Back to Journals » Patient Preference and Adherence » Volume 10
Nepalese patients’ perceptions of treatment modalities for type 2 diabetes
Authors Sapkota S, Brien J, Aslani P
Received 24 May 2016
Accepted for publication 28 June 2016
Published 13 September 2016 Volume 2016:10 Pages 1777—1786
DOI https://doi.org/10.2147/PPA.S113467
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Sujata Sapkota, Jo-anne E Brien, Parisa Aslani
Faculty of Pharmacy, The University of Sydney, Sydney, NSW, Australia
Background: Perceptions and beliefs about treatment can influence patients’ adherence to treatment regimens. Perceptions, in turn, are often shaped by patients’ sociocultural context. Nepal and the Nepalese have unique sociocultural traditions and beliefs, and their perceptions of diabetes treatment remain largely unexplored. This study explored Nepalese participants’ perceptions of diabetes treatment, and whether perceptions differed between the Nepalese living in Australia and Nepal.
Methods: Face-to-face qualitative interviews (n=48) were conducted with Nepalese participants with type 2 diabetes in Sydney and Kathmandu. All interviews were audio-recorded, transcribed verbatim, and thematically analyzed.
Results: Perceptions of diabetes treatment were similar among Nepalese participants in Australia and Nepal. There was a general reluctance to start oral antidiabetic medications and an even greater reluctance to commence parenteral (insulin) therapy. Participants preferred to try lifestyle modifications and alternative treatments such as herbs and “traditional” medicines, particularly as a first step. Unwillingness to take medications was primarily associated with the belief that, once started, these medications needed to be taken for life, and perceptions of long-term harms caused by such medications. Even when commenced on medication, participants were averse to any type of therapy escalation, for example, moving to insulin therapy. Insulin was perceived as the “last option” available for diabetes treatment. Most participants, however, did not find medication taking challenging once they had commenced treatment.
Conclusion: Antidiabetic medications were perceived to be harmful and unstoppable once initiated. These perceptions significantly impacted participants’ willingness to commence antidiabetic medications and therefore have the potential to adversely affect their medication-taking behavior. This study therefore highlights the need to explore the impact of these perceptions on participants’ medication-taking behavior, and the need to address patients’ views of “modern” (commonly prescribed) and “traditional” (natural) medications through information and education, to ensure increased understanding of how medications are used for diabetes management.
Keywords: adherence, antidiabetic medications, qualitative study, Nepal, Australia
Introduction
Diabetes mellitus, a chronic disease characterized by hyperglycemia, is becoming increasingly common in most countries worldwide.1 The total number of people with diabetes is projected to rise from 285 million to 438 million by 2030.2 Diabetes has been recognized as a significant public health problem in Nepal, with the reported urban prevalence of diabetes at ~15% among people aged ≥20 years and 19% among people aged ≥40 years.3 Diabetes is also reported as the third highest prevalent noncommunicable disease in hospitals in Nepal after chronic obstructive pulmonary diseases and cardiovascular diseases.4
The chronic nature of the disease and the associated complications make the management of diabetes complex. While diet, exercise, and education are the foundation of any type 2 diabetes (T2D) treatment program, a wide array of oral hypoglycemic agents (OHAs) and/or insulin are available for diabetes management.5 Individualization of both glycemic targets and therapies is considered ideal and recommended for effective management of diabetes.5 Although treatment varies between patients, diabetes treatment is usually started with diet modification and exercise. OHAs, particularly metformin, are started as first-line therapy, followed by other oral agents and insulin. However, whether or not patients are kept on medications, effective lifestyle management is still important.
Poor adherence or suboptimal use of available treatments, including adherence to lifestyle recommendations, may lead to inadequate blood glucose level control.6 It is thought that individuals’ beliefs and perceptions influence how people interpret information, which in turn impacts their experiences and guides their behavior.7 Perceptions and beliefs about treatment can thus have an influence on patients’ behavior toward recommended treatment options. Additionally, beliefs and perceptions can be influenced, and are often shaped, by sociocultural context.8 Social, psychological, and culturally mediated health beliefs can pose challenges to effective diabetes management.9,10 Racial/ethnic differences in patients’ concerns related to diabetes medications have also been documented.11
The sociocultural construct, traditions, and the ideologies of the people of Nepal are complex and unique. It has been reported that perceptions of illness causation in Nepal vary from individual carelessness to supernatural causes to blaming unseen malign forces.12 For example, some people in Nepal perceive diseases such as HIV/AIDS and leprosy as a result of bad karma, curse, or sin.13,14 Similarly, unique treatment and healing traditions are practiced in Nepal and can range from the practice of Ayurveda to faith-healers to “Western” medicines.15 For instance, treatment methods used in Nepal for the fainting episodes during epilepsy vary from treatment methods used by traditional healers, such as sprinkling treated water over the forehead [jhar phuk], herbal medicine, casting a spell, smelling dirty clothes and shoes, to the use of modern anticonvulsant treatments.16 Nepalese health and treatment beliefs, therefore, can be based on biomedical, natural, supernatural, or combination of different categories.12,15
The health and treatment beliefs of Nepalese patients with T2D remain largely unexplored. Understanding patients’ own values and beliefs about diabetes treatment along with their treatment preferences can provide some insights into patients’ likely medication-taking behavior and into the factors to be considered while prescribing treatments to achieve better adherence. To address this gap in the literature, this paper aims to shed light on the perceptions, attitudes, and beliefs about diabetes treatment options of Nepalese patients with T2D and investigates if the perceptions differ between Nepalese participants living in Australia and Nepal.
