Back to Journals » Clinical Ophthalmology » Volume 14
Near Vision Spectacle Coverage and Associated Factors Among Adults Living in Finote Selam Town, Northwest Ethiopia: Community-Based Cross-Sectional Study
Authors Fekadu S , Assem A , Mengistu Y
Received 21 August 2020
Accepted for publication 22 September 2020
Published 7 October 2020 Volume 2020:14 Pages 3121—3130
DOI https://doi.org/10.2147/OPTH.S278262
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Sofonias Fekadu,1 Abel Assem,1 Yitayeh Mengistu2
1Department of Optometry, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia; 2Department of Physiology, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Sofonias Fekadu Email [email protected]
Background: Near visual impairment leads to difficulty with near tasks at a working distance (40 centimeters) when near visual acuity is 6/12 (N8) or worse. High cost is the main barrier reported for low near vision spectacle coverage.
Objective: This study aimed to determine near vision spectacle coverage and associated factors among adults living in Finote Selam town, Northwest Ethiopia.
Methods: A community-based, cross-sectional study was applied from June 3 to 25, 2019. A total of 565 study participants aged ≥ 35 years were recruited using a systematic random sampling technique. A pre-tested questionnaire with adequate physical examination was used for data collection. The data were entered into EPI INFO software and exported to a statistical package for science for analysis. Mean (standard), frequencies, tables, and figures were used to present descriptive statistics. A bi-variable and multivariable logistic regression was used to determine the association between independent variables and outcome variable with a P-value of less than 0.20 and a P-value of less than 0.05, respectively. Odds ratios and a 95% confidence interval were used to show strength of association.
Results: A total of 549 adults participated, with a response rate of 97.20% and a mean age of 46.4± 8.7 years. The near vision spectacle coverage was 156 (28.42%; 95% CI=24.65– 32.31). Higher education level (AOR=2.8; 95% CI=1.21– 5.21), history of eye examination (AOR=2.40; 95% CI=1.51– 3.81), awareness about near vision problems (AOR=2.12; 95% CI=1.41– 3.24), and need of a high plus lens (AOR=4.21; 95% CI=2.41– 7.39) were associated with near vision spectacle coverage.
Conclusion: Near vision spectacle coverage was low among adults living in Finote Selam town. Higher educational level, history of eye examination, awareness about near vision problems, and need of a high plus lens were associated with near vision spectacle coverage.
Keywords: near vision spectacle coverage, near visual impairment, Finote Selam, Ethiopia
Introduction
Near visual impairment (NVI) is defined as difficulty with near tasks at a working distance (40 centimeters) when near visual acuity (NVA) is 6/12 (N8) or worse.1 Presbyopia, which is an age-related reduction in accommodation due to inelasticity of the lens, accounts for most of the causes of near visual impairment in adults.2,3 NVI is said to be correctable when it is possible to have the best-corrected binocular near visual acuity (NVA) greater than 6/12 (N8), and uncorrectable when best-corrected binocular NVA is ≤ 6/12.4 Old age, female sex, educational status, low income, unaware of near vision problem, and absence of eye checkup practice are identified associated factors with near visual impairment.5,6 According to the reports of the World Health Organization (WHO), a total of 2.2 billion people are visually impaired or blind, among which more than 80% were preventable and more than 90% are found in developing countries.7 More than 1.8 billion people are living with presbyopia worldwide and the global unmet need/without spectacle correction is 45%, which indicates that most of the near visual impairment burden is from presbyopia.8 This causes more than 25.4 billion-dollars of economic loss globally.9 More than 50% of those aged greater than 50 years are from developing countries, where lack of awareness and controlling the problem are challenges due to economical constraints and the scarcity of eye care professionals.4,–9–11 A report of the world economic forum indicated that 23% of employees compromised their work due to the effect of NVI and the unavailability of near vision correction.12 The proportion of near visual impairment reaches from 61.7% to 85.4% in East Africa, including Ethiopia.13
