Back to Journals » Patient Preference and Adherence » Volume 10
Medication adherence in patients in treatment for rheumatoid arthritis and systemic lupus erythematosus in a university hospital in Brazil
Authors Prudente L, Diniz J, Ferreira T, Lima D, Silva N, Saraiva G, Silveira, Dewulf N, Amaral R
Received 17 December 2014
Accepted for publication 17 February 2015
Published 19 May 2016 Volume 2016:10 Pages 863—870
DOI https://doi.org/10.2147/PPA.S79451
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Luciana Resende Prudente,1 Juliana de Souza Diniz,2 Tatyana Xavier Almeida Matteucci Ferreira,3 Dione Marçal Lima,2 Nílzio Antônio Silva,4 Guylherme Saraiva,4 Erika Aparecida Silveira,4 Nathalie de Lourdes Souza Dewulf,2 Rita Goreti Amaral2
1University Pharmacy, Faculty of Pharmacy, 2Faculty of Pharmacy, 3Clinical Hospital, 4Faculty of Medicine, Federal University of Goiás, Goiânia, Brazil
Abstract: Medication adherence is essential for the control of symptoms and progression of rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE). The aim of the study was to investigate medication adherence in outpatients in treatment for RA and SLE in a university hospital in Brazil. This was a quantitative, cross-sectional analytical study. A total of 92 patients (55 RA patients and 37 SLE patients) were included in the study. A structured questionnaire for patients’ interview and a form for collecting data from medical records were used for data collection. Adherence to drug treatment was assessed by the Morisky scale questionnaire. Data storage and analysis were performed using Epi Info 3.5.4 and statistical analysis by Stata/SE 12.0. The Pearson’s chi-squared test and Fisher’s exact test were applied for statistical and bivariate analyses. For multivariate data analysis the Poisson regression and the Wald test were used. The prevalence of adherence to drug treatment was 16.4% in RA patients and 45.9% in SLE patients. The final model of the multivariate analysis demonstrated associations between medication adherence and the following covariates for both RA and SLE groups: duration of therapy for rheumatic disease at the institution greater than 15 years and presence of more than six chronic comorbidities. The parameter “acquisition of medication at the high-cost pharmacy” was differently associated with medication adherence by group, and for the SLE group, living outside the city of Goiânia was a protective factor associated with adherence. This study demonstrated a low prevalence of medication adherence in patients in treatment for RA and SLE treated at this institution. These findings will serve as a base for future studies to elucidate what factors may positively or negatively affect medication adherence in this population. In addition, multidisciplinary approaches are needed to enhance adherence to drug treatment in patients in treatment for rheumatic disease.
Keywords: compliance, phamacotherapy, rheumatic diseases
Introduction
Rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) are systemic autoimmune rheumatic diseases, with unknown cause. Both RA and SLE may affect individuals in different grades of severity. In all, 50% of individuals suffering from RA will have their work capacity reduced within 10 years of disease onset and 23% with SLE will stop working in the first 5 years of diagnosis.1,2 These rheumatic diseases may represent direct costs related to outpatient and hospital therapies, estimated at €4.737–€15.637 per patient per year for RA3 and US$3,735–US$14,410 for SLE.4 The costs of RA and SLE treatments are comparable with other chronic conditions, including diabetes and cardiovascular diseases. For example, a study conducted in three European countries in 2008 estimated that the annual cost in patients with hypertension was €5,341, €2,682, and €5,957 in Germany, Spain, and Italy, respectively.5 Indirect costs of illnesses comprise reduction in productivity related to non-paid and paid activities, and are estimated at €34,9153 for RA patients and €1,093–€14,614 for SLE patients.4
The treatment of SLE and RA is aimed at improving symptoms, slowing the progression of the disease, and inducing clinical remission. The standard medication includes glucocorticosteroids, which is generally affordable as compared to other drugs used in the control of rheumatic disease and is effective in controlling pain and inflammation, even with their adverse effects, especially when used in long-term therapies.6 In addition, nonsteroidal anti-inflammatory drugs, other analgesics, and disease-modifying antirheumatic drugs (DMARDs) are widely used in RA. DMARDs are slow-acting drugs, used to slow down the progression of the disease.7