Methods
Ethical clearance for the conduct of the broader research project, which aimed to explore diabetes management in Nepalese patients with T2D, was obtained from the Human Research Ethics Committee at the University of Sydney in Australia and from the Nepal Health Research Council Ethical Review Board in Kathmandu, Nepal.
Participant selection and recruitment process
Adult (≥18 years of age) Nepalese patients with T2D on at least one antidiabetic medication were recruited for interview in Sydney and in Kathmandu. For the purpose of recruitment in Sydney, “Nepalese” was defined as “any person who was born in Nepal or whose one or both parents were born in Nepal”. The sample qualifying under the above definition could be in Australia on a temporary or permanent basis.
The participants in Sydney were recruited through advertisements in print (Nepalese newspapers), Facebook and Gumtree, advertisements placed in selected grocery shops and restaurants, word of mouth, and snowballing.17 Similarly, the recruitment process in Kathmandu involved advertisements in pharmacies and medical centers within traveling distance of Kathmandu, word of mouth, and snowballing.
Data collection and analysis
In-depth, face-to-face (semistructured) interviews were conducted with the participants. Each participant provided a written informed consent to participate in the study, before the interview. Data collection continued until the repetition and redundancy in the data in each cohort was evident; in other words, interviews were conducted to ensure “data saturation”18 was reached in each country. Eighteen participants in Sydney and 30 in Kathmandu were interviewed. The interviews were based on an interview protocol developed to investigate patients’ experiences with diabetes and to explore their overall diabetes management and factors that influenced antidiabetic medication taking. The protocol was tested for face and content validity19 with a sample of researchers and potential participants (data not included in the final analysis) prior to commencing the study. The broad themes explored during the interviews are presented in Table 1. This paper only presents the findings on the perceptions of, and attitudes to, treatment options for diabetes.
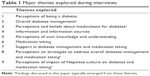  | Table 1 Major themes explored during interviews |
All interviews were conducted by SS, a Nepali pharmacist and researcher, in Nepali language, and were audio-recorded with the written permission of all participants. The duration of the interviews was approximately 1 hour. The interviews were transcribed verbatim and thematically analyzed. The first three transcripts were translated into English and independently analyzed by SS and PA. Consensus was reached regarding themes, after which the remaining interviews were analyzed by SS; a constant comparison approach was used throughout the analysis process to compare the data. Field notes taken after each interview were also assessed and analyzed. Data analysis revealed that there were no significant differences in participants’ perceptions of treatments for diabetes between the two countries. Therefore, the findings from the interviews conducted in both countries have been grouped together and the differences reported where applicable.
Results
Participants’ demographics
A total of 48 participants were interviewed (Table 2). Out of 18 participants interviewed in Sydney, 12 were first-generation migrants and six were visiting parents. The median age of the participants was 55.5 years and majority were male (n=30; 62.5%). The median duration of diagnosis was 7.7 years. At the time of interview, 46 patients were taking OHAs, and six were using insulin, with or without OHAs. None of the participants in Australia were using insulin at the time of interviews. The perceptions of treatment modalities for diabetes have been reported under the themes outlined in Table 3.
  | Table 2 Demographic characteristics of the participants |
  | Table 3 Key themes about patients’ perceptions of diabetes treatment |
Perceptions of treatments for diabetes
Overall, treatments employed by Nepalese participants for diabetes ranged from standard methods of diabetes treatment, which included alterations in lifestyle practices (diet and exercise) and using conventional prescribed medications (OHAs and insulin), to the use of alternative practices, such as using traditional medications (ayurvedic/herbal medicines/herbs), home remedies, or other alternative methods. Particularly at the initial phases of diagnosis and treatment, most participants preferred to use alternative methods and lifestyle modifications rather than prescribed antidiabetic medications.
