Back to Journals » Patient Preference and Adherence » Volume 13
Mechanisms for improving diabetes patient–provider communication through optimal use of e-clinical technologies
Authors Khurana L, Durand EM, Gary ST, Otero AV, Dumais KM , Beck J, Zurakowski D, Hall CT, Dallabrida SM
Received 27 February 2019
Accepted for publication 2 May 2019
Published 24 June 2019 Volume 2019:13 Pages 981—992
DOI https://doi.org/10.2147/PPA.S207008
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Laura Khurana,1 Ellen M Durand,1 Sarah Tressel Gary,1 Antonio V Otero,1 Kelly M Dumais,1 Jamie Beck,1 David Zurakowski,2 Christine Teel Hall,1 Susan M Dallabrida1
1eResearch Technology (ERT), Boston, MA, USA; 2Harvard Medical School, Boston Children’s Hospital, Boston, MA, USA
Purpose: Effective health care and patient adherence to their prescribed regimens relies on successful communication between patients and their providers. This study examined mechanisms for optimizing patient–physician communication in subjects with type 2 diabetes, with a focus on optimizing the incorporation of e-clinical technology to improve engagement and communication.
Methods: A total of 105 subjects with type 2 diabetes participating in a large US mode equivalency study were surveyed independently of this trial. In addition to demographic information, each subject was queried on their familiarity with and preference for e-clinical technologies. Survey questions focused on mobile technology use, perceptions, and preferences for improving communication and interactions with health care providers.
Results: Subjects were diverse in age, sex, education, and ethnicity. Forty nine percent owned a smartphone, and 64% had a computer at home. Most subjects (81%) were interested in using electronic methods (eg, app on a smartphone, email, or text messages) to interact more with physicians between visits. The majority of subjects were interested in using technology to help manage their type 2 diabetes, including 62% favoring communicating with their health-care providers via email and a considerable fraction interested in using smartphones to be provided medication reminders (56%), clinical visit scheduling (55%), and text messaging (49%).
Conclusion: Subjects are interested in using electronic methods to increase communication with their physicians and manage their type 2 diabetes. Health-care providers should consider engaging patients with e-clinical technology to increase patient–physician communication and for the ultimate goal of improved health care.
Keywords: technology, eCOA, preferences, electronic, smartphone
A Letter to the Editor has been published for this article
Plain language summary
Many patients are not satisfied with how their doctors communicate with them. Patients want to be more involved in planning their care and making decisions about their treatment. It is often difficult for patients to understand all the instructions from their doctors, especially when they receive too much information at one time. This is especially true for patients with chronic diseases, such as diabetes, where treatment is complicated and lifelong. Using electronic methods, such as smartphones, email, or text message, may help improve communication between patients and doctors. We surveyed 105 participants with type 2 diabetes and found that most participants were interested in using electronic methods to communicate more with their doctors between visits. Participants showed interest in using email to communicate with their doctor, and using a smartphone for medication reminders and scheduling doctor visits. Patients need support and encouragement from their doctors, especially when dealing with lifelong complicated treatments, such as for type 2 diabetes. Our study shows that patients with type 2 diabetes are willing and interested in using electronic methods to increase communication with their doctors to manage their disease. This suggests that health care providers should consider using electronic methods to increase communication with the goal to improve health care.
