Back to Journals » Clinical Ophthalmology » Volume 12
Monovision LASIK in emmetropic presbyopic patients
Authors Peng MY, Hannan S, Teenan D , Schallhorn SJ, Schallhorn JM
Received 11 April 2018
Accepted for publication 12 June 2018
Published 4 September 2018 Volume 2018:12 Pages 1665—1671
DOI https://doi.org/10.2147/OPTH.S170759
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Michelle Y Peng,1 Stephen Hannan,2 David Teenan,2 Steven J Schallhorn,1,3 Julie M Schallhorn1,4
1Department of Ophthalmology, University of California, San Francisco, CA, USA; 2Optical Express, Glasgow, UK; 3Carl Zeiss Meditec, CA, USA; 4F.I. Proctor Foundation, University of California, San Francisco, CA, USA
Background: To evaluate the efficacy and patient satisfaction of laser in situ keratomileusis (LASIK) monovision correction in presbyopic emmetropic patients.
Methods: A retrospective review of 294 patients who underwent LASIK for monovision was conducted. All patients had preoperative uncorrected distance visual acuity in each eye of 20/25 or better in both eyes and underwent primary LASIK treatment in one eye with a near target; 82 patients underwent surgery in the distant eye for hypermetropia. Patients completed a patient-reported-outcome questionnaire at their one-month postoperative visit. Analysis was performed on a per patient basis with a logistic regression model.
Results: Patients achieved a postoperative mean spherical equivalent of -0.05 diopters (D) in the distant eye and -1.92 D in the near eye. Prior to surgery, 64.7% (n=178) of patients reported they were satisfied or very satisfied with their vision; postoperatively, this increased to 85.4% (n=251). The greatest predictor of dissatisfaction after surgery was severe patient-reported visual phenomena (glare, halos, starbursts, ghosting) (odds ratio 1.18, P=0.001).
Conclusions: LASIK monovision for presbyopic patients with low refractive error and good preoperative uncorrected distance visual acuity is both safe and effective with high patient satisfaction. Patients who were dissatisfied in the postoperative period tended to be those with postoperative visual symptoms.
Keywords: monovision, LASIK, presbyopia, refractive surgery
Background
The treatment of presbyopia remains a challenge in refractive surgery. Numerous surgical options exist, including monovision from laser-assisted in situ keratomileusis (LASIK) or photorefractive keratectomy; corneal inlays;1 multifocal2 or aspheric corneal ablation;3 and refractive lens exchange with a multifocal, accommodating or extended depth of focus intraocular lens.4 Monovision with LASIK has been shown to be a safe and effective means of treating presbyopia with high patient satisfaction.5–7
Presbyopic correction in emmetropic or low hypermetropic patients requires particular attention, as patients have had good uncorrected vision prior to presbyopia and thus carry high expectations. A few studies have been performed regarding the use of LASIK monovision in emmetropes; however, they indicate promising results with regard to effectiveness and patient satisfaction.3,7–9 In this study, we assess the visual and patient-reported outcomes of emmetropic patients who underwent LASIK specifically for monovision to treat presbyopia.
Methods
This retrospective study was reviewed and approved by the Committee on Human Research, the institution-specific name for Institutional Review Board at the University of California, San Francisco. It was deemed exempt from review as it contained only de-identified information. This work is compliant with the Health Insurance Portability and Accountability Act of 1996 and has adhered to the tenets of the Declaration of Helsinki. All patients provided informed consent to undergo refractive surgery, but consent for participation was not sought as this study only used retrospective, de-identified data.
The records of Optical Express (Glasgow, UK), a large provider of refractive surgical services, were searched to identify all cases between January 1, 2012, and December 31, 2015, that met the following criteria: patients aged 45 or older who underwent primary LASIK treatment with an uncorrected distance visual acuity of 20/25 or better, underwent monovision treatment with a target of at least −1.0 D (diopters) in the near eye, attended a one-month follow-up visit and completed a patient-reported-outcome (PRO) questionnaire.
