the year had no influence on the decline in number of steps per day (mean Coef. [95% CI] −18.4 [−250.9/214.1], P=0.877), even after adjusting for baseline number of steps (P=0.245). There was no significant difference in change in number of steps per day between exacerbation categories (no exacerbation/moderate exacerbation/severe exacerbation) (Table 2A). Adjusting for baseline number of steps per day revealed a slightly greater decline in daily PA over time in patients with at least one severe exacerbation. However, it did not reach statistical significance (Table 2A and Figure 2).
Exacerbation categories (no exacerbation, 1 moderate exacerbation, ≥2 moderate exacerbations, ≥1 severe exacerbation) in accordance to Demeyer et al13 showed no significant difference in change in number of steps per day over time, unadjusted and adjusted for baseline number of steps per day (Table 2B).
Furthermore, the decline in number of steps per day over time was not significant different between frequent exacerbators and infrequent exacerbators (mean Coef. [95% CI] −136.9 [−746.9/473.1], P=0.660; mean Coef. [95% CI] adj. for baseline number of steps per day 241.9 [−179.9/663.6], P=0.261).
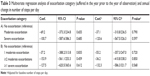
Exacerbations in the year prior to the year of observation
The annual change in number of steps per day was not influenced by the number of exacerbations in the previous year (mean Coef. [95% CI] −58.4 [−189.3/72.5], P=0.382). Furthermore, there was no significant difference in annual change in number of steps per day between different exacerbation–severity categories (no exacerbation/moderate exacerbation/severe exacerbation and no exacerbation/1 moderate exacerbation/≥2 exacerbations/≥1 severe exacerbation, respectively) (Table 3A and B). Frequent exacerbators did not show a significant different annual change in number of steps per day compared to infrequent exacerbators (mean Coef. [95% CI] −192.9 [−538.6/152.8], P=0.274).
Adjusting for baseline number of steps did not yield any changes in our findings.
Stratification by possible confounders
Neither age, sex, body mass index, airway obstruction (GOLD stages), seasonality of PA assessment, number of comorbidities nor COPD risk category revealed a subgroup in which exacerbation profile is associated with a decline in number of steps per day. Although COPD-related symptoms (mMRC and CAT) significantly increased over time, there was no influence on the annual decline in number of steps per day, irrespective of exacerbation category. Furthermore, there seems to be no healthy survivor effect since there was no different associations between exacerbation categories and change in number of steps per day in patients who died within or after the study period (last update in November 2017) and patients who survived.
Discussion
This study investigated the hypothesis whether the frequency and severity of exacerbations influence PA in patients with COPD over a period of up to 7 years. We found that neither the number nor the severity of exacerbations was related to the overall decline in PA over time. This study shows that although a considerable drop of PA has been attributed to the phase of an AE in previous studies, this decline seems not to be a lasting phenomenon leading to a fundamental change in activity behavior.
AEs are known to have an important impact on the quality of life and mortality in patients with COPD. It can take several weeks until respiratory symptoms are back to baseline.24 Although a deteriorating of respiratory symptoms is by definition a key feature of an AE, several additional observations can be made such as a profound reduction of daily PA. In a prospective study of almost 2,500 COPD patients, Esteban et al11 reported that after a moderate to severe COPD exacerbation, a failure to recover the level of PA (baseline to 2 months after the event assessed by questionnaire) had an important negative impact on survival at the 1-year follow-up.
