Back to Journals » Psychology Research and Behavior Management » Volume 11
Mild and severe childhood depression: differences and implications for prevention programs in the school setting
Authors Bernaras E , Garaigordobil M, Jaureguizar J , Soroa M
Received 15 August 2018
Accepted for publication 3 October 2018
Published 12 November 2018 Volume 2018:11 Pages 581—588
DOI https://doi.org/10.2147/PRBM.S184014
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Einar Thorsteinsson
Elena Bernaras,1 Maite Garaigordobil,2 Joana Jaureguizar,3 Marian Soroa1
1Department of Developmental and Educational Psychology, Faculty of Education, Philosophy and Anthropology, University of the Basque Country, San Sebastián, Spain; 2Department of Personality, Assessment and Psychological Treatments, Faculty of Psychology, University of the Basque Country, San Sebastian, Spain; 3Department of Developmental and Educational Psychology, Faculty of Education of Bilbao, University of the Basque Country, Lejona, Spain
Purpose: The study had two goals as follows: 1) to identify the prevalence of children with mild and severe depression (MD and SD), exploring sex differences; and 2) to determine possible significant differences in adaptive and clinical variables between children with different levels of depression (absence of depression, MD, and SD).
Materials and methods: We used a sample of 420 participants aged 7–10 years (53.3% boys) enrolled in third and fourth grade of primary education, from schools in the Basque Country (Spain). The Children’s Depression Scale (CDS, self-assessment) was administered as well as six more assessment instruments.
Results: It was found that 84.2% of children had no depression, 10% had MD, and 5.8% had SD. Compared with children with depressive symptoms, participants without depression had significantly: 1) lower levels of maladjustment, stress, emotional symptoms, internalizing problems, and behavioral problems; and 2) higher levels of personal adjustment, resilience, social skills, and self-concept. In addition, children with MD had significantly lower levels of clinical maladjustment, emotional symptoms, and stress than children with SD. However, no differences were found in school maladjustment, internalizing problems, behavioral problems, personal adjustment, resilience, social skills, and self-concept between children with MD and SD.
Conclusion: The discussion emphasizes the importance of identifying children with MD and implementing universal prevention programs from an early age.
Keywords: clinical maladjustment, school maladjustment, social skills, self-concept, resilience, stress
Introduction
The WHO states that depression is the most important cause of ill health and disability.1 The different classifications of mental illness (Diagnostic and Statistical Manual of Mental Disorders, DSM-5, American Psychiatric Association)2 and the International Classification of Diseases, ICD-10, WHO, hardly distinguish adult depression from childhood depression.3 The DSM-5 has incorporated the disruptive mood dysregulation disorder into its classification. Children and young people aged 7–18 years with this disorder present chronic, severe and recurrent irritability, which can be expressed verbally and behaviorally. In major depressive disorder, reference is also made to children showing their discomfort with an irritable mood. The ICD-10 assumes that there are no differences between the characteristics of depression at early ages and in adulthood.
Although the diagnosis of childhood depression is complex, it seems obvious that children’s manifestations of distress cannot be the same as those of adults, given that their cognitive, social, and emotional evolution is in the process of development. However, Cumsille et al claimed that depressive symptoms that develop in adolescence have a considerable impact on health in adulthood.4 It is, therefore, necessary to delve into the characteristics of childhood depression and, in addition to determining the prevalence of children with serious depressive symptomatology, discover how many have less severe symptoms. Normally, the studies show data with more severe symptoms of childhood depression, but the percentages of children who have risk symptoms are barely identified, and if such symptoms are not detected and eliminated early on, they could turn into severe cases of depression in the not-too-distant future. Childhood depression requires further research due to its severe consequences in children development, such as the risk of other mental pathologies in childhood or adulthood.
