Back to Journals » Medical Devices: Evidence and Research » Volume 15
MRI Safety Practice Observations in MRI Facilities Within the Kingdom of Jordan, Compared to the 2020 Manual on MR Safety of the American College of Radiology
Authors Ayasrah M
Received 4 February 2022
Accepted for publication 9 May 2022
Published 13 May 2022 Volume 2022:15 Pages 131—142
DOI https://doi.org/10.2147/MDER.S360335
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mohammad Ayasrah
Department of Allied Medical Sciences-Radiologic Technology, Faculty of Applied Medical Sciences, Jordan University of Science and Technology, Irbid, Amman, Jordan
Correspondence: Mohammad Ayasrah, Department of Allied Medical Sciences-Radiologic Technology, Faculty of Applied Medical Sciences, Jordan University of Science and Technology, PO Box 3030, Irbid, 22110, Jordan, Tel +962 27201000-26939, Fax +962 27201087, Email [email protected]
Purpose: The absence of ionizing radiation in MRI applications does not guarantee absolute safety. Implementing of safety guidelines can ensure high-quality practice in the clinical MRI with the minimum risk. For this purpose, this cross-section quantitative study conducted in Jordan Kingdom aimed to assess current MRI safety guidelines in comparison with those of 2020 Manual on MR Safety of the American College of Radiology (ACR).
Patients and Methods: A site observation study of 38 MRI units was undertaken in June 2021. A well-structured MRI safety questionnaire was the primary data collection method. Data were subjected to a descriptive statistics content analysis by the SPSS version 20. The results were analyzed to yield comprehensive discussions.
Results: A total of 38 MRI facilities in participated in this study with the responding rate of 44.7%. Patient screening areas and changing rooms were available in about 29% (11/38) of the MRI facilities. Most facilities (55%, 21/38) conducted verbal screening only whereas 21% implemented both written and verbal screening for their patients and companions in zone II, which was present in a percentage of 29% in the approached facilities. Meanwhile, only 13 (43.2%) of 38 facilities used handheld magnets for physical screening, 25 (65.8%) of MRI units did not use any kind of ferromagnetic metal detection systems. Three (7.9%) participating centers had MR-safe wheelchairs, ventilators, anesthesia machines, and stretchers. Most MRI facilities participating in this study (71%) had emergency preparedness plans for alternative power outages. Despite a relatively low number of participating centers having an emergency exit or code (26.3% and 10.5%, respectively), none of them performed practice drills for such scenarios.
Conclusion: Investing in new MR-safe equipment requires introducing ferromagnetic detecting systems. More research is needed to establish the degree of MRI professional’s safety-related education.
Keywords: magnetic resonance imaging safety, Jordan, imaging risks, ferromagnetic detection, screening, imaging policy
Introduction
Magnetic resonance imaging (MRI) has been a main important element in diagnostic imaging and is considered a non-invasive and safe modality uses of non-ionizing radiation.1 Compared to computed tomography (CT) and other conventional radiology. MRI devices provide higher contrast resolution, create three-dimensional detailed anatomical images of the human body, and easier treatment monitoring.2,3
Current Status of MRI and Its Risks
Recent technological advances in MRI cause positive impacts on medical imaging, including image quality, examination times, and productivity.4 MRI has been extensively established throughout the last years, and more than 36,000 MRI scanners carry out nearly 95 to 100 million of examinations each year worldwide.5,6 This indicates that providing MRI safety not only is an integral component for the imaging process, but it also is crucial for all involved parties, including MR personnel, patients, and health-care professionals. Ignoring this importance in the MRI, however, may pose severe risks to patients, staff, and equipment h.6 Radiation is classified as being either non-ionizing or ionizing. The non-ionizing radiation is observed with lower frequency, lower energy, and longer wavelength whereas the ionizing radiation has been observed with high energy, high frequency and shorter wavelength. The ionizing radiation possess adequate energy for producing the ions at molecular level.7 MRI do not use ionizing radiation and is considered a non-invasive procedure. Instead, MRIs use a strong magnetic field and radio waves, which has to be considered to avoid harm in patients and caregivers. Risks in clinical MRI are broadly classified into magnetism and non-magnetism-related risks.8 The magnetism-related risks originate from the static magnetic field of the main magnet, time-varying of the gradients, and radiofrequency (RF) of the coils in the MRI process.9 The static magnetic field hazards include signs of transient sensory induction, which mainly produces negative interaction between equipment and human tissue.10 The risk associated with the RF involves tissue heating and specific absorption rate (SAR) problems. Concerning time-varying gradients, the induced current may cause peripheral nerve stimulation, impression of implanted medical devices, and acoustic noise.11–15 Cryogenic hazards consist of cold burns, equipment damage, frostbite, and asphyxiation in the case of escaping helium cryogen inside the scanning room, and in this situation. Meanwhile, the adverse impacts of Gadolinium contrast medium are uncommon, but reactions like nausea, headache, transient dizziness, and injection pain inevitably occur even in a highly accredited healthcare facility.16,17
