Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 15
Melatonin and Sleep Disturbances in Children With Atopic Dermatitis
Authors Dwiyana RF , Nuraeni L , Diana IA, Effendi RMRA , Gondokaryono SP , Ruchiatan K , Hindritiani R , Gunawan H
Received 17 March 2022
Accepted for publication 1 June 2022
Published 27 June 2022 Volume 2022:15 Pages 1175—1182
DOI https://doi.org/10.2147/CCID.S366854
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jeffrey Weinberg
Reiva Farah Dwiyana, Lita Nuraeni, Inne Arline Diana, Raden Mohamad Rendy Ariezal Effendi, Srie Prihianti Gondokaryono, Kartika Ruchiatan, Reti Hindritiani, Hendra Gunawan
Department of Dermatology and Venereology, Faculty of Medicine, Universitas Padjadjaran-Dr. Hasan Sadikin Hospital, Bandung, West Java, Indonesia
Correspondence: Reiva Farah Dwiyana; Lita Nuraeni, Department of Dermatology and Venereology, Faculty of Medicine, Universitas Padjadjaran - Dr. Hasan Sadikin Hospital, Jl. Pasteur 38, Bandung, West Java, 40161, Indonesia, Email [email protected]; [email protected]
Objective: To evaluate the correlation between melatonin levels and sleep quality, based on the Children’s Sleep Habit Questionnaire (CSHQ), among children with atopic dermatitis (AD).
Methods: This was an analytic study with a cross-sectional design involving two groups, AD children as the case group and participants without AD as the control group, conducted at the Pediatric Dermatology Clinic of Dr. Hasan Sadikin Hospital, Bandung, Indonesia. Melatonin levels and CSHQ score in the case group were compared to that in the control group. Correlation analysis was performed between melatonin levels and sleep quality based on CSHQ in the case group.
Results: Participants in this study consisted of 19 children with moderate AD, (no patient with mild and severe AD was recruited), and 19 participants without AD. The mean CSHQ score in the case group was significantly higher than the control group (47.84 vs 36.79; p< 0.05). The mean melatonin level in the case group was significantly lower than the control group (320.18 pg/mL vs 383.86 pg/mL; p< 0.05). Comparative analysis was conducted using independent t-test. There was a significant Pearson’s correlation index between SCORAD and CSHQ (p< 0.05). However, there was no correlation between melatonin levels and CSHQ, as well as between melatonin levels and SCORAD (p< 0.05).
Conclusion: Children with moderate AD have impaired sleep quality and lower melatonin levels compared to controls. No correlation was found between melatonin levels and CSHQ, as well as melatonin levels and SCORAD, although there was a strong and significant correlation between SCORAD and CSHQ. Therefore, melatonin levels may not be the main cause of sleep disturbances in children with moderate AD.
Keywords: atopic dermatitis, CSHQ, melatonin, SCORAD
Introduction
Atopic dermatitis (AD; atopic eczema – AE) is a chronic, recurrent, common inflammatory skin disease, characterized by periods of exacerbation and remission. The disease manifests itself as an intense itching accompanied by skin lesions of an eczematous morphology (acute, subacute or chronic), whose location depends on the patient’s age. In children the lesions are found in the flexural folds of the extremities.1,2 The pathogenesis of AD is not fully understood.3,4 Atopic dermatitis is thought to be influenced by genetic and environmental factors, as well as immunological and skin barrier disorders.4,5 Clinical manifestations of AD can be accompanied by itching that often occurs at night, referred to as nocturnal pruritus.5 This cause sleep disturbances in children with AD, which can result in behavioral problems, emotional disturbances, and learning difficulties.5,6 Sleep disturbances in children with AD are thought to be influenced by various factors, including changes in cortisol secretion patterns, abnormal melatonin production, high levels of proinflammatory cytokines, and increased transepidermal water loss (TEWL), which are influenced by the circadian rhythm (CR).7 Sleep loss is an undisputed feature of AD, which must be taken into account when in assessing disease severity using the Scoring Atopic Dermatitis (SCORAD) scale.8 Sleep disturbances among AD patients is prevalent and frequently reported, especially in children with moderate-severe AD.8 Although the main symptoms of AD, such as excessive itch and the consequent scratching, seem to sufficiently explain the abnormal sleep pattern seen among patients, previous studies have reported that children with AD in remission experience significant sleep disturbances not related to scratching.9 This raises the suspicion that more complex underlying mechanisms are involved.5,10 A vast variety of interleukins, chemokines, neuropeptides, and even hormones are linked to abnormal sleep in AD.8 Another molecule which provisionally plays a crucial role in sleep disturbance in AD is melatonin.6
The circadian rhythm regulates variations in the physiological and biological rhythms in order to adapt to the changes that occur every day, including changes in the physiological functions of the skin.5,10 Melatonin is a hormone secreted by the pineal gland that is located in the epithalamus.7 This hormone has an important physiological function to regulate the circadian rhythm by inducing sleep activity.11 Melatonin secretion fluctuates following the CR and is affected by light.11 Light conditions in the bedroom during sleep can affect melatonin secretion.11 Light from electronic devices can also delay and reduce melatonin secretion.12
To date, research on melatonin levels in children with AD remains limited.8 Therefore, this study aims to analyze the correlation between melatonin levels and sleep quality, as assessed using the Indonesian version of the Children’s Sleep Habits Questionnaire (CSHQ), in children with AD.