Depression during childhood and adolescence is a concern and a challenge for families, educators, and health professionals, occupying a prominent place in the research on child–juvenile psychopathological disorders. Many studies warn of the high prevalence of depression at early ages.5,6 A study carried out in schools in the Basque Country, using self-reports to assess severe depression (SD), indicates prevalence rates of 4% in children aged 8–12 years.7
Depression has been linked to problems in peer relations,7–9 anxiety,6,7,10 low self-esteem/self-concept,7,11–13 low resilience,14 and poor academic performance.15,16
Rodríguez-Fernández et al claimed that the sense of belonging and acceptance within one’s youth group of friends is associated with well-being.17 Poor relations among classmates are an important stress factor, and usually leads to the emergence of socioemotional distress.8 In addition, school adjustment problems have been linked to emotional and behavioral disorders.18
Resilience is another variable that studies have related to depression. Connor and Davidson argued that resilience improves well-being and promotes recovery from stressful experiences and traumatic events.19 Niu et al found that resilience was negatively associated with depression and could mitigate the harmful effect of loneliness.14
Stress is also very closely related to depression. Stressful life events precipitate episodes of major depression.2 Such stressors are normally related to interpersonal factors or factors related to physical well-being. Some studies consider that depression and its severity should be considered in studies examining reactivity to stress.20 Zhang et al also observed that early adversity is one of the environmental factors that can increase susceptibility to depression, especially when the person is exposed to chronic stress.21 Recent stressful experiences in life are also associated with greater severity of depression.22,23
The following have been noted among the variables that predict depression: health and adaptation problems,24 lack of social support,25 adverse childhood experiences,26 low self-esteem,10,27 low resilience,26 high-level stress,22 low self-concept, and few social skills.28
Within this setting, the study has two goals as follows: 1) to identify the prevalence of children with mild depression (MD) and SD, exploring sex differences; and 2) to determine possible significant differences between children with different levels of child depression (absence of depression = NoD, MD, and SD) in clinical variables (clinical and school maladjustment, emotional symptoms, stress, internalizing/externalizing problems, and behavioral problems), and in adaptive variables (personal adjustment, self-concept, social skills, and resilience). In accordance with these goals, three hypotheses are proposed:
H1. We will find a relevant percentage of children aged 7–10 years with depressive symptoms; ~ 4% will suffer from SD and 10% from MD.
H2. Participants with no symptoms of depression will have significantly lower levels of clinical and school maladjustment, behavioral and externalizing problems, internalizing problems, stress, and other emotional symptoms than children with depression (MD and SD); furthermore, children with MD will have significantly lower levels of all these variables than children with SD.
H3. Participants without depression will have significantly higher levels of personal adjustment, self-concept, social skills, and capacity for resilience compared with those who manifest depressive symptoms (MD and SD).
Materials and methods
Participants
The sample comprised 420 students from schools of the Basque Country (Spain): 53.3% were boys (n=224) and 46.7% were girls (n=196). They were aged 7–10 years: a total of 59.5% (n=250) were between 7 and 8 years and 40.5% (n=170) were between 9 and 10 years of age. The sample was made up of students of third and fourth grade of primary education: a total of 52.6% (n=221) studied in third grade and 47.4% (n=199) in the fourth grade. The sample was selected intentionally by balancing public and private/concerted schools: 53.6% (n=225) from public schools, 46.4% (n=195) from private/concerted schools.
Assessment instruments
Children’s Depression Scale (CDS)
It is a self-report questionnaire to assess depressive symptoms in children, with 66 statements rated on a 5-point scale according to the degree of agreement with the content of the sentence (1= disagree strongly; 5= strongly agree).29 The internal consistency of the test in its Spanish adaptation was analyzed by the Kuder–Richardson 20 formula, yielding an index of 0.91, which indicated a good level of internal consistency. Cronbach´s alpha in this study was 0.88. Significant correlations between the score in the CDS and personality instability show concurrent validity.
Spanish adaptation of the Behavior Assessment System for Children and Adolescents (BASC-S2)
In its self-report form, it is composed of 146 sentences to be answered on a True/False scale.30,31 It consists of clinical scales (negative attitude to school, negative attitude to teachers, atypicality, external locus of control, social stress, anxiety, depression, and sense of incapacity) and adaptive scales (interpersonal relations, relations with parents, self-esteem, and self-confidence). The global indices of the BASC-S2 are clinical maladjustment, school maladjustment, personal adjustment, and emotional symptoms index. BASC-S2 showed good internal consistency (Cronbach’s alpha between 0.70 and 0.80), and the Cronbach’s alpha in this study was highest (α=0.92). The validity was evidenced by the high correlations found between the index of emotional symptoms and the general maladjustment, clinical maladjustment, and personal maladjustment in the TAMAI (Multifactor Self-Assessment Test of Child Adjustment), as well as between the school maladjustment and school mismatch of the TAMAI.