Alahmari et al6 assessed daily step count prior, during and after AE in 73 COPD patients and found a median step count of 198 days per patient. Daily step-count returned to the level prior to AE within a median (interquartile range) of 3.5 (1–8) days. A larger fall in daily step count at exacerbation implicates a longer period to return to the normal activity level. Some studies showed a prolonged recovery time to initial daily PA level or even no return to baseline level.5,11 A study with 17 COPD patients admitted to hospital due to AE revealed a reduced time on weight-bearing activities (walking and sitting) not only during hospitalization but also 1 month after discharge when compared to stable COPD patients.5
Demeyer et al13 recently report the results of a larger cohort consisting of 141 COPD patients, looking at PA (by accelerometer) and number and severity of COPD exacerbations. Two or more moderate exacerbations or a severe exacerbation led to a significant greater decline in daily step count after 1 year compared to patients without exacerbations. In our cohort these findings could not be confirmed. Patients with more frequent or severe exacerbations were not prone to an accelerated annual decline in PA. Comparing patients with severe exacerbations to the ones with no or moderate exacerbations showed qualitatively a slightly greater decrease that was however not statistically significant (Figure 2). It could be hypothesized that after a severe exacerbation these patients might almost but not fully reach their level of daily PA prior to hospitalization. However, there is only one study investigating the minimal important difference (MID) in number of steps per day in patients with COPD. In 74 patients, MID was set between 600 and 1,100 steps per day.25 Therefore, it is not possible to conclude if this slightly greater decrease reports an MID despite nonsignificance.
Different considerations have to be taken into account when comparing both cohorts. The observation time relies on two time points (measurement at baseline and at 12 months’ follow-up) in the analysis by Demeyer et al.13 In our cohort, patients were observed up to 7 years. Further, PA did not decline in their cohort while our patients showed a significant annual decline in daily steps over time. This decline corresponds approximately to the decline of PA described by Waschki et al.26 Overall, our cohort was slightly less active. However, the different findings between both studies cannot be explained by this fact since all results were also adjusted for baseline PA.
The hypothesis that an increase in COPD related symptoms (assessed by mMRC or CAT) as a consequence of more frequent exacerbations may lead to a downward spiral resulting in a lower level of daily PA cannot be confirmed in our cohort. Therefore, further longitudinal analysis including the whole spectrum of COPD patients is needed to determine the effect of exacerbations on the level of PA over time.
A limitation of this study is that we cannot exclude that some patients underwent pulmonary rehabilitation after a severe exacerbation weakening the effect of exacerbation on decline in PA. However, duration between pulmonary rehabilitation and measurement can be assumed as random and patients were measured with a delay of 6 weeks after exacerbations. Furthermore, the effect of pulmonary rehabilitation on PA beyond 3 months is unclear;27 thus, we think it will not influence our results. Exacerbation duration and time between exacerbations and study visits were not analyzed, although a shorter time interval between last exacerbation and study visit could have influenced the number of steps per day in the individual patient. Due to the high number of exacerbations during the observation period, we assume that they are evenly distributed among a study year and therefore show no impact on our results. This COPD cohort study was designed to characterize COPD patients with annual follow-ups. Therefore, no sample size calculation was performed a priori for our outcomes. A lack of significance of some predictors (e.g., severe exacerbations) cannot be excluded due to a possible small number of events each year.
In conclusion, the findings of the current study do not support the hypothesis that frequency and severity of exacerbations have a significant impact on the decline of daily PA over time.
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki, and all subjects gave written informed consent to participate. The Ethics Committee of the Canton of Zurich approved the study (EK-ZH-NR: 1734 and 2011-0106) and the study is registered at www.ClinicalTrials.gov, NCT01527773.
Data sharing statement
The data sets used and analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
This study was supported by Lunge Zurich, Lung league of both Basel, Gottfried and Julia Bangerter-Rhyner foundation, Freiwillige Akademische Gesellschaft Basel, Lung league of Canton Thurgau, Lung league of Canton St Gallen, Lung league of Canton Aargau and Lung league of Canton Glarus.
