Back to Journals » International Medical Case Reports Journal » Volume 8
N-acetylcysteine overdose after acetaminophen poisoning
Authors Mahmoudi GA , Astaraki P, Zafar Mohtashami A, Ahadi M
Received 18 September 2014
Accepted for publication 26 November 2014
Published 27 February 2015 Volume 2015:8 Pages 65—69
DOI https://doi.org/10.2147/IMCRJ.S74563
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ronald Prineas
Ghafar Ali Mahmoudi,1 Peyman Astaraki,1 Azita Zafar Mohtashami,1 Maryam Ahadi2
1Faculty of Medicine, Department of Internal Medicine, Lorestan University of Medical Sciences, 2Legal Medicine Research Center of Lorestan, Khorramabad, Iran
Abstract: N-acetylcysteine (NAC) is used widely and effectively in oral and intravenous forms as a specific antidote for acetaminophen poisoning. Here we report a rare case of iatrogenic NAC overdose following an error in preparation of the solution, and describe its clinical symptoms. Laboratory results and are presented and examined. A 23-year-old alert female patient weighing 65 kg presented to the emergency ward with weakness, lethargy, extreme fatigue, nausea, and dizziness. She had normal arterial blood gas and vital signs. An excessive dosage of NAC over a short period of time can lead to hemolysis, thrombocytopenia, and acute renal failure in patients with normal glucose-6-phosphate dehydrogenase, and finally to death. Considering the similarity between some of the clinical symptoms of acetaminophen overdose and NAC overdose, it is vitally important for the administration phases and checking of the patient's symptoms to be carried out attentively and cautiously.
Keywords: N-acetylcysteine, overdose, acetaminophen poisoning, medication error
Introduction
Acetaminophen is a widely used analgesic and antipyretic agent. However, acetaminophen overdose is common in patients who present to hospital emergency rooms, and in many cases causes liver and renal necrosis.1–3 Previous studies reported that a sterile 20% solution of N-acetylcysteine (NAC) administered intravenously was effective in the treatment of acetaminophen overdose.4–6 Their NAC regimen was 150 mg/kg body weight given over 15–30 minutes, 50 mg/kg over 4 hours, and 100 mg/kg over 16 hours, with the final dose of 100 mg/kg repeated three times until liver aminotransferase levels reverted to normal.7–9 NAC solution has been used for over two decades in emergency wards in Iran. However, despite its efficacy in reducing mortality due to acetaminophen poisoning, intravenous NAC can cause anaphylactoid reactions.6–8 Due to the complexity of preparation of NAC as well as its side effects, mistakes are possible. Here we report a rare case of iatrogenic NAC overdose due to an error made during preparation of the solution. Clinical symptoms, laboratory test results, are presented and discussed.
Case report
Four hours after taking 50 acetaminophen 325 mg tablets, a 23-year-old alert female patient weighing 65 kg presented to the emergency ward with weakness, lethargy, nausea, and dizziness. She had normal arterial blood gas and vital signs. Following administration of activated charcoal, in view of the toxic dose of acetaminophen ingested, treatment with NAC was started, with a 10 g loading dose of NAC 150 mg/kg given over 30 minutes, followed by a 9.5 g maintenance dose with 500 mL of 5% dextrose water administered over 20 hours. The patient developed agitation, nausea, vomiting, dyspnea, tachypnea, hypotension (blood pressure 80 mmHg), drowsiness, and periorbital edema. Suspecting a drug allergy, the physician stopped administration of NAC, but further investigation revealed that a nurse had administered NAC 100 g (instead of 10 g) as the loading dose. After administration of NAC 100 g, the patient’s pupils were normal, symmetric, and reactive to light. However, her level of consciousness decreased to 7/15 on the Glasgow Coma Scale, her hypotension became severe, her radial pulse became unpalpable, and her respiratory rate increased to 32 per minute. She was intubated and transferred to the intensive care unit, where she died 12 days later.