Screening for Children’s Emotional and Behavioral Problems (SPECI, Teacher)
Teachers answer this questionnaire in relation to each of their students.32 They are asked to specify the frequency with which they detect emotional and behavioral problems in their students on a 3-point scale (0= not at all, 1= fairly, 2= very much). Each emotional and behavioral problem is explained by an illustrative example (eg, “Withdrawal: He/she is withdrawn and inhibited, prefers to be alone and seems isolated; not very active and reserved in his/her relation with others”). The SPECI assesses internalizing problems (withdrawal, somatization, anxiety, infantile dependence, thought problems, and depression) and externalizing problems (attention-hyperactivity, disruptive behavior, academic achievement, and violent behavior). The internal consistency obtained with the original sample was adequate (α=0.82), in the same direction as that obtained with the sample of the present study (a=0.89). Multivariate analysis of variance (MANOVA) results found differences between the participants with and without clinical problems in the set of the categories diagnosed by the SPECI (Trace of Pillai =0.298, F1, 1270 = 49.99, P<.001), with a large effect size (η2=0.298; r=0.54), that confirmed the criterion validity of SPECI.
“Inventario de estrés cotidiano infantil” (IECI, inventory of daily stress in children)
This self-report questionnaire assesses daily stress (health/psychosomatic problems, stress in school setting, and stress in family environment), by 22 sentences that must be answered “Yes” or “Not”.33 The internal consistency for the global stress variable with the original study sample was adequate (a=0.81), and similar to the sample in this study (a=0.73). The tests of external validity showed positive and significant relationships with socioemotional maladjustment, anxiety, anger, and depression and negative relationships with personal adaptation, interpersonal relationships, self-esteem, and self-confidence.
Cuestionario de Autoconcepto (CAG, self-concept questionnaire)
The CAG is a self-report questionnaire to measure global self-concept, as well as its different dimensions (physical self-concept, social self-concept, intellectual self-concept, family self-concept, personal self-concept, and sense of control).34 It consists of 48 statements in which the participants are asked to rate the degree to which they can self-apply the content of the sentences on a 5-point scale (1= Never, 2= Not often, 3= Do not know, 4= Often, and 5= Always). In the original sample, the test showed adequate internal consistency (a=0.87), and the Cronbach’s alpha in this study was 0.74. The validity was confirmed through the significant correlations found between the scores in this test and those obtained in other tests of self-concept and self-esteem.
Social Skills Improvement System
It is 75-item self-report questionnaire to assess social skills (communication, cooperation, assertiveness, responsibility, empathy, self-control, and involvement/participation) and problem behaviors (externalizing, bullying, inattention-hyperactivity, and internalizing).35 The respondents are asked to rate the degree of agreement with the content of the items through four response options (Not true, Not very true, Fairly true, and Very true). Internal consistency with the original sample of the test was confirmed as Cronbach’s alpha coefficients were ≥0.70 at all scales. Cronbach’s alpha for the scales of the instrument in this study was between 0.98 and 0.99. Correlations with another test (BASC-S2) measuring similar constructs were adequate (0.64–0.80), confirming their criterion validity.
The Resiliency Scales for Children and Adolescents
This resiliency rating questionnaire is a self-report questionnaire with 64 statements in which the respondents are asked to indicate the frequency with which they have the thought, feeling, or behavior on a 4-point scale (0= Never, 1= Rarely, 2= Sometimes, 3= Often, and 4= Almost always).36 The questionnaire assesses three dimensions: sense of competence (optimism, self-efficacy, and adaptability), sense of affiliation (sense of affiliation, self-confidence, support, comfort, and tolerance), and emotional reactivity (sensitivity, recovery, and alteration). The Cronbach’s alpha coefficients of the original sample (sense of competence, a=0.85, sense of affiliation, a=0.90, and reactivity, a=0.90) were high, in the same direction as those obtained in this study (sense of competence, a=0.84, sense of affiliation, a=0.89, and reactivity, a=0.90). The validity was evidenced by comparisons between control groups (without problems) and clinically diagnosed groups, confirming that those in the control group obtained higher scores in both scales.