Perceptions of first-line treatment methods (lifestyle practices and OHAs)
Despite initial hesitation to start medications (OHAs), most had faith in the ability of conventional medications to manage hyperglycemia. Opinions about the effectiveness of lifestyle methods and medications differed. For example, while some perceived exercise or diet or medication as the most effective measure for diabetes control, others perceived the decrease in blood glucose as a cumulative effect of the three. A few who experienced a more obvious improvement in blood glucose level with exercise and diet felt the two were more important than medications. Overall, participants preferred to adopt lifestyle modifications rather than the medications for diabetes.
Initial perceptions
A majority of the participants interviewed in Australia and Nepal reported their initial hesitation to start antidiabetic medications. The general fear and reluctance toward using conventional antidiabetic medications was associated with participants’ beliefs that a more “natural” way of treatment was a better strategy for diabetes management and that conventional medications could have long-term negative effects on the body.
I said to the doctor, ‘doctor, I will not take [start] the medications for sometimes; may be it will get easier like that [without medicines]? I will walk, control my diet’. (Nepal [N] 013, 45 years[Y]/female[F])
A majority also perceived that once started, conventional medications could not be stopped. The perceived beliefs about harm from conventional medications and about “natural” being safe, were derived from preconceived ideas prevalent in Nepalese society, especially in the villages:
In villages, it’s like this […] that when you take ‘English’ medicines, it will harm this, it will harm that! A lot of people told me that. (N003, 44 Y/male[M])
Participants also actively resisted any type of therapy escalation – an increase in the dose, increase in the number of medications, or having to use insulin; and hoped for de-escalation.
Implementation and beliefs
Participants’ experiences with, and increased understanding about, diabetes made most of them appreciate the need for antidiabetic medications. Most expressed faith in the medications they were taking and said they believed that medications were effective in controlling hyperglycemia. Some considered medications to be essential to live and/or to avoid complications arising from diabetes. Hence, despite reservations, participants accepted the need for medications. A few specifically acknowledged that they experienced symptoms or an increase in blood glucose level if they missed their antidiabetic medication dose and hence were firm believers of the importance of their medications. Adapting to and implementing the medications was not perceived to be difficult, by most.
A few believed that taking a medication was the only choice they had, as “there are no other means available” (N030, 64/M). A few said they trusted their doctors and their recommendations and hence trusted the medications they prescribed. While most reported faith in their medications, some were uncertain about the impact of medications in diabetes control, and appeared confused as to why their blood glucose levels did not come down despite regular medication taking.
In my experience, I can’t say if the medications have worked or is it because I have controlled my diet. I can’t specify. Yes, there has been a reduction […] it [blood sugar] is not like before […] but how it decreased, I can’t say […] whether it is because of medications or because of control in food habit, that I cannot say! (Australia [A] 003, 67 Y/M)
Now whether it is because my diabetes is old [been diabetic for a long time] […] the medicines […] now it [blood sugar] is not decreasing. To say I don’t believe, I am taking them […] but [diabetes] does not get controlled. The doctor says he has increased (the dose) to the maximum power. But the medicines have not controlled my diabetes. (N001, 54Y/F)
A few still perceived “natural” way as a better treatment method, despite being on medications, and regretted having initiated medications, as now they believed, they cannot discontinue.
It’s better not to take them [medications] at first […] it’s better [to control] with something else, by avoiding sugar and rice, avoiding potatoes […] now when you become habituated [to medications], then to stop it is not possible […] it’s better to take herbs, herbs are better. Once you start taking medications, after 1–2 years of taking medications, using insulin […] there is a fear if anything would happen if you stop it […] no the doctor won’t let you stop […] that is what has happened. Actually it is better not to take medications. From my experience […] my thinking, it is better not to take! (N008, 66Y/F)
A participant in Australia, who reported that her blood glucose level mostly stayed at the higher side of the normal range, appeared unconvinced that the antidiabetic medication prescribed for her was necessary; she felt the doctor did not want to take a risk by keeping her without medication.
In my opinion, if I was in Nepal, the doctors would not have started the medications so soon. But here the doctors don’t take risk […] as soon as they see little bit [increase] […], because if anything happens, the doctors [will be in trouble]. People sue him, so, it might create a problem for him, they never take more risk. If anything happens, they give the medicines immediately. And in my case as well […] in my opinion it was not that high. (A007, 54Y/F)
Medication was perceived by some to “weaken” the body, and a few participants felt that an adequate amount of food was essential to help the body “balance” the effect of medications. On the other hand, a few perceived being on medications provided one the freedom to be “less-careful” with diet.