Introduction
Current costs of diabetes care and treatment account for 12% of global health-care expenditure. The US alone is projected to spend over $260 billion on diabetes care by 2030. The projected increase in costs is influenced by more patient visits and hospitalizations, medications, long-term care, and emergency care.1 By 2030, 552 million people worldwide will have diabetes, with the majority of these being type 2. The prevalence of type 2 diabetes is growing, presumably due to an increase in the aging and obese population.2
Type 2 diabetes is a chronic disease associated with many complications, including renal failure, lower-limb amputation, increased risk of stroke and tuberculosis, and visual impairment and blindness.3 Patients are prescribed complex therapeutic programs to prevent secondary complications, but adherence to these regimens is low.4,5 Treatment for type 2 diabetes and concomitant conditions is costly to health-care systems, and improved patient adherence could enhance the success of clinical care and ultimately reduce costs. Nevertheless, in developed countries patient adherence to long-term therapies for chronic conditions is only 50%.6 In the US, <2% of adults with diabetes undertake the full level of care that is recommended by the American Diabetes Association.7 This is largely influenced by the multifaceted nature of diabetes management, which requires major lifestyle and behavioral changes, including daily medication, improving diet and exercise habits, and regularly monitoring blood sugar and other disease-related symptoms.8
Improved adherence and compliance will have a beneficial impact on the health of individuals with type 2 diabetes. Patients who adhere to their prescribed medications, like insulin, demonstrate lower HbA1c levels and improved glycemic control than those that do not follow prescribed treatment regimens. This correlates with fewer hospitalizations, decreased duration of hospital stays, and overall lower treatment costs.9–11 Adherence to a low-fat or low-carbohydrate diet results in weight loss and improvements in glycemia, insulin sensitivity, and plasma-lipid levels in patients with type 2 diabetes.12,13 Furthermore, nonpharmacological intervention, such as diet modification and lifestyle adaptations, prevents the onset of type 2 diabetes in high-risk individuals.14
Consistent adherence to a treatment regimen is critical for patients to manage their type 2 diabetes. Nonadherence can result from multiple factors, but one major influence is patient–doctor communication. Many patients do not understand medical instructions they receive from physicians, and the amount of information provided at one time might be overwhelming. It has been reported that patients forget 40%–80% of treatment instructions they are given once they leave the clinic.15–17 Adherence is also impacted by the amount of medications patients are prescribed or the complexity of the treatment regimen. A study of primary-care physicians in Boston reported that almost 70% of their patients with type 2 diabetes required complex care and were prescribed an average of 20 different medications.18 Many patients are dissatisfied with how their physicians communicate with them. They feel that doctors do not understand or appreciate the challenges of keeping up with a daily regimen.19 Patients prefer that their physicians communicate more frequently about the effects of their conditions and monitor this information on a regular basis.19 Adherence metrics are reflective of the burden on individuals: patients with type 2 diabetes are more likely to adhere to medications than lifestyle changes, like improving diet and exercise.20–22 Successful diabetes clinical care and research relies on patient engagement and strong communication between patients and providers. Improving doctor–patient interactions through effective communication will likely help patients commit to these more challenging lifestyle adaptations.23,24
Utilizing electronic clinical (e-clinical) technology is potentially one method to achieve this goal. Access to individual electronic health records and patient portals are designed to improve patient–provider communications in the clinical setting, similarly to e-clinical technologies used within clinical trials. Collecting electronic clinical outcome assessments with smartphones or tablets enables additional access points for patient–provider communications via the provision of patient-connected suites of information, such as email, texts, reminders/alarms, clinic-visit scheduling, and educational and physician contact information in a centralized location.
Evidence shows that patients want to be more involved in planning their care, more involved in decisions about their treatment, and better supported to manage their conditions independently.25 Therefore, we predicted that patients with type 2 diabetes would be interested in using e-clinical technologies to improve communication with their provider. We propose that optimal implementation of such a technology platform will factor in patient preference and ease of use, and that incorporating such patient recommendations into e-clinical technology designs will lead to increased patient compliance and ultimately translate into improved clinical care.
Methods
Recruitment and IRB approval
Subjects with type 2 diabetes (n=105) were recruited from the general public in the Boston area via advertisements placed online and in newspapers, and screened over the phone. Eligible subjects then participated in a US randomized, crossover-design study examining the equivalence of paper and electronic (smartphone) modes of patient-reported outcome instrument administration. Both paper and electronic modes were administered on the same day, with a break between administrations, during which subjects completed demographic and health-care questionnaires on paper as distraction activities. It was these demographic and health-care questionnaires that were examined in the current study. All questionnaires were developed by the authors. The demographic questionnaire contained questions on basic demographics and technology use, and the health-care questionnaire contained questions on subjects’ understanding of their disease and preferences for using technology to manage their disease and interact with their health-care provider. This study was approved by the Copernicus Group institutional review board on April 21, 2014 and was conducted from June to October 2014.