A multi-country prospective study done in China, Nepal, India, Niger, South Africa, and the US showed low prevalence of near vision spectacle coverage.14 Near vision spectacle coverage varies from 0.7% in a study done in rural China15 to 99.5% in a study done in the US.2 Most of the governmental and non-governmental work activities are based on near and intermediate working distances which rely on the usage of near corrections. Furthermore, fishing, swing, and preying are potential areas that are expected to benefit from the use of near corrections.16
Uncorrected near visual impairment affects day-to-day activities performed at near/intermediate distances and vision-related quality of lives.2,4,17 Correction of near vision problems is an important positive factor to motivate adult workers, especially in low- and middle-income countries.12 Awareness to burden of near vision problems and economical status of the study areas mainly affects the coverage of near vision correction. High cost is the main barrier reported for low correction coverage (unmet need) for near vision. The average cost for near spectacles (single vision, bifocal, or progressive) in Ghana is $5.8, and in Ethiopia the willingness-to-pay for spectacles is about $17.9.16
A global action plan in 2014–2019 adopted by WHO plans to reduce the burden of visual impairment by 25% by the year 2019 using different approaches and correction mechanisms.18 Most of the near visual impairment is corrected by wearing reading eyeglasses as prescribed by Optometrists/Ophthalmologists.2,10 Besides, monovision contact lenses (one eye for distance and one for near), bifocal and multifocal contact lenses, accommodative intraocular lenses, and refractive surgery were other options of correction mechanisms.11,19
Most studies done in different areas including Ethiopia focused on distance visual impairment, and near visual impairment was reported as presbyopia, though they are not interchangeable, rather presbyopia is a major cause of NVI. There is a paucity of information on near vision spectacle coverage in Ethiopia as a whole and the absence of published studies even showing the proportion of NVI in the study area. Therefore, this study aims to determine near vision spectacle coverage (NVSC) and its associated factors among adults aged 35 years and above living in Finote Selam town Northwest Ethiopia.
Materials and Methods
Study Design, Method, and Setting
A community-based, cross-sectional study was conducted from June 3 to 25, 2019 in Finote Selam town Northwest Ethiopia. The town has 6123 households and six kebeles (smallest administrative unit). It has two hospitals and five private clinics with only a one room ophthalmic clinic in the general hospital.
Study Population, Inclusion and Exclusion Criteria
All adult population aged 35 years and above living in Finote Selam town during the data collection period were the study population and those adults living in the town for at least the last 6 months were included in the study. Adults who were severely ill and unable to communicate were excluded from the study.
Sample Size Determination and Techniques
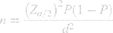
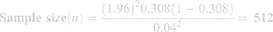
A single population proportion formula was used to calculate the minimum sample size required to carry out this study by taking the proportion from a similar study done in Ethiopia as 30.8%20 and using the assumptions of 95% confidence interval and 4% margin of error.
where; n = sample size,
Z = z statistic at 95% confidence interval = 1.96,
P = Proportion of near vision spectacle coverage among adults = 30.8%, and
d = Maximum allowable error (marginal error) 4% = 0.04.
After considering a 10% non-response rate the final sample size was calculated as 565.
The study participants were selected by using a systematic random sampling procedure after calculating the interval K by dividing the total households in the town to the sample size. Lottery method was used to select the first household that was used as a starting point of the study and every Kth household were included to the study. Study participants were selected with the assumption that each household contains one adult and, in houses which had more than one adult, a lottery method was applied to select one participant per household. Next households were taken when there were no adults aged ≥35 years in the selected households.
Operational Definitions
Near vision spectacle coverage (%) was determined as: 100(the total number of participants with current near vision spectacle)∕(total number of participants with current near vision correction+total number of participants without near vision corrections).
Presbyopia correction coverage (PCC %) was determined as: 100(n with presbyopia need met)/(n with presbyopia need unmet).