Perceptions of insulin use
Negative emotions were mostly associated with the possibility of insulin requirement for diabetes management. Participants were, in general, reluctant to incorporate insulin into their antidiabetic regimen. The thought that one might require insulin created panic. In addition to the concern about the inconvenience of “injecting everyday”, participants considered insulin as being the “last option” and wanted to avoid it as much as possible. Insulin was understood as a remedy when nothing else worked. Additionally, people perceived that closer control and greater cautiousness would be required with insulin therapy; for example, participants perceived a stricter schedule was required for timing of food intake and insulin injections. “To control [blood sugar] […] and not to take it to ‘insulin’s stage’” (N025, 72Y/M) was reported as the goal of diabetes management.
Insulin is the last option. When you go to insulin, you have to think that it’s time to go [die]. (A015, 63Y/F).
Participants who were on OHAs expressed their concern about the possible need for insulin. They did not want insulin as part of therapy and would avoid it if possible. The transition from oral medications to insulin therapy brought back the reluctance and fear patients had at the start, when they were told to initiate medications (the OHAs).
Till now [oral] medications were working. Currently the doctor has been saying that these medications are not working and insulin must be given. Now as I am being directed towards insulin, I have the same kind of feeling […] like the one that I had at the beginning. (N001, 54Y/F)
Insulin was also reported, by a few participants in Nepal, to burden and worry the family members or the carers involved.
But for my family, “he will be in pain while injecting […] Now this has to be done daily, injected”. […] for people who witness, like the day before yesterday a sister had visited. Just at the time that I was injecting, she […] she felt bad. “oh, you have to do this?”. But for me, I have already accepted it. But people do feel, like even my own family, and others, they have […] when it’s insulin, it has moved towards difficult […] that type of feeling is there. (N020, 53Y/M)
There was also mention of the “secrecy” surrounding insulin use. Diabetes was considered a “big” issue, and people preferred keeping silent about using insulin for diabetes.
In villages diabetes is considered a big issue! Let’s say, people don’t think that “diabetes is normal, it’s like this”. Because of that they don’t talk a lot about diabetes. And about insulin they prefer not to talk at all. In villages no one says that he is using insulin. (N005, 47Y/M)
Participants considered using insulin in front of other people as inconvenient, and stated that people sometimes associated needles, and injection use with illicit drug use. This negative perception of, and stigma associated with, insulin use was perceived as a reason for unavailability of insulin in some areas of Nepal.
Despite general reluctance, it was interesting to note that participants who were actually using insulin as part of their regimen appeared satisfied with daily insulin usage. Physicians’ advice and assurance significantly helped reduce fears associated with insulin and helped participants accept and integrate insulin into their everyday life. Moreover, availability of the insulin pen made insulin use more convenient.
Perceptions of alternative strategies for diabetes management
Most of the respondents, both in Nepal and in Australia, appeared willing to try anything that would reduce blood glucose level and had no side effects. The alternative strategies used for diabetes management varied from use of traditional home remedies (such as specific vegetables and spices) to herbs/herbal products, “Ayurvedic” medications, to finding other complementary and health care approaches (such as Ceragem therapy- a Korean therapy where patient is treated using an equipment that uses infrared light technology).
If I find anything that would help reduce diabetes, does not have any side effect, I would never avoid them. When they say it does not have any side effects and help reduce diabetes, then it is fine. Even if it does not work, then it does not matter. (A002, 56Y/M)
Such alternative strategies had more appeal than the conventional medications because unlike conventional medications, “natural” strategies were perceived as safe and devoid of long-term harm, and also that they could be ceased at any time without consequences.
Herbal product is natural. Medication, let’s say, is something else. If anything will be okay with a natural process then why go to medications? I had that kind of thought. (A017, 40Y/M)
Anything bitter was considered better for diabetes; the bitterness was believed to combat the “sweetness” in blood. A few also felt that such (bitter) remedies helped to counteract the effect of negligent eating. Some of the examples of bitter provided were fenugreek powder/paste, bitter gourd and its juice, jasmine flowers, and soaked bitter herbs, such as Chirayata (Herb, Swertia chirata). Almost all participants shared that they had used at least one of these alternatives for a short or a long period, particularly the home remedies, and the use of bitter were popular.
Although actively exploring and trying herbs/herbal products and Ayurvedic medicines was common for participants residing in Nepal, the Nepalese in Australia reported they had limited access to such herbs and medicines, or they were expensive. They tended to use home remedies (along with their medications). For example, participants reported eating cinnamon and drinking water in which okra was soaked overnight. A few had their supplies of Ayurvedic medicines ordered from Nepal and herbal products ordered online from the United States.