According to the clinical evaluations, the patient’s pupils were normal, symmetric, and reactive to light until the third day, when they became mydriatic and reacted slowly to light thereafter. Computed tomography of the brain showed signs of edema. Respiratory tract secretions increased significantly, and the patient had dyspnea, tachypnea, and shallow breathing early on. Her breath sounds were decreased on auscultation of the lungs. Her arterial blood gas measurements indicated metabolic acidosis and respiratory alkalosis that was resistant to treatment in the first 18 hours, but was controlled by ventilation and infusion of sodium bicarbonate.
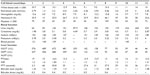
On the first day, there was a gradual increase in edema around the eyes and face. The patient also became oliguric, with a urine output of less than 250 mL in 24 hours. On the second day, generalized edema was observed. Biochemistry showed hypernatremia and increased blood urine and creatinine from the first day onward (Table 1).
Liver function tests showed elevated alanine aminotransferase and aspartate aminotransferase (22 and 12 times the upper limit of normal, respectively) until the second day of poisoning and a gradual decrease to normal by the seventh day. Partial thromboplastin time, international normalized ratio, prothrombin time, and total bilirubin levels were within normal limits during hospitalization (Table 1).
Between the first and second day of NAC administration, the patient’s hemoglobin and hematocrit levels decreased markedly from 12.6 g/dL and 35% to 4.5 g/dL and 13%, respectively. Her hemoglobin continued to decrease steadily, despite administration of a peak cell injection. Her platelet level was 70×1,000/mm3 in the first 24 hours after the poisoning and 29×1,000/mm3 on the second day. As with her hemoglobin levels, an intermittent decrease in platelets was observed, prompting administration of platelets and fresh frozen plasma (Table 1). Schistocytes peripheral blood film slide by thrombotic thrombocytopenic purpura and hemolytic anemia diagnosis; plasmapheresis was also performed 7 days after taking acetaminophen.
Discussion
The issue of patient health is a priority in medicine and is paramount in research. Each year, a large number of patients are harmed as a result of medical errors, many of which are preventable.10–12 The risk of such events occurring can be greatly reduced by identifying and understanding their causes. Hepatotoxicity is a well-known side effect of acetaminophen poisoning.13–15 Acetaminophen toxicity was recognized in our patient, who presented to the emergency ward after taking 16.25 g of acetaminophen in an attempt to commit suicide. She was complaining of peptic stomach pain, dizziness, and headache. Her serum aminotransferases indicated phase 2 toxicity; they remained elevated for 48 hours, then decreased and finally reverted to normal level on the third day of hospitalization. Other liver function tests, including international normalized ratio, prothrombin time, alkaline phosphatase, and bilirubin were reported to be normal. These findings and normal liver histology (Lam liver) represents a slight injury to hepatocytes and no liver failure and encephalopathy in the patient’s NAC seemed effective to prevent liver damage due to the poisoning.
NAC is derived from the amino acid, L-cysteine, oral and intravenous formulations of which are used widely and effectively as an antidote for acetaminophen poisoning (especially during the first 10 hours after poisoning) to prevent hepatotoxicity.16–19 Acetylcysteine is rapidly absorbed from the gastrointestinal tract, with maximal plasma concentrations achieved within half an hour of administration of a therapeutic dose.20,21 The mechanism via which acetylcysteine works in acetaminophen poisoning is not clear. At least four mechanisms have been proposed, including: intracellular activity of NAC as a substitute for glutathione, its combination with toxic metabolites, and elimination of their toxic effects (ie, a direct antidotal effect); stimulation of glutathione synthesis; stimulation of acetaminophen sulfate and antioxidant effects; and decreasing the effects of the inflammatory response induced in the liver.22–25
The most commonly reported adverse effects of intravenous acetylcysteine are anaphylactic reactions, including rash, pruritus, angioedema, bronchospasm, tachycardia, and hypotension.26–29 A previous study reported that approximately 15% of patients treated with intravenous acetylcysteine had an anaphylactic reaction within 2 hours after the initial infusion, and that increasing the infusion time from 15 minutes to 60 minutes did not alter the rate of adverse events.30–32 Other common adverse effects included vomiting and flushing. Further, retrospective studies have identified adverse effects in approximately 5% of cases.32–34
Considering the toxic dose of acetaminophen ingested by this patient, the physician prescribed intravenous NAC. Because of a mistake made by a nurse, the patient received seven times more NAC over 20 minutes that she should have. A number of clinical symptoms were reported following NAC overdose, including vomiting, nausea, exacerbation of respiratory distress (bronchospasm), periorbital angioedema, and hypotension while receiving the antidote.