Met need includes persons with functional presbyopia and had spectacles that allowed near vision to improve to 20/50 (N8) or better.20
Unmet need includes those with near vision 20/50 (N8) or worse due to functional presbyopia who did not have near-vision corrective spectacles but which can be corrected to N8 or better.
Awareness of near vision problems was defined as having ever heard of age-related near vision problems (presbyopia).5
Alcohol consumption was measured as yes or no. Participants who drinks more than three units of alcohol (a single unit is 300 mL) in day or most days of a week were considered as an alcohol drinker.21
Near visual impairment was defined as difficulty of reading ability at a working distance (40 cm) or uncorrected near visual acuity/habitual near VA of ≤N8 at 40 cm (6/12).1,3,14
Presenting near visual impairment (PNVI) was defined based on the updated International Classification of Diseases ICD 11 as presenting near visual acuity worse than 6/12.3,22
NVI was graded as “mild” when PNVA was less than 6/12 to 6/18 (worse than N8 to N10), “moderate” when PNVA was less than 6/18 to 6/60 (worse than N10 to N18), and “severe” when PNVA was less than 6/60 (worse than N18).5,15
Functional presbyopia was defined as binocular near vision less than N8 (20/50) at 40 cm with presenting distance refractive correction, to achieve a near visual acuity (VA) criterion (≥1 line of acuity improvement N8 print or (20/50)).6,23
Data Collection Instruments and Procedures
The data collection tool was developed after reviewing different works of literature3,4,6,20,23 across the world and adapted accordingly in a way that can measure the study area. The data were collected by eight BSc holder qualified optometrists under two supervisors. Both interobserver and intraobserver agreement were determined between optometrists with respect to visual acuity measurement and refraction. Advanced training was given to data collectors and a pilot study was carried out in a nearby town using similar ophthalmic instruments. First, a face-to-face semi-structured interview was applied using socio-demographic, socio-economic, behavioral, and awareness parts of the questionnaire to know the presence of spectacle coverage and different factors associated with NVI. After completing the interview, physical examination was carried out using distance and near vision charts, torches, trial sets, and streak retinoscopy. The reliability of the questionnaire was assessed by using Cronbach alpha which was 0.78. Initially, the distance unaided presenting visual acuity UPVA (for those who presented with no previous correction) and habitual presenting visual acuity HPVA (for those who presented with previous spectacle correction) were taken to estimate the status of distance vision using a reduced 3 meters illiterate-E chart (tumbling E). Binocular near visual acuity (NVA), both with and without refraction, was measured at 40 cm using a Tumbling E chart under normal room illumination to diagnose the level of NVI. Visual acuity (VA) was recorded as the smallest/last line read with one or no letter miss. Participants with distance presenting/habitual VA of less than 6/12 were refracted using a Retinoscope and near refraction was done on the top of distance correction.15,24 Near refraction was done for all adults whose near visual acuity was ≤N8 using plus lens. Near add was determined by adding plus lenses on the trial frame in a step of +0.25 (+0.25, +0.50, +0.75, and so on) diopters until the participants report “no change” to their near visual acuity at 40 centimeters. Participants whose near vision was corrected to the level of N8 or better were given a formal spectacle prescription and participants with other ocular disorders were referred accordingly.
Data Quality Assurance
The questionnaire was first formatted in English and then translated to local Amharic language and back to English by professional language experts to keep consistency. A pretest was done using 56 (10%) adults in Burie town to measure the coherency, understandability, and cultural acceptance of the questions, and modifications were made accordingly. The data collectors and supervisors were given training for 1 day before data collection. A daily based checkup and correction were done by the supervisors and the principal investigator.
Data Processing and Analysis
After appropriate checking, editing, and coding, the collected data were entered into EPI info version 7 software and exported to statistical package for social sciences (SPSS) for formal analysis. The descriptive statistics were presented using mean (standard deviation), frequencies, percentages, tables, and figures. All variables in a bi-variable logistic regression with a P-value of <0.20 were entered into a multivariable logistic regression to control confounding effect. A P-value of <0.05 in multivariable logistic regression was used to decide statistical significance between independent variables and NVSC. Adjusted odds ratio and 95% confidence level were used to show the strength of association between independent variables and NVSC.