Materials and Methods
Study Population
This study is an analytical study with a cross-sectional design that took place between May-August 2021. Nineteen patients aged from 4–10 years of either sex with moderate AD based on SCORAD, visiting the outpatient in the Pediatric Dermatology Clinics of Dr. Hasan Sadikin Hospital, Bandung, Indonesia, were selected as cases using the consecutive sampling method. Nineteen participants without AD were recruited as controls. The age limit of 4–10 years was applied, in accordance with the CSHQ as the tool for assessing sleep quality. Those suffering from neuropsychiatric diseases or scabies, have liver or kidney disorders, taking medication for insomnia or antidepressants for the past four weeks, or taking antihistamines, beta-blockers, nonsteroidal anti-inflammatory drugs, or systemic corticosteroids for the past three days were excluded. Additionally, those suffering from AD or other skin disorders and sleep disturbances were excluded from the controls.
This study was planned to include children with moderate to severe AD as subjects; however, all participants in the case group were children with moderate AD.
Study Tools
A pre-developed questionnaire for history and clinical examination was used. In the case group, severity was calculated using SCORAD with the following categories: mild < 25, moderate 25–50, and severe > 50.13 There was no consensus on normal melatonin levels. First morning urine (taken at 05.00–07.00 am) was collected from all participants. Urinary melatonin was measured using the enzyme-linked immunosorbent assay (ELISA) kit supplied by the Bioassay Technology Laboratory. Sleep quality was rated using the Indonesian version of CSHQ consisting of 33 questions that were organized into five subscales, including bedtime, sleep behavior, night awakening, morning wake time, and daytime sleepiness.14
Ethics
The study procedures were conducted in accordance with the Declaration of Helsinki. The study protocol and ethical approval were granted by the Health Research Ethics Committee of Dr. Hasan Sadikin General Hospital, Bandung, Indonesia (ethical clearance number: LB.02.01/x.6.5/111/2021). All parents were informed about the purpose of the study and informed consent was obtained prior to participation in the survey interview. Data confidentiality and participant’s privacy were strictly maintained, and participants were informed that they had the right to withdraw from the study at any time.
Statistical Analysis
All data were analyzed using the Statistical Package for Social Sciences (SPSS) version 17. All quantitative variables were estimated using measures of central location (mean, median). For normally distributed data, variables were compared using independent t-test. Qualitative variables were presented as frequencies and proportions. Correlations were determined using Pearson’s correlation coefficient and values (r) interpretation as follows: <0.20 very weak; 0.20–0.39 weak; 0.40–0.59 moderate; 0.60–0.79 strong; and ≥0.80 very strong. A p‑value of <0.05 was considered significant.
Results
The participant’s demographic and clinical characteristics are presented in Table 1. Nineteen children with moderate AD aged 4–10 years (mean±SD 7.32 ± 1.95 years; 8 males and 11 females) were included in the case group. The same number of participants without AD were included in the control group (mean age ± SD 7.16 ± 1.42 years; 12 males and 7 females). Groups had no statistical difference in age. All of the cases had moderate disease as measured with SCORAD (score 25–50).
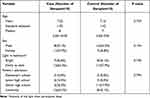 |
Table 1 Characteristic of Case and Control |
Melatonin secretion in the body is influenced by light stimulation, so all participants were asked about the condition of the room light during sleep, whether is bright or dimly to dark. In this study, seven participants from the case group and eight participants from the control group slept in a bright room, while the other participants slept in a dimly to dark rooms. The use of the word “dimly to dark” was decided because of the non-uniformity of light intensity in the participant’s bedrooms. Some of the participants who slept in a “dimly to dark” room did not turn on the light during sleep, the rest used a light sleeper with a different light intensity. The control group in this study had room light conditions during sleep that were homogeneous with the case group so that it was feasible for comparative analysis to be carried out.