Some studies reported that administration of NAC 63.6% and even 50% is associated with mild to life-threateningly severe side effects; these are quite prevalent when using oral treatment, and there is always a risk of iatrogenic overdose when using intravenous NAC. More serious side effects have been observed during actual administration of NAC and in the first hour following the dose.9,18,19
The most common side effects of treatment with intravenous NAC are anaphylactic reactions, including nausea, vomiting, flushing, hives, and rashes in non-severe cases, and bronchospasm, angioedema, and hypotension in severe cases. These reactions are dose-dependent and preceded by release of histamine. Usually the side effects are mild and resolve rapidly after discontinuation of the drug or a reduction in the injection rate.19,21,23,24 Regarding the allergic reactions in this case, the physician stopped the intravenous NAC and administered chlorphenamine and hydrocortisone.
Hypotension is reported to be an unusual symptom of acetaminophen. NAC has a nitrate-based vasodilating effect, and is commonly used to prevent nephropathy associated with radiocontrast agents. Our patient’s blood pressure was normal until the NAC overdose occurred, after which time her systolic pressure decreased to 60 mmHg. Normal saline solution was administered to increase her blood pressure, but without success. Her hypotension was controlled by administration of dopamine at a maximum dose of 15 mg/kg/h.25
In a previous paper, a cumulative intravenous NAC dose of 2,450 mg/kg was reported to be associated with status epilepticus, intracranial hypertension, and death in a child. Anuria, uremia, edema, loss of consciousness, and a decrease in glomerular filtration rate to approximately 40% of normal was seen within the first day after NAC overdose, and intensifying the process in the days after acetaminophen poisoning (Table 1), suggesting acute renal failure. Decreased hemoglobin, hematocrit, and platelet levels, the presence of schistocytes on a peripheral blood smear, along with other examinations on hematology, a negative Coombs test, hemolytic anemia, and thrombotic thrombocytopenic purpura orimmune thrombocytopenia caused by drug overdose suggested hemolytic uremic syndrome caused by NAC overdose.
Acute tubular necrosis and nephrotoxicity are reported in 1%–2% of cases of acetaminophen poisoning,26and can occur in isolation or along with hepatoxicity caused by NAC overdose.27,28 Its created metabolism is said to be dependent on toxic metabolite from renal cells’ cytochrome P450 activities and prostaglandin reactions. In many cases, renal failure due to acetaminophen ingestion develops after liver poisoning. It should be distinguished from hepatorenal symptoms caused by rapid liver failure.26 None of the liver function tests in our patient were in favor of liver failure or hepatorenal syndrome. Severe hypotension seen in NAC overdose due to a vasodilatory effect and the consequent oliguria raises the issue of prerenal pathophysiology and acute renal failure. Administration of 700 mL of NAC within 20 minutes, blood osmolality changes, and changes in glomerular filtration made renal failure possible. Unfortunately after the patient’s anuria and poor response to fluid therapy of sedimentation, urinary test was not possible, and differentiation between prerenal and post-renal failure was not carried out.