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Burge S, Wedzicha JA. COPD exacerbations: definitions and classifications. Eur Respir J Suppl. 2003;41:46S–53S. | ||
Seemungal TAR, Donaldson GC, Paul EA, Bestall JC, Jeffries DJ, Wedzicha JA. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157(5):1418–1422. | ||
Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002;57(10):847–852. | ||
Groenewegen KH, Schols AM, Wouters EF. Mortality and mortality-related factors after hospitalization for acute exacerbation of COPD. Chest. 2003;124(2):459–467. | ||
Pitta F, Troosters T, Probst VS, Spruit MA, Decramer M, Gosselink R. Physical activity and hospitalization for exacerbation of COPD. Chest. 2006;129(3):536–544. | ||
Alahmari AD, Patel ARC, Kowlessar BS, et al. Daily activity during stability and exacerbation of chronic obstructive pulmonary disease. BMC Pulm Med. 2014;14(1):98. | ||
Ehsan M, Khan R, Wakefield D, et al. A longitudinal study evaluating the effect of exacerbations on physical activity in patients with chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2013;10(6):559–564. | ||
Garcia-Aymerich J, Farrero E, Félez MA, et al. Risk factors of readmission to hospital for a COPD exacerbation: a prospective study. Thorax. 2003;58(2):100–105. | ||
Garcia-Aymerich J, Lange P, Benet M, Schnohr P, Antó JM. Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population based cohort study. Thorax. 2006;61(9):772–778. | ||
Seidel D, Cheung A, Suh ES, Raste Y, Atakhorrami M, Spruit MA. Physical inactivity and risk of hospitalisation for chronic obstructive pulmonary disease. Int J Tuberc Lung Dis. 2012;16(8):1015–1019. | ||
Esteban C, Garcia-Gutierrez S, Legarreta MJ, et al. One-year mortality in COPD after an exacerbation: the effect of physical activity changes during the event. COPD. 2016;13(6):718–725. | ||
Clarenbach CF, Sievi NA, Haile SR, et al. Determinants of annual change in physical activity in COPD. Respirology. 2017;22(6):1133–1139. | ||
Demeyer H, Costilla-Frias M, Louvaris Z, et al. Both moderate and severe exacerbations accelerate physical activity decline in COPD patients. Eur Respir J. 2018;51(1):1702110. | ||
Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: gold executive summary. Am J Respir Crit Care Med. 2007;176(6):532–555. | ||
van Remoortel H, Raste Y, Louvaris Z, et al. Validity of six activity monitors in chronic obstructive pulmonary disease: a comparison with indirect calorimetry. PLoS One. 2012;7(6):e39198. | ||
Watz H, Pitta F, Rochester CL, et al. An official European Respiratory Society statement on physical activity in COPD. Eur Respir J. 2014;44(6):1521–1537. | ||
Laurent S, Boutouyrie P, Asmar R, et al. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001;37(5):1236–1241. | ||
Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med Overseas Ed. 2010;363(12):1128–1138. | ||
Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. | ||
Macintyre N. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J. 2005;26(4):720–735. | ||
Global Initiative for Chronic Obstructive Lung Disease: Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Disease. Available from: https://goldcopd.org/global-strategy-diagnosis-management-prevention-copd-2016/. 2016. | ||
Mahler DA, Wells CK. Evaluation of clinical methods for rating dyspnea. Chest. 1988;93(3):580–586. | ||
Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD assessment test. Eur Respir J. 2009;34(3):648–654. | ||
Seemungal TAR, Donaldson GC, Bhowmik A, Jeffries DJ, Wedzicha JA. Time course and recovery of exacerbations in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000;161(5):1608–1613. | ||
Demeyer H, Burtin C, Hornikx M, et al. The minimal important difference in physical activity in patients with COPD. PLoS One. 2016;11(4):e0154587. | ||
Waschki B, Kirsten AM, Holz O, et al. Disease progression and changes in physical activity in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2015;192(3):295–306. | ||
Mantoani LC, Rubio N, McKinstry B, Macnee W, Rabinovich RA. Interventions to modify physical activity in patients with COPD: a systematic review. Eur Respir J. 2016;48(1):69–81. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.