Ethical Issues
Ethical clearance was obtained from the University of Gondar, College of Medicine and Health Sciences ethical review committee in accordance with the Declaration of Helsinki. After stating the objective of the study, formal written informed consent was obtained from each study participant. To maintain the confidentiality, names and other identifiers were not collected. Appropriate advice was given to the participants about the nature of eye problems diagnosed.
Results
Socio-Demographic Characteristics
There were 549 study participants with a response rate of 97.20% and a mean age of 46.4±8.7 years. The majority 296 (53.92%) of the study participants were males and only 145 (26.42%) of the participants were getting a monthly income of ≥142 USD. Most of the participants (451, 82.15%) were married and slightly more than one-third (207, 37.70%) of the participants were in the age group 35–46 years (Table 1).
 |
Table 1 Sociodemographic Characteristics of Study Participants Living in Finote Selam Town Northwest, Ethiopia, 2019 |
Behavioral and Vision-Related Factors
More than half (351, 63.94%) of the participants had no awareness of near vision-related problems/presbyopia and more than two-thirds (382, 69.58%) of the participants had no history of eye examination in the past year. Nearly half (177, 43.17%) of the participants needed from +2.25 Diopters to +2.75 Diopters lenses to correct their near vision and only 81 (14.75%) of them had their distance spectacle correction. The main challenge to wearing near correction was the high cost of spectacles in 232 (42.26%) (Table 2).
 |
Table 2 Behavioral and Vision-Related Characteristics of the Study Participants Living in Finote Selam Town, Northwest, Ethiopia, 2019 |
Near Visual Impairment and Its Spectacle Correction Coverage
The present study confirmed that the overall near vision spectacle coverage among adults living in Finote Selam town was 156 (28.42%;95% CI=24.65–32.31). A total of 432 (78.69%) study participants had NVI. Almost all (410, 94.91%) of the NVI cases were correctable (presbyopia) and 22 (4.76%) of them were non-correctable conditions. Nearly half (220, 50.93%) of the participants had mild NVI, followed by moderate NVI (143, 33.10%) (Figure 1). Furthermore, the “met need” for presbyopia was 156 (38.05%; 95% CI=33.48–42.84).
 |
Figure 1 Degree of visual impairment and its near vision spectacle coverage among study participants living in Finote Selam town, Northwest Ethiopia, 2019. |
Factors Associated with Near Vision Spectacle Coverage
After checking all independent variables in bi-variable logistic regression, those having a P-value of less than 0.20 including sex, age group, monthly income, alcohol drink, educational level, history of an eye examination, awareness of near vision problems, residence, degree of NVI, amount of near addition needed, and presence of distance correction were entered to multivariable logistic regression.
After controlling the effect for confounders in multivariable logistic regression, having a college/university education (AOR=2.8; 95% CI=1.21, 5.21), history of eye checkup/examination (AOR=2.40; 95% CI+1.51–3.81), having awareness about near vision problems (AOR=2.12; 95% CI=1.41–3.24), and need of high plus lens for near correction (AOR=4.21; 95% CI=2.41–7.39) were significantly associated with near vision spectacle coverage with 95% CI and a P-value of less than 0.05 (Table 3).
 |
Table 3 Factors Associated with Near Vision Spectacle Coverage Among Adults Living in Finote Selam Town, Northwest Ethiopia, 2019 |
Discussion
This community-based, cross-sectional study was conducted to determine the near vision spectacle coverage and possible risk factors associated with it among adults living in Finote Selam town, Northwest Ethiopia. The near vision spectacle coverage was found to be 156 (28.42%; 95% CI=24.65–32.31) among adults aged 35 years and above. This result is similar to a study done in India where the near spectacle coverage was reported as 30%.25 This might be due to similarities in the mean age of study participants and the criteria used in the studies. The result of the present study is higher than a similar study conducted in rural China (0.70%).15 The present near vision spectacle coverage is lower as compared with other similar studies reported in Ghana (70.40%),26 North China (51.50%),23 and the US (99.5%).3 This might be due to variations in study setting, study population, and socio-economic conditions between study areas.
