Back to Journals » International Medical Case Reports Journal » Volume 16
Neonatal Spontaneous Bilateral Posterior Fossa Chronic Subdural Hematoma and Obstructive Hydrocephalus with a Successful Outcome: A Case Report
Authors Bergene E , Tira AE , Hussen E , Smith CJ, Fetle YT
Received 14 April 2023
Accepted for publication 3 June 2023
Published 8 June 2023 Volume 2023:16 Pages 351—355
DOI https://doi.org/10.2147/IMCRJ.S413163
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Eyerusalem Bergene,1 Abdi Ermolo Tira,2 Endris Hussen,1 Caitlyn J Smith,3 Yonas T Fetle4
1Department of Neurosurgery, St. Paul’s Millennium Medical College, Addis Ababa, Ethiopia; 2Department of Neurosurgery, St. Peter’s Comprehensive Specialized Hospital, Addis Ababa, Ethiopia; 3Department of Neurosurgery, University of Missouri School of Medicine, Columbia, MO, USA; 4Department of Neurosurgery, Addis Ababa University College of Health Science, Addis Ababa, Ethiopia
Correspondence: Eyerusalem Bergene, Email [email protected]
Background: Chronic supratentorial subdural hematoma is uncommon in neonates but accounts for most neurosurgical procedures in neonatal age. However, its occurrence in the posterior fossa is extremely rare. It can be caused by instrumental delivery, coagulation abnormality, hypoxic insult, and various structural abnormalities. Furthermore, spontaneous onset has been reported only in a few case reports.
Case Presentation: A twenty-nine-day-old male neonate presented with failure to suck for three days duration associated with vomiting. Imaging showed bilateral posterior fossa chronic subdural hematoma and obstructive hydrocephalus. Bilateral burrhole craniostomy and hematoma evacuation was done which resulted in an excellent outcome.
Conclusion: Posterior fossa chronic subdural hematoma is extremely rare in the neonatal period. It can be caused by various possible etiologic agents; however, rarely it can occur spontaneously. Management with suboccipital burrhole craniostomy and hematoma evacuation can result in a good outcome. Intraoperative monitoring and management with an experienced anesthesiology team are indispensable for a good outcome.
Study Setting: Pediatrics neurosurgery ward, St Peter’s Comprehensive Specialized Hospital, Addis Ababa, Ethiopia.
Keywords: posterior fossa, chronic, subdural hematoma, neonate
Introduction
Symptomatic posterior fossa subdural hematoma (PFSDH) in term neonates is a rare condition with a reported incidence of 0.3 per 100,000 live births. There are less than 100 cases described in the literature.1 Chronic PFSDH at this age is an even rarer disease entity, reported in only two cases2,3 (Table 1). Neonates can present either with an acute presentation in the first few hours of life with brain stem dysfunction from compression or delayed presentation with signs of hydrocephalus.1,4,5 Breech presentation, prolonged delivery, instrumentation with forceps or vacuum, primiparity, and extreme multiparity are the most frequent factors associated.6,7 The option of management can be conservative, burrhole craniostomy, or suboccipital craniectomy based on the clinical presentation.
 |
Table 1 Previous Cases with Posterior Fossa Chronic Subdural Hematoma in Neonatal Age |
Case Presentation
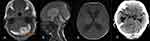
A 3050-g full-term male neonate was born after an uncomplicated pregnancy to a 20-year-old primiparous woman at a gestational age of 39 weeks. The pregnancy was uncomplicated. The labor was not prolonged with uneventful spontaneous vaginal delivery. Apgar scores were 8 and 9 at 1 min and 5 min, respectively, with a normal grimacing response score of 2. His Apgar remained to be 9 at 10 and 20 minutes. He was alert with a good cry, pink color, a pulse rate of 134 and respiratory rate of 56. He was given vitamin K at birth. He presented to our hospital with failure to suck for three days at age of 29 days. The family also stated that he had intermittent vomiting since birth. Otherwise, there was no history of bleeding diathesis, fever, neck stiffness, or seizure. At presentation, he had a bulging anterior fontanelle. Moro was incomplete; sucking was not sustained but good muscle tone was noted in all extremities. His complete blood count (CBC) and coagulation profile were normal. Brain MRI (Figure 1A–C) showed bilateral cerebellar convexity T1WI and T2WI hyperintense hematoma measuring 2cm with supracerebellar and periaqueductal extension. Furthermore, obliteration of the fourth ventricle and dilation of the third and lateral ventricles was also noted. Under general anesthesia, the patient was placed in a prone position utilizing a midline skin incision, bilateral burrhole craniostomy was done. After the dura was opened in a cruciate incision, a well-defined thick membrane; with dark hemolyzed blood came out with pressure. Intraoperatively, the patient had a cardiac arrest for which one cycle of cardiopulmonary resuscitation (CPR) was done and a return of spontaneous circulation was achieved. Afterward, the skin was closed subdural drain was placed and the patient was extubated and transferred to the intensive care unit (ICU). Control CT scan (Figure 1D) done on 3rd post-op day showed complete evacuation of the hematoma and improvement of the hydrocephalus. The patient was discharged on the 7th post-op day improved. The first-month post-op follow-up was uneventful with normal developmental milestones achieved for his age.