Data on demographic information (date of birth, gender, dominant eye), preoperative and postoperative refractive error (manifest refraction, uncorrected distance visual acuity [Snellen visual acuity chart]), uncorrected near reading acuity (measured with a logarithmic Bailey–Lovie near reading chart), best-corrected visual acuity (BCVA), keratometry (Pentacam, Oculus, Inc., Arlington, WA), the use of contact lens trial, preoperative and postoperative PRO, date of surgery and laser treatment were obtained.
All patients desired improved near vision without optical aids and met the indications for laser vision correction as specified by the excimer laser user manual (VISX Star S4, Abbott Medical Optics, Santa Ana, CA) with the exception that patients with autoimmune disease could undergo surgery if their condition was stable and well controlled. The patients provided full informed consent for LASIK surgery. All ablations were performed on the VISX Star S4 laser using a standard, wavefront-guided or iDesign ablation. All flaps were created with the Intralase iFS (Abbot Medical Optics).
Patients who expressed interest in monovision received a monovision trial with trial frames in clinic. If they liked this monovision trial, then they were scheduled thereafter for surgery. Patients who were unsure underwent a contact lens monovision trial prior to surgery. A near target was selected for their nondominant eye unless they preferred near vision in the dominant eye with a monovision demonstration.
The PRO provided was based on the questionnaire offered to patients in the Patient Reported Outcomes with LASIK (PROWL) trials.10 The survey was self-administered in a private kiosk in the clinic, and patients were assured that all the information would remain anonymous and the results would not be shared with their treating physician or be used to inform their care. All response fields used a Likert scale to obtain the patient’s preferences or degree of agreement. The incidence of visual phenomena, such as starburst, halo, glare, and ghost images/double vision, was rated on a scale between 1 (no difficulty) and 7 (severe difficulty). Ability to perform activities of daily living, including hobbies, driving and sports, was also assessed from 0 (no difficulty) to 4 (severe difficulty), with an option to indicate that patients did not partake in these activities for other reasons.
Descriptive statistics were obtained using Excel (Microsoft, Redmond, WA, USA). For the safety analysis, only patients with a recorded month-1 refraction and best-corrected distance acuity were included. For nonparametric data, averages are reported as the mean with the interquartile range (IQR), or the distribution between the 25th and 75th percentiles. For dichotomous outcomes (satisfied vs dissatisfied), Pearson’s chi-squared test was used for significance. Analysis was conducted using the Stata software package (STATACorp, College Station, TX, USA) and on a per-patient basis. A univariate logistic regression model was fitted into the data, and odds ratios (ORs) for patient dissatisfaction were calculated. Factors with a P-value of ≤0.1 from the univariate model were utilized to construct a multivariate model.
Results
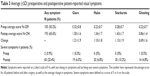
Two hundred and ninety-four patients were identified, including 134 females (45.6%), with an average age of 52.5±4.5 years (Table 1). One hundred and sixty-nine of these patients (57.5%) trialed monovision with contact lenses prior to their LASIK procedure; the remainder trialed monovision in clinic and found it acceptable or had been using monovision in their habitual correction. Eighty-two patients (27.9%) also underwent LASIK for the distant eye for hypermetropia, with a good preoperative uncorrected acuity but symptoms of eyestrain when not wearing correction. Near eye treatment was performed in the right eye in 165 patients (56.1%). The near target range ranged from −1 to −2.25, with a mean of −1.48 (IQR 0.3). Postoperative refraction and acuity data for treated near and distance targets are outlined in Table 2.
  | Table 1 Demographic information |
In patients with recorded postoperative near reading acuity, near acuity improved to 20/40 or better in 88.9% (n=184 of 207 patients with recorded near acuity) as compared to 4.7% (n=9) preoperatively (Figure 1). The final uncorrected distance visual acuity (UCDVA) in the distant eye (including both treated and untreated eyes) was 20/20 or better in 89.8% (n=265) and 20/25 or better in 98.3% (n=289). Of the 273 near eyes for which BCVA was available at one month, 1.1% (n=3) of patients gained ≥2 lines of best-corrected acuity, 6.2% (n=17) gained 1 line, 66.3% (n=181) had no change, 32.2% (n=88) lost 1 line, and 0.7% (n=2) lost ≥2 lines. Of those patients who lost two or more lines, one lost two lines and one lost three lines, with a final BCVA of 20/32 in both cases. Both patients reported they were satisfied with their vision at one month.
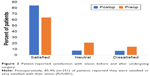
Preoperatively, 221 of 294 patients (75.2%) answered questions pertaining to visual satisfaction, and all patients answered at month 1. Preoperatively, 64.7% (n=143) of patients reported they were satisfied or very satisfied with their vision. Postoperatively, 85.4% (n=251) of patients reported they were satisfied or very satisfied with their vision (Figure 2), an increase that was statistically significant (P=0.001). Eighty-nine percent (n=262) of patients would recommend the experience, 84.0% (n=247) felt that it improved their life and 87.8% (n=258) stated that they would have the procedure again.
Patients answered questions pertaining to their level of difficulty with driving, sports and hobbies (Figure 3). There was an increase in reported difficulty with driving from preoperatively to postoperatively, with 86.0% (n=194) reporting little to no difficulty with driving preoperatively and 71.1% (n=209) reporting little to no difficulty postoperatively, P<0.001. The reverse was true for hobbies and sports, with more patients reporting little to no difficulty postoperatively than preoperatively (P<0.001 for both).
Patients reported an increase in visual symptoms in all four categories postoperatively as compared to preoperatively (Table 3). Preoperatively, only two patients reported any severe or very severe visual symptoms, whereas 60 patients reported at least one severe or very severe symptom postoperatively (P<0.001).
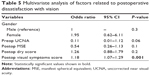
A logistic regression was performed to determine whether there were any significant factors related to patient dissatisfaction after surgery. In the univariate model, preoperative uncorrected near acuity, postoperative MSE, postoperative dry symptoms and postoperative visual symptoms were significantly related to patient satisfaction (Table 4). In the multivariate model (Table 5), only postoperative visual symptoms were significant (OR for dissatisfaction 1.18 for every unit increase in visual symptoms score, P=0.001). Postoperative MSE in the near eye correlated with visual symptoms (correlation coefficient =−1.85, 95% CI −2.75 to −0.95, P<0.001); however, in the multivariate model, only visual symptoms were a significant predictor of postop dissatisfaction. Ninety-eight percent (n=96) of patients who reported zero visual symptoms were satisfied as compared with 0% (n=6) of patients who reported severe symptoms in all categories (Figure 4). There were no other significant relationships with other factors analyzed, including preoperative visual satisfaction, preoperative visual symptoms, preoperative dry eye, preoperative and postoperative refraction and change in refraction. There was no correlation between age or near target and patient dissatisfaction with vision (P>0.5 for both).
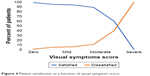  | Figure 4 Patient satisfaction as a function of visual symptom score. |
Discussion
Presbyopia remains a significant challenge in refractive surgery. Although there are many new options for treatment, including corneal inlays and refractive lens exchange with multifocal or accommodating IOLs, monovision remains the treatment with the longest track record.11–13 More specifically, LASIK monovision has been shown to be safe and efficacious; however, there seems to be some tradeoff of the extended range of vision for stereo acuity and contrast acuity.14
In this study, we investigated monovision LASIK specifically in emmetropic presbyopic patients. These patients had excellent uncorrected visual acuity and underwent LASIK with the goal of treating their presbyopia. As these patients were either emmetropic or mildly hyperopic, all treatments performed in this study were hyperopic treatments. Hyperopic treatments have been shown to be less reliable than myopic treatments, but they match the visual and safety outcomes reported here.15
This patient cohort is one of the most demanding that a refractive surgeon will encounter in their practice, and in this study did well with good refractive results and high levels of satisfaction. Previous studies have similarly shown increased postoperative satisfaction with presbyopic correction in emmetropes.16–18 We found that 85% of patients were satisfied with their vision at 1 month as compared to 65% preoperatively and found an increase in near acuity to 20/40 or better in 89.8% of patients. Patients reported an increased ability to play sports and perform near work in hobbies.
We also found an increase in patient-reported difficulty with driving, as well as an increase in visual phenomena, including glare, halos, starbursts and ghosting. Patients who experienced these symptoms were more likely to report dissatisfaction with their vision than those who did not. Unfortunately, there were no preoperative predictors of patient dissatisfaction that we found that might be used to screen patients more likely to end up unhappy. However, the number of patients dissatisfied with their vision was small (21 patients), which likely hampered our ability to find significant contributors.
Interestingly, a significant number of patients (46.5%) opted to not undergo a contact lens trial prior to undergoing monovision. We found no correlation between having undergone a contact lens trial and postoperative patient satisfaction, indicating that a trial may not always be necessary prior to surgery. This is similar finding to that of Reilly et al, who found no correlation between a contact lens trial and desire for reversal of monovision.19 However, as this is a retrospective study, it is possible that some of these patients had previously undergone a monovision and therefore opted out, which would not have been captured in this dataset.
The increase in visual symptoms as well as driving difficulty that we saw may be attributable to either the imbalance induced by the monovision correction or inherent to the hyperopic LASIK procedure itself. A previous study compared visual symptoms after monovision LASIK in myopic and hyperopic patients, and found hyperopic patients had more visual symptoms than their myopic counterparts.20 Data on patient-reported visual symptoms after hyperopic LASIK are scant. The PROWL studies included hyperopes, but these were a very small percentage of the entire cohort and a specific subanalysis was not conducted.10 It has been described that monovision decreases stereo acuity and low-contrast vision,14 with an effect that increases with increasing refractive difference between the eyes.21 A direct comparison with monovision LASIK in myopic eyes would thus be useful in elucidating the source of these symptoms.
Limitations of this study include its retrospective nature and short follow-up. The PROWL-1 study demonstrated a decrease in visual phenomena between the three- and six-month visits and did not include a one-month time point of evaluation.10 It is possible that those patients in this study may have an improvement in bothersome visual phenomena or neuroadaptation to monovision with time, as has been previously demonstrated.22,23
Conclusion
We present a large retrospective study of LASIK monovision for presbyopic correction in a population of emmetropes, which demonstrates procedural safety and visual success. Postoperative symptomatology was shown to be associated with overall procedural dissatisfaction.
Data availability
Data are available upon reasonable request to the corresponding author.
Acknowledgments
The authors thank Catherine Oldenburg, PhD, of the F.I. Proctor Foundation, University of California, San Francisco, for her assistance with the statistical methods. This study was supported by departmental funds from the Department of Ophthalmology at the University of California, San Francisco. The Department of Ophthalmology at the University of California, San Francisco, is supported by an unrestricted grant from Research to Prevent Blindness.
Author contributions
MYP – data analysis, drafting of manuscript. JMS – study conceptualization, data analysis, critical revision of manuscript. SJS – study conceptualization, critical revision of manuscript. SH – study conceptualization, critical revision of manuscript. DT – data acquisition, critical revision of manuscript. The authors certify that they have agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
Julie M Schallhorn – consulting fees from Avellino Labs, unrelated to this work. Steve J Schallhorn – consultant to Optical Express, which provided the data, Medical Director of Carl Zeiss Meditech, USA. Stephen Hannan – employee of Optical Express. David Teenan – employee of Optical Express. The other author reports no conflicts of interest in this work.
References
Lindstrom RL, Macrae SM, Pepose JS, Hoopes PC. Corneal inlays for presbyopia correction. Curr Opin Ophthalmol. 2013;24(4):281–287. | ||
Pallikaris IG, Panagopoulou SI. PresbyLASIK approach for the correction of presbyopia. Curr Opin Ophthalmol. 2015;26(4):265–272. | ||
Reinstein DZ, Carp GI, Archer TJ, Gobbe M. LASIK for presbyopia correction in emmetropic patients using aspheric ablation profiles and a micro-monovision protocol with the Carl Zeiss Meditec MEL 80 and VisuMax. J Refract Surg. 2012;28(8):531–541. | ||
Venter JA, Pelouskova M, Bull CE, Schallhorn SC, Hannan SJ. Visual outcomes and patient satisfaction with a rotational asymmetric refractive intraocular lens for emmetropic presbyopia. J Cataract Refract Surg. 2015;41(3):585–593. | ||
Garcia-Gonzalez M, Teus MA, Hernandez-Verdejo JL. Visual outcomes of LASIK-induced monovision in myopic patients with presbyopia. Am J Ophthalmol. 2010;150(3):381–386. | ||
Braun EH, Lee J, Steinert RF, Monovision In L. Monovision in LASIK. Ophthalmology. 2008;115(7):1196–1202. | ||
Levinger E, Trivizki O, Pokroy R, Levartovsky S, Sholohov G, Levinger S. Monovision surgery in myopic presbyopes: visual function and satisfaction. Optom Vis Sci. 2013;90(10):1092–1097. | ||
Ayoubi MG, Leccisotti A, Goodall EA, Mcgilligan VE, Moore TC. Femtosecond laser in situ keratomileusis versus conductive keratoplasty to obtain monovision in patients with emmetropic presbyopia. J Cataract Refract Surg. 2010;36(6):997–1002. | ||
Jain S, Ou R, Azar DT. Monovision outcomes in presbyopic individuals after refractive surgery. Ophthalmology. 2001;108(8):1430–1433. | ||
Eydelman M, Hilmantel G, Tarver ME, et al. Symptoms and Satisfaction of Patients in the Patient-Reported Outcomes with Laser in Situ Keratomileusis (PROWL) Studies. JAMA Ophthalmol. 2017;135(1):13–22. | ||
Goldberg DB. Laser in situ keratomileusis monovision. J Cataract Refract Surg. 2001;27(9):1449–1455. | ||
Finkelman YM, Ng JQ, Barrett GD. Patient satisfaction and visual function after pseudophakic monovision. J Cataract Refract Surg. 2009;35(6):998–1002. | ||
Greenbaum S. Monovision pseudophakia. J Cataract Refract Surg. 2002;28(8):1439–1443. | ||
Alarcón A, Anera RG, Villa C, Jiménez del Barco L, Gutierrez R. Visual quality after monovision correction by laser in situ keratomileusis in presbyopic patients. J Cataract Refract Surg. 2011;37(9):1629–1635. | ||
Varley GA, Huang D, Rapuano CJ, et al. LASIK for hyperopia, hyperopic astigmatism, and mixed astigmatism: a report by the American Academy of Ophthalmology. Ophthalmology. 2004;111(8):1604–1617. | ||
Dexl AK, Seyeddain O, Riha W, et al. One-year visual outcomes and patient satisfaction after surgical correction of presbyopia with an intracorneal inlay of a new design. J Cataract Refract Surg. 2012;38(2):262–269. | ||
Tomita M, Kanamori T, Waring GO, Got W, et al. Simultaneous corneal inlay implantation and laser in situ keratomileusis for presbyopia in patients with hyperopia, myopia, or emmetropia: six-month results. J Cataract Refract Surg. 2012;38(3):495–506. | ||
Alfonso JF, Fernández-Vega L, Valcárcel B, Ferrer-Blasco T, Montés-Micó R. Outcomes and patient satisfaction after presbyopic bilateral lens exchange with the ResTOR IOL in emmetropic patients. J Refract Surg. 2010;26(12):927–933. | ||
Reilly CD, Lee WB, Alvarenga L, Caspar J, Garcia-Ferrer F, Mannis MJ. Surgical monovision and monovision reversal in LASIK. Cornea. 2006;25(2):136–138. | ||
Goldberg DB. Comparison of myopes and hyperopes after laser in situ keratomileusis monovision. J Cataract Refract Surg. 2003;29(9):1695–1701. | ||
Hayashi K, Yoshida M, Manabe S, Hayashi H. Optimal amount of anisometropia for pseudophakic monovision. J Refract Surg. 2011;27(5):332–338. | ||
Azuma M, Yabuta C, Fraunfelder FW, Shearer TR. Dry eye in LASIK patients. BMC Res Notes. 2014;7:420. | ||
Levitt AE, Galor A, Weiss JS, et al. Chronic dry eye symptoms after LASIK: parallels and lessons to be learned from other persistent post-operative pain disorders. Mol Pain. 2015;11:21. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.