A few participants in Nepal, however, held reservations about the safety of bitter products. They perceived that “bitter” would harm kidneys, or bring greater reduction in blood glucose resulting in hypoglycemia.
They say to take Neem [Margosa] […] I haven’t taken Neem, but fenugreek does control [blood sugar] […] they said it [Neem] might attack the kidney. (N011, 66Y/F)
If it’s too high, fenugreek controls […] bitter gourd controls; do not eat more bitter gourd, when it lowers, it also lowers very much. If there is a slight increase [in blood sugar], once in a month take it weekly […] that too eat with rice […] because bitter gourd will keep on decreasing and rice will keep on increasing […] then there will be balance. (N011, 66Y/F)
A few others also perceived that Ayurvedic medications were not effective once the disease had progressed or once conventional medications were started. Overall, participants’ desire and use of natural treatments were influenced by indigenous knowledge rather than a specific recommendation from a health care professional.
Perceived problems, concerns, and difficulties with antidiabetic medication
[I] wished, I would not have to take [the medicines], and I had to [take them]! That is the biggest worry [laughs] (A015, 63Y/F).
Although expressed in good humor, the above quote is representative of how participants generally felt about their antidiabetic medications. The need to take medications each day made people sad. Chronic lifelong use and potential long-term adverse effects were commonly reported concerns. Except one participant who suspected that his fatty liver disease was a side effect of his antidiabetic medication, none of the others reported any incidences of side effects, or any concerns about experiencing side effects.
Although antidiabetic medications were considered to be expensive by some participants, and “not so” expensive by others, cost of medications was acknowledged as a concern, particularly by those living in Nepal. The necessity to take the medications for life added to the already existing economic burden patients faced in their life and impacted initiation of therapy. A notable observation was the concern expressed about the continuing financial impact of medication use, persisting with medications and the potential adverse effects of diabetes.
A few, mostly housewives and older participants in Nepal, who were financially dependent on their family members were not aware exactly how much was being paid for their medications. For participants with a permanent resident status interviewed in Australia, the cost of antidiabetic medications was not a serious concern, as they were entitled to pharmaceutical benefits offered by the Australian Government and therefore the cost of their medications was subsidized.
While recognizing that carrying medications with them was necessary to avoid missing medications, the need to take medications with them on different occasions, for example, during a social function, during travel, or while on holidays, was reported as a major difficulty of medication taking. Impact of missing medications was reported as a concern.
Long-term […] till how long will you keep on taking the medications? Sometimes, in case you miss, whether you would fall (unconscious) […] that risky point is there (as a concern) […] that’s why every time you have to be careful about your medications. (N030, 64Y/M)
Insulin usage also presented challenges for the participants in Nepal. These included the high cost, inconvenience in taking insulin when traveling, storage requirements, rotating the place of injection, and, in one case, finding a person who could inject the insulin. Insulin was reported as more expensive than OHAs and often out of stock in rural areas. Refrigeration requirements added further complexity to the problem of insulin transport.
Discussion
Our study revealed that participants’ perceptions of diabetes treatment modalities were mostly similar among Nepalese participants living in Sydney and in Kathmandu. Overall, the participants had a strong reluctance toward taking conventional antidiabetic medications, including insulin, for diabetes management. Even though they believed in the effectiveness of the medications, the participants demonstrated a greater preference for utilizing “natural” methods (lifestyle modifications and natural medications) to manage their diabetes. When on medication, participants resisted any type of therapy escalation, including changing from OHAs to insulin.
“Considerable reluctance to take medicine and a preference to take as little as possible” have also been reported in other patients who suffer from chronic diseases.20 Patients’ perceptions toward their medications may be shaped and influenced by several factors, including the disease and the nature of treatment.10 As diabetes is an incurable disease that progresses with time, chronic medication use becomes a key aspect of diabetes management. The concern that, once started, the medications could not be ceased and had to be continued for life was one of the major reasons for reluctance to using conventional medications for diabetes treatment and for continued concern about therapy observed in this study. Adverse effects from medications have been recognized as a significant factor that impacts how patients assess their medications.21 Nepalese study participants’ apprehension toward pharmacotherapy was not related to the “side effects” per se but to the anticipated long-term harm from medications. Participants preferred a more natural way of treatment. They perceived “natural” as “safe” and that natural medications, unlike conventional medications, could be discontinued without harm. Previous studies have also documented patients’ dislike for prescribed medications and their preference for and use of natural remedies for diabetes.22,23
Besides the “natural is safe” myth, participants’ inclination toward “natural/traditional medications” in this population can also be associated with the traditional healing culture of Nepal. Traditional healing methods such as Ayurvedic medicines and herbal remedies are inherent to Nepal and have been an integral part of health development in the country.15 Although people have assimilated the new/modern medicines/therapy, there is a juxtaposition of the modern with the traditional methods. Ironically, however, the use of natural remedies does not seem to be guided by “professional knowledge” but rather by “indigenous knowledge”. “Traditional” methods in case of diabetes management appear to be used to escape the anticipated consequences from the “conventional” methods. In addition to the “self-guided” use of Ayurvedic medications, herbs, and home remedies, the fear/reluctance toward conventional medications has also made the respondents susceptible to any product and services claiming to lower blood glucose level. Participants appeared keen to try anything that might help and had no “side effect”. While the right product/service may be beneficial in such cases, this has exposed the people, particularly in Nepal, to the risk of unauthorized and unauthentic products/services. It is, therefore, important that the practice of natural therapy is made on the advice of professional experts, and their effects and interactions with the conventional medications are carefully contemplated. This study identified that the need to guide patients about the use and effectiveness of such natural medications and herbs in the treatment of diabetes is of prime importance in the Nepalese population.