Procedure
The research project was explained to the selected schools; first, in a letter and second, in a scheduled interview with the headmasters. Next, the informed consent forms for parents and/or legal guardians were requested. We administered the assessment instruments to the participants in the classrooms in two 45-minute assessment sessions, on successive days, and the teachers were asked to fill the SPECI with regard to each student. The study met the ethical values required in research with human beings, respecting the fundamental principles included in the Declaration of Helsinki: informed consent signed by the parents or legal guardians and right to information, protection of personal data, and guarantees of confidentiality, non-discrimination, gratuity, and the possibility of dropping out of the study in any of its phases. The study was approved by the Commission of Research Ethics of the University of the Basque Country (CEISH/266MR/2014).
Data analysis
After calculating the norms obtained with the CDS scores, we classified the sample according to varying degrees of depression: Absent (NoD =≤ percentile 84), MD (85–94 percentile), and SD (≥ percentile 95). Then, we conducted ANOVA, MANOVA, and post hoc (Bonferroni) analyses in the studied variables to determine possible differences in clinical and adaptive variables between the three groups. The effect size (partial squared Eta) is interpreted according to the parameters as follows: a total of 0.01 was considered to be small effect size; 0.06 medium or moderate effect size; and 0.14 large effect size.
Results
Prevalence: percentage of students who suffer MD and SD
The results showed that 84.2% had no depression (n=351), 10% had MD (n=42), and 5.8% had SD (n=24). The percentage of boys and girls in each group was as follows: NoD: a total of 43.6% boys and 40.5% girls; MD: a total of 7% boys and 3% girls; and SD: a total of 3.1% boys and 2.6% girls. The differences between the sexes were nonsignificant (χ2=4.46, P=0.107), although the percentage of boys with MD was slightly higher.
Degrees of depression and relationship with clinical/adaptive variables, emotional/behavioral problems, and childhood stress
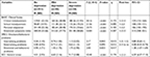
The results of the MANOVA performed on the 12 variables assessed with the BASC yielded significant differences between the three groups, BASC Λ=0.662, F (32, 796)=5.68, P<0.001, with a large effect size (η2=0.186, r=0.43). The ANOVA (Table 1) confirmed that the NoD group had lower levels of clinical maladjustment (anxiety, external locus of control, and atypicality) and fewer emotional symptoms (anxiety, sadness, loneliness, negative interpersonal relationships, social stress, low self-esteem, and feelings of incapacity) than the MD and the SD groups; also, the MD group had significantly lower levels of these variables than the SD group. In school maladjustment (negative attitude toward school and teachers) and personal adjustment (interpersonal relationships, relations with parents, self-confidence, and self-esteem), the NoD group was significantly better than the groups of children with depression, but there were no differences between the MD and the SD groups.
The results of the MANOVA carried out with the 10 variables assessed with the SPECI, filled in by the teachers, showed significant differential tendencies between the three groups, SPECI Λ=0.978, F (4, 812)=2.29, P<0.058, with a medium effect size (η2=0.011, r=0.10). The ANOVA (Table 1) confirmed that the NoD group had significantly fewer internalizing problems (withdrawal, somatization, anxiety, infantile dependence, thought problems, and depression) than the SD group. However, no differences were found in internalizing problems between the NoD and MD groups or between the MD and SD groups. No differences were found in externalizing problems between the three groups.
The results of the MANOVA carried out with the three variables evaluated with the IECI revealed significant differences between the three groups, IECI Λ=0.822, F (6, 820)=14.10, P<0.001, with a medium effect size (η2=0.094, r=0.30). The ANOVA (Table 1) confirmed that the children classified in the NoD group had significantly less general stress (health/psychosomatic problems, school and family stress) than the MD group, whereas the MD group had significantly less stress than the SD group.
In addition, as shown in Table 1, the effect size is large in some variables (clinical maladjustment, emotional symptoms index, and general stress), moderate in others (school maladjustment and personal adaptation), and small in internalizing and externalizing problems.
Degrees of depression and relationship with self-concept, social skills, and resilience
The results of the MANOVA performed with the six variables evaluated with the CAG revealed significant differences between the three groups, CAG Λ=0.799, F (12, 818)=8.10, P<0.001, with a medium effect size (η2=0.106, r=0.32). The ANOVA (Table 2) confirmed that the NoD group had a significantly better self-concept than the MD and SD groups, in which self-concept was similar.