Table 2 shows the differences in urinary melatonin levels and CSHQ scores between the cases and controls and their correlation with SCORAD severity. The scatterplots showing Pearson’s correlation between SCORAD and CSHQ, SCORAD and urinary melatonin, CSHQ and urinary melatonin of case group can be seen on Figure 1.
 |
Table 2 Urinary Melatonin Levels and CSHQ Scores in Cases and Controls with Their Correlation Coefficients with SCORAD and Respective P value |
 |
Figure 1 Scatterplots showing Pearson’s correlation between (A) SCORAD and CSHQ of case group, (B) SCORAD and urinary melatonin of case group, (C) CSHQ and urinary melatonin of case group. |
Table 3 compares the CSHQ subscale scores of both the case and the control groups. In the case group there was a very significant increase (p<0.01) in the sleep behavior, night awakening and daytime sleepiness subscales, and a significant increase (p<0.05) in the bedtime subscale compared to the control group.
 |
Table 3 Comparison of CSHQ Subscale Scores Between Case and Control Groups |
Table 4 shows the correlation between urinary melatonin levels and CSHQ score. The mean level of urinary melatonin was 320.18 pg/mL and 383.86 pg/mL, in the case and control group, respectively. The mean CSHQ score in the case group was 47.84, whereas in the control group it was 36.79, with a statistically significant difference (p<0.05). There was a very strong significant correlation between SCORAD and CSHQ scores (r=0.991 and p-value<0.01). However, none of the parameters had a statistically significant correlation with melatonin.
 |
Table 4 Urinary Melatonin Levels with Correlation Coefficients with CSHQ Scores in Cases and Respective P values |
Discussion
Sleep is the essential functional state of the central nervous system and its disorders result in unfavourable psychosocial and economic consequences in AD patients (eg, lower material status, concentration disorders, increased number of visits to the doctor).15,19 Sleep disturbance is frequently reported in AD patients.16 There are several measurement tools that can be used to assess sleep quality, including polysomnography (PSG), electroencephalography (EEG), actigraph, and sleep assessment questionnaires. Among these, PSG, EEG, and actigraph can assess sleep disturbances objectively, while questionnaires are more subjective.17 In contrast to other tests that require special tools and experts for interpretation, assessment of sleep quality using a questionnaire is cheaper and more practical to use.18 In this study, sleep quality was evaluated using the Indonesian version of the CSHQ. The control and case groups in this study had homogeneous characteristics of age, sex, and room light conditions during sleep, and thus it was feasible to do a comparative analysis. Sleep quality was assessed on all study participants, which involved completion of the questionnaire by the parents of the study participants, accompanied by the researcher.
The average CSHQ score were 47.84±6.96 and 36.79±2.79 in the case and control group, respectively. There was a highly significant difference in mean CSHQ score (p<0.01) between the case group and the control group. A CSHQ score of >41 indicates a disturbance in sleep quality,14,18 indicating a significant decrease in sleep quality in the case group compared to the control group. Similar findings were reported by a 2016 Latin-American study by Pereira et al, where a decrease in sleep quality based on CSHQ score was observed in children with AD, especially in patients with moderate-severe cases compared to the controls.16 Children with AD have a higher risk of sleep disturbances compared to participants without AD. About 50–80% of pediatric AD patients and 30–90% of adults AD patients have sleep disturbances.17,19,20 The causes of sleep disorders in AD are very complex,8 one of them being severe itch at night associated with an increase in TEWL and decrease in sebum during that time.5 In addition, sleep disturbances in AD are thought to be associated with decreased melatonin levels due to low interferon gamma (IFN-ɣ).21
In our study, the case group had more irregular sleep behavior, shorter sleep duration, more frequent awakenings at night, and more daytime sleepiness compared to the control group. Sleep disturbances will affect emotions and learning abilities of children with AD. Children who have trouble sleeping at night will experience sleepiness during the day and this will affect their quality of life. Children with severe AD are known to have lower achievements in school than non-DA children.22 This is partly influenced by the poor quality of sleep in AD children. Therefore, good quality sleep is important in children with AD. In this study, disturbed sleep quality was found to be more frequent in the AD group, as measured by CSHQ score.