Study population
Eligible subjects were 18 years of age or older, able to complete the surveys alone and in English, and provided signed informed consent that indicated an understanding of the study objectives and study procedures and a willingness to participate in the study. Eligible subjects reported that they had been told by a doctor or health professional that they had any of the following conditions: type 2 diabetes, high blood sugar, or sugar in their urine. Eligible subjects also responded “yes” to at least one of: Do you take insulin injections for your diabetes? or Do you take medicine for your diabetes, such as pills/tablets or injectable medications other than insulin? Subjects were excluded from this study if they reported having a traumatic brain injury or a psychiatric condition, such as dementia or schizophrenia. Subjects currently affected by alcohol or drug dependence were also excluded from the study. A total of 129 subjects were screened, and 105 completed the study.
Statistical analysis
Frequency and percentage tables were produced for all categorical and dichotomous variables. Data were further stratified by age, education, income, and smartphone usage. All analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA) or 10 (StataCorp, College Station, TX, USA).
All questions from the Demographic and Condition Questionnaire were evaluated against questions 8, 10, 20, and 22 from the Health care Questionnaire (see Supplementary material for text from these questions). Question 8 was evaluated as a binary (yes/no) variable for parts A–E. Question 10 was categorized into not preferred and preferred and assessed as a binary (not preferred/preferred). Subjects were asked to rank the four response options to question 10 from 0 to 3, with 0 being least likely preferred and 3 being most likely preferred. We categorized a response of 0 or 1 as not preferred and a response of 2 or 3 as preferred. Question 20 was categorized into interested (response of 1 or 2) and not interested (response of 3 or 4) and assessed as a binary variable. Question 22 was evaluated as a binary (yes/no) variable for parts A–D. Categorical variables were evaluated using χ2. Continuous variables were evaluated using an independent Student t-test. The impact of each technology-usage factor and patient interest in electronic communication with their physician was assessed using logistic regression, with ORs and 95% CIs used to measure the association. A two-tailed P<0.05 was considered statistically significant, based on the likelihood-ratio test.
Results
Subject demographics
Subjects who completed the study were 35–79 years old and 50% female. See Table 1 for demographic information. Subjects were diverse in ethnicity, education, relationship status, and income. Many had graduated high school (28%), finished some college or held a technical degree (36%), had a college degree (18%), or advanced degree (9%), and 4% had completed 8th grade or less. In sum, 40% of subjects had never been married, 26% were either separated or divorced, 60% reported an annual household income of <$20,000, and 3% reported over $100,000 annually. Forty nine percent reported owning a smartphone, and 51% reported that they did not own one. Almost half the subjects reported using a smartphone on a daily basis (45%), and 28% used them to track appointments. More than half of subjects sent text messages every day (53%), most (64%) reported having a computer in their home, and 58% had access to the Internet at home. Subjects indicated that they used the Internet on a daily (52%) or weekly (13%) basis, with the remainder using the Internet less frequently or not at all. Similarly, 54% and 11% of subjects reported using email on a daily or weekly basis, respectively. To browse the Internet, most subjects reported using a desktop or laptop (49%), followed by smartphones (14%), tablets (6%), and multiple devices (4%), with 28% not browsing the Internet.
 | Table 1 Diabetes-subject demographics |
Communicating disease information and knowledge
We asked subjects how they would like to communicate with physicians regarding treatment and disease information. When asked how often they would like to contact their physician between visits, 57% of subjects reported wanting to contact their physicians between visits as needed (Figure 1A). Others wanted to be able to contact their physicians on a weekly (15%) or monthly (25%) basis, while 3% preferred only to communicate with their physicians at scheduled visits (Figure 1A). Similarly, 61% of subjects wanted their physicians to contact them as needed between appointments, 9% and 28% preferred to be contacted by their doctors on a weekly or monthly basis, respectively, and 2% preferred only to communicate with their physicians at visits (Figure 1SA). In a multiple-selection question, subjects indicated that they would like their physicians to contact them between appointments by phone call (57%), email (27%), and text message (16%; Figure S1B).
 | Figure 1 Subject responses to questions related to physician communication (A) and disease knowledge (B). Subjects were allowed to select more than one response in part B (n=103). |
When subjects received information from physicians that was not clear to them, 30% reported waiting until their next clinical visit to get clarification, 22% turned to family or friends, and 21% performed Internet searches (Figure S1C). Only 19% of subjects called their physician to gain a better understanding of instructions (Figure S1C). However, 48% of subjects reported that they would prefer to ask any unanswered questions they had by calling their physicians (Figure S1D).