The results of the MANOVA carried out with the 11 variables evaluated with the SSIS showed significant differences between the three groups, SSIS Λ=0.799, F (24, 806)=3.98, P<0.001, with a medium effect size (η2=0.106, r=0.32). The ANOVA (Table 2) confirmed that the NoD group had significantly more social skills (communication, cooperation, assertiveness, responsibility, empathy, engagement/participation, and self-control) than the depressed groups (MD and SD), whereas these latter groups had similar levels of social skills. Complementarily, the results confirmed that the NoD group had significantly fewer behavioral problems (externalizing – aggressive physical and verbal behavior, bullying – peer-directed aggressive behaviors, inattention-hyperactivity – easily distracted, impulsive, and excessively active, and internalizing problems – anxiety, sadness, and loneliness) than children with depression (MD and SD), whereas both groups of depressed children had similar levels of behavioral problems.
The results of the MANOVA conducted with the 10 variables evaluated with the RSCA revealed significant differences between the three groups, RSCA Λ=0.830, F (20, 810)=3.95, P<0.001, with a medium effect size (η2=0.089, r=0.29). The ANOVA (Table 2) of the variables related to resilience – sense of competence (optimism, self-efficacy, and adaptability), sense of affiliation (trust in others, perception of social support in adverse situations, and feeling comfortable with others), and emotional reactivity (vulnerability, agitation, hypersensitivity, alteration, and emotional imbalance) – revealed that the NoD group had significantly higher levels than the MD and SD groups (greater sense of competence, affiliation, and less emotional reactivity), although none of the three variables differentiated between the two depressed groups.
In addition, the effect size (Table 2) is moderate in some variables (self-concept, problem behaviors, and sense of competence), and small in others (social skills, sense of affiliation, and emotional reactivity).
A summary of the results of the present study is given in Table 3.
Discussion
The goals of the study were to identify the prevalence of children with MD and SD, exploring sex differences, and determine possible significant differences between children with different levels of self-assessed childhood depression in clinical and adaptive variables.
First, results show that a significant percentage (84.2%) of children aged 7–10 years are not depressed, 10% presented mild depressive symptomatology, and 5.8% showed severe depressive symptomatology, and no differences between the sexes were found. Therefore, Hypothesis 1 is confirmed; the percentage of children aged 7–10 years with many depressive symptoms is even slightly higher than that of the hypothesized 4%, which was based on previous studies.7 The study reveals a prevalence that is worthy of consideration, and it especially provides more information by focusing on children with MD, which has been unusual in the previous studies.
Second, the results confirm that the participants without depression, compared with those with depression, had significantly lower levels of clinical maladjustment, school maladjustment, emotional symptoms internalizing problems, stress, and behavioral problems. In addition, the MD group had significantly lower levels than the SD group in some variables (clinical maladjustment, emotional symptoms, and stress). However, in other variables (school maladjustment, internalizing problems, and behavioral problems), we found no differences between the MD and SD groups. Therefore, Hypothesis 2 is partially confirmed, as no significant differences between the three groups were found in externalizing problems (assessed by the teachers), or between the MD and SD groups in school maladjustment, internalizing problems, and behavioral problems. The results confirm studies that have linked depression to anxiety,6,7,10 poor academic performance,15,16 and stress.21–23,28
Third, results in adaptive variables show that children without depression had significantly better personal adjustment, self-concept, social skills, and resilience capacity (high capacity of competence and affiliation and low emotional reactivity) than children with depression. No differences were found between the MD and SD groups in these variables. Therefore, Hypothesis 3 is ratified. These results confirm studies that have linked depression to problems with peer relationships,8,9 low self-esteem/self-concept,7,11–13 low resilience,14,19,26 as well as studies that have found lack of social support,25 low self-concept,10,27 and few social skills to be predictors of depression.28
As a limitation of the study, we include the fact that we used a convenience sample. However, the study makes relevant contributions, which include: 1) having identified that, in addition to the 5.8% of children who suffer SD, 10% have MD, an aspect that has been little analyzed in previous studies, and also reveals an increase in the prevalence of SD; 2) increasing our understanding of childhood depression by confirming that children with symptoms of depression have high levels of clinical and school maladjustment, emotional symptoms, internalizing problems, stress, behavioral problems, and low levels of personal adjustment, self-concept, social skills, and resilience; and 3) having focused on children who have mild depressive symptoms, but who, in the light of the results, have many characteristics and problems similar to those of children with SD (eg, school maladjustment, internalizing problems, behavioral problems, personal adjustment, low self-concept, social skills, and resilience capacity), and some of these variables are indicators to identify students with depressive symptomatology.