The met need for presbyopia was also determined as 156 (38.05%; 95% CI=33.48–42.84) in adults aged 35 years and older in Finote Selam town, which is in line with a study reported in Ghana.6 The met need in this study is higher than studies done in Bahir Dar, Ethiopia (30.8%),20 Ghana (30.4%),26 and India (30.00%).25 On the contrary, this result is lower than studies conducted in Hawassa, Ethiopia,5 and Nigeria,27 which were 48.74% and 63.6%, respectively. This might be due to the differences in the study population because studies done in Hawassa and Nigeria include only school teachers.
Low near vision spectacle coverage in this study is due to high cost of a spectacle lens (232, 42.26%) followed by the unavailability of optical workshops (141, 25.68%). This is supported by a study done in Ethiopia16 and China.15 The possible explanation could be due to optical workshops and eye care centers only being available in big cities, which might contribute to the inaccessibility and low spectacle coverage for those with near vision problems.
This research also identified different factors that were significantly associated with near vision spectacle coverage. Participants who needed a ≥+2.75 Diopter lens for near add were 4.21-times more likely to have near vision spectacle correction as compared to those who needed a +1.00 to +2.00 Diopter lens. This is in agreement with a study done in China.23 The possible explanation could be due to participants who need a high amount of plus lens (near add) having moderate–severe near visual problems that may challenge them to perform their near activities. This might obligate adults to collect glasses to resolve their near vision problems.4
In agreement with studies done in Ethiopia,20 adult participants who had a history of eye checkup were 2.40-times more likely to afford near vision spectacle correction than those who had no eye checkup history. This could be due to those participants who had a history of eye check-up previously might get supporting information and health education for the eye problems including near vision spectacle correction options that could motivate them to collect their spectacle corrections.12
The odds of having near vision spectacle correction were 2.16-times more likely among adults who were aware about near vision problems as compared to others who had no awareness.
Having awareness about near vision problems might lead the participants to search for and read more materials which could in turn encourage them to decide to wear near corrections. Lack of awareness of near vision impairment and place of refraction service was a major factor for uncovered near vision problems.23 Health promotion activities including education might also increase the awareness about spectacle need of adults with near visual impairment.6
Furthermore, in agreement with a study in China,28 participants having college/university education were 2.80-times more likely to have near vision spectacle correction as compared to those having no education. Participants who have a higher level of education could access many sources of information and knowledge about near vision problems29 which might contribute to eye checkup practices including near vision refraction. In addition, educated persons spend most of their time in near work activities, which might obligate them to use near vision spectacles to perform their tasks efficiently, as compared to illiterates.
Limitation
Vital documents, including birth certificates, are not practiced well in Ethiopia. Due to this, the study participants were telling their age by guess. This adds a challenge in the inclusion criteria of study participants. Measuring distance refractive error was also a challenge in ambient light conditions, since it affects the visibility of streak movement of the retinoscope. In addition, some of the questions depend on the participants ability to remember in the previous 12 months, which might create a recall bias to the study.
Conclusion
The near vision spectacle coverage was low among adults living in Finote Selam town. The need of high plus lens (add) for near vision correction, having college/university education, history of eye checkup, and awareness about near visual impairment were identified as significant factors for near vision spectacle coverage.
Abbreviations
AOR, adjusted odds ratios; HPVA, habitual presenting visual acuity; NVA, near visual acuity; NVI, near visual impairment; NVSC, near vision spectacle coverage; PNVA, presenting near visual acuity; UPVA, unaided presenting visual acuity; USD, United States Dollars; VA, visual acuity; WHO, World Health Organization.