Australian participants’ faith in Nepalese traditional medicines demonstrated the deep-rooted historical and cultural beliefs in this group of participants. However, participants in Australia had limited access to traditional Nepalese medications/herbs. Thus, despite their preference and faith in natural medications, they appeared less focused on traditional medication use than the participants in Nepal. The participants in Australia, unlike those in Nepal, are therefore less vulnerable to the negative consequences (if any) of such natural medications/services.
Insulin was regarded as an inconvenience and most importantly the “ultimate” treatment option for diabetes, and participants were therefore more reluctant to use insulin. Insulin has been associated with chronicity of diabetes.24 As insulin in most cases is started at the later stages of diabetes treatment, and often in the setting of the failure of adequate blood glucose control by OHAs, it is not surprising that participants connected insulin with uncontrolled blood glucose and/or deteriorating diabetes. Any type of therapy escalation process, for example, increase in doses of the OHAs, or addition of a new oral medication, signaled inability of blood glucose control with the existing measures and a step closer to insulin therapy. Hence, participants hesitated and sought ways to avoid any therapy escalation, particularly moving from OHAs to insulin. As diabetes is not typically related to physical discomfort and is generally symptomless, people may often find it hard to appreciate the need for therapy escalation and/or insulin, if they are not aware that diabetes is a progressive disease. That people fail to understand the need for insulin and seek ways to control blood glucose level without insulin has been previously reported.25,26
It was interesting to note, however, that despite their trepidation toward conventional medications (both OHAs and insulin), participants ultimately commenced the prescribed conventional medications, based on the suggestions of their doctors. The balance between experiencing possible complications of diabetes if untreated with medications, lifelong need, and anticipated long-term harm from the medications was like being “between a rock and a hard place”. Most participants, therefore, can be classified as “passive adopters” of medications. Despite their unwillingness, it was noteworthy observing that once started, the participants did not perceive it very difficult to adapt to antidiabetic medications, including insulin therapy. In addition to improved understanding gained from counseling by health care providers that facilitated acceptance of overall antidiabetic therapy, participants’ actual experiences with insulin use and the introduction and availability of insulin pen have helped greatly in insulin acceptance and incorporation into a daily schedule.
Educating patients about diabetes, its impact, and significance of each treatment modality could help in reducing the concern about conventional pharmacotherapy. This may assist in facilitating acceptance of conventional pharmacotherapy. Furthermore, gauging and addressing these emotional and cognitive factors during care of a patient are essential to effectively address and improve diabetes management and medication taking.
Participants’ interpretation of effectiveness of different treatment methods was based on their experiences. While most had faith in conventional medications, confusion prevailed in those who did not see the desired control, despite adhering to medications. Such experiences led the patients to question their own beliefs in medications and the significance of taking medications every day. Participants weighed the effect of nonpharmacological and pharmacological treatment modes based on experiences and made their own decisions about which was more effective and important for the control of blood glucose level. Understanding gained from such experience, combined with patients’ preference for natural therapies (including lifestyle management) over conventional medications for diabetes control, could have an impact on patients’ behavior involving different treatment modalities. The variance in patients’ adherence to different approaches to diabetes management has been previously reported.27 It is therefore important to gain a better understanding of how perceptions impact medication-taking behavior.