Conclusion
These findings have important practical implications and suggest the importance of: 1) identifying children with MD, paying more attention to children who have a low self-concept, few social skills, behavioral problems, school maladjustment, and low resilience capacity; and 2) implementing universal prevention programs for childhood depression from an early age in educational settings. In the light of the results obtained, these programs should preferably encourage self-esteem/self-concept, social skills (positive social behaviors, problem solving, etc.), resilience, emotion regulation, stress control, and school adjustment. Among others, we suggest cooperative games and emotional intelligence programs that may promote the development of social and emotional skills that are related to childhood depression. Future studies should explore the development of children with MD, given its risk of becoming SD, and implement prevention programs at an early age to ensure all children’s psychological well-being.
Acknowledgment
The Research Project was sponsored by the Alicia Koplowitz Foundation with grant number FP15/62, and by the University of the Basque Country, UPV/EHU, with grant number PPG17/31.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization [webpage on the Internet]. “Depression: Let’s talk” says WHO, as depression tops list of causes of ill health. Available from: http://www.paho.org/hq/index.php?option=com_content&view=article&id=13102%3Adepression-lets-talk-says-who-as-depression-tops-list-of-causes-of-ill-health&catid=740%3Apress-releases&Itemid=1926&lang=es. Accessed March 03, 2018. | ||
American Psychiatric Association,APA. Manual diagnóstico y estadístico de los trastornos mentales (DSM-5) [diagnostic and statistical manual of mental disorders (DSM–5)]. Madrid: Médica Panamericana; 2014. | ||
World Health Organization,WHO. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Vol 1. Geneva: World Health Organization; 1992. | ||
Cumsille P, Martínez ML, Rodríguez V, Darling N. Parental and individual predictors of trajectories of depressive symptoms in Chilean adolescents. Int J Clin Health Psychol. 2015;15(3):208–216. | ||
Katz SJ, Conway CC, Hammen CL, Brennan PA, Najman JM. Childhood social withdrawal, interpersonal impairment, and young adult depression: a mediational model. J Abnorm Child Psychol. 2011;39(8):1227–1238. | ||
Kovacs M, Lopez-Duran N. Prodromal symptoms and atypical affectivity as predictors of major depression in juveniles: implications for prevention. J Child Psychol Psychiatry. 2010;51(4):472–496. | ||
Bernaras E, Jaureguizar J, Soroa M, Ibabe I, de Las Cuevas C. Evaluation of the depressive symptomatology and the related variables in the school context. An Psicol. 2013;29(1):131–140. | ||
Flanagan KS, Vanden Hoek KK, Ranter JM, Reich HA. The potential of forgiveness as a response for coping with negative peer experiences. J Adolesc. 2012;35(5):1215–1223. | ||
Hames JL, Hagan CR, Joiner TE. Interpersonal processes in depression. Annu Rev Clin Psychol. 2013;9:355–377. | ||
Wu YL, Zhao X, Li YF, et al. The risk and protective factors in the development of childhood social anxiety symptoms among Chinese children. Psychiatry Res. 2016;240:103–109. | ||
Bos AER, Huijding J, Muris P, Vogel LRR, Biesheuvel J. Global, contingent and implicit self-esteem and psychopathological symptoms in adolescents. Personal Individ Differ. 2010;48(3):311–316. | ||
Garalgordobil M, Durá A. Relaciones de autoconcepto y la autoestima con sociabilidad, estabilidad emocional y responsabilidad en adolescentes de 14 a 17 años [Relationships of self-concept and self-esteem with social behaviours and personality traits in adolescents aged 14 to 17]. Anal. Modif. Cond. 2006;32(141):37–64. | ||