The patient was treated with daily hemodialysis. Hemolysis is not a common side effect of acetaminophen poisoning. Some papers have reported hemolytic anemia due to glucose-6-phosphate dehydrogenase (G6PD) deficiency.29,30 G6PD deficiency was not confirmed in our patient. A justifiable mechanism and cause for hemolysis and thrombocytopenia are not known. In the current case, daily plasmapheresis, administration of fresh frozen plasma, and platelet injections were also performed. Regrettably, the patient died as a result of hemolytic uremic syndrome after 12 days of treatment.
Animal studies and previous case reports strongly suggest that NAC overdose causes cerebral edema and seizures. To minimize the possibility of dosing errors, intravenous NAC should be administered as 12.5 mg/kg/h for 4 hours followed by 6.25 mg/kg/h for 16 hours.33
Conclusion
An excessive dosage of NAC over a short period of time can lead to hemolysis, thrombocytopenia, acute renal failure, and death in patients with normal G6PD. Considering the similarity between some of the clinical symptoms of acetaminophen overdose and NAC overdose, it is important to carry out the administration phases and check the patient’s symptoms more attentively and cautiously.
Disclosure
The authors report no conflicts of interest in this work.
References
Whyte AJ, Kehrl T, Brooks DE, Katz KD, Sokolowski D. Safety and effectiveness of acetadote for acetaminophen toxicity. J Emerg Med. 2010;39:607–611. | |
Clemmesen JO, Ott P, Dalhoff KP, Astrup LB, Tage-Jensen U, Poulsen HE. [Recommendations for treatment of paracetamol poisoning. Danish Medical Society, Study of the Liver]. Ugeskr Laeger. 1996;158:6892–6895. | |
Schmidt LE, Dalhoff K. Risk factors in the development of adverse reactions to N-acetylcysteine in patients with paracetamol poisoning. Br J ClinPharmacol. 2001;51:87–91. | |
Mant TG, Tempowski JH, Volans GN, et al. Adverse reactions to acetylcysteine and effects of overdose. BMJ. 1984;289:217–219. | |
Kerr F, Dawson A, Whyte IM, et al. The Australasian Clinical Toxicology Investigators Collaboration randomized trial of different loading infusion rates of N-acetylcysteine. Ann Emerg Med. 2005;45: 402–408. | |
Atkuri KR, Mantovani JJ, Herzenberg LA, Herzenberg LA. N-Acetylcysteine, a safe antidote for cysteine/glutathione deficiency. Curr Opin Pharmacol. 2007;7:355–359. | |
Mullins ME, Vitkovitsky IV. Hemolysis and hemolytic uremic syndrome following five-fold N-acetylcysteine overdose. Clin Toxicol (Phila). 2011;49:755–759. | |
Haddad LM, Winchester JF. Clinical Management Poisoning and Drug Overdose. Philadelphia, PA, USA: WB Saunders; 1995. | |
Viccelio P, Bania T, Brent J, et al, editors. Emergency Toxicology. Chapter 3. Philadelphia, PA, USA: Lippincott-Raven; 1998. | |
Corcoran GB, Mitchell JR, Vaishnav YN, et al. Evidence that acetaminophen and N-hydroxyacetaminophen form a common arylating intermediate, N-acetyl-p-benzoquinoneimine. Mol Pharmacol. 1980;18:536–542. | |
Buckpitt AR, Rollins DE, Mitchell JR. Varying effects of sulfhydryl nucleophiles on acetaminophen oxidation and sulfhydryl adduct formation. Biochem Pharmacol. 1979;28:2941–2946. | |
Slattery JT, Wilson JM, Kalhorn TF, et al. Dose-dependent pharmacokinetics of acetaminophen: evidence of glutathione depletion in humans. Clin Pharmacol Ther. 1987;41:413–418. | |