In Brazil, the list of drugs approved by the Ministry of Health for the treatment of RA includes analgesics (dipyrone and paracetamol), glucocorticoids (prednisone, prednisolone, and methylprednisolone), nonsteroidal anti-inflammatory drugs (naproxen and ibuprofen), synthetic DMARDs (chloroquine, hydroxychloroquine, methotrexate, leflunomide, azathioprine, and sulfasalazine), and biological DMARDs (adalimumab, certolizumab pegol, etanercept, infliximab, golimumab, abatacept, rituximab, and tocilizumab). With regard to the treatment of SLE, in addition to the glucocorticoids and synthetic DMARDs used for the management of RA, the Brazilian guidelines for the management of SLE recommend the use of immunomodulatory drugs (thalidomide, cyclophosphamide, cyclosporine, and mycophenolate mofetil).8 Although a wide range of alternatives of medications are available for RA and SLE treatments, the access and adherence to the drug therapy by the patients are crucial for the success of the therapy and improvement of patients’ quality of life. Several studies have demonstrated that patient non-compliance to drug therapy may be attributed to a number of causes, including factors related to patient, disease, therapeutics, health care service, and communication between physicians and patients, depending on different diseases and study population.9 Adherent patients are three times more likely to achieve desired outcomes, eg, better quality of life and greater functional capacity as compared to non-adherent patients.10 Non-adherence is considered by the World Health Organization (WHO) as a paramount public health problem.11 Nearly 50% of individuals with chronic disease who need long-term therapies are actually adherents to the drug therapy in developed countries. In developing countries, on the other hand, such prevalence is estimated to be lower due to less access to medication and health services.11 Studies and researches on medication adherence are as important as the development of new therapeutic advances. Also, multidisciplinary approaches, including the physician–pharmacist interactions, may lead to relevant discussions and promising actions.12
Few studies have been conducted on adherence in rheumatologic disorders as compared to other diseases such as hypertension, diabetes, and asthma.13 Considering that rheumatologic diseases consist of a public health problem affecting a nationwide social insurance system, studies aimed at investigating medication adherence and developing strategies to promote adherence among these patients are needed. In light of this, this study aimed at investigating drug therapy adhesion in outpatients with RA and SLE treated in a university hospital in Brazil.
Materials and methods
This was a quantitative, cross-sectional, analytical study, conducted at the Clinical Hospital of the Federal University of Goiás (CH-FUG) in Brazil, between June 2013 and February 2014. The study was approved by the ethics committee of the Federal University of Goiás, and written informed consent was obtained from all participants.
Sample size was calculated on the basis of the number of patients registered at the CH-FUG (n=516), 80% power at the 0.05 level of significance, and a 5% margin of error with 99.9% confidence interval (CI). Based on this assumption, we estimated that a sample size of 116 patients would be needed. A total of 206 patients attending the outpatient clinic for rheumatologic disease were invited to participate in the study, and only 101 agreed to participate. Nine patients were excluded because of lack of information on medical records and/or non-response or non-completion of questionnaires. A total of 92 patients completed the study.
Patients’ information regarding their socioeconomic and demographic characteristics, satisfaction with health care services, and knowledge about medication were collected by using a structured questionnaire. Patients’ clinical profile was obtained from medical records by using a standardized form. These instruments were developed and used by our group in previous studies on medication adherence in other conditions.14 The interviews were performed at the waiting room of the clinic. Adherence behavior was assessed by the Morisky scale questionnaire.15 When patients aged less than 18 years, the instruments were applied to their parents or caregivers. Severity of disease was classified according to patients’ reports. To assess the complexity of pharmacotherapy, a modified, validated version of the pharmacotherapy complexity index was used.16 Complexity of pharmacotherapy was dichotomized into low (<14) and high (>14) complexities, and the drugs considered for assessment were those documented in the medical records.
Inclusion criteria were a probable or confirmed diagnosis of RA and SLE and continuous use of medication for rheumatic disease treatment. Exclusion criteria included lack of clinical and/or cognitive conditions for completion of the interview process or questionnaires, and/or incomplete collection of medical records data.
Data storage and analysis were performed using Epi Info 3.5.4 and statistical analysis by Stata/SE 12.0 (StataCorp LP, College Station, TX, USA). Prevalence of adherence and adherence behavior among patients were calculated separately by group (RA or SLE) and as a whole (ie, RA + SLE patients). The Pearson’s chi-squared test and Fisher’s exact test were used for bivariate analysis to investigate the association between adherence and the other covariates. In the Poisson regression, all covariates with a P-value <0.20 were included for multivariate data analyses, and only the covariates with a P-value <0.05 were included in the final model. The prevalence ratio (PR) and the 95% CI for these covariates were also calculated. The Wald test was used to test the significance of each parameter.
Results
Most of patients were female, 85 (92.39%), and aged between 41 years and 59 years, 67 (73.12%).