Slaninova G, Stainerova M. Trauma as a component of the self-concept of undergraduates. 5th ICEEPSY International Conference on Education & Educational Psychology. 2015;171:465–471. | ||
Niu G-F, Sun X-J, Tian Y, Fan C-Y, Zhou Z-K. Resilience moderates the relationship between ostracism and depression among Chinese adolescents. Pers Individ Dif. 2016;99:77–80. | ||
Jaureguizar J, Bernaras E, Garaigordobil M. Child depression: prevalence and comparison between self-reports and teacher reports. Span J Psychol. 2017;20:E17. | ||
Orgilés, M, Gómez M, Piqueras JA, Espada JP. Relations between school performance and depressive symptoms in Spanish children. Electron J Res Educ Psychol. 2014;12(2):447–460. | ||
Rodriguez-Fernandez A, Droguett L, Revuelta L. School and personal adjustment in adolescence: the role of academic self-concept and perceived social support. Rev Psicodidact. 2012;17(2):397–414. | ||
Herman KC, Lambert SF, Reinke WM, Ialongo NS. Low academic competence in first grade as a risk factor for depressive cognitions and symptoms in middle school. J Couns Psychol. 2008;55(3):400–410. | ||
Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18(2):76–82. | ||
Harkness KL, Stewart JG, Wynne-Edwards KE. Cortisol reactivity to social stress in adolescents: role of depression severity and child maltreatment. Psychoneuroendocrinology. 2011;36(2):173–181. | ||
Zhang ZY, Mao Y, Feng XL, et al. Early adversity contributes to chronic stress induced depression-like behavior in adolescent male rhesus monkeys. Behav Brain Res. 2016;306:154–159. | ||
Plieger T, Melchers M, Montag C, Meermann R, Reuter M. Life stress as potential risk factor for depression and burnout. Burn Res. 2015;2(1):19–24. | ||
Richards D, Richardson T, Timulak L, et al. Predictors of depression severity in a treatment-seeking sample. Int J Clin Health Psychol. 2016;16(3):221–229. | ||
Wang L, Feng Z, Yang G, et al. Depressive symptoms among children and adolescents in western china: an epidemiological survey of prevalence and correlates. Psychiatry Res. 2016;246:267–274. | ||
Colman I, Zeng Y, McMartin SE, et al. Protective factors against depression during the transition from adolescence to adulthood: findings from a national Canadian cohort. Prev Med. 2014;65:28–32. | ||
Poole JC, Dobson KS, Pusch D. Childhood adversity and adult depression: the protective role of psychological resilience. Child Abuse Negl. 2017;64:89–100. | ||
Babore A, Trumello C, Candelori C, Paciello M, Cerniglia L. Depressive symptoms, self-esteem and perceived parent-child relationship in early adolescence. Front Psychol. 2016;7:982. | ||
Garaigordobil M, Bernarás E, Jaureguizar J, Machimbarrena JM. Childhood depression: relation to adaptive, clinical and predictor variables. Front Psychol. 2017;8:821. | ||
Lang M, Tisher M. Children’s depression scale. Camberwell, Victoria, Australia: Australian Council for Educational Research Hawthorn. 1983. | ||
Reynolds C, Kamphaus R. Behavior Assessment System for Children: Manual. Circle Pines, MN: American Guidance Service; 1992. | ||
González J, Fernández S, Pérez E, Santamaría P. BASC Sistema de evaluación de la conducta de niños y adolescentes. Madrid: TEA Ediciones; 2004. | ||
Garaigordobil M, Maganto C. SPECI: Screening de problemas emocionales y de conducta infantil. Madrid: TEA Ediciones; 2012. | ||
Trianes M, Blanca M, Fernández-Baena F, Escobar M, IECI ME. Inventario de estrés cotidiano infantil. Madrid: TEA Ediciones; 2011. | ||
García Torres B. CAG. Cuestionario de autoconcepto. Manual. versión 1.0. Madrid: EOS; 2001. | ||
Gresham FM, Elliott SN. Social Skills Improvement System: Rating scales manual. Minneapolis, MN: NCS Pearson; 2008. | ||
Prince-Embury S. Resiliency Scales for Children & Adolescents (RSCA). San Antonio: Pearson; 2008. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.