Data Sharing Statement
The data will be available upon request from the corresponding author.
Consent for Publication
Not applicable.
Acknowledgment
We would like to acknowledge the West Gojjam health office and Finote Selam town administrative office for their technical support to carry out this study.
Authors’ Information
Sofonias Addis (BSc, MSc, Lecturer of Optometry) Department of Optometry, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Abel Sinshaw (BSc, MSC, Lecturer of Optometry) Department of Optometry, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Yitayeh Belsti (BSc, Lecturer of Medical Physiology): Department of Physiology, College of Medicine and Health Sciences, University of Gondar, Ethiopia
Author Contributions
All authors made substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed on the journal to which the article will be submitted; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
Not applicable for this study.
Disclosure
We, the authors, declare that we have no competing interests for this study.
References
1. He M, Abdou A, Naidoo KS, et al. Prevalence and correction of near vision impairment at seven sites in China, India, Nepal, Niger, South Africa, and the United States. Am J Ophthalmol. 2012;154(1):107–116.e1. doi:10.1016/j.ajo.2012.01.026
2. Zebardast N, Friedman DS, Vitale S. The prevalence and demographic associations of presenting near-vision impairment among adults living in the United States. Am J Ophthalmol. 2017;174:134–144. doi:10.1016/j.ajo.2016.11.004
3. Varadaraj V, Lee MJ, Tian J, Ramulu PY, Bandeen-Roche K, Swenor BK. Near vision impairment and frailty: evidence of an association. Am J Ophthalmol. 2019;208:234–241. doi:10.1016/j.ajo.2019.08.009
4. Fricke TR, Tahhan N, Resnikoff S, et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: systematic review, meta-analysis, and modelling. Ophthalmology. 2018;125(10):1492–1499. doi:10.1016/j.ophtha.2018.04.013
5. Munaw MB, Kebede BN, Adimassu NF. Unmet need for presbyopia correction and its associated factors among school teachers in Hawassa city, South Ethiopia. BMC Ophthalmol. 2020;20(1):1–8. doi:10.1186/s12886-020-01454-5
6. Ntodie M, Abu SL, Kyei S, Abokyi S, Abu EK. Near vision spectacle coverage and barriers to near vision correction among adults in the cape coast metropolis of Ghana. Afr Health Sci. 2017;17(2):549–555.
7. Lin W, Wang SL, Wu HJ, et al. Associations between arsenic in drinking water and pterygium in southwestern Taiwan. Environ Health Perspect. 2008;116(7):952–955. doi:10.1289/ehp.11111
8. Bourne RRA, Flaxman SR, Braithwaite T, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Heal. 2017;5(9):e888–97. doi:10.1016/S2214-109X(17)30293-0
9. Frick KD, Joy SM, Wilson DA, Naidoo KS, Holden BA. The global burden of potential productivity loss from uncorrected presbyopia. Ophthalmology. 2015;122(8):1706–1710. doi:10.1016/j.ophtha.2015.04.014
10. Hutchins B, Huntjens B. Patients’ attitudes and beliefs to presbyopia and its correction. J Optom. 2020;1–6. doi:10.1016/j.optom.2020.02.001
11. Wolffsohn JS, Davies LN. Presbyopia: effectiveness of correction strategies. Prog Retin Eye Res. 2019;68:124–143. doi:10.1016/j.preteyeres.2018.09.004
12. Chan VF, MacKenzie GE, Kassalow J, Gudwin E, Congdon N. Impact of presbyopia and its correction in low- And middle-income countries. Asia-Pacific J Ophthalmol. 2018;7(6):370–374.