Participants, particularly in Nepal, reported the high cost as the major concern with antidiabetic medications. Medications for chronic diseases such as diabetes can impose a huge financial burden to individuals.5 High cost has also been identified as a barrier for medication adherence.28,29 Unlike health care in Australia, the health system in Nepal faces numerous challenges, including inadequate budget allocation for health, a lack of an insurance system, and poor infrastructure.30 In Nepal, people are liable to bear the health care cost mostly by themselves. The need for lifelong consumption of medications can therefore be an economic burden. The anticipated financial impact could be speculated as a reason for reluctance to commence therapy, particularly in patients with low socioeconomic status. While in Australia, the medications were subsidized for permanent residents, and for them the high cost was not a major concern. Australian residents are entitled to Medicare services under which they receive free or subsidized medical and health services.31 However, participants reported their struggle with finances while on a temporary visa, as they were not eligible for Medicare. Therefore, in Nepal it is recommended that health care service reforms be implemented. The provision of low-cost (if not free) health care and medication services might improve medication use and outcomes for chronic illnesses such as diabetes. A recent review looking at how different payment schemes affected medication adherence reported that not only the amount of money spent for medications but also the perceived financial burden of medications could influence adherence.32 Thus, patients’ concerns relating to the cost of medications need to be carefully gauged, and their possible impact on adherence assessed.
Limitations of the study
There are some limitations to this study. First, the study was qualitative; therefore the findings are not generalizable, and are not intended to be generalizable. Second, in Nepal, participants were interviewed only in Kathmandu. Considering the cultural and ethnic diversity of Nepal, there can be substantial differences in perceptions and attitudes to treatment between participants coming from different regions of the country. In addition a large segment of Nepal is rural. The findings, therefore, may not be representative of the rural context. However, participants from different parts of the country were included and interviewed in Kathmandu. Finally, the interviews were conducted in Nepali language, and all the quotes presented in this paper are the translated versions, where the translator has retained as much of the cultural context as possible.
Conclusion
Overall perceptions of diabetes treatment were not very different between Nepalese participants in Australia and in Nepal. Despite variations in individual perceptions of the effectiveness of lifestyle treatment methods and therapeutic management, participants in general were more willing to adopt lifestyle modifications than to use medications for blood glucose control. The reported reluctance to use conventional medications and preference for natural methods of treatment were primarily due to perceptions that conventional medications, once started, “have to be taken for life”, and that these medications have a long-term negative impact on the body.
Patients’ preference for a natural means of diabetes management, and belief that “natural is safe”, may drive some patients toward any kind of products/services claiming to be “natural” and “beneficial” for diabetes. This phenomenon could expose patients, particularly in Nepal, to the risk of unauthorized/unauthentic products and services and to the consequences of uncontrolled diabetes. Health care professionals involved in care of Nepalese T2D patients therefore need to be vigilant about patients’ perceptions of pharmacotherapy and their preferred choices of treatment for diabetes as this could be a possible predictor of patients’ behavior with prescribed treatment.
Increased patient awareness and understanding of the importance of pharmacotherapy for diabetes management are vital to achieve the desired health outcomes with their treatment. It is important to guide Nepalese patients on the effectiveness and suitability of “natural” and alternative methods for diabetes treatment. Addressing existing individual and social (mis)conceptions about diabetes and diabetes treatment methods is key in the Nepalese population.
Acknowledgments
The authors acknowledge the participation of all participants in the study. The authors are also thankful to all members of the Nepali community in Sydney for their valuable guidance and assistance in helping them locate the volunteers for the research. They also thank the owners of the Nepalese grocery shops and Nepalese restaurants around Sydney for helping them advertise the project. Furthermore, the authors express their gratitude toward the members of the health institutions, pharmacies, friends, and family in Nepal for helping them advertise the project.
SS was supported by the Australia Awards Scholarship from the Australian Government for her PhD.
Disclosure
The authors report no conflicts of interest in this work.
