Back to Journals » International Medical Case Reports Journal » Volume 15
Long-Term Bilateral Poorly Treated Acute Syphilitic Posterior Placoid Chorioretinitis Complicated with Choroidal Neovascularization: A Case Report
Authors Vieira R , Furtado MJ
Received 26 April 2022
Accepted for publication 6 July 2022
Published 30 September 2022 Volume 2022:15 Pages 543—549
DOI https://doi.org/10.2147/IMCRJ.S369324
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Rita Vieira, Maria João Furtado
Ophthalmology Department of Centro Hospitalar Universitário do Porto (CHUPorto), Oporto, Portugal
Correspondence: Rita Vieira, Ophthalmology Department of Centro Hospitalar Universitário do Porto (CHUPorto)- Largo do Prof. Abel Salazar, Oporto, 4099-001, Portugal, Tel +351 913748812, Email [email protected]
Purpose: To describe a case of long-term poorly treated bilateral acute syphilitic posterior placoid chorioretinitis (ASPPC) complicated with choroidal neovascularization, with a multimodal imaging approach.
Patients and Methods: Retrospective case report. Analysis of patient’s clinical data.
Case Report: A healthy 66-year-old man complained of decreased visual acuity in the right eye (RE). He had a past history of bilateral exudative maculopathy of unknown etiology, lasting for more than 10 years and leading to severe and irreversible vision loss on the left eye. The corrected distance visual acuity (CDVA) was 20/63 on the RE and < 20/400 on the left eye (LE). On slit-lamp, no anterior chamber reaction was observed, a vitreous haze was present on the RE as well as large, bilateral yellowish lesions in the macula, with exuberant macular atrophy, particularly on the LE. These well-defined lesions were confined to the posterior pole. The spectral domain optical coherence tomography (SD-OCT) showed a flat retinal pigmented epithelium (RPE) detachment with hyperreflective material beneath the RPE and cystoid macular edema on the RE and an exuberant macular atrophy on the LE, with both eyes showing anomalous enlargement of choroidal vessels. The fluorescein angiography showed general hypofluorescence and indocyanine green angiography revealed a heterogeneous pattern. The OCT angiography (OCTA) of the RE demonstrated an anomalous vascular network related to the presence of choroidal neovascularization (CNV). An etiological study was performed and a positive treponemal test (TPHA) was found. The patient experienced visual acuity improvement to 20/25 after systemic treatment with Penicillin and anti-VEGF injections.
Conclusion: Clinical data and multimodal imaging information suggest that this case represents a complication of long-term untreated bilateral acute syphilitic posterior placoid chorioretinitis (ASPPC) with associated choroidal neovascularization. Once the RE presented signs of active disease, besides intravitreal anti-VEGF, treatment of the underlying disease was essential for visual recovery.
Keywords: ASPPC, syphilis, neovascularization, ocular syphilis
Introduction
Acquired syphilis is a chronic sexually transmitted disease caused by the spirochete Treponema pallidum. Syphilis, known as the great imitator, can affect any organ including the skin, heart, blood vessels, bone, nervous system, and the eye. Ocular syphilis is a relatively unusual manifestation of this infection, and it occurs more often during the secondary or latent stages of infection.1,2 As this disease can affect any organ and ophthalmological manifestations can be varied, Syphilis should always be considered in patients with uveitis. It’s prevalence among patients with uveitis can be up to 8%.3
The most common manifestation of ocular syphilis is uveitis, particularly the pan-uveitis. The posterior segment manifestations include vitreous haze, chorioretinitis, retinal vasculitis, venous occlusion, papilledema, and retrobulbar neuritis. The acute syphilitic posterior placoid chorioretinitis (ASPPC) is a distinct entity of ocular syphilis, that affects the outer retina and the inner choroid.1,4,5 Although most cases occur in immunosuppressed patients, particularly in HIV positive,1,5,6 some reports of ASPPC in immunocompetent patients have been published.
ASPPC, first described by Gass et al7 in 1988, consists of an uncommon manifestation of ocular syphilis. Clinically, ASPPC is characterized by the appearance of yellowish placoid lesions typically located in the macula, with no peripheral changes, and there is a profound loss of visual acuity. Spectral-domain optical coherence tomography (OCT) and fundus fluorescein angiography (FA) findings may help in diagnosis. OCT findings generally show hyper-reflectivity of the RPE with nodular elevations and loss of the ellipsoid zone (EZ); FA typically shows a hypofluorescent central lesion in the early phase and progressive hyperfluorescence in the later phases, although FA findings can be varied.1,8,9
After systemic adequate treatment with intravenous Penicillin G 18 to24 MU, improvement in visual acuity, in retinal structure, and OCT findings is generally observed.