Effective Management of MRI
MRI safety policies primarily focus on who is directly or indirectly involved in the MRI imaging process, where the majority of hazards are linked to the patient communities.18 Based on the analyzed MRI safety reports, referral of contraindicated devices (32% of reports) and a failure to verify safety (21.5%) were identified as the two main trends.19 A Swedish study found that incidents involving MRIs are commonly underreported.20 MRI accidents can be minimized by implementing strict guidelines, effective management, and establishing MRI safety policies. It is noted that the staff attitude and management style are the major factors that affect MRI safety.17,21 International entities such as (ACR),22 UK’s MHRA,23 and Royal Australia/New Zealand College of Radiology (RANZCR)24 solidly establish the MRI safety guidelines. In 2020, ACR published guidance on MRI safe practice, addressing several safety pillars on access control, zoning, responsibilities, and annual training safety of MRI. Primarily, MRI safety guides deal with MRI personnel’s responsibilities, screening patients for MRI procedures and placing safety cautions like zoning and signage. Four zones with associated signs of solid magnetic field presence, five Gauss lines, and equipment compatibility are controlled by MR personnel.25 Zones VI and III are MR controlled access and monitored areas. Only accessible to authorized MR personnel and use appropriate control methods, such as nonmagnetic keys or plastic cards. In Zone III, ACR recommends using metal detectors or ferromagnetic detection system (FDS) to physically screen for the presence of metallic material.26 It is not recommended to use conventional hand-held metal detectors because they do not distinguish between ferromagnetic and nonferromagnetic materials.27 The use of FDS is suggested as a supplement to thorough and careful screening of people and devices approaching Zone IV. Zone II generally refers to the patient waiting and screening area, where all personnel are permitted to enter Zone II but supervised by MR staff. In Zone I, all areas that are freely accessible to the public, including the parking lot and general hallway, are beyond the control of MR personnel.28 It is important to post signs describing the presence of magnetic fields, warnings that the magnet is always on, and a warning that the magnetic field exceeds five Gauss in the vicinity.29 An ACR standard classifies and labels MRI equipment into MR-Safe, MR-Conditional, and MR-Unsafe categories. This prevents projectile effect accidents that could cause injury.30 The new version of 2020 Manual on MR Safety recommends each MRI site have designated or appointed MR Medical Director (MRMD), MR Safety Officer (MRSO), and MR Safety Expert (MRSE) and documented on the MRI policies and procedures section.22
MRI Safety Legal/Regulatory/Accreditation Environment Within Jordan
Health performance in Jordanian health institutions, and their subordinate departments, has remained stagnant because of an absence of policy and procedures by working owners, relying mostly on legacy processes.31 The Health Care Accreditation Council (HCAC) was founded in 2007 as a private non-profit shareholding company to assist the government in adopting a regulatory agenda for the health sector by establishing globally accepted healthcare standards and accreditation.32 The mission of HCAC is to develop standards, build capacity, and accredit healthcare programs that provide quality and safety to facilities and communities.33
MRI facilities in Jordan have witnessed various degrees of MRI accidents that have not been linked to patient harm, severe mortality during the last 5 years. Among these risks, cryogen quench accounted for the majority of ones.34 This is due to the absence of a specific MRI safety policy and special requirements for MRI technologists. Nowadays, witnessing a substantial increase in the MRI units and the number of its clinical application investigations in as well as safety-related accidents around the world, the MRI risk assessments is so fundamental to identify the hazards of healthcare workers, patients, and MR staff members.35 This study aims to determine the level of safety practice at MRI facilities in using the 2020 Manual on MR Safety of ACR. It sheds light on the current status of safety practices and procedures and is extremely important for decision-makers to adopt policies that promote patients’ safety. To the best of the researcher’s knowledge, no previous studies on MRI safety have been conducted in Jordan. The scarcity of studies, combined with the relatively high occurrences of safety-related events worldwide and the widespread use of MRI services in Jordan, have justified the need for research into this field