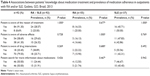
The prevalence of medication adherence was 16.4% in RA patients and 45.9% in SLE patients. Patients’ socioeconomic and demographic data as well as the bivariate analyses between these variables and adherence are shown in Table 1. Adherence to drug treatment was significantly associated (P=0.032) with the education level in the RA group and with acquisition of medications at the high-cost pharmacy in the SLE group (P=0.014) (Table 1).
No association between medication adherence and patients’ perception of health care service was observed in the groups (Table 2). Adherence was significantly associated (P=0.012) with the number of chronic comorbidities in the RA group and was nearly significant in the RA + SLE group (P=0.005). No associations between time of diagnosis, duration of treatment, and severity and complexity of the disease were observed in the RA group or in the RA + SLE group (Table 3). Adherence to medication was not associated with patients’ perception or knowledge about the drug therapy in the three groups (Table 4). The variables included in the multivariate analysis model for the RA + SLE group were trust in the staff, duration of therapy for rheumatic disease at the institution, and number of chronic comorbidities. For the SLE group, the covariates included were high-cost pharmacy, duration of therapy for rheumatic disease at the institution, and number of outpatient appointments and for the RA group, education level, occupation, city of origin, high-cost pharmacy, duration of therapy for rheumatic disease at the institution, and number of chronic comorbidities. Results of the multivariate analysis showed that duration of therapy for rheumatic disease at the institution greater than 15 years (PR =2.23; 95% CI 1.03–4.81) and having more than six chronic comorbidities (PR =3.33; 95% CI 1.51–7.37) remained associated in the final model for the RA + SLE group, high-cost pharmacy (PR =5.95; 95% CI 1.02–34.69) remained associated in the final model for the SLE group, and living outside the city of Goiânia remained associated as a protective factor (PR =8.43; 95% CI 1.03–4.81).
Acquisition of medication at the high-cost pharmacy was associated with adherence in both RA and SLE groups, however by an inverse influence (Table 5).
Discussion
In this study, we identified a low prevalence of medication adherence in patients with RA in contrast to previous studies. Adherence to drug treatment in the SLE group, on the other hand, was similarly prevalent (46%) to those found by other authors, although it still falls short of desirable levels.
Factors related to adherence, including how long the patient has been under treatment at the CH-FUG, where the patient obtains his/her medication, number of comorbidities, and city of origin were similar to those reported in the literature. So far, there is no gold standard method to measure medication adherence and to establish its associated factors. Although it has been considered a very strict method, and limited in psychometric properties,17 the original Morisky scale has been implemented in a large number of study as an indirect method to perform a primary identification of medication adherence in several populations.14,18,19 Few studies have evaluated medication adherence in RA and SLE by using the Morisky scale. One previous investigation, also performed in Brazil, found a prevalence of 32% of adhesion in SLE patients.14 Systematic reviews using different medication adherence scales reported a prevalence of adhesion varying from 18% to 99% in RA and SLE patients,20 from 30% to 92% in RA patients, and from 49% to 93% in SLE patients.21 The methods utilized in these studies defined adherence in different ways and considered adherence as the fulfillment of at least 80% of medical prescriptions or recommendations. The Morisky scale is comparatively stricter in defining adherence, and such differing measures of adherence may explain the differences in the results. This discrepancy between different methods to measure adherence is also observed in studies on different diseases. Prevalence of adhesion in patients with hypertension, for example, was 13%22 as measured by the Morisky scale and varied from 51% to 84% in other studies using other methods.23,24 This study demonstrated, by bivariate analysis, that education level was associated with medication adherence. This is in accordance with previous findings reporting that individuals with higher educational level have greater concern about health issues and cooperation with their treatment plan.14,25 However, the multivariate analysis did not corroborate this finding in our study.
A significant association was found between medication adherence and concomitant occurrence of duration of treatment at the institution greater than 15 years and more than six chronic diseases. Patients with severe clinical conditions tend to be more receptive to the treatment and positively contribute to medication adherence.26 The number of chronic comorbidities may not be a determining factor but rather an indicator of the severity of health conditions.