The mean and standard deviation of melatonin levels in the case and control groups were 320.18±49.92 and 383.78±74.53 pg/mL, respectively. The difference in mean melatonin levels among the case and control groups was statistically highly significant (p<0.01). This finding is in accordance with previous studies reporting that serum melatonin levels in AD patients are lower than those in the control group.23
Data on the correlation between melatonin and AD were limited.24 The correlation between them was thought to be related to IFN-ɣ which plays a role in melatonin synthesis.24 Patients with AD tend to have lower IFN-ɣ levels compared to participants without AD due to oxidative stress.24–26 Melatonin is synthesized from tryptophan, which undergoes hydroxylation and decarboxylation into serotonin and is then converted into melatonin,27 thus IFN-ɣ increases the ability of lymphocytes and macrophages to bind tryptophan in the circulation, increasing the melatonin synthesis.27 The low level of IFN-ɣ in AD is thought to cause lower melatonin levels in AD compared to control patients.27
The case group consists of 19 children with moderate AD, with a mean SCORAD index of 31.49. This group had a mean CSHQ score of 47.38. Based on the statistical analysis, there was a significant correlation with a positive direction between SCORAD and CSHQ. This indicates that the higher the SCORAD score, the higher the CSHQ score. An increase in the CSHQ score indicates a disturbance in sleep quality. In other words, the higher the SCORAD score, the more disturbed the sleep quality.
Similar findings have been reported by a 2016 Latin-American study by Pereira et al and a 2016 Korean study by Kong et al who demonstrated a positive correlation between CSHQ and the severity of disease.16,28 An increase in the severity of AD is associated with an increase in itching sensation. As the disease to get worse children with AD tend to scratch their skin more often and as a result their sleep quality is increasingly disturbed.
In addition to AD, sleep disorders are also found in other chronic dermatological diseases such as psoriasis that leads to decreasing quality of life.29 However, Kaaz et al30 on their study found that subjects with AD experienced more problems with insomnia and sleep quality than did those with psoriasis. Establishing recommendations concerning screening for sleep disorders and their predictors should be considered on patients with chronic dermatological diseases.
The case group had an average melatonin value of 320.18 pg/mL with a range of 244.5–455.95 pg/mL. Based on the statistical analysis, no correlation was found between SCORAD and melatonin levels (p>0.05). The correlation between SCORAD and melatonin levels has not been widely studied.8 A Turkish study by Uysal et al in 2016 reported a significant negative correlation between SCORAD in severe AD and melatonin levels, while in mild-moderate cases, a non-significant correlation was found.31 In this study, all participants in the case group had moderate AD, thus data on the correlation between melatonin levels and SCORAD in severe AD were not obtained.
The correlation between melatonin and sleep activity in AD patients has previously been investigated in several studies. However, the results obtained by these studies varied. This is presumably due to variations in sampling methods and assessment tools. Kimata et al in 2007, Chang et al in 2014, and Chang et al in 2016, reported a positive correlation between melatonin levels and sleep quality.6,32,33 In the study by Kimata et al the participants slept in the hospital, samples were taken from saliva at 23:00, 02:00, and 05:00, and sleep quality was assessed using the Subjective Pittsburgh Sleep Quality Index questionnaire.33 Chang et al in 2014 examined urine melatonin levels of pediatric AD patients, which were found to be correlated with sleep quality, as assessed using an actigraph. A subsequent study by the same authors in 2016 investigated the effect of melatonin supplementation in children with AD on sleep quality, as assessed using an actigraph.32
No significant correlation was observed in our study between melatonin levels and CSHQ score (p>0.05). This is presumably due to the absence of severe AD patients, the varied use of electronic devices before bed, the intensity of the light used in the bedroom, and the lack of objective sleep assessment tools due to limited facilities. However, a similar result was reported by Ali et al in 2020, who found no significant improvement in sleep quality based on the Sleep Disturbances Scale for Children questionnaire, between pediatric AD patients who received melatonin supplements and the control group who received placebo.34 Dimitrov et al in 2006 reported that earlier sleep induces Th1-produced cytokine production while sleeping late at night will induce a shift in T-helper differentiation towards Th2. This is thought to indirectly reduce IFN-ɣ levels and will decrease T-helper levels.35 Therefore, it is suspected that the decrease in melatonin levels in AD patients is also indirectly caused by sleep disturbances caused by the severity of the disease. However, studies investigating the correlation between melatonin levels, sleep disturbance, and melatonin prescription in children with AD should be evaluated further.