References
Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94(3):311–321. | ||
Hu FB. Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care. 2011;34(6):1249–1257. | ||
Bhattarai MD, Singh DL. Learning the lessons – preventing type 2 diabetes in Nepal. Diabetes Voice. 2007;52(2):9–11. | ||
Bhandari GP, Angdembe MR, Dhimal M, Neupane S, Bhusal C. State of non-communicable diseases in Nepal. BMC Public Health. 2014;14(1):23. | ||
Inzucchi SE, Bergenstal RM, Buse JB, et al; American Diabetes Association (ADA); European Association for the Study of Diabetes (EASD). Management of hyperglycemia in type 2 diabetes: a patient-centered approach position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35(6):1364–1379. | ||
Rhee MK, Slocum W, Ziemer DC, et al. Patient adherence improves glycemic control. Diabetes Educ. 2005;31(2):240–250. | ||
Odegan J. Health Psychology: A Textbook. 5th edition. Philadelphia: McGraw- Hill Education (UK); 2012. ISBN 0335243843. | ||
Chinenye S, Ogbera AO. Socio-cultural aspects of diabetes mellitus in Nigeria. J Soc Health Diabetes. 2013;1(1):15–21. | ||
Davies M. Psychological aspects of diabetes management. Medicine. 2010;38(11):607–609. | ||
Sachdeva S, Khalique N, Ansari MA, Khan Z, Mishra SK, Sharma G. Cultural determinants: addressing barriers to holistic diabetes care. J Soc Health Diabetes. 2015;3(1):33–38. | ||
Huang ES, Brown SE, Thakur N, et al. Racial/ethnic differences in concerns about current and future medications among patients with type 2 diabetes. Diabetes Care. 2009;32(2):311–316. | ||
Subedi M. Illness causation and interpretation in a Newar town. Dhaulagiri Journal of Sociology and Anthropology. 2012;5: 101–120. | ||
Wasti SP, Randall J, Simkhada P, van Teijlingen E. In what way do Nepalese cultural factors affect adherence to antiretroviral treatment in Nepal? Health Sci J. 2011;5(1):37–47. | ||
Sermrittirong S, Van Brakel WH. Stigma in leprosy: concepts, causes and determinants. Lepr Rev. 2014;85(1):36–47. | ||
Shankar PR, Paudel R, Giri BR. Healing traditions in Nepal. J Am Assoc Integr Med. (Online) 2006. Available from: http://www.aaimedicine.com/jaaim/sep06/Healing.pdf. Accessed February 19, 2016. | ||
Rajbhandari KC. Epilepsy in Nepal. Can J Neurol Sci. 2004;31(2): 257–260. | ||
Merriam SB, Tisdell EJ. Qualitative Research: A Guide to Design and Implementation. 4th ed. Hoboken: Wiley; 2015. | ||
Mason M. Sample Size and Saturation in PhD Studies Using Qualitative Interviews. Forum Qualitative Sozialforschung/Forum: Qualitative Social Research; 2010. ISSN-1438-5627. Available at: http://www.qualitative-research.net/index.php/fqs/article/view/1428/3027. Accessed January 9, 2016. | ||
Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–115. | ||
Pound P, Britten N, Morgan M, et al. Resisting medicines: a synthesis of qualitative studies of medicine taking. Soc Sci Med. 2005;61(1):133–155. | ||
Hauber AB, Mohamed AF, Johnson FR, Falvey H. Treatment preferences and medication adherence of people with Type 2 diabetes using oral glucose-lowering agents. Diabet Med. 2009;26(4):416–424. | ||
Nair KM, Levine MA, Lohfeld LH, Gerstein HC. “I take what I think works for me”: a qualitative study to explore patient perception of diabetes treatment benefits and risks. Can J Clin Pharmacol. 2007;14(2):e251–e259. | ||
Modak M, Dixit P, Londhe J, Ghaskadbi S, Devasagayam TP. Indian herbs and herbal drugs used for the treatment of diabetes. J Clin Biochem Nutr. 2007;40(3):163–173. | ||
Snoek FJ, Skinner TC. Psychological aspects of diabetes management. Medicine. 2006;34(2):61–62. | ||
Haque M, Emerson SH, Dennison CR, Navsa M, Levitt NS. Barriers to initiating insulin therapy in patients with type 2 diabetes mellitus in public-sector primary health care centres in Cape Town. S Afr Med J. 2005;95(10):798–802. | ||
Ng CJ, Lai PS, Lee YK, Azmi SA, Teo CH. Barriers and facilitators to starting insulin in patients with type 2 diabetes: a systematic review. Int J Clin Pract. 2015;69(10):1050–1070. | ||
Krass I, Schieback P, Dhippayom T. Adherence to diabetes medication: a systematic review. Diabet Med. 2015;32(6):725–737. | ||
Awah PK, Unwin N, Phillimore P. Cure or control: complying with biomedical regime of diabetes in Cameroon. BMC Health Serv Res. 2008;8(1):43. | ||
Tiv M, Viel JF, Mauny F, et al. Medication adherence in type 2 diabetes: the ENTRED study 2007, a French population-based study. PLoS One. 2012;7(3):e32412. | ||
Mishra SR, Khanal P, Karki DK, Kallestrup P, Enemark U. National health insurance policy in Nepal: challenges for implementation. Glob Health Action. 2015;8. doi: 10.3402/gha.v8.28763. | ||
Department of Human Services AG. Medicare services. Available from: https://www.humanservices.gov.au/customer/subjects/medicare-services. Accessed February 22, 2016. | ||
Aziz H, Hatah E, Makmor Bakry M, Islahudin F. How payment scheme affects patients’ adherence to medications? A systematic review. Patient Prefer Adherence. 2016;10:837–850. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