Discussion
Posterior fossa subdural hematoma in neonates is an infrequent neurosurgical emergency that is usually caused by trauma, coagulation disorder, hypoxia, and structural abnormalities.6 Frequently associated risk factors in the literature are breech presentation, prolonged delivery, instrumentation with forceps or vacuum, primiparity, or extreme multiparity.6,7 Our patient was a term neonate, born from primiparous by a spontaneous vaginal delivery.
The proposed mechanism that is inferred from cases with instrumental delivery is that: distortion of the neonate’s cranium by forceps, vacuum extraction, or natural delivery results in disruption of the falx and angulation of the tentorium. This causes posterior fossa bridging vein avulsion which results in posterior fossa hemispheric or vermian subdural hematoma.4,6,7 The rate of hemorrhage can be massive enough to cause acute SDH or slow accumulation of blood from tear of tentorial leaflets and can present as a chronic subdural hematoma.3 The second mechanism proposes occipital osteodiastasis, which; usually occurs in the aftercoming head during breech delivery, causes cerebellar hemisphere laceration and subsequent intracerebral or subdural hematoma. Furthermore, massive posterior fossa hematoma can be caused by dural sinus laceration and rupture of the vein of Galen.3,4,7
The first neonatal posterior fossa reported in the literature in which the neonates survived after management was described by Coblentz in 1940 and Nelson in 1959.8,9 Since this first report, the outcome and accuracy of diagnosis have significantly improved with the advent of CT and MRI. Diagnosis can easily be established rapidly by CT using coronal and sagittal plane images. In neonates, it was reported that coronal ultrasonography can be highly diagnostic. In addition, it can detect hydrocephalus and allows close monitoring of ventricular size. However, the relative inaccessibility of the posterior fossa may produce many false-negative results. The recent reports illustrate the potential of MRI in neonatal PFSDHs as a modality of choice. The anatomy of the posterior fossa can be delineated better by an MRI. Particularly, sagittal images are helpful to localize bleeding relative to the tentorium and show the degree of brainstem compression as well as the aqueduct compromise and size estimation of the bleed.4,5,10
Depending on the amount and rapidity the bleeding neonates with posterior fossa subdural hematoma can present in different ways. Acute presentation from brainstem dysfunction or delayed presentation with signs and symptoms of hydrocephalus are the major clinical findings.1,4,11 Clinical findings of PFSDHs can be nonspecific mimicking or coexisting with neonatal hypoxic-ischemic encephalopathy. In these patients, early screening trans-fontanelle ultrasound is required.12 The patient in our report had a delayed presentation with clinical manifestation of hydrocephalus.
Conservative management with close follow-up can be an option of management in neonates with small PFSDHs that are not causing brain stem compression or obstructing the CSF outflow pathway. However, neonates with hematoma thickness >15mm; signs of progressive brainstem compression such as apnea, bradycardia, and hypotension; and acute obstructive hydrocephalus should promptly get an operative intervention.1,4,5,13
Clinically significant PFSDHs can be managed utilizing several different types of neurosurgical procedures. These include subdural taps of the posterior fossa clot through the lambdoid suture and squamous portion of the occipital bone, occipital burr holes and PFSDH drainage, insertion of an external ventricular drain for obstructive hydrocephalus, and posterior fossa craniectomy and clot evacuation.2–4 The management option preferred for our patient was a bilateral burrhole without an extra ventricular drain. In the literature, despite the presence of large clots and fourth ventricular obstruction, the requirement for CSF shunting in PFSDHs ranges from 30% to 50%.4,14 Biphasic dilation of the ventricles with initial dilation from the PFSDHs and normal ventricles after hematoma evacuation followed by the development of secondary communication hydrocephalus has been reported.14 Our patient remains shunt-free after three months post-op.
The operating surgeon needs to be cognizant of neonatal vascular posterior fossa dura, friable and soft cerebellum, and limited blood volume. The expertise of a skilled pediatric neuro-anesthesiologist is invaluable in cases with vigorous bleeding because successful evacuation will result in rapid regain of normal brain stem function. Therefore, neonates can be extubated shortly and get discharged from the hospital within a few days with extremely gratifying recovery even in these potentially fatal cases.3,4,12
Evidence of the long-term outcomes of neonates with PFSDH is scarce, and outcomes vary across case series.1,4,5 According to Perrin et al case series, severely affected neonates had supratentorial parenchymal injuries in addition to their PFSDHs, indicating a more severe degree of brain damage.1
Limitation and Strength
The follow up for the neonate is short term and therefore it can only conclude on short-term outcome. However, it showcases posterior fossa chronic subdural hematoma can be managed with suboccipital burrhole and hematoma evacuation without CSF diversion procedures.