Research Method
This research tried to evaluate the present safety procedures implemented in the MRI departments in Jordan kingdom compared to those in the 2020 Manual on MR Safety of ACR. For this purpose, this research article was conducted on 85 MRI scanner units (governmental hospitals, private hospitals, and private diagnostic centers) in 11 provinces as the target population. At first, an invitation letter, a copy of Institutional Review Board (IRB) approval, and the survey questionnaire were sent via e-mail to these facilities to conduct a site survey on their facilities within the developed 2020 ACR Manual on MR Safety. Participation in the study was on voluntary bases and informed about the right not to participate. They were informed that replying to an email implicitly means that they have given informed consent and accept participation in the study. This indicates that the study complies with the Declaration of Helsinki. The study was approved by the Institutional Review Board of Jordan University of Science and Technology (127/136/2020). Respondents were given the choices of confidentiality and anonymity. The research team consisted of a biomedical MRI engineer and a senior technician to conduct the field survey. The survey questionnaire was included 30 questions about MRI equipment (eg, magnet strength, MRI department affiliation, type of the MRI open or close, and MRI clinical settings hospital-based or outpatient clinic), MRI safety policies and procedures (MRI safety policy and compliance, patient screening methods, emergency preparedness, infection control, MRI safety accessories, equipment safety, signs and barriers, and reporting, incident report registrar, access, and communication). The study excluded the new recommendations in the ACR Manual on MR Safety to designate or appoint MR Medical Director (MRMD), MR Safety Officer (MRSO), and MR Safety Expert (MRSE). The IBM Statistical Package for the Social Sciences (SPSS) Statistics software package was used to analyze the data, and finally, the findings were interpreted to the descriptive statistic (graphs and tables). This statistical test was used to compare the categorical variables and zoning for MRI facility design were analyzed.
Results
This study examined whether ACR safety policies and guidelines were available at an MRI facility in and if the staff followed them. The present study also investigated the MRI safety policy and compliance, patient screening methods, emergency preparedness, MRI safety accessories, equipment safety, signs and barriers, reporting, incident report registrar, access, and communication. This study surveyed 38 of Jordan’s 85 MRI scan centers, yielding a 44.7% response rate. The majority of the facilities (71.1%) used 1.5 Tesla magnets. Private radiology clinics and military hospitals had the major participants in the study (29% and 26%, respectively), as shown in Table 1.
 |
Table 1 Distribution of Healthcare Sectors Participating in the Study |
Figure 1 illustrates the availability of the main elements of the MRI Safety Policy and Procedure Manual recommended by the ACR. All MRI facilities failed to implement the above discussed major MRI safety policies and procedures. There were only 4 facilities out of 38 that implemented MRI safety training courses. The absence of an MRI safety policy manual that would outline the management structure to designate MR Medical Director (MRMD) with authority to assign MR Safety Officer (MRSO), and MR Safety Expert (MRSE) and other MRI personnel was disconcerting, thus reflecting the lack of MRI safety knowledge and awareness of the MRI safety issues.
 |
Figure 1 The availability of MRI safety policies criteria. |
The results of MRI facility safety design elements are depicted in Figure 2. Patient screening area, changing room, and zone III access control were available in about (29%. 11/38) of MRI facilities, whereas the rest of the safety design items were totally absent or hardly available. The implantation of the zoning system was not implemented, demarcated, or assigned. The frequency of availability of these zones was varied. MRI zones, including I, III and IV, were fully available because of the nature of work in MRI. However, zone II was accessible in 29% (11/38) of these screened facilities.
 |
Figure 2 Frequency of MRI facility safety design elements. |
The distribution of the available zone II was the greatest (35%) in the MRI centers of private hospitals, while it was the lowest in the private clinics, as shown in Table 2.