Subjects were more likely to take proactive measures if they had more information and knowledge about their disease. In a multiple-selection question, subjects indicated they would be more likely to speak with their physicians (46%), more likely to report disease symptoms (38%), more likely to report on their quality of life (37%), and more likely to take prescribed medications (32%) if they had more knowledge about their disease (Figure 1B). Age was an indicator as to whether or not subjects believed that more knowledge about their disease might impact their health. A higher percentage of patients aged 45 years and older felt that more knowledge might have an effect on their health compared to those aged 35–44 years (P=0.029). Although all subjects in the study were diagnosed with type 2 diabetes, subjects with certain concomitant diseases more often reported that with more knowledge about their disease, they would be more likely to take prescribed medications, specifically those with arthritis or rheumatism (P=0.047) and dermatitis or other chronic skin conditions (P=0.001). Those with hypertension reported that having more knowledge about their disease(s) would make them more likely to report on their quality of life to their physicians (P=0.025).
Managing disease with increased communication
Subjects reported that they would be able to manage their type 2 diabetes most effectively by communicating and sharing information more frequently with their providers. In a multiple-selection question, 40% of subjects stated they would be able to improve their health and manage/treat their disease most effectively by increasing communication and interactions with their physicians (Figure 2), 38% were interested in regularly monitoring and tracking their disease, symptoms, and/or medications electronically so that doctors could access their health status in real time (Figure 2), and 7% thought that changing to another physician would be most effective for managing their type 2 diabetes (Figure 2).
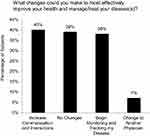 | Figure 2 Subject responses regarding self-care behaviors to improve health and manage/treat disease. Subjects were allowed to select more than one response (n=105). |
Subjects with congestive heart failure, or enlarged heart (P=0.008), or other heart conditions, such as problems with valves or rhythm of heartbeat (P=0.002), and those with osteoporosis (P=0.034) reported most often that monitoring and tracking their disease, symptoms, and/or medications electronically on a regular basis would be the change that would most effectively improve their health and management of disease. Subjects with other specific concomitant diseases reported the greatest likelihood of improving their health and managing their disease(s) with increased physician communication, specifically those with chronic allergies or sinus trouble (P=0.019), chronic back problems or sciatica (P=0.020), and osteoporosis (P=0.041).
Subjects who stated they were already doing everything possible to manage their disease experienced far fewer days (4±6 days) wherein their normal activities were affected by illness, injury, medical treatment, or other health problems compared to subjects who stated they could more effectively improve health and manage their disease by increasing communication with their physicians (11±15 days; P=0.004). Overall, subjects who indicated that increased communication and interaction with their physicians would improve their health more often reported that they sacrificed daily activities due to illness, injury, medical treatment, or other health problems (12±17 days) than those who did not report this (6±8 days; P=0.026).
When asked what types of information they would research, subjects were most likely to research their currently prescribed treatments (39%, Figure S1E), 24% were likely to research new drugs, 17% to investigate the impact of diet on their disease, and only 5% were likely to research the impact of exercise on their type 2 diabetes (Figure S1E).
Using electronic methods to increase communication
More than 80% of subjects surveyed were interested in using electronic methods to increase interactions with their physicians between visits in order to help manage and treat their disease (Figure 3A). Potential methods of communication included email, text messaging, or a smartphone application. Men were significantly more interested than women in using electronic methods to interact with their physicians between visits (P=0.042). Diabetes patients who used more technologies as a means of communication in their daily life were significantly more likely to have an interest in interacting with their physician by electronic methods. The five technology-usage factors associated with significantly increased odds of an interest in electronic methods to increase interactions with physicians between visits to help manage and treat their type 2 diabetes were access to the Internet at home (OR 3.64, P=0.024), owning a smartphone (OR 6.05, P=0.007), using a smartphone daily (OR 5.50, P=0.011), checking email daily (OR 2.80, P=0.048), and sending text messages daily (OR 4.90, P=0.009; Figure 3B).
In a multiple-selection question, subjects were asked which e-clinical method they would prefer to use to manage their disease better: 62% preferred to use email communication with their health-care providers, 55% preferred to schedule clinical visits using a smartphone, 56% preferred to get medication reminders on a smartphone, and 49% preferred to use text messaging to communicate with their health-care providers (Figure S1F).
Discussion
The current study suggests that adults with type 2 diabetes are willing and able to use e-clinical approaches to communicate more effectively with their health-care providers. It is widely accepted that patient adherence is a growing concern and a major health problem, particularly for chronic conditions like type 2 diabetes. Poor adherence has adverse clinical consequences for individuals with type 2 diabetes, including elevated risk of associated complications. For such reasons as associated costs, medical beliefs, or fear of reprimand, some patients are not straightforward with their doctors regarding noncompliance.26 This is detrimental to the treatment and management of their disease, as physicians cannot always determine the reason certain therapeutic regimens fail. In addition, poor adherence leads to increased hospitalizations, emergency care, and additional medical complications, which are a financial burden on patients and the general population.
One of the most significant barriers to adherence is patient–physician communication. This is especially critical for patients that require complex therapeutic regimens. Successful management of type 2 diabetes requires extensive alterations to lifestyle and behavior. More effective communication fostered by patient-preferred methods of interaction might help patients commit to multifaceted treatment regimens. This logic is twofold. First, consistent communication may improve medical literacy and confidence in clinical recommendations. Some patients do not understand treatment instructions or forget complex regimens. Our study demonstrates that even when subjects are confused by the information given to them by doctors, almost a third will wait until their next scheduled appointment for clarification. Recently, adherence has been linked to patients’ perception of medicine and the effectiveness of different treatments in disease management.27 Patients with type 2 diabetes rank medications as higher in importance than diet or exercise for managing disease. This corresponds with better adherence to prescriptions than alterations in behavior or lifestyle.28 Adherence may be improved by changing the perceptions patients have of the effectiveness of treatment regimens on managing disease. Continued patient–provider communication through e-clinical technology may achieve this goal.
Secondly, individuals struggle with making daily changes to their behavior and lifestyle. Only 5% of subjects in this study were likely to research the impact of exercise on their type 2 diabetes, while 7% were likely to investigate alternative treatments. Patients need more support and understanding from their physicians so that they are encouraged to commit to a regimen and are not permanently discouraged when they temporarily waver. Structured and individualized care for people with type 2 diabetes improves compliance and wellness. Patients are more likely to adhere to treatment regimens when they communicate and set goals together with a physician.29 In addition, greater patient-perceived communication quality at diagnosis is associated with better self-care.30 Continuity of provider also improves glycemic control and diet management in patients with type 2 diabetes, and is an important factor for good health-related quality of life.8,31 Similarly, we observed that only 7% of subjects believed changing physicians would improve their health and management of disease. This suggests that continuity of physician care is important to individuals with type 2 diabetes.
Conclusion
Currently, there are no variables to predict patient adherence and no definitive methods known to improve compliance. However, a significant barrier to adherence is poor patient–physician communication. Management of type 2 diabetes requires constant and consistent care, and adherence to complicated therapeutic regimens. This is perceived as a daily burden by many patients. Patients must be properly informed on the medical consequences of adherence on disease management. Individuals need support and encouragement from providers as they commit to lifelong, complex treatment regimens. Patients with type 2 diabetes prefer to communicate frequently with their physicians, and are willing and able to use technology to achieve this. Incorporating e-clinical technologies may increase patient compliance and ultimately improve patient health, and prevent the progressive nature of type 2 diabetes and associated clinical sequelae.
Abbreviation list
e-clinical, electronic clinical; eCOA, electronic clinical outcome assessments; SMS, short-message service
Acknowledgments
The authors would like to acknowledge the subjects who participated in the study. The authors would also like to acknowledge Optum for assistance in designing the study protocol for the equivalence study, and Endpoint Outcomes for assistance in executing the study. This work was supported by eResearch Technology (ERT).
Disclosure
The authors LK, EMD, STG, AVO, KMD, JB, CH, and SMD are current or past employees of ERT. The authors report no other conflicts of interest in this work.
References
1. Zhang P, Zhang X, Brown J, et al. Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(3):293–301. doi:10.1016/j.diabres.2010.01.026
2. García-Pérez L-E, Alvarez M, Dilla T, Gil-Guillén V, Orozco-Beltrán D. Adherence to therapies in patients with type 2 diabetes. Diabetes Ther. 2013;4(2):175–194. doi:10.1007/s13300-013-0034-y
3.
4. Mannucci E, Monami M, Lamanna C, Gori F, Marchionni N. Prevention of cardiovascular disease through glycemic control in type 2 diabetes: a meta-analysis of randomized clinical trials. Nutr Metab Cardiovasc Dis. 2009;19(9):604–612. doi:10.1016/j.numecd.2009.03.021
5. Donnelly LA, Doney ASF, Morrist AD, Palmer CNA, Donnan PT. Long-term adherence to statin treatment in diabetes. Diabet Med. 2008;25(7):850–855. doi:10.1111/j.1464-5491.2008.02476.x
6.
7. Beckles GL, Engelgau NM, Venkat Narayan KM, et al. Population- based assessment of the level of care among adults with diabetes in the U.S. Diabetes Care. 1998;21(9):1432–1438.
8. Parchman ML, Pugh JA, Noël PH, Larme AC. Continuity of care, self-management behaviors, and glucose control in patients with type 2 diabetes. Med Care. 2002;40(2):137–144. doi:10.1097/00005650-200202000-00008
9. Lee WC, Balu S, Cobden D, Joshi AV, Pashos CL. Medication adherence and the associated health-economic impact among patients with type 2 diabetes mellitus converting to insulin pen therapy: an analysis of third-party managed care claims data. Clin Ther. 2006;28(10):1712–1725. doi:10.1016/j.clinthera.2006.10.004
10. Donnelly LA, Morris AD, Evans JMM. Adherence to insulin and its association with glycaemic control in patients with type 2 diabetes. Q J Med. 2007;100(6):345–350. doi:10.1093/qjmed/hcm031
11. Rhee MK, Slocum W, Ziemer DC, et al. Patient adherence improves glycemic control. Diabetes Educ. 2005;31(2):240–250. doi:10.1177/0145721705274927
12. Barnard ND, Cohen J, Jenkins DJ, et al. A low-fat vegan diet and a conventional diabetes diet in the treatment of type 2 diabetes: A randomized, controlled, 74-wk clinical trial. Am J Clin Nutr. 2009;89(5). doi:10.3945/ajcn.2009.26736H
13. Boden GB, Sargrad K, Homko C, Mozzoli M, Stein TP. Effect of a low-carbohydrate diet on appetite, blood glucose levels, and insulin resistance in obese patients with type 2 diabetes. Ann Int Med. 2005;142:403–412. doi:10.7326/0003-4819-142-6-200503150-00006
14. Tuomilehto J, Indstrom J, Eriksson J, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344(18):1343–1350. doi:10.1056/NEJM200105033441801
15. Shankar J. Patients’ memory for medical information. J R Soc Med. 2003;96(10):520.
16. Ley P. Memory for medical information. Br J Clin Pyschology. 1979;18(2):245–255. doi:10.1111/j.2044-8260.1979.tb00333.x
17. Sherlock A, Brownie S. Patients’ recollection and understanding of informed consent: a literature review. ANZ J Surg. 2014;84:207–210. doi:10.1111/ans.12555
18. Grant RW, Wexler DJ, Ashburner JM, Hong CS, Atlast SJ. Characteristics of “complex” patients with type 2 diabetes mellitus according to their primary care physicians. Arch Intern Med. 2015;172(10):821–823.
19. Vermeire E, Van Royen P, Coenen S, Wens J, Denekens J. The adherence of type 2 diabetes patients to their therapeutic regimens: a qualitative study from the patient’s perspective. Pract Diabetes Int. 2003;20(6):209–214. doi:10.1002/pdi.505
20. Kurtz SM. Adherence to diabetes regimens: empirical status and clinical applications. Diabetes Educ. 1990;16(1):50–59. doi:10.1177/014572179001600112
21. Nelson KM, Reiber G, Boyko EJ. Diet and exercise among adults with type 2 diabetes. Diabetes Care. 2002;25(10):1722–1728. doi:10.2337/diacare.25.10.1722
22. Vijan S, Stuart NS, Fitzgerald JT, et al. Barriers to following dietary recommendations in type 2 diabetes. Diabet Med. 2005;22(1):32–38. doi:10.1111/j.1464-5491.2004.01342.x
23. Golin C, DiMatteo M, Gelberg L. The role of patient participation in the doctor visit. Implications for adherence to diabetes care. Diabetes Care. 1996;19(10):1153–1164. doi:10.2337/diacare.19.10.1153
24. Jackson SL, DesRoches CM, Frosch DL, Peacock S, Oster NV, Elmore JG. Will use of patient portals help to educate and communicate with patients with diabetes? Patient Educ Couns. 2018;101(5):956–959. doi:10.1016/j.pec.2017.11.004
25. Borg S, Palaszewski B, Gerdtham UG, Fredrik O, Roos P, Gudbjörnsdottir S. Patient-reported outcome measures and risk factors in a quality registry: a basis for more patient-centered diabetes care in Sweden. Int J Environ Res Public Health. 2014;11:12223–12246. doi:10.3390/ijerph111212223
26. Lapane KL, Dubé CE, Schneider KL, Quilliam BJ. Misperceptions of patients vs providers regarding medication-related communication issues. Am J Manag Care. 2007;13(11):613–618.
27. Harvey JN, Lawson VL. The importance of health belief models in determining self-care behaviour in diabetes. Diabet Med. 2009;26(1):5–13. doi:10.1111/j.1464-5491.2008.02628.x
28. Broadbent E, Donkin L, Stroh JC. Illness and treatment perceptions are associated with adherence to medications, diet, and exercise in diabetic patients. Diabetes Care. 2011;34(2):338–340. doi:10.2337/dc10-1779
29. Olivarius NDF, Beck-Nielsen H, Andreasen AH, Hørder M, Pedersen PA. Randomised controlled trial of structured personal care of type 2 diabetes mellitus. Bmj. 2001;323:1–9. doi:10.1136/bmj.323.7303.1
30. Polonsky WH, Capehorn M, Belton A, et al. Physician-patient communication at diagnosis of type 2 diabetes and its links to patient outcomes: new results from the global IntroDia® study. Diabetes Res Clin Pract. 2017;127:265–274. doi:10.1016/j.diabres.2017.03.016
31. Hänninen J, Takala J, Keinänen-Kiukaanniemi S. Good continuity of care may improve quality of life in type 2 diabetes. Diabetes Res Clin Pract. 2001;51(1):21–27. doi:10.1016/S0168-8227(00)00198-4
Supplementary material
Question 8: How do you think more knowledge about your disease(s) might impact your health? Please select all that apply.
Question 10: Which method would you prefer to use to help you better manage your disease? Please rank the options, with 3 being the most likely and 0 being the least likely.
___Text-message communication with your health-care provider
___Email communication with your health-care provider
___Medication reminders on a smartphone
___Clinical visit scheduling on a smartphone
Question 20: How interested are you in using electronic methods (eg, app on a smartphone, email, text messages) to interact more with your physician between visits to help manage and treat your disease(s)? Please select one answer.
Question 22: What changes could you make to most effectively improve your health and manage/treat your disease(s)? Select all that apply.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