Limitation
- There were no study participants with mild and severe AD, and hence there was no description of the variations in melatonin and CSHQ levels in AD among children with mild and severe AD.
- The intensity of light in the bedroom and gadget use before bedtime was not comparable among the study participants.
- Our study was limited by a relatively small number of patients.
Conclusion
There is a decrease in sleep quality as indicated by increased CSHQ scores in children with moderate AD. Melatonin levels in children with moderate AD are lower than those in participants without AD. Melatonin urine concentration cannot become a marker/predictor of sleep disorders in moderate AD children.
Consent Statement
The authors certify that they have obtained all appropriate patient consent forms. The patients signed a consent form for the publication of the case details and images.
Acknowledgments
The authors would like to thank the staff of the Department of Dermatology and Venereology, Faculty of Medicine, Universitas Padjadjaran – Dr. Hasan Sadikin General Hospital, Bandung, West Java, Indonesia.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Weidinger S, Novak N. Atopic dermatitis. Lancet. 2016;387(10023):1109–1122. doi:10.1016/S0140-6736(15)00149-X
2. Ständer S. Atopic Dermatitis. N Engl J Med. 2021;384(12):1136–1143. doi:10.1056/NEJMra2023911
3. Simpson EL, Leung DYM, Eichenfield LF, et al. Atopic dermatitis. In: Kang S, Amagai M, Bruckner AL, Enk AH, Margolis DJ, McMichael AJ, editors. Fitzpatrick’s Dermatology in General Medicine.
4. Ardakani AT, Farrehi M, Sharif MR, et al. The effects of melatonin administration on disease severity and sleep quality in children with atopic dermatitis: a randomized, double-blinded, placebo-controlled trial. Pediatr Allergy Immunol. 2019;29(8):834–840. doi:10.1111/pai.12978
5. Vaughn AR, Clark AK, Sivamani RK, Shi VY. Circadian rhythm in atopic dermatitis pathophysiology and implications for chronotherapy. Wiley Pediatr Dermatol. 2017;35:1–6.
6. Chang Y, Chou Y, Lee J, et al. Atopic dermatitis, melatonin, and sleep disturbance. Pediatri. 2014;134(2):297–403.
7. Gheban BA, Rosca IA, Crisan M. The morphological and functional characteristics of the pineal gland. Medi Pharm Rep. 2019;92(3):226.
8. Jaworek AK, Szepietowski JC, Hałubiec P, Wojas-Pelc A, Jaworek J. Melatonin as an antioxidant and immunomodulator in atopic dermatitis–a new look on an old story–A Review. Antioxidants. 2021;1179(10):1–16.
9. Reuveni H, Chapnick G, Tal A, Tarasiuk A. Sleep fragmentation in children with atopic dermatitis. Arch Pediatr Adolesc Med. 1999;153(3):249–253. doi:10.1001/archpedi.153.3.249
10. Mehling A, Fluhr JW. Chronobiology: biological clocks and rhythms of the Skin. Skin Pharmacol Physiol. 2006;19(4):182–189. doi:10.1159/000093113
11. Brzezinski A, Epstein FH. Melatonin in humans. N Engl J Med. 1997;336(3):186–195. doi:10.1056/NEJM199701163360306
12. Rzepka-Migut B, Paprocka J. Melatonin-Measurement methods and the factors modifying the results. A systematic review of the literature. Int J Environ Res Public Health. 2020;17(6):1916. doi:10.3390/ijerph17061916
13. Oranje AP, Glazenburg EJ, Wolkerstorfer A. Practical issues on interpretation of scoring atopic dermatitis: the SCORAD index, objective SCORAD and the three‐item severity score. Br J Dermatol. 2007;157(4):645–648. doi:10.1111/j.1365-2133.2007.08112.x
14. Hartini S, Sunartini S, Herini ES, Takada S. Item analysis and internal consistency of children’s sleep habit questionnaire (CSHQ) in Indonesian version. Belitung Nurs J. 2017;3(6):645–655. doi:10.33546/bnj.184
15. Li JC, Fishbein A, Singam V, et al. Sleep disturbance and sleep-related impairment in adults with atopic dermatitis: a cross-sectional survey-based study. Dermatitis. 2018;29(5):270. doi:10.1097/DER.0000000000000401
16. Urrutia-Pereira M, Solé D, Rosario NA, et al. Sleep-related disorders in Latin-American children with atopic dermatitis: a case-control study. Allergol Immunopathol. 2017;45(3):276–282. doi:10.1016/j.aller.2016.08.014
17. Chang YS, Chiang BL. Sleep disorders and atopic dermatitis: a 2-way street? J Allergy Clin Immunol. 2018;142(4):1033–1040. doi:10.1016/j.jaci.2018.08.005
18. Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23(8):1043–1052.