13. Burke AG, Patel I, Munoz B, et al. Population-based study of presbyopia in rural Tanzania. Ophthalmology. 2006;113(5):723–727. doi:10.1016/j.ophtha.2006.01.030
14. He M, Abdou A, Ellwein LB, et al. Age-related prevalence and met need for correctable and uncorrectable near vision impairment in a multi-country study. Ophthalmology. 2014;121(1):417–422. doi:10.1016/j.ophtha.2013.06.051
15. Cheng F, Shan L, Song W, Fan P, Yuan H. Distance- and near-visual impairment in rural Chinese adults in Kailu, Inner Mongolia. Acta Ophthalmol. 2016;94(4):407–413. doi:10.1111/aos.12808
16. Alemu HW. Willingness to pay for spectacle: an outreach-based cross-sectional study. Ophthalmic Epidemiol. 2020;00(00):1–5. doi:10.1080/09286586.2020.1786589
17. Sivardeen A, McAlinden C, Wolffsohn JS. Presbyopic correction use and its impact on quality of vision symptoms. J Optom. 2020;13(1):29–34. doi:10.1016/j.optom.2018.12.004
18. World Health Organization. Universal eye health - A global action plan 2014-2019. WHO Libr Cat Data. 2013;22. https://www.who.int/blindness/AP2014_19_English.pdf?ua=1.
19. Charman WN. Non-surgical treatment options for presbyopia. Expert Rev Ophthalmol. 2018;13(4):203–215. doi:10.1080/17469899.2018.1506330
20. Girum M, Gudeta AD, Alemu DS. Determinants of high unmet need for presbyopia correction: a community-based study in Northwest Ethiopia. Clin Optom. 2017;9:25–31. doi:10.2147/OPTO.S123847
21. Andualem HB, Assefa NL, Weldemichael DZ, Tefera TK. Prevalence and associated factors of presbyopia among school teachers in Gondar city, Northwest Ethiopia, 2016. Clin Optom. 2017;9:85–90. doi:10.2147/OPTO.S129326
22. Kortüm K, Hirneiß C, Müller M, Babenko A, Kampik A, Kreutzer TC. The influence of a specific ophthalmological electronic health record on ICD-10 coding. BMC Med Inform Decis Mak. 2016;16(1):1–7. doi:10.1186/s12911-016-0340-1
23. Lu Q, He W, Murthy GVS, et al. Presbyopia and near-vision impairment in rural northern China. Investig Ophthalmol Vis Sci. 2011;52(5):2300–2305. doi:10.1167/iovs.10-6569
24. Marmamula S, Keeffe JE, Rao GN. Uncorrected refractive errors, presbyopia and spectacle coverage: results from a rapid assessment of refractive error survey. Ophthalmic Epidemiol. 2009;16(5):269–274. doi:10.1016/j.preteyeres.2018.09.004
25. Nirmalan PK, Krishnaiah S, Shamanna BR, Rao GN, Thomas R. A population-based assessment of presbyopia in the state of Andhra Pradesh, south India: the Andhra Pradesh eye disease study. Investig Ophthalmol Vis Sci. 2006;47(6):2324–2328. doi:10.1167/iovs.05-1192
26. Kumah DB, Lartey SY, Amoah-Duah K. Presbyopia among public senior high school teachers in the Kumasi metropolis. Ghana Med J. 2011;45(1):27–30. doi:10.4314/gmj.v45i1.68919
27. Elijah CN. Barriers to uptake of presbyopic correction among primary and secondary teachers in public schools in B/K-dere communities in Rivers State, Nigeria. Adv Ophthalmol Vis Syst. 2016;5(3):282–284.
28. Zhu M, Tong X, Zhao R, et al. Visual impairment and spectacle coverage rate in Baoshan district, China: population-based study. BMC Public Health. 2013;13:1. doi:10.1186/1471-2458-13-311
29. Bourne RRA, Dineen BP, Noorul Huq DM, Ali SM, Johnson GJ. Correction of refractive error in the adult population of Bangladesh: meeting the unmet need. Investig Ophthalmol Vis Sci. 2004;45(2):410–417. doi:10.1167/iovs.03-0129
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.