In this report, we present a case of long-term bilateral acute syphilitic posterior placoid chorioretinitis (ASPPC) with associated choroidal neovascularization, in an immunocompetent healthy patient, that was not treated properly in the past.
Methods
This was a retrospective case report, after analysis of patient clinical data. This study was conducted in accordance with the Declaration of Helsinki (1964) and its latest amendment (Brazil, 2013). The patient provided written informed consent to publish their case details and any accompanying images. The study protocol complies with the requirements of the institute’s committee (“Departamento de Ensino, Formação e Investigação”) on human research and institutional approval was not required to publish the case details.
Case Report
A 66-year-old man, without known systemic diseases, was referred to our department with a progressive decrease in visual acuity of his right eye (RE).
He had been assisted at our department more than 10 years before due to exudative bilateral maculopathy of unknown etiology. At that time, exuberant atrophic macular abnormalities had been recorded in both eyes, more pronounced in the LE. He had been submitted to full dose photodynamic therapy with verteporfin (PDT) and several anti-VEGF intravitreal injections. He underwent cataract surgery with intraocular lens implant. In the last registered visit, he presented a corrected distance visual acuity (CDVA) of 20/32 on his RE and counting fingers on his LE.
The patient was lost to follow-up at our department for 10 years and he returned in December 2020 complaining of RE vision loss. The CDVA was 20/63 on the RE and counting fingers on the LE. On slit-lamp examination, no anterior chamber reaction was observed but a vitreous haze was present on the RE. Fundoscopy revealed bilateral large, yellowish lesions located in the macula, associated with significant atrophy, particularly in the LE (Figure 1). No changes were observed in peripheral retina.
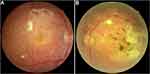 |
Figure 1 Fundus photography and RE (A) and LE (B), respectively. |
Optical coherence tomography (OCT) showed a flat retinal pigmented epithelium (RPE) detachment with hyper-reflective material under RPE, damage of external retinal layers, including external limiting membrane, ellipsoid zone and RPE, and cystoid macular edema on the RE (Figure 2A and B). The LE showed a large area of macular atrophy, with subretinal fibrosis (Figure 2C); both eyes exhibited an anomalous OCT pattern of the inner choroid with extensive loss of choriocapillaris. Fundus autofluorescence (FAF) showed central hypoautofluorescence secondary to RPE and photoreceptors loss (Figure 3).
The RE FA showed an early irregular pattern with significant late hyperfluorescence due to staining (Figure 4A). On the LE, a large early hypofluorescent lesion involving all macular areas and extending to the temporal optic disc border, with well-defined edges and late internal hyperfluorescent areas, was defined (Figure 4B). In the indocyanine green angiography (ICGA), an heterogenous pattern with anomalous dilated choroidal vessels could be observed (Figure 5).
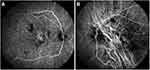 |
Figure 5 Indocyanin-green angiography of the RE (A) and LE (B). An heterogenous pattern and anomalous enlargement of choroidal vessels in the macular area is observed, particularly in the LE. |
The OCT angiography (OCTA) of the RE demonstrated an anomalous vascular network, suggestive of choroidal neovascularization (Figure 6).
 |
Figure 6 Angiography-OCT of the RE showing an anomalous vascular network. |
Systemic work-up revealed a positive TPHA test and a negative VDRL. The patient confirmed a known past history of syphilis of more than 30 years eventually treated with oral antibiotics, when living in a sub-Saharan African country. Since then, the patient did not develop any other symptoms or signs suggestive of syphilis. No other significant changes were found on the systemic work-up, including evidence of other infectious or immune diseases.
With collaboration of the Infectious Diseases department, the patient was admitted in the hospital and started systemic treatment with intravenous Penicillin G for 14 days as well as intravitreal ranibizumab injections on the RE in a PRN regimen.
After systemic and intravitreal treatment, the patient experienced visual acuity improvement to 20/25, without metamorphopsia. There was a regression of the RPE detachment and cystoid macular edema, since the first month after systemic treatment. Figure 7 shows macular OCT of the RE 1 month (7A) and 6 months (7B) after systemic treatment.
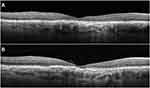 |
Figure 7 (A and B) Macular OCT of the RE in the last visit, 6 months after systemic treatment. |
A regular follow-up is maintained in order to evaluate the need for repeated intravitreal injections.
Discussion
Acute syphilitic posterior placoid chorioretinitis is a relatively uncommon manifestation of ocular syphilis. To date, searching on PubMed, there are only 68 reports of ASPPC.
Although systemic treatment of the underlying secondary syphilis or neurosyphilis is generally associated with disease resolution, spontaneous improvement had been reported in the literature.10–13 This fact may suggest that ASPPC is the result of cellular immune response that can locally control the infection. Also, it has been postulated that the immune privilege of the eye may play an important role in these spontaneous resolution case reports. Nevertheless, initial spontaneous resolution of ASPPC may not reflect a definitive cure.10 As Syphilis is characterized by intermittent episodes of active disease, placoid lesions may disappear for a long period and relapse years later. As an example, Baek et al14 reported a case of a 70-year-old man with diabetes, who presented with decreased visual acuity on the LE (6/96), bilateral yellowish placoid macular lesions in fundus examination, and a neurosensory retinal detachment on the LE. One week later, spontaneous visual acuity improvement was noticed and the placoid lesions disappeared as well as the subretinal fluid on the LE. Laboratory testing demonstrated a positive treponemal test, but the patient refused treatment since he experienced spontaneous improvement of his vision. Nine months later, the patient returned with complaints of severe bilateral visual acuity decrease, and a bilateral pan-uveitis was diagnosed. He was then submitted to intravenous Penicillin G for 14 days and 1 month later his vision improved significantly.
In our case, we cannot exclude the possibility of initial spontaneous resolution and posterior relapse of ocular Syphilis, considering past history of primary Syphilis more than 30 years before, not adequately treated. Taking into account the past medical history, serology results for Syphilis and compatible multimodal imaging findings, we established an untreated long-term ASPPC complicated with CNV as our first diagnosis hypothesis. The absence of typical secondary syphilitic cutaneous lesions caused a delay in diagnosis.
In fact, multimodal imaging may be an important tool to establish diagnosis in atypical and challenging cases. In a recent work, reported by Wong et al,15 a multimodal imaging study during 18 months of follow-up was performed, in order to study imagiology findings during the clinical course of ASPPC including the pre-placoid stage, placoid stage, and after treatment. In their study, there was a complete resolution of the irregular thickening of the RPE and hyperreflective dots within the retina and choroid, while autofluorescence showed bilateral persistence of the hypoautofluorescent spots in the juxtafoveal region 14 months after treatment. FA and ICGA showed total resolution 14 months after treatment. In our case, with the presence of chronic exuberant atrophic changes, we could not expect resolution of imaging findings after treatment. However, the RE experienced a significant improvement of visual acuity from 20/63 to 20/25, with resolution of metamorphopsia, which may be due to both intravenous Penicillin and anti-VEGF intravitreal injections. On the LE, the subretinal fibrosis was extensive and, as expected, no change in visual acuity was noticed by the patient.
Syphilitic CNV is exceptionally rare and difficult to distinguish among chorioretinal scars. In a recent report, Giuffrè et al16 demonstrated a case of syphilitic CNV that manifested 2 years after correct systemic treatment for bilateral chorioretinitis with a full course of antibiotics and steroids. Syphilitic CNV was then treated with a combination of anti-VEGF and oral corticosteroids after ruling out syphilitic reinfection by dosing the serum and cerebrospinal fluid VDRL titers.
In the present case, the hypothesis of reinfection was discarded after a negative nontreponemic testing with VDRL serum titers. Nevertheless, the patient underwent systemic intravenous Penicillin G for 14 days since he never received the correct treatment.
Conclusions
From our knowledge, there are only a few reports that associate syphilitic chorioretinitis with choroidal neovascularization.16–18
Our case reflects the natural course of a long-term ASPPC that was not properly treated in the past. It is possible that the continuous inflammatory stimulus on the outer retina may produce an ischemic environment that may lead to choroidal neovascularization.
This report aims to highlight that, even in cases of chronic maculopathy and severe retinal atrophy, past medical history and systemic work-up may help in establishing a diagnosis. Multimodal imaging findings proved crucial to support our diagnosis suspicion and to monitor patient evolution and treatment response throughout follow-up.
Consent Statement
The patient provided written informed consent to publish their case details and any accompanying images.
Funding
This study received no funding.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Eandi CM, Neri P, Adelman RA, Yannuzzi LA, Cunningham ET; International Syphilis Study Group. Acute syphilitic posterior placoid chorioretinitis: report of a case series and comprehensive review of the literature. Retina. 2012;32:1915–1941. doi:10.1097/IAE.0b013e31825f3851
2. Klausner JD. The great imitator revealed: syphilis. Top Antivir Med. 2019;27(2):71–74.
3. Aldave AJ, King JA, Cunningham ET. Ocular syphilis. Curr Opin Ophthalmol. 2001;12:433–441. doi:10.1097/00055735-200112000-00008
4. Plana-Pla A, Pelegrín-Colás L, Bielsa-Marsol I, Ferrandiz-Foraster C. Secondary syphilis presenting as oral lesions and posterior placoid chorioretinitis in an immunocompetent patient. Actas Dermosifiliogr. 2016;107(9):783–784. English, Spanish. doi:10.1016/j.ad.2016.04.023
5. Molina-Sócola FE, López-Herrero F, Medina-Tapia A, Rueda-Rueda T, Contreras-Díaz M, Sánchez-Vicente JL. Syphilitic posterior placoid chorioretinitis as initial presentation of early neurosyphilis. Arch Soc Esp Oftalmol. 2017;92(10):490–494. English, Spanish. doi:10.1016/j.oftal.2016.10.019
6. Baglivo E, Kapetanios A, Safran AB, et al. Fluorescein and indocyanine green angiographic features in acute syphilitic macular placoid chorioretinitis. Can J Ophthalmol. 2003;38:401–405. doi:10.1016/S0008-4182(03)80053-4
7. Gass JDM, Braunstein RA, Chenoweth RG. Acute syphilitic posterior placoid chorioretinitis. Ophthalmology. 1990;97:1288–1297. doi:10.1016/S0161-6420(90)32418-1
8. Wong W, Naing T, Bhargava M, Chee C, Lingam G, Holder GE. Acute syphilitic posterior placoid chorioretinitis. Retin Cases Brief Rep. 2019. doi:10.1097/icb.0000000000000896
9. Marchese A, Agarwal AK, Erba S, et al. Placoid lesions of the retina: progress in multimodal imaging and clinical perspective. Br J Ophthalmol. 2022;106:14–25. doi:10.1136/bjophthalmol-2020-318337
10. Casalino G, Erba S, Sivagnanavel V, Lari S, Scialdone A, Pavesio C. Spontaneous resolution of acute syphilitic posterior placoid chorioretinitis: reappraisal of the literature and pathogenetic insights. GMS Ophthalmol Cases. 2020;10:Doc26. doi:10.3205/oc000153
11. Ji YS, Yang JM, Park SW. Early resolved acute syphilitic posterior placoid chorioretinitis. Optom Vis Sci. 2015;92(4Suppl 1):S55–S58. doi:10.1097/OPX.0000000000000531
12. Aranda S, Amer R. Sequential spontaneous resolution of acute syphilitic posterior placoid chorioretinitis. Eur J Ophthalmol. 2015;25(3):263–265. doi:10.5301/ejo.5000530
13. Franco M, Nogueira V. Severe acute syphilitic posterior placoid chorioretinitis with complete spontaneous resolution: the natural course. GMS Ophthalmol Cases. 2016;6:Doc02. doi:10.3205/oc000039
14. Baek J, Kim KS, Lee WK. Natural course of untreated acute syphilitic posterior placoid chorioretinitis. Clin Exp Ophthalmol. 2016;44(5):431–433. doi:10.1111/ceo.12679
15. Wong W, Naing T, Bhargava M, Chee C, Lingam G, Holder GE. Acute syphilitic posterior placoid chorioretinitis: multimodal imaging and electrophysiologic findings before and after treatment. Retin Cases Brief Rep. 2021;15(6):662–669. doi:10.1097/ICB.0000000000000896
16. Giuffrè C, Marchese A, Cicinelli MV, et al. Multimodal imaging and treatment of syphilitic choroidal neovascularization. Retin Cases Brief Rep. 2022;16(1):85–88. doi:10.1097/ICB.0000000000000912
17. Balaskas K, Spencer S, D’Souza Y. Peripapillary choroidal neovascularization in the context of ocular syphilis is sensitive to combination antibiotic and corticosteroid treatment. Int Ophthalmol. 2013;33:159–162. doi:10.1007/s10792-012-9641-2
18. Halperin LS, Lewis H, Blumenkranz MS, et al. Choroidal neovascular membrane and other chorioretinal complica- tions in acquired syphilis. Am J Ophthalmol. 1989;108:554–562. doi:10.1016/0002-9394(89)90433-9
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