Acquisition of medication at the high-cost pharmacy was associated with adherence in the SLE group, when adjusted by number of appointments during the previous year and duration of treatment. This result may be explained by the fact that SLE patients refractory to first choice, more accessible therapies or patients with more severe forms of the disease generally suffer from a variety of symptoms and are more likely to be adherent to their therapies in an attempt to control these symptoms.10 In the RA group, medication adherence was associated with patients’ place of origin, number of chronic disease, and place of acquisition of medication. Patients living in other cities than Goiânia tend to have fewer conditions to attend the CH-FUG, due to transport difficulties. This observation is in accordance with a previous study demonstrating lower adherence among patients who lived further from the reference hospital14 and with data from the literature as well.11
In addition, the number of chronic diseases remained associated with adherence in the RA group, suggesting a worsening in their health condition. However, differently from the SLE group, non-acquisition of medication at the high-cost pharmacy was associated with greater adherence. Such contrast may be related to different stages of the course of the disease or of the therapy these patients have been experiencing. Both SLE and RA are rheumatologic diseases with their specificities. The main clinical manifestations of SLE are cardiovascular diseases, lupus pneumonitis, autoimmune hemolytic anemia, chronic arthritis, and neuropsychiatric disorders,14 which cause acute or resistant symptomatology that demands continuous attention. In RA, treating joint manifestations of the disease is the primary concern expressed by the patient, more importantly than comorbidities, diabetes, systemic arterial hypertension, dyslipidemia, and osteoporosis. In light of this, the clinical course of such diseases should be carefully considered in order to evaluate all factors related to medication adherence. In the SLE treatment, disease-modifying drugs and biological agents exert an important role in case of resistant patients to first-line therapy. However, in the treatment of severe symptomatology and comorbidities, other specific therapies are still needed. Therefore, for SLE patients, one may infer that perceived symptoms lead to greater concern about treatment and greater adherence to the therapy.
For RA patients, biological agents are immunosuppressive drugs that reduce inflammation and joint damage and are used in the treatment of moderate-to-severe active disease, in case of severe affection of functional capacity.7 The relief of these symptoms by biological drugs may, however, negatively influence adherence to drug therapy of other comorbidities by RA patients. Disappearance of symptoms and occurrence of silent disease are commonly associated with non-adherence.11,27
Although some of our results did not achieve statistical significance, it is of note that SLE patients had greater satisfaction with the health care service and drug therapy as well as greater knowledge about the medication used for SLE treatment as compared with RA patients, as demonstrated by the bivariate analysis. Satisfaction with the health care service and team and knowledge about the medications may positively influence adherence to the prescribed therapy.11 This is corroborated by our results, demonstrating that 46% of SLE patients and 16% of RA patients were considered as adherent.
Finally, a number of limitations need to be considered. First, data collection was partially hampered by features of the place where it was performed, including small spatial dimensions, inadequate ventilation, excessive noise, and lack of privacy for the interviews. Second, reasons for non-participation in the study reported by eligible patients included a feeling of frustration for having participated in previous studies and not receiving a feedback from the investigators, and concern about sharing personal data with the investigators. Also, some patients were not willing to answer the questionnaire due to physical and mental tiredness, which was either reported by the patients or noticed by the investigators. Besides, it is worth mentioning that mental distress and psychological disorders such as depression have been reported in 13%–47% of RA and 45.2% of SLE patients.28
Interventional studies aiming at enhancing adherence to medication treatment have demonstrated that these actions need to be based on multidisciplinary approaches, since adherence is a health care team’s responsibility and is not only dependent on patients’ decision. In addition, government support for research and implementation of strategies for improving adherence is needed, in order to assure not only access to medications but also their rational use by patients, and hence efficient use of public investments.
Conclusion
In this study, we identified a low prevalence of medication adherence in patients with RA and SLE. These findings highlight the need for future studies to understand the mechanisms underlying adherence to drug treatment for rheumatologic disease. Also, this study may serve as a base for future investigations on alternative methods to measure adherence and new interventions to enhance medication adherence in RA and SLE.
Acknowledgments
This study is supported by Foundation of Support Research of State Goiás and Clinical Hospital of the Federal University of Goiás, Brazil.
Disclosure
The authors declare that there are no conflicts of interest.
