Back to Journals » Journal of Pain Research » Volume 7
Liposomal bupivacaine infiltration into the transversus abdominis plane for postsurgical analgesia in open abdominal umbilical hernia repair: results from a cohort of 13 patients
Authors Feierman D, Kronenfeld M, Gupta PM, Younger N, Logvinskiy E
Received 29 March 2014
Accepted for publication 9 June 2014
Published 16 August 2014 Volume 2014:7 Pages 477—482
DOI https://doi.org/10.2147/JPR.S65151
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Dennis E Feierman, Mark Kronenfeld, Piyush M Gupta, Natalie Younger, Eduard Logvinskiy
Department of Anesthesiology, Maimonides Medical Center, Brooklyn, NY, USA
Background: Achieving adequate control of postsurgical pain remains a challenge in patients undergoing abdominal surgery. Transversus abdominis plane (TAP) infiltration has been shown to provide postsurgical analgesia following lower abdominal surgery. We assessed the safety and efficacy of a prolonged-release liposomal formulation of the local anesthetic bupivacaine administered via infiltration into the TAP in a cohort of patients undergoing open abdominal umbilical hernia repair.
Methods: Patients included in the study were 18–75 years of age, had American Society of Anesthesiologists physical classification status 1–3, and underwent open abdominal umbilical hernia repair with ultrasound-guided TAP infiltration immediately after surgery using an equal-volume bilateral infusion of liposomal bupivacaine 266 mg (diluted to 30 mL in normal saline). Outcome measures included patient-reported pain intensity (11-point numeric rating scale), satisfaction with postsurgical analgesia (5-point Likert scale), incidence of opioid-related adverse events, and time to first use of supplemental rescue analgesia.
Results: Thirteen patients underwent surgery and received bilateral TAP infiltration with liposomal bupivacaine; TAP infiltration failed in the first patient. Mean numeric rating scale pain scores were 0.6 immediately before TAP infiltration and remained ≤2.3 through 120 hours after infiltration; mean scores at 120 hours and 10 days were 0.9 and 0.4, respectively. Ten patients (77%) required supplemental analgesia; median time to first use was 11 hours. At discharge and day 10, 54% and 62% of patients, respectively, were “extremely satisfied” with postsurgical analgesia (Likert score 5). There were no opioid-related or other adverse events.
Conclusion: Although the current study was limited by both its lack of a control group and its small size, to our knowledge, it is the first published report on use of liposomal bupivacaine for TAP infiltration. In this cohort, liposomal bupivacaine was observed to be well tolerated with encouraging analgesic efficacy.
Keywords: analgesia, bupivacaine, hernia repair surgery, postoperative pain, infiltration anesthesia
Introduction
Achieving adequate postsurgical pain control remains a significant challenge for surgical teams. Despite efforts to reduce both the incidence and severity of postsurgical pain, results from patient surveys conducted during the past two decades suggest that there has been little improvement in these parameters, with high incidence rates of moderate to severe pain after surgery.1–3
Transversus abdominis plane (TAP) infiltration, which involves infiltration of local anesthetic into the TAP between the internal oblique and transversus abdominis muscles, has been used to provide postsurgical analgesia in a range of surgical procedures involving the middle or lower abdominal wall.4,5 This analgesic technique is aimed at sensory afferents of the lower thoracic and upper lumbar nerves. It was introduced as a landmark-based method in 2001, and has since been refined with the use of ultrasound guidance to improve the accuracy of anesthetic placement.4,5
A 2012 meta-analysis of nine studies evaluating TAP infiltration in abdominal surgery found that its use was associated with significant reductions in postsurgical opioid use and in the incidence of postoperative nausea and vomiting compared with placebo, as well as a trend toward reduced visual analog scale (VAS) pain scores.4 In patients undergoing inguinal hernia repair, randomized studies have shown that ultrasound-guided TAP infiltration significantly reduces postsurgical pain scores and postsurgical opioid use, compared with ilioinguinal/iliohypogastric nerve block6 or with conventional wound infiltration with local anesthetic.7
In our surgical practice, we have employed ultrasound-guided TAP infiltration using the local anesthetic bupivacaine HCl for patients undergoing inguinal hernia repair. There is little evidence in the published literature showing postsurgical analgesia lasting longer than 24 hours following TAP infiltration with traditional formulations of local anesthetics.6–9 In our practice, we have observed that TAP infiltration with bupivacaine HCl typically results in persistent analgesia for approximately 12–18 hours after surgery. A liposomal formulation of bupivacaine (Exparel®; bupivacaine liposome injectable suspension, Pacira Pharmaceