Back to Journals » Patient Preference and Adherence » Volume 16
Medication Adherence Among Geriatric Patients with Chronic Diseases in Riyadh, Saudi Arabia
Authors Alhabib MY, Alhazmi TS, Alsaad SM , AlQahtani AS, Alnafisah AA
Received 8 April 2022
Accepted for publication 2 August 2022
Published 8 August 2022 Volume 2022:16 Pages 2021—2030
DOI https://doi.org/10.2147/PPA.S363082
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Johnny Chen
Mohammed Y Alhabib,1,* Taha S Alhazmi,1 Saad M Alsaad,1,* Alhanouf S AlQahtani,2 Aisha A Alnafisah3
1Department of Family and Community Medicine, College of Medicine, King Saud University, Riyadh, Saudi Aribia; 2General Administration of Pharmaceutical Care, Ministry of Health, Riyadh, Saudi Aribia; 3Department of Clinical Pharmacy, College of Pharmacy, Riyadh, King Saud University, Riyadh, Saudi Aribia
*These authors contributed equally to this work
Correspondence: Saad M Alsaad, Department of Family and Community Medicine, College of Medicine, King Saud University, Riyadh, Saudi Aribia, Tel +966505493944, Email [email protected]
Background: Medication non-adherence is a common and significant public health problem, especially among the geriatric population. This study’s objective was to measure medication adherence and associated factors among geriatric patients with chronic diseases.
Methods: A cross-sectional study targeted outpatient geriatrics who suffer from chronic diseases at King Saud University Medical City (KSUMC), Riyadh, Saudi Arabia. Telephone interviews were utilized to collect data from participants using a structured questionnaire and the GMAS validated instrument scale (General Medication Adherence Scale) intended to measure important determinants impacting adherence: patient behaviour, cost, comorbidity, and pill burden.
Results: A total of 422 patients were assessed for medication adherence. The Mean overall score for GMAS was 29.9± 3.1 out of 33. (64.9%) of the patients had a high level of medication adherence. The patients had a high adherence on the domain of patient behavior related non-adherence (PBNA) (13.5± 1.9) out of 15, a high adherence on the domain of additional disease and pill burden (ADPB) (11.2± 1.4) out of 12, and good to high adherence on the cost-related non-adherence (CRNA) (5.25± 1.1) out of 6.
Conclusion: The geriatric population with chronic diseases in our study had a good level of adherence to medication if compared with other international figures. To promote better medication adherence, patients must have a good understanding of their disease and strong beliefs about the medications prescribed.
Keywords: frailty, older patients, hospitalized, prevalence, Saudi Arabia
A Letter to the Editor has been published for this article.
Introduction
Worldwide, the geriatric population aged more than 60 years tends to be increasing significantly. The number will be expanding from 1 billion in 2019 to 21 billion by 2050.1
In Saudi Arabia, the most recent elderly survey by General Authority for Statistics revealed that the elderly represents 4.19% of the total Saudi population,2 and are estimated to reach 18.4% by 2050.3
Population ageing has its consequences, including health-related issues such as multimorbidity of chronic diseases. Most common preventable chronic diseases in Saudi Arabia related to lifestyle and strongly correlated with ageing are hypertension, diabetes type 2, dyslipidemia and obesity.1 Multimorbidity of chronic diseases refers to the coexistence of two or more chronic conditions present for more than one year.4 Chronic conditions in the elderly have been paralleled with increasing healthcare costs and utilization,5 polypharmacy, and medication non-adherence.6
Medication non-adherence is a common and significant public health issue. A previous study has shown that up to 50% of patients with chronic diseases do not take their medication as prescribed.7 This suboptimal adherence can worsen medical conditions, reduce the quality of life, and increase mortality and morbidity.8 In older patients, the magnitude of the problem is even greater. It is estimated that around 10% of geriatrics hospitalizations are due to medication non-adherence,9 and the rate of non‐adherence in older adults as high as 75%.10 The World Health Organization (WHO) has identified multifactorial determinants that influence adherence, categorizing them into five dimensions: patient-related factors, socioeconomic factors, therapy-related factors, condition-related factors, health care team, and system-related factors.8 Further studies show that the most influencing barriers found between the elderly were beliefs about treatment necessity, regimens complexity, and concerns regarding potential side effects.10
Assessment of the patients’ compliance with the treatment regimen is crucial. However, there is no standard method for assessing medication adherence. Self-reported medication adherence questionnaires are one of the acceptable tools.11 In Saudi Arabia, Morisky’s Medication Adherence Scale (MMAS) and General Medication Adherence Scale (GMAS) are common validated instruments used for assessing medication adherence.12 GMAS is considered more sensitive, specific, and accurate than MMAS.13
Despite the magnitude of non-adherence in geriatrics, the problem is yet overlooked, and to the extent of our knowledge, no previous study has surveyed the adherence among elderly patients in Saudi Arabia. Therefore, this study aims to measure medication adherence level among geriatric population with chronic diseases and to assess the associated factors among this group in Saudi Arabia.
Materials and Methods
Design and Setting
A cross-sectional study targeted outpatient geriatric population who suffered from chronic disease and visited the clinics at King Saud University Medical City (KSUMC), Riyadh, Saudi Arabia.
Sample Size and Study Population
The sample size was calculated, assuming 50% prevalence, 95% confidence interval (CI), and 5% margin of error. Based on this, 422 patients were required for the study. A random sampling technique was utilized to select study participants from a list of elderly patients following up in the outpatient clinics at KSUMC. Patients were recruited according to the following criteria: aged 60 years and above, having one or more of the following diseases (Diabetes: Haemoglobin A1c above 6.5%; Hypertension: blood pressure readings above 140/90; Dyslipidaemia: use of any statin for dyslipidemia and obesity: BMI above 24.9 kg/m2) for more than one year, having visited a clinic at least twice, taking at least one medication for chronic disease, and able to communicate in Arabic. The following exclusion criteria were used to reject interviewees: the patient who has diseases that may affect their ability to answer the study questionnaire—including cognitive impairment, dementia, psychiatric disorders, hearing or vision loss, severe comorbidity, palliative care for any malignancy—and bedridden patients on nasogastric or percutaneous endoscopic gastrostomy feeding or refuse to participate.
All patients provided written informed consent, and the study was conducted in accordance with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Ethical approval was obtained from the Institutional Review Board (IRB) at KSUMC, reference (No. 20/0529/IRB). The data collection sheet was strictly observed to ensure participants’ confidentiality throughout the study using the anonymous unique serial number for each subject. Furthermore, the analysis was encrypted and carried out anonymously.
Instrument
The GMAS is a novel, self-reporting adherence instrument recently translated and validated in Saudi patients with chronic diseases. This scale intended to measure three important determinants impacting adherence: patient behaviour, cost, comorbidity, and pill burden.14 It consists of 11 questions, each containing four possible options. The total score ranges from −0-33, a higher score indicating a high adherence level. The final score is stratified into five groups; high (30–33), good (27–29), partial (17–26), low (11–16), and poor (≤10). Prior to conducting this study, permission to use the tool was obtained.14
Data Collection
All participants provided a written informed consent after their clinic visits and if he/she agreed to participate in the research then a telephone interviews were utilized to collect data from participants because of COVID-19 precaution measures. The purposes of the study were explained to participants. Those who agreed to participate were asked to complete the questionnaire. The questionnaire was divided into three sections. Participants’ demographic characteristics were covered in section one, while patient’ health status variables, including Body Mass Index (BMI), blood pressure (BP), haemoglobin A1c, and complete lipid panel, were covered in section two, which was calculated using electronic medical records. Results assessed medication adherence as the outcome variable using GMAS. The interviews were facilitated by three research team members and lasted approximately 10–15 minutes.
Statistical Analysis
The study used the Statistical Package of Social Sciences (SPSS) (v. 26.0 IBM Corp.) to process the data gathered in this study. The normal distribution of the data was ensured before using the parametric tests. The Kolmogorov Smirnov test revealed a K-S value of (0.498) and The Shapiro–Wilk test revealed a significance value of 0.168. Therefore, parametric tests were used to analyze the data gathered in this study. Descriptive statistics were used to analyze the participants’ socio-demographic and clinical characteristics. Moreover, descriptive statistics (Means and standard deviations) were used to determine the medication adherence score on the GMAS scale used in this study. In additional Simple linear regression analysis was used to determine the predictors of medication adherence among the enrolled patients. Moreover, Independent samples t-test and ANOVA test were used to identify any significant statistical differences in medication adherence based on the patients’ socio-demographic or clinical characteristics.
Results
Participants’ Characteristics
Total of 422 patients participated in this study. Table 1 shows the sociodemographic characteristics of the study participants. The mean age was 69.7±6.8 years. Most of the patients were females (56.2%), married (77.3%), living with their families (95.3%), in the Riyadh area (88.9%), and had obtained school education (33.6%). The majority of the patients were retired (93.1%) and had a monthly income (<SAR 5000) (35.1%). In addition, it was found that about 95.3% (n=402) of the study participants were living with their families, whereas 4.7% (n=20) were living alone.
 |
Table 1 Participants’ Sociodemographic Characteristics. (N= 422) |
Table 2 showed the clinical characteristics of the participants. The average number of patients with chronic diseases in this study was (4.3±1.6). %). Dyslipidemia was the highest chronic condition because we considered dyslipidemia in any patient on statin. Hypertension (HTN) was the second most common chronic disease reported in the study sample (83%), followed by diabetes mellitus (DM) (81.8%) Also, the average number of medications taken by the patients was (6.8±3.0), and the daily frequency was (2.7±0.95). Most of the patients were taking their medications by themselves (88.4%) (Table 2).
 |
Table 2 Participants’ Clinical Characteristics |
Medication Adherence Among the Study Participants
The results in (Figure 1) represent the medication adherence level, most of the patients in this study had high adherence levels (64.9%), while 21.3% had good adherence. Some patients (13.3%) were partially adherent, and a few 0.5% had a low level of adherence, and (Table 3) shows the level of medication adherence according to GMAS constructs.
 |
Table 3 GMAS Constructs Scores |
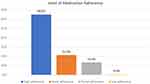 |
Figure 1 Level of medication adherence. |
A generalized linear model was calculated to predict medication adherence based on patients’ demographic and clinical characteristics. A significant regression equation was found (F (9,412) =1.961, p≤0.05), with an R2 of 0.203 (Tables 4 and 5). The simple linear regression model indicated that smoking status is a significant predictor of medication adherence among the enrolled patients, b=−0.118, t=−2.397, p=0.017 (Table 6).
 |
Table 4 Model Summary |
 |
Table 5 ANOVA Test for Dependent Variable: GMAS11 |
 |
Table 6 Coefficients for Dependent Variable: GMAS11 |
An independent sample t-test was conducted to explore the significant statistical differences in medication adherence between the study participants. The test showed significant statistical differences in medication adherence between males (30.26±2.93) and females (29.66±3.23), t = 1.964, p=0.05. Moreover, the results showed significant statistical differences in the medications adherence between working patients (31.10±2.59) and patients retired (29.84±3.13), t =2.113, p=0.035 (see Table 7).
 |
Table 7 Independent Samples t-Test for the Differences in Medication Adherence |
A one-way analysis of variance (One-Way ANOVA) was conducted to determine the influence of independent variables (social status, educational level, monthly income, smoking status, using medications with or without prescription, year of starting to take medications, who are providing medications, cost of medications, and COVID-19 vaccination. The results showed that there were significant statistical differences in medication adherence referred to the variable (who is providing medication) at a significance level of p≤0.05 for the three conditions [F (2, 418) =7.317, p=0.001]. Moreover, there were significant statistical differences in medication adherence referred to the variable (cost of medication) at a significance level of p≤0.05 for the three conditions [F (2, 419) =5.230, p=0.006] (Table 8).
 |
Table 8 One Way ANOVA Test for the Differences in Medication Adherence |
Discussion
Medication adherence is a critical element in treating chronic diseases, and non-adherence among elderly patients is an issue facing health care providers. Previous studies report that measuring adherence and patient compliance is quite difficult and is patient-dependent most of the time.15–18 Hence, this study aimed to assess medication adherence among elderly chronic disease patients in Saudi Arabia and factors influencing their medication adherence. We found that 64.9% of participants had a high level of medication adherence, 21.3% had a good level of adherence, 13.3% had a partial level of adherence, and 0.5% had a low level of adherence. These findings rates are higher than those in previous studies that used different medication adherence assessment tools.19,20 One similar study in Saudi Arabia used the same tool to assess diabetic patients, reporting that a third of patients were (highly adherent 35.8%), (22.6% were good), (34.9% were partial), and (4.7% of patients had low medication adherence).21 The high level of adherence in this study might have been related to populations’ age (69.7±6.8); another study in Saudi Arabia founds a positive correlation between the level of adherence and age, high rates of adherence in patients aged 60 years and above.22 Furthermore, one factor that might have contributed to this finding was that we used validated Arabic translation questionnaires to ensure participants clearly understood the questions.13
Although a few of enrolled participants were smokers in this study, however, smoking was found to be a significant predictor of medication adherence (P = 0.017), this finding was also reported by other similar studies.33 Gender showed a statistically significant correlation, where males were more adherent than females. However, in general, the effect of gender on the rate of adherence to medication in other research studies is contradictory. Some researchers found that female patients have better adherence.23 While other studies could not find a relationship between gender and adherence to medication.24
Family support plays a beneficial role in the treatment and medication adherence.25 In this study, we asked the patients if they take medications by themselves or with the assistance of family members. The results show a significant correlation between family help in giving medication and the level of adherence (P=0.001). Similar findings were also noticed in different studies.20,26
One of the factors that may determine the affordability for the health care services and medication adherence is the financial status of the study subjects or their family and health insurance coverage. However, in this study, the monthly income had no statistically significant difference in the different levels of adherence (p= 0.404). This finding may be because patients usually do not need to pay for their medications in government hospitals. However, there was a significant correlation between medication cost consideration and the level of adherence in this study (P=0.006).
The education level may play a positive role in improving medication adherence by understanding the nature of their disease and the importance of treatment. However, this study failed to show the correlation between educational status and medication adherence (0.200). Otherwise, other studies have shown a positive correlation between educational status and adherence level.27,28
Although few patients were employed in this study group, there was a significant positive correlation with adherence. Similar positive correlations were found in some previous studies.29,30 However, the impact of employment status showed inconsistent results and thus, was mostly uncertain.24
This study was implemented during the COVID-19 pandemic and how it has strongly impacted the whole world in various dimensions, including the rising mortality risk in older patients with chronic diseases.31,32 Therefore, we asked patients if the pandemic positively or negatively impacted their medication adherence; the results showed no statistically significant association with medication adherence.
In this study, several limitations have been recognized. The first is the small sample size. Second, during data collection, some patients gave typical answers because they feared stopping drug provision from the hospital for non-adherence. Finally, participants were interviewed by telephone calls, which may affect the understanding in elderly patients, and it would be better to use personal interviews if the COVID-19 precautionary measures are elevated. Also, this is cross-sectional study and should not be generalized for the entire Saudi geriatric population because this study was conducted in an academic tertiary hospital which may be why most of the participants are adherent to their medication as most of them are retired academic staff.
Conclusion
A high level of adherence to medication was found among the geriatric population with chronic diseases in our study. However, this cannot be generalized to all geriatric population in Saudi Arabia. In addition, on the basis of the associated factors, an educational program for healthcare professions in primary care clinics should be developed and modified to deliver an appropriate message for the assessment of adherence to medication and address the associated factors. We recommend that researchers use more than one assessment tool, subjective and objective measurement, to better assess medication adherence levels among geriatric populations and understand factors that may trigger non-adherence in this group.
Acknowledgment
The authors would like to express special gratitude to the College of Medicine Research Center, Deanship of Scientific Research, King Saud University, Riyadh, KSA for their support. The authors would like also to thank the King Saud University Medical City (KSUMC) for its unlimited support represented in the materials, laboratories, use of infrastructure, human resources, and allowing the authors to conduct this research in the facility. Furthermore, we would thank Dr. Bushra A. Kakandi from the College of Medicine, King Saud University, for contributing to data collection.
Funding
This project was supported by the College of Medicine Research Centre, Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. World Health Organization. Ageing and health; 2018. Available from: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health.
2. Saquib N, Saquib J, Alhadlag A, et al. Chronic disease prevalence among elderly Saudi men. Int J Health Sci. 2017;11(5):11–16.
3. Khoja AT, Aljawadi MH, Al-Shammari SA, et al. The health of Saudi older adults; results from the Saudi National Survey for Elderly Health (SNSEH).. Saudi Pharm J. 2018;26:292–300. doi:10.1016/j.jsps.2017.11.008
4. Fabbri E, Zoli M, Gonzalez-Freire M, et al. Aging and multimorbidity: new tasks, priorities, and frontiers for integrated gerontological and clinical research. J Am Med Dir Assoc. 2015;16:640–647. doi:10.1016/j.jamda.2015.03.013
5. Lehnert T, Heider D, Leicht H, et al. Health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev. 2011;68:387–420. doi:10.1177/1077558711399580
6. Pasina L, Brucato AL, Falcone C, et al. Medication non-adherence among elderly patients newly discharged and receiving polypharmacy. Drugs Aging. 2014;31:283–289. doi:10.1007/s40266-014-0163-7
7. Bazargan M, Smith J, Yazdanshenas H, et al. Non-adherence to medication regimens among older African-American adults. BMC Geriatr. 2017;17:1–12. doi:10.1186/s12877-017-0558-5
8. Sabaté E. Adherence to Long-Term Therapies: Evidence for Action. World Health Organization; 2003.
9. Iuga AO, McGuire MJ. Adherence and health care costs. Risk Manag Healthc Policy. 2014;7:35. doi:10.2147/RMHP.S19801
10. Félix IB, Henriques A. Medication adherence and related determinants in older people with multimorbidity: a cross‐sectional study. Nurs Forum. 2021;56:834–843. doi:10.1111/nuf.12619
11. Alalaqi A, Lawson G, Obaid Y, et al. Adherence to cardiovascular pharmacotherapy by patients in Iraq: a mixed methods assessment using quantitative dried blood spot analysis and the 8-item morisky medication adherence scale. PLoS One. 2021;16(5):e0251115. doi:10.1371/journal.pone.0251115
12. Naqvi AA, AlShayban DM, Ghori SA, et al. Validation of the general medication adherence scale in Saudi patients with chronic diseases. Front Pharmacol. 2019;10:633. doi:10.3389/fphar.2019.00633
13. Naqvi AA, Mahmoud MA, AlShayban DM, et al. Translation and validation of the Arabic version of the General Medication Adherence Scale (GMAS) in Saudi patients with chronic illnesses. Saudi Pharm J. 2020;28(9):1055–1061. doi:10.1016/j.jsps.2020.07.005
14. Naqvi AA, Hassali MA, Rizvi M, et al. Development and validation of a novel General Medication Adherence Scale (GMAS) for chronic illness patients in Pakistan. Front Pharmacol. 2018;9(9):1124. doi:10.3389/fphar.2018.01124
15. Yap AF, Thirumoorthy T, Kwan YH. Systematic review of the barriers affecting medication adherence in older adults. Geriatr Gerontol Int. 2016;16(10):1093–1101. doi:10.1111/ggi.12616
16. Chisholm-Burns MA, Spivey CA. The cost of medication nonadherence: consequences we cannot afford to accept. J Am Pharm Assoc. 2012;52(6):823–826. doi:10.1331/JAPhA.2012.11088
17. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–497. doi:10.1056/NEJMra050100
18. Brundisini F, Vanstone M, Hulan D, et al. Type 2 diabetes patients’ and providers’ differing perspectives on medication nonadherence: a qualitative meta-synthesis. BMC Health Serv Res. 2015;15(1):1–23. doi:10.1186/s12913-015-1174-8
19. Tourkmani AM, Al Khashan HI, AlBabtain MA, et al. Medication adherence among patients in a chronic disease clinic. Saudi Med J. 2012;33(12):1278–1284.
20. Shruthi R, Jyothi R, Pundarikaksha HP, et al. A study of medication compliance in geriatric patients with chronic illnesses at a tertiary care hospital. JCDR. 2016;10(12):FC40. doi:10.7860/JCDR/2016/21908.9088
21. AlQarni K, AlQarni EA, Naqvi AA, et al. Assessment of medication adherence in Saudi patients with type II diabetes mellitus in Khobar City, Saudi Arabia. Front Pharmacol. 2019;10:1306. doi:10.3389/fphar.2019.01306
22. Altuwairqi HB. Barriers to medication adherence among cardiac patients following at King Fahad Medical City, Riyadh, Saudi Arabia. Saudi J Med Med Sci. 2016;5(1):20. doi:10.4103/2278-0521.182861
23. Jin J, Sklar GE, Oh VM, et al. Factors affecting therapeutic compliance: a review from the patient’s perspective. Ther Clin Risk Manag. 2008;4(1):269. doi:10.2147/TCRM.S1458
24. Gast A, Mathes T. Medication adherence influencing factors—an (updated) overview of systematic reviews. Syst Rev. 2019;8(1):1–7. doi:10.1186/s13643-019-1014-8
25. Kasznicki J, Głowacka A, Drzewoski J. Type 2 diabetic patients’ compliance with drug therapy and glycaemic control. Diabetologia Doswiadczalna i Kliniczna. 2007;7(4):199.
26. Voils CI, Steffens DC, Bosworth HB, et al. Social support and locus of control as predictors of adherence to antidepressant medication in an elderly population. Am J Geriatr Psychiatry. 2005;13(2):157–165. doi:10.1097/00019442-200502000-00010
27. Nichols-English G, Poirier S. Optimizing adherence to pharmaceutical care plans. JAPHA-WASHINGTON. 2000;40(4):475.
28. MacLaughlin EJ, Raehl CL, Treadway AK, et al. Assessing medication adherence in the elderly. Drugs Aging. 2005;22(3):231–255. doi:10.2165/00002512-200522030-00005
29. Gemeda DH, Gebretsadik LA, Dejene T, et al. Determinants of non-compliance with antiretroviral therapy among adults living with HIV/AIDS: a systematic review. JBI Evid Synth. 2012;10(56):3596–3648.
30. Nachega JB, Uthman OA, Peltzer K, et al. Association between antiretroviral therapy adherence and employment status: systematic review and meta-analysis. Bull World Health Organ. 2014;93:29–41. doi:10.2471/BLT.14.138149
31. SeyedAlinaghi S, Abbasian L, Solduzian M, et al. Predictors of the prolonged recovery period in COVID-19 patients: a cross-sectional study. Eur J Med Res. 2021;26(1):1. doi:10.1186/s40001-021-00513-x
32. Lim JP, Low KY, Lin NJ, et al. Predictors for development of critical illness amongst older adults with COVID-19: beyond age to age-associated factors. Arch Gerontol Geriatr. 2021;94:104331. doi:10.1016/j.archger.2020.104331
33. Mirahmadizadeh A, Khorshidsavar H, Seif M, et al. Adherence to medication, diet and physical activity and the associated factors amongst patients with type 2 diabetes. Diabetes Ther. 2020;11(2):479–494. doi:10.1007/s13300-019-00750-8
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