References
Goeldner I, Skare TL, Reason ITM, Utiyama RR. Rheumatoid arthritis: a current view. J Bras Patol Med Lab. 2011;47(5):495–503. | ||
Al Dhanhani AM, Gignac MAM, Jiandong S, Fortin PR. Work disability in systemic lupus erythematosus. Arthritis Rheum. 2009;61(3):378–385. | ||
Huscher D, Merkesdal S, Thiele K, et al; German Collaborative Arthritis Centres. Cost of illness in rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis and systemic lupus erythematosus in Germany. Ann Rheum Dis. 2006;65(9):1175–1183. | ||
Zhu TY, Tam LS, Li EK. Cost-of-illness studies in systemic lupus erythematosus: a systematic review. Arthritis Care Res (Hoboken). 2011;63(5):751–760. | ||
Wille E, Scholze J, Alegria E, et al. Uhl-Hochgraeber modelling the costs of care of hypertension in patients with metabolic syndrome and its consequences, in Germany, Spain and Italy. Eur J Health Econ. 2011;12:205–218. | ||
Spies CM, Bijlsma JWJ, Buttgereit F. Pharmacology of glucocorticoids in rheumatoid arthritis. Curr Opin Pharmacol. 2010;10(3):302–307. | ||
Wolowacz SE, Samuel M, Brennan VK, Jasso-Mosqueda JG, Van Gelder IC. The cost of illness of atrial fibrillation: a systematic review of the recent literature. Europace. 2011;13(10):1375–1385. | ||
Malottki K, Barton P, Tsourapas A, et al. Adalimumab, etanercept, infliximab, rituximab and abatacept for the treatment of rheumatoid arthritis after the failure of a tumour necrosis factor inhibitor: a systematic review and economic evaluation. Health Technol Assess. 2011;15(14):1–278. | ||
Singh JA, Furst DE, Bharat A, et al. 2012 update of the 2008 American college of rheumatology recommendations for the use of disease-modifying antirheumatic drugs and biologic agents in the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken). 2012;64(5):625–632. | ||
DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: a meta-analyses. Med Care. 2002;40(9):794–811. | ||
World Health Organization (WHO). Adherence to Long-Term Therapies: Evidence for Action. 2003. Available from: whqlibdoc.who.int/publications/2003/9241545992.pdf | ||
Laufs U, Rettig-Ewen V, Böhm M. Strategies to improve medication adherence. Eur Heart J. 2011;32(3):264–268. | ||
Elliott RA. Poor adherence to medication in adults with rheumatoid arthritis. Dis Manag Health Outcomes. 2008;16(1):13–29. | ||
Oliveira-Santos M, Verani J, Klumb E, Albuquerque E. Evaluation of adherence to drug treatment in patients with systemic lupus erythematosus in Brazil. Lupus. 2011;20(3):320–329. | ||
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. | ||
Melchiors AC, Correr CJ, Fernández-Llimos F. Translation and validation into Portuguese language of the medication regimen complexity index. Arq Bras Cardiol. 2007;89(4):210–218. | ||
Tan X, Patel I, Chang J. Review of the four item Morisky medication adherence scale (MMAS-4) and eight item Morisky medication adherence scale (MMAS-8). Inov Pharm. 2014;5(3):8. [article 165]. | ||
Trauthman SC, Biudes MF, Mello AF, Rosa FS, Peters CA, Galato D. Methods for evaluation of therapeutic medication adherence adopted in Brazil. Infarma Cienc Farm. 2014;26(1):11–26. | ||
Dewulf NLS, Monteiro RA, Passos ADC, Vieira EM, Troncon LEA. Compliance to drug therapy in inflammatory bowel diseases outpatients from an university hospital. Arq Gastroenterol. 2007;44(3):289–296. | ||
Harrold LR, Andrade SE. Medication adherence of patient with selected rheumatic conditions: a systematic review of the literature. Semin Arthritis Rheum. 2009;38(5):396–402. | ||
de Achaval S, Suarez-Almazor ME. Treatment adherence to disease-modifying antirheumatic drugs in patients with rheumatoid arthritis and systemic lupus erythematosus. Int J Clin Rheumtol. 2010;5(3):313–326. | ||
Dosse C, Cesarino CB, Martin JFV, Castedo MCA. Factors associated with patients’ noncompliance with hypertension treatment. Rev Lat Am Enfermagem. 2009;17(2):201–206. | ||
Bloch KV, Melo NA, Nogueira AR. Prevalence of anti-hypertensive treatment adherence in patients with resistant hypertension and validation of three indirect methods for assessing treatment adherence. Cad Saude Publica. 2008;24(12):2979–2984. | ||
Sokol MC, Mcguigan KA, Verbrugge RR, Epstein RS. Impact of medication on adherence on hospitalization risk and healthcare cost. Med Care. 2005;43(6):521–530. | ||
Garcia-Gonzalez A, Richardson M, Garcia Popa-Lisseanu M, et al. Treatment adherence in patients with rheumatoid arthritis and systemic lupus erythematosus. Clin Rheumatol. 2008;27(7):883–889. | ||
Goldring AB, Taylor SE, Kemeny ME, Anton PA. Impact of health beliefs, quality of life and the physician-patient relationship on the treatment intentions of inflammatory bowel disease patients. Health Psychol. 2002;21(3):219–238. | ||
Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patients adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26(5):331–342. | ||
Maneeton B, Maneeton N, Louthrenoo W. Prevalence and predictors of depression in patients with systemic lúpus erythematosus: a cross-sectional study. Neuropsychiatr Dis Treat. 2013;9:799–804. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.