Back to Journals » International Journal of General Medicine » Volume 11
Mini-laparoscopic cholecystectomy with the MiniLap® percutaneous surgical system: a series of 32 patients
Authors Sapalidis K , Kosmidis C , Michalopoulos N, Laskou S , Pavlidis E , Mantalovas S, Giannakidis D , Amaniti A , Koulouris C, Katsaounis A, Munteanu AC, Surlin V , Zarogoulidis P, Kesisoglou I
Received 30 April 2018
Accepted for publication 25 July 2018
Published 20 September 2018 Volume 2018:11 Pages 369—371
DOI https://doi.org/10.2147/IJGM.S172655
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Konstantinos Sapalidis,1 Christoforos Kosmidis,1 Nikos Michalopoulos,1 Stylianni Laskou,1 Efstathios Pavlidis,1 Stelios Mantalovas,1 Dimitrios Giannakidis,1 Aikaterini Amaniti,1 Charilaos Koulouris,1 Athanasios Katsaounis,1 Alexandru C Munteanu,1 Valeriou Surlin,1 Paul Zarogoulidis,2 Isaak Kesisoglou1
1Third Department of Surgery, AHEPA Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece; 2Pulmonary-Oncology Department, “Theageneio” Cancer Hospital, Thessaloniki, Greece
Background: In recent years, mini-laparoscopic procedures are gaining the preference of most surgeons due to their potentially better surgical outcomes. The Mini Lap Percutaneous Surgical System with MiniGrip® Handle is currently the less invasive instrument and can be applied to a wide range of operations. The current paper presents its application on percutaneous laparoscopic cholecystectomy.
Materials and methods: From January 2017 to June 2017, 32 patients underwent percutaneous laparoscopic cholecystectomy with the MiniLap® system. All operations were performed by the same surgical team.
Results: No conversions and no overall complications were reported. Drainage were not necessary. Mean surgical time was 35 minutes, while patients were released in <24 hours after the operation.
Conclusion: The MiniLap system with the use of the mini grip handle seems to sustain the benefits of performing laparoscopically. However, further trials should be conducted so as to establish its safety on cholecystectomies.
Keywords: cholecystectomy, minimally invasive surgery, MiniGrip handle, percutaneous cholecystectomy, mini-laparoscopy
Introduction
Laparoscopic cholecystectomy (LC) is the procedure of choice for symptomatic cholelithiasis. The advantages of LC, compared to the open procedure, are well described and include decrease postoperative pain, shortened hospital stay, early return to activity, improved cosmesis, and patient’s complete satisfaction.1 Traditionally, LC employs 4 ports. Recently, modified techniques to perform LC have been proposed to make the procedure less invasive, to cause less postoperative pain, and to improve cosmesis. Such procedures include single-incision LC, natural orifice transluminal endoscopic cholecystectomy, and mini-laparoscopic cholecystectomy (MLC).2–4
The aim of this study was to evaluate the efficiency and the safety of MLC. MLC employs smaller instruments in contrast to LC and has been associated with potentially decreased postoperative pain and improved cosmetic outcome, pulmonary function, and overall patient satisfaction in elective cases of cholecystectomy.5,6
Materials and methods
Thirty-two patients with symptomatic cholelithiasis consented to undergo MLC with MiniLap System (Teleflex Incorporated, Morrisville, NC, USA) and the MiniGrip® Handle (Teleflex Incorporated). All procedures were performed by the same operating team. The study was approved by the Investigational Review Board of our institution “Aristotle University of Thessaloniki”, and written informed consent was obtained from the patients. Entry into the abdomen was achieved under direct visualization, a 10 mm Hasson trocar was placed, and pneumoperitoneum was created. After insufflations, a 30° Camera was inserted, and an initial diagnostic laparoscopy was performed. Afterwards, a second 10 mm trocar was introduced in the subxyphoid area and a MiniGrip® handle in the right epigastrium. The integrated needle tip allowed direct insertion through the skin so that a 5 mm trocar was eliminated. The next steps are the same as the conventional LC. The gallbladder was retrieved through the 10 mm umbilical port. The fascia was closed with 0-polyglactin (Vicryl™, Ethicon Inc., Bridgewater, NJ, USA). Subcuticular suturing was used for the incisions of the trocars, while the percutaneous access site was closed with Steri-Strips™ (3M, St. Paul, MN, USA) only. Patients were discharged after meeting standard criteria, including adequate pain control management and resumption of oral intake. All of them were followed up 1 month and 3 months postoperatively. Data were collected prospectively.
Results
From January 2017 to June 2017, 32 MLCs with the MiniLap Percutaneous Surgical System with MiniGrip® Handle were performed. Female patients outweighed male with a ratio 27:5. Mean age was 57.2±5 years, and mean body mass index was 26 (18–30) kg/m2. All patients were diagnosed as cholelithiasis, none experienced cholecystitis or any other signs of inflammation. Patients were preoperatively assessed and classified as low-risk patients (American Society of Anaesthesiologists I and II).
As far as the operation was concerned, mean surgical time was 35 minutes. It should also be mentioned that the first 2 MLCs lasted 60 and 48 minutes, respectively. No patient required conversion to an open procedure, and there were no intraoperative complications. Drainages were not used. Within 24 hours postoperatively, patients were discharged from hospital. Within the established 1-month and 6-month follow-up intervals, clinical examination and scar evaluation were assessed. No cases of postoperative complication due to surgical technique were marked. In 25 of the 32 patients (78%), the percutaneous access site was almost invisible even the first postoperative day (Figure 1) and 1 week later (Figure 2).
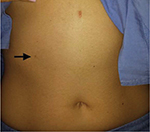  | Figure 1 Cosmetic result right after surgery. Note: The arrow indicates where the MiniLap trocar was inserted. |
  | Figure 2 Cosmetic result 1 week postoperatively. Note: The arrow indicates where the MiniLap trocar was inserted. |
Discussion
MC represents a technological advancement of laparoscopic surgery and is a safe and technically feasible alternative for the treatment of gallstone disease. The main contraindication for MLC is acute cholecystitis. Mini-laparoscopic instruments are thin, and the use of 3 mm graspers on thickened and inflammatory gallbladder walls potentially leads to frequent perforation of the gallbladder with contamination of the operative field.7 Mini-laparoscopy can be proposed for approximately 50% of patients undergoing elective cholecystectomy. Antecedent abdominal surgery is not a limitation for this approach.8
Leggett et al11 in 2000 performed, successfully, MLC with the insertion of 3 laparoscopic ports, while Unger et al12 performing less invasively, reported successful MLC with port sizes as small as 2 mm. Many modifications for micro-laparoscopies exist. In the present paper, the MiniLap System with the MiniGrip® Handle was used, making the procedure advantageous to both surgeons and patients alike.
The MLC technique followed the same principles as an LC, allowing the surgeon to gradually perform the same operative technique as a traditional LC. The learning curve for the MiniGrip® Handle seems to range from 2 to 3 patients. Moreover, the surgeon bore the possibility of upsizing or adding additional trocars in technically difficult cases, when its continuation would have a deleterious impact on the patient.
For the patient, the benefits of the “Mini” was the smaller total volume of parietal injury, smaller total area of tension in the incisions, less somatic pain, and better cosmesis than LC.11
Conclusion
Technical innovation within surgery is a desired consequence of the quest to achieve optimum outcomes for patients. Current literature remains insufficient for the correct assessment of new minimally invasive approaches for LC.12 In this series, the efficacy and safety of MiniLap System with the MiniGrip® Handle is demonstrated. Unfortunately, we did not have a control group and this is a limitation of our study. MLC seems to be a viable option in minimizing incisions and eliminating trocars, while allowing maintenance of the basic, safe laparoscopic principles, leaving a nearly unnoticeable scar and potentially less pain.
Disclosure
The authors report no conflicts of interest in this work.
References
Ellison EC, Carey LC. Lessons learned from the evolution of the laparoscopic revolution. Surg Clin North Am. 2008;88(5):927–941. | ||
Monson JR. Advanced techniques in abdominal surgery. BMJ. 1993;307(6915):1346–1350. | ||
Chalkoo M, Ahangar S, Durrani AM, Chalkoo S, Shah MJ, Bashir MI. Mini-lap cholecystectomy: modifications and innovations in technique. Int J Surg. 2010;8(2):112–117. | ||
Vagenas K, Spyrakopoulos P, Karanikolas M, Sakelaropoulos G, Maroulis I, Karavias D. Mini-laparotomy cholecystectomy versus laparoscopic cholecystectomy: which way to go? Surg Laparosc Endosc Percutan Tech. 2006;16(5):321–324. | ||
Osborne D, Boe B, Rosemurgy AS, Zervos EE. Twenty-millimeter laparoscopic cholecystectomy: fewer ports results in less pain, shorter hospitalization, and faster recovery. Am Surg. 2005;71(4):298–302. | ||
Bisgaard T, Klarskov B, Trap R, Kehlet H, Rosenberg J. Pain after microlaparoscopic cholecystectomy. A randomized double-blind controlled study. Surg Endosc. 2000;14(4):340–344. | ||
Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I, Cholecystectomy O-Woundlaparoscopic. One-wound laparoscopic cholecystectomy. Br J Surg. 1997;84(5):695. | ||
Marescaux J, Dallemagne B, Perretta S, Wattiez A, Mutter D, Coumaros D. Surgery without scars: report of transluminal cholecystectomy in a human being. Arch Surg. 2007;142(9):823826–826827discussion. | ||
Swanstrom LL, Whiteford M, Khajanchee Y. Developing essential tools to enable transgastric surgery. Surg Endosc. 2008;22(3):600–604. | ||
Palanivelu C, Rajan PS, Rangarajan M, et al. NOTES: Transvaginal endoscopic cholecystectomy in humans-preliminary report of a case series. Am J Gastroenterol. 2009;104(4):843–847. | ||
Leggett PL, Bissell CD, Churchman-Winn R, Ahn C. Three-port microlaparoscopic cholecystectomy in 159 patients. Surg Endosc. 2001;15(3):293–296. | ||
Unger SW, Paramo JC, Perez M. Microlaparoscopic cholecystectomy. Less invasive gallbladder surgery. Surg Endosc. 2000;14(4):336–339. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