19. Silverberg JI, Garg NK, Paller AS, Fishbein AB, Zee PC. Sleep disturbances in adults with eczema are associated with impaired overall health: a US population-based study. J Invest Dermatol. 2015;135(1):56–66. doi:10.1038/jid.2014.325
20. Dogan DG, Canaloglu SK, Kivilcim M, Kum YE, Topal E, Catal F. Sleep patterns of young children with newly diagnosed atopic dermatitis. Postepy Dermatol Alergol. 2011;34(2):143.
21. Weidinger S, Illig T, Baurecht H, Irvine AD, Rodriguez E, Diaz-Lacava A. Loss-of-function variations within the filaggrin gene predispose for atopic dermatitis with allergic sensitizations. J Allergy Clin Immunol. 2006;118(1):214–219. doi:10.1016/j.jaci.2006.05.004
22. Abuabara K. Atopic dermatitis and academic achievement–more to learn. JAMA dermatol. 2021;157:637. doi:10.1001/jamadermatol.2021.0007
23. Muñoz‐Hoyos A, Espín‐Quirantes C, Molina‐Carballo A, et al. Neuroendocrine and circadian aspects (melatonin and β‐endorphin) of atopic dermatitis in the child. Pediatr Allergy Immunol. 2007;18(8):679–686. doi:10.1111/j.1399-3038.2007.00574.x
24. Marseglia L, D’Angelo G, Manti S, Salpietro C, Arrigo T, Barberi I. Melatonin and atopy: role in atopic dermatitis and asthma. Int J Mol Sci. 2014;15(8):13482–13493. doi:10.3390/ijms150813482
25. Chung F. Anti-inflammatory cytokines in asthma and allergy: interleukin-10, interleukin-12, interferon-γ. Mediators Inflamm. 2001;10(2):51–59. doi:10.1080/09629350120054518
26. Wardhana M, Suryawati S, Rusyati,LM. Role of psychological stress on Interferon-Gamma (IFN-γ) in atopic dermatitis. Biomed Pharm J. 2018;11(2):889–895. doi:10.13005/bpj/1445
27. Zhao D, Yu Y, Shen Y, et al. Melatonin synthesis and function: evolutionary history in animals and plants. Front Endocrin. 2019;10:249. doi:10.3389/fendo.2019.00249
28. Kong HH, Oh J, Deming C, et al. Temporal shifts in the skin microbiome associated with disease flares and treatment in children with atopic dermatitis. Genome Res. 2012;22(5):850–859. doi:10.1101/gr.131029.111
29. Nowowiejska J, Baran A, Lewoc M, Grabowska P, Kaminski TW, Flisiak I. The assessment of risk and predictors of sleep disorders in patients with psoriasis—a questionnaire-based cross-sectional analysis. J Clin Med. 2021;10(4):664. doi:10.3390/jcm10040664
30. Kaaz K, Szepietowski JC, Matusiak Ł. Influence of itch and pain on sleep quality in atopic dermatitis and psoriasis. Acta Derm Venereol. 2019;99(2):175–180. doi:10.2340/00015555-3065
31. Uysal P, Avcil S, Abas Bİ, Yenisey Ç. Evaluation of oxidant-antioxidant balance in children with atopic dermatitis: a casecontrol study. Am J Clin Dermatol. 2016;17(5):527–537. doi:10.1007/s40257-016-0210-8
32. Chang YS, Lin MH, Lee JH, et al. Melatonin supplementation for children with atopic dermatitis and sleep disturbance: a randomized clinical trial. JAMA pediatr. 2016;170(1):35–42. doi:10.1001/jamapediatrics.2015.3092
33. Kimata H. Elevation of salivary melatonin levels by viewing a humorous film in patients with atopic eczema. Horm Metab Res. 2007;39(4):310–311. doi:10.1055/s-2007-973815
34. Ali DM, Saeed MM, Ibrahim W, Elsayed AS. Evaluation of melatonin supplementation in children with atopic dermatitis at Aboreesh Hospital, Egypt. J Env Treatment Tech. 2020;8(3):1084–1088.
35. Dimitrov S, Lange T, Tieken S, Fehm HL, Born J. Sleep associated regulation of T helper 1/T helper 2 cytokine balance in humans. Brain Behav Immun. 2004;18(4):341–348.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