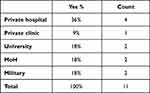 |
Table 2 The Distribution of the Available Zone II According to the Facility Affiliation |
Regarding pre-examination screening (Figure 3), it was conducted by MRI receptionists in Zone II using MRI safety screening form. Twenty-one percent of MRI facilities (8/38) used both oral and written screening methods recommended by the ACR for patients and their companions. The vast majority of the facilities (55%, 21/38) used only verbal screening methods. A pre-scheduling screening method, however, was not available.
 |
Figure 3 Frequency of preliminary MRI clinical screening methods. |
The MRI room possesses a powerful magnetic field; therefore, it is strictly prohibited to use other metal objects within the area. It is mandatory to take out any ferromagnetic objects before entering MRI room. The utilization of conventional metal detectors in MR does not differentiate between the non-ferromagnetic and ferrous materials, which is generally not recommended. The employment of FDS is strongly recommended as an adjunct for conscientious and thorough screening of the devices and persons to be admitted to zone IV.
In Figure 4, we illustrate the variety of physical screening methods including handheld and fixed metal detection systems. One-third (34.2%) of the 38 facilities used handheld magnetic detection systems, while 65.8% used no type of magnetic detection system. The MRI-compatible equipment at the MRI centers in this study is shown as graph in Figure 5. As can be seen, all MRI centers were not equipped with MR-Safe or MR-Conditional fire extinguishers. Regarding MR-Safe wheelchairs, ventilators, anesthesia machines, and stretchers, only 3 (7.9%) of the participating centers were equipped with this recommended equipment. Examination results of emergency preparedness are provided in Figure 6. Based on mentioned Figure, plans for alternative power outage was available in most MRI centers (71%, 27/38). A low percentage of the centers had an emergency exit or emergency code (26.3%, 10.5%), respectively. On the contrary, none of the participating centers performed drills on emergency response or had a specific emergency plan for quench or specific emergencies, including fire, water flood, and other critical situations.
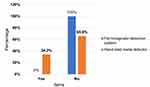 |
Figure 4 Availability of physical screening methods. |
 |
Figure 5 Count distributions of MR-compatible equipment. |
 |
Figure 6 The level of emergency preparedness action. |
Discussion
The present study reported the results of current MRI safety practices in Jordan. It provided numerical and graphic illustrations of current safety practices. While MRI can provide valuable diagnostic accuracy and detailed anatomic information without using ionizing radiation,36 its environment is still associated with many potential risks for the patients and staff, related healthcare workers, and the general public. MRI accidents, which are disproportionately underreported, are on the rise worldwide.37 Besides protecting people from potential dangers, it is vital to protect equipment against damage and breakdown. Radiology departments and their management must be assessed in order to ensure correct safety practices in clinical MRI environments in order to ensure the safety of MRIs.38
Safety Policies and Procedures
This study revealed the absence of an MRI safety policy manual that would outline the organizational structure for designating a MR Medical Director (MRMD) with authority to assign MR Safety Officer (MRSO), and MR Safety Expert (MRSE) and other MRI personnel. This could be disconcerting, thus reflecting the low level of MRI safety knowledge and awareness of the MRI safety issues. Piersson and Gorleku,39 in their national MRI safety survey, found that about half of the surveyed centers had no MRI safety policy document in the workplace. Opoku et al40 also found a lack of knowledge and training gap among MRI staff that might contribute to the absence of such cornerstone documents. Establishing and updating MRI safety policy by telling MRI staff about safety aims and objectives of safety guidelines and showing the chain of command during incidents are recommended. ACR supports establishing, implementing, and reviewing the safety guidelines, considering it essential for passing MRI facility accreditation.3,6,8
MRI Facility Safety Design
MRI suite design can hinder the effectiveness of safety screening practices.26 An appropriate MRI design includes zoning and labeling support by implementing the physical and clinical screening system. Unfortunately, the results of this study showed some deficiency in the implementation of zoning and labeling the MRI system. As shown in Table 3, zone labelling and demarcation are not applicable in all MRI systems regardless of their affiliation. ACR has developed four zones for MRI zoning; despite its wide acceptance globally, several equivalent alternative schemes have been developed. However, the Medicines and Healthcare Products Regulatory Agency (MHRA) in the United Kingdom identifies three zones. The MRI Controlled Access Area matches ACR Zone III, the MR Environment is similar to ACR Zone IV, and the MR Projectile Zone is a subset of the MR Environment within the magnet’s 3 mT fringe field. All three zones make up the MRI Controlled Access Area.25,41 The rationale behind the zoning strategy is to make it difficult for unqualified staff and unscreened patients to reach the potentially dangerous zone IV of the MRI center, thus minimizing the risk of projectile accidents and impairment of patient implanted devices.42 The new ACR recommendations treat the cryogens discharge zone similar to Zone III’s in labeling and access. The sub-zone I in different MRI facility locations is also recommended by ACR, such as transfer area/ferrous quarantine storage (Zone II), patient holding zone, MR conditional devices holding area, and emergency resuscitation equipment (Zones II or III). The results of this study also showed that these 4 zones were not fully applicable. As well, none of the surveyed MRI centers had the new recommended cryogen zone. Demarcations of safety zones and labelling of the 5-gauss line in zone IV were not applicable in all MRI systems regardless of their affiliation. Zone II played a vital role in providing comfort for patients waiting and providing privacy for the patients during clinical screening. It acts as the first line of defense to prevent unauthorized people from entering zone III. It was only available in 31.6% (12/38) of the MRI centers. MRI centers in the rest of the MRI centers combined zones II and III, which compromised all safety procedures. Restricted access doors between zones II and III were another essential safety step to prevent soliciting unauthorized people from entering zone three. The present study revealed that few (31%, 12/38) MRI centers had used restricted access doors between zones II and III. Because of this low percentage, the controlled zones III and IV could be vulnerable to accidents.
 |
Table 3 The Availability of ACR Recommended MRI Zones and Their Signages |
Patients Screening
Preventing potentially hazardous events necessitates application of possible MR imaging safety interventions including thorough screening of patients and personnel, the availability of ferromagnetic detection devices and warning signs, and strict adherence to the patient-gowning policy.43 Before scheduling an MRI, the first level of screening should ideally begin with a preliminary evaluation of the referring physician. The second critical level of screening begins when the patient arrives at the MRI screening area (Zone II) to fill out the MRI screening form. Prior to allowing a patient access to Zone III, MRI technicians must review the MRI screening form. Screening provides information about any relevant patient conditions, contrast media contraindications, the presence of implantable medical devices, and metallic objects.16 This ensures that MRI scanning will not be hampered by any potential contraindications. Zone II is critical for patient clinical screening, providing comfort and privacy during waiting times, and preventing unscreened individuals from accessing potentially dangerous zones III and IV. The study showed that zone II was available in 29% of the approached MRI centers. On the other hand, Zones III and IV were available by default in all surveyed facilities as a part of vendor design templates in the installation process. Zone III is a precautionary area adjacent to Zone IV (magnet room), where the RF or gradient fields may be too strong to pose a physical threat to unscreened patients or personnel. Zone IV is a potentially dangerous zone where the MRI main magnet produces a magnetic field greater than 5 Gauss. Any ferromagnetic objects should be excluded of this room by clearly labeling it as a danger zone.17 Figure 4 shows that none of the MRI centers performed a preliminary screening prior to scheduling an MRI. There were 23.6% of centers that did not use any form screening methods, and only 8 centers out of 38 (21%) used both the screening form filling and verbal verification methods, as recommended by ACR. However, 55.3% (21/38) of MRI centers only performed verbal screenings. The majority of MRI-related incidents were caused by deficiencies in screening methods and improper controls on access to the MRI environment, especially when preventing personal items from entering the magnet room.44 In addition to written screening, physical screening is crucial to reduce MRI incidents. The conventional method of patients’ physical screening is the use of a portable handheld detector. ACR recommends the fixed implementation of a FDS. This type of detection device aims to detect metallic objects before Zone VI.8
Emergency Preparedness
This study showed that the vast majority (65.8%, 25/38) were not equipped with any metal detector. Only 34.2% (13/38) of the study’s MRI centers were equipped with a handheld metal detector, as shown in Figure 5. This study showed that only 3 out of 38 centers had access to emergency preparedness accessories, such as a secure stretcher, fire extinguisher, safe wheelchair, ventilator, anesthesia, and other power sources in case of an outage. Nevertheless, the scarcity of such MRI Conditional equipment in MRI suites is extremely unfortunate, especially for patients with unstable health conditions. The present study revealed no specific written plan or code of practice for emergencies such as quenching, fire, and water flooding, nor any practice drills on such scenarios. The emergency exits were installed in 89.5% (34/38) of the MRI center buildings. These results are significantly higher than those found in studies conducted in Greece (81.7%) and Ghana (67%). A total of 10.5% (4/38) of the buildings did not have an emergency code of practice or an emergency exit. In contrast, the majority of centers (71%, 27/38) had alternative power outage source, particularly those in hospital settings. The findings of this study are much less than those found in Greece and Ghana studies.39,45 Therefore, the training of staff involved in emergency response is essential to improve an organization’s ability to deal with any type of emergency to ensure that staff feels confident and competent in any emergency situation they may encounter during their clinical practice.46
Significance of the Study
MRI Safety practices associated with its clinical significance has to be considered more seriously. The MR staffs and technologists has to be completely aware of such procedures followed by every time follow-up to keep the zone free from hazards. Generally MRI employs a powerful magnet that can cause possible risks to the individuals present inside the room. Although there exists increased scrutiny by several health-care organisations on the accessibility, utility and the associated costs with imaging, MRI is considered to one of the most dynamic diagnostic tool in the prevailing medical system. Despite these highlights, the geographical distributions of the equipment and its reliable applications in resource of constrained countries like Jordan needs in-depth investigation for applying safety policies and procedures.
Conclusions
Many MRI centers have demonstrated compliance with ACR MRI safety guidelines in some areas; however, there are several areas where the guidelines may not be met. Facility designers can ensure they are thinking about patient and staff safety while adding value by collaborating with the facility on the zoning for MRI facility design. Therefore, MRI safety must be improved, and compliance with the ACR guidelines established by the agency must be achieved. The findings of the research does not conflict with the safety regulation of patient care. Specific identification of the MR safety procedures are presented in this paper. Infrastructure and population density are important factors to consider in future planning to ensure equitable distribution of high-tech medical equipment. It is, therefore, strongly recommended to invest in new MR-safe equipment, mainly in terms of emergency resuscitation equipment, as well as the implementation of ferromagnetic detection systems. This will be a practical approach to improve MRI safety for both patients and healthcare workers and lower the chance of severe safety occurrences. More research is, however, needed to determine the extent of safety-related education held by MRI experts.
Acknowledgments
We would like to thank our respectful research assistants for their distinguished role of data collection.
Funding
This work supported by Jordan University of Science and Technology, Irbid-Jordan, under grant number 20210006.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Watson RE. Lessons learned from MRI safety events. Curr Radiol Rep. 2015;10(3):1–7. doi:10.1007/s40134-015-0122-z
2. Lin E, Alessio A. What are the basic concepts of temporal, contrast, and spatial resolution in cardiac CT? J Cardiovasc Comput Tomogr. 2009;3(6):403–408. doi:10.1016/j.jcct.2009.07.003
3. Han T, Sohn Y, Park SJ, et al. Reduction of magnetic resonance image artifacts of NiTi implant by carbon coating. Mater Sci Eng C Mater Biol Appl. 2019;98:1–8. doi:10.1016/j.msec.2018.12.072
4. Sun J, Barnes M, Dowling J, Menk F, Stanwell P, Greer PB. An open source automatic quality assurance (OSAQA) tool for the ACR MRI phantom. Australas Phys Eng Sci Med. 2015;38(1):39–46. doi:10.1007/s13246-014-0311-8
5. Ogbole GI, Adeyomoye AO, Badu-Peprah A, Mensah Y, Nzeh DA. Survey of magnetic resonance imaging availability in West Africa. Pan Afr Med J. 2018;30:240. doi:10.11604/pamj.2018.30.240.14000
6. Sotardi ST, Degnan AJ, Liu CA, et al. Establishing a magnetic resonance safety program. Pediatr Radiol. 2021;51(5):709–715. doi:10.1007/s00247-020-04910-y
7. Chandarana H, Wang H, Tijssen R, Das IJ. Emerging role of MRI in radiation therapy. J Magn Reson Imaging. 2018;48(6):1468–1478. doi:10.1002/jmri.26271
8. Orchard LJ. Implementation of a ferromagnetic detection system in a clinical MRI setting. Radiography. 2015;21(3):248–253. doi:10.1016/j.radi.2014.12.007
9. Fountain AJ, Corey A, Malko JA, Strozier D, Allen JW. Imaging appearance of ballistic wounds predicts bullet composition: implications for MRI safety. Am J Roentgenol. 2021;216(2):542–551. doi:10.2214/AJR.20.23648
10. Hartwig V, Biagini C, De Marchi D, et al. Analysis, comparison and representation of occupational exposure to a static magnetic field in a 3-T MRI site. Int J Occup Saf Ergon. 2022;28(1):76–85. doi:10.1080/10803548.2020.1738114
11. Winter L, Seifert F, Zilberti L, Murbach M, Ittermann B. MRI-related heating of implants and devices: a review. J Magn Reson Imaging. 2021;53(6):1646–1665. doi:10.1002/jmri.27194
12. Hartwig V, Giovannetti G, Vanello N, Lombardi M, Landini L, Simi S. Biological effects and safety in magnetic resonance imaging: a review. Int J Environ Res Public Health. 2009;6(6):1778–1798. doi:10.3390/ijerph6061778
13. Abo Seada S, Price AN, Hajnal JV, Malik SJ. Minimum TR radiofrequency-pulse design for rapid gradient echo sequences. Magn Reson Med. 2021;86(1):182–196. doi:10.1002/mrm.28705
14. Glans A, Wilén J, Lindgren L. Maintaining image quality while reducing acoustic noise and switched gradient field exposure during lumbar MRI. J Magn Reson Imaging. 2021;54(1):315–325. doi:10.1002/jmri.27527
15. Hansson B, Olsrud J, Wilén J, Owman T, Höglund P, Björkman-Burtscher IM. Swedish national survey on MR safety compared with CT: a false sense of security? Eur Radiol. 2020;30(4):1918–1926. doi:10.1007/s00330-019-06465-5
16. MacIntyre S. Regulating MR safety standards. Radiol Technol. 2021;93(1):75–89.
17. Kanal E, Barkovich AJ, Bell C, et al. ACR guidance document for safe MR practices: 2007. AJR Am J Roentgenol. 2007;188(6):1447–1474. doi:10.2214/AJR.06.1616
18. Sadigh G, Applegate KE, Saindane AM. Prevalence of unanticipated events associated with MRI examinations: a benchmark for MRI quality, safety, and patient experience. J Am Coll Radiol. 2017;14(6):765–772. doi:10.1016/j.jacr.2017.01.043
19. Hudson D, Jones AP. A 3-year review of MRI safety incidents within a UK independent sector provider of diagnostic services. BJR Open. 2019;1(1):20180006. doi:10.1259/bjro.20180006
20. Kihlberg J, Hansson B, Hall A, Tisell A, Lundberg P. Magnetic resonance imaging incidents are severely underreported: a finding in a multicentre interview survey. Eur Radiol. 2022;32(1):477–488. doi:10.1007/s00330-021-08160-w
21. Crisp S, Dawdy K. Building a magnetic resonance imaging safety culture from the ground up. J Med Imaging Radiat Sci. 2018;49(1):18–22. doi:10.1016/j.jmir.2017.10.005
22. ACR Committee on MR Safety. ACR manual on MR safety version 1.0, 2020; 2020. Available from: https://www.acr.org/-/media/ACR/Files/Radiology-Safety/MR-Safety/Manual-on-MR-Safety.pdf.
23. Medicines and Healthcare products Regulatory Agency M. Safety guidelines for magnetic resonance imaging equipment in clinical use, 2021; 2021. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/958486/MRI_guidance_2021-4-03c.pdf.
24. The Royal Australian and New Zealand College of Radiologists (RANZCR). MRI safety guidelines version 3.0 2021; 2021.
25. Greenberg TD, Hoff MN, Gilk TB, et al. ACR guidance document on MR safe practices: updates and critical information 2019. J Magn Reson Imaging. 2020;51(2):331–338. doi:10.1002/jmri.26880
26. Chandra T, Chavhan GB, Sze RW, et al. Practical considerations for establishing and maintaining a magnetic resonance imaging safety program in a pediatric practice. Pediatr Radiol. 2019;49(4):458–468. doi:10.1007/s00247-019-04359-8
27. Shellock FG, Karacozoff AM. Detection of implants and other objects using a ferromagnetic detection system: implications for patient screening before MRI. AJR Am J Roentgenol. 2013;201(4):720–725. doi:10.2214/AJR.12.10332
28. Gilk TB. MR imaging safety: siting and zoning considerations. Magn Reson Imaging Clin N Am. 2020;28(4):481–488. doi:10.1016/j.mric.2020.07.006
29. Tsai LL, Grant AK, Mortele KJ, Kung JW, Smith MP. A practical guide to MR imaging safety: what radiologists need to know. RadioGraphics. 2015;35(6):1722–1737. doi:10.1148/rg.2015150108
30. Jaimes C, Biaggotti D, Sreedher G, Chaturvedi A, Moore MM, Danehy AR. Magnetic resonance imaging in children with implants. Pediatr Radiol. 2021;51(5):748–759. doi:10.1007/s00247-021-04965-5
31. Hameed AA. Implement some basic health accreditation standards Issued by the Health Care Accreditation Council (HCAC) for auditing the performance of hospitals applied research at the education children protection hospital. J Account Financial Stud. 2020;15(50):1–13.
32. Al-Faouri I, Al-Dmour A, Al-Ali N, AbuALRub R, Abu Moghli F. Effect of Health Care Accreditation Council survey site visit on perceived stress level among Jordanian healthcare providers. Nurs Forum. 2019;54(1):30–37. doi:10.1111/nuf.12294
33. The Health Care Accreditation Council. (“HCAC”. The Health Care Accreditation Council/About Us. HCAC). Available from: https://hcac.jo/en-us/About-Us.
34. Ayasrah M. Analysis of collected magnetic resonance imaging incidents in Jordan. Mater Today. 2021. doi:10.1016/j.matpr.2021.07.172
35. Ayasrah M. Current status, utilization, and geographic distribution of MRI devices in Jordan. Appl Nanosci. 2021;1–10. doi:10.1007/s13204-021-01904-6
36. Artificial intelligence enables whole-body positron emission tomography scans with minimal radiation exposure | SpringerLink. Available from: https://link.springer.com/article/10.1007/s00259-021-05197-3.
37. Khazi SS. Magnetic resonance imaging mishaps: a brief review. Available from: http://www.journaldmims.com/article.asp?issn=0974-3901;year=2018;volume=13;issue=3;spage=160;epage=161;aulast=Khazi.
38. Rathebe PC Health and safety control measures and MR quality control results in the MRI units of two public hospitals within the Mangaung metropolitan | SpringerLink. Available from: https://link.springer.com/article/10.1007/s42452-021-04707-0#Tab6.
39. Piersson AD, Gorleku PN. A national survey of MRI safety practices in Ghana. Heliyon. 2018;3(12):e00480. doi:10.1016/j.heliyon.2017.e00480
40. Opoku AS, Antwi W, Sarblah SR. Assessment of safety standards of magnetic resonance imaging at the Korle Bu Teaching Hospital (KBTH) in Accra, Ghana | IntechOpen. In: imaging and radioanalytical techniques in interdisciplinary research. Open access peer-reviewed edited volume; 2013. Available from: https://www.intechopen.com/chapters/43524.
41. Keevil S. Safety in magnetic resonance imaging. Med Phys. 2016;4:9.
42. Kamvosoulis P, Currie GM. PET/MRI, part 1: establishing a PET/MRI facility. J Nucl Med Technol. 2021;49(2):120–125. doi:10.2967/jnmt.120.261339
43. Goolsarran N, Martinez J, Garcia C. Using near-miss events to improve MRI safety in a large academic centre. BMJ Open Qual. 2019;8(2):e000593. doi:10.1136/bmjoq-2018-000593
44. Cross NM, Hoff MN, Kanal KM. Avoiding MRI-related accidents: a practical approach to implementing MR safety. J Am Coll Radiol. 2018;15(12):1738–1744. doi:10.1016/j.jacr.2018.06.022
45. Stogiannos N, Westbrook C. Investigating MRI safety practices in Greece. A national survey. Hell J Radiol. 2020;5(2). doi:10.36162/hjr.v5i2.347
46. Ladapo JA, Spritzer CE, Nguyen XV, Pool J, Lang E. Economics of MRI operations after implementation of interpersonal skills training. J Am Coll Radiol. 2018;15(12):1775–1783. doi:10.1016/j.jacr.2018.01.017
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