Conclusion
Posterior fossa spontaneous chronic subdural hematoma in a neonate is extremely rare. It can present with brainstem and fourth ventricle compression in a delayed manner. With burrhole and hematoma evacuation alone, excellent results can still be achieved without extra ventricular drain placement even in the presence of hydrocephalus. An experienced pediatric neuro anesthesiology team is essential for intraoperative monitoring and management.
Abbreviations
CBC, Complete blood count; CPR, Cardiopulmonary resuscitation; CSF, Cerebrospinal fluid; CT, Computerized tomography; ICU, Intensive care unit; MRI, Magnetic resonance imagining; PFSDH, Posterior fossa subdural hematoma; SDH, Subdural hematoma.
Patient Consent
Written consent for publication was obtained from the neonate’s mother. We have also received approval for publication from the hospital where the patient was managed.
Disclosure
The authors report no conflicts of interest in this case report.
References
1. Sreedhara MS, Ninan B, Prakash A, Visvanathan K, Shekhar R, Devi RU. First case report of spontaneous posterior fossa subdural hemorrhage – a rare cause of neonatal encephalopathy. J Clin Neurosci. 2019;67:277–279. doi:10.1016/j.jocn.2019.05.047
2. Rousslang LK, Rooks EA, Meldrum JT, Hooten KG, Wood JR. Neonatal infratentorial subdural hematoma contributing to obstructive hydrocephalus in the setting of therapeutic cooling: a case report. World J Radiol. 2021;13(9):307. doi:10.4329/wjr.v13.i9.307
3. Franklin J, Belkin R, Howieson J, Gallo A. Posterior fossa chronic subdural hematoma in the neonate. Am J Neuroradiol. 1986;7(6):1099.
4. Perrin RG, Rutka JT, Drake JM, et al. Management and outcomes of posterior fossa subdural hematomas in neonates. Neurosurgery. 1997;40(6):1190–1200. doi:10.1097/00006123-199706000-00016
5. Blauwblomme T, Garnett M, Vergnaud E, et al. The management of birth-related posterior fossa hematomas in neonates. Neurosurgery. 2013;72(5):755–762. doi:10.1227/NEU.0b013e318286fc3a
6. Usul H, Karaarslan G, Çakir E, Kuzeyl K, Baykal S. Conservative management of spontaneous posterior fossa subdural hematoma in a neonate. J Clin Neurosci. 2005;12(2):196–198. doi:10.1016/j.jocn.2004.03.034
7. Menezes AH, Smith DE, Bell WE. Posterior fossa hemorrhage in the term neonate. Neurosurgery. 1983;13(4):452–456. doi:10.1227/00006123-198310000-00021
8. Reigh EE, Nelson M. Posterior-fossa subdural hematoma with secondary hydrocephalus: report of case and review of the literature. J Neurosurg. 1962;19(4):346–348. doi:10.3171/jns.1962.19.4.0346
9. Hernansanz J, Muñoz F, Rodríguez D, Soler C, Principe C. Subdural hematomas of the posterior fossa in normal-weight newborns: report of two cases. J Neurosurg. 1984;61(5):972–974. doi:10.3171/jns.1984.61.5.0972
10. Koch TK, Jahnke SE, Edwards MS, Davis SL. Posterior fossa hemorrhage in term newborns. Pediatr Neurol. 1985;1(2):96–99. doi:10.1016/0887-8994(85)90043-8
11. Hayashi T, Hashimoto T, Fukuda S, Ohshima Y, Moritaka K. Neonatal subdural hematoma secondary to birth injury. Childs Nerv Syst. 1987;3(1):23–29. doi:10.1007/BF00707189
12. Henzi BC, Wagner B, Verma RK, Bigi S. Perinatal infratentorial haemorrhage: a rare but possibly life-threatening condition. Case Rep. 2017;2017:bcr–2017. doi:10.1136/bcr-2017-221144
13. Scotti G, Flodmark O, Harwood-Nash DC, Humphries RP. Posterior fossa hemorrhages in the newborn. J Comput Assist Tomogr. 1981;5(1):68–72. doi:10.1097/00004728-198102000-00013
14. Tanaka Y, Sakamoto K, Kobayashi S, Kobayashi N, Muraoka S. Biphasic ventricular dilatation following posterior fossa subdural hematoma in the full-term neonate. J Neurosurg. 1988;68(2):211–216. doi:10.3171/jns.1988.68.2.0211
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.