Harrison PM, Keays R, Bray-GP, et al. Improved outcome of paracetamol induced hepatic failure by late administration of acetylcysteine. Lancet. 1995;335:1572–1573. | |
Smilkstein MJ, Knapp GL, Kulig KW, Rumack BH. Efficacy of oral N-acetyl cysteine in the treatment of acetaminophen overdose. N Engl J Med. 1988;319:1557–1562. | |
Prescott FF, Illingworth RN, Critchley JA, Stewart MJ, Adam RD. Intravenous treatment is the treatment of choice or paracetamol poisoning. BMJ. 1978;2:1097–1100. | |
Prescott L. Oral or intravenous N-acetylcysteine for acetaminophen poisoning? Ann Emerg Med. 2005;45:409–413. | |
Smilkstein MJ, Bronstein AC, Linden C. Acetaminophen overdose: a 48-hour intravenous N-acetylcysteine treatment protocol. Ann Emerg Med. 1991;20:1058–1063. | |
Bateman DN, Woodhouse KW, Rawlins MD. Adverse reactions to N-acetylcysteine. Hum Toxicol. 1984;3:393398. | |
Schmidt LE, Dalhoff KP. [Side-effects of N-acetylcysteine treatment in patients with paracetamol poisoning]. Ugeskr Laeger. 1999;161:2669–2672. Danish. | |
Dawson AH, Henry DA, McEwan J. Adverse reactions to N-acetylcysteine during treatment for paracetamol poisoning. Med J Aust. 1989;150:329–331. | |
Millea PJ. N-acetylcysteine: multiple clinical applications. Am Fam Physician. 2009;80:265–269. | |
Mazer M, Perrone J. Acetaminophen-induced nephrotoxicity: pathophysiology, clinical manifestations, and management. J Med Toxicol. 2008;4:2–6. | |
Blakely P, McDonald BR. Acute renal failure due to acetaminophen ingestion: a case report and review of the literature. J Am Soc Nephrol. 1995;6:48–53. | |
Kasap B, Türkmen M, Alaygut D, Soylu A, Kavukçu S. Acetaminophen-induced nephrotoxicity in an adolescent girl. Turk Pediatri Arsivi. 2011;46:343–345. | |
Sklar GE. Hemolysis as a potential complication of acetaminophen overdose in a patient with glucose-6-phosphate dehydrogenase deficiency. Pharmacotherapy. 2002;22:656–658. | |
Wright RO, Perry HE, Woolf AD, Shannon MW. Hemolysis after acetaminophen overdose in a patient with glucose-6-phosphate dehydrogenase deficiency. J Toxicol Clin Toxicol. 1996;34:731–734. | |
Heard K, Schaeffer TH. Massive acetylcysteine overdose associated with cerebral edema and seizures. Clin Toxicol. 2011;49:423–425. | |
Kante MZ. Comparisonof oral and iv acetylcysteine in the treatment of acetaminophen poisoning. Am J Health Syst Pharm. 2006;63: 1821–1827. | |
Brok J, Buckley N, Gluud C. Interventions for paracetamol (acetaminophen) overdose. Cochrane Database Syst Rev. 2006;2: CD003328. | |
James LP, Mayeux PR, Hinson JA. Acetaminophen-induced hepatotoxicity. Drug Metab Dispos. 2003;31:1499–1506. | |
Borgström L, Kågedal B, Paulsen O. Pharmacokinetics of N-acetylcysteine in man. Eur J Clin Pharmacol. 1986;31:217–222. | |
Bailey B, Blais R, Letarte A. Status epilepticus after a massive intravenous N-acetylcysteine overdose leading to intracranial hypertension and death. Ann Emerg Med. 2004;44:401–406. | |
Miller LF, Rumack BH. Clinical safety of high oral doses of acetylcysteine. Semin Oncol. 1983;10 Suppl 1:76–85. | |
Kerr F, Dawson A, Whyte IM, et al. The Australasian Clinical Toxicology Investigators Collaboration randomized trial of different loading infusion rates of N-acetylcysteine. Ann Emerg Med. 2005;45:402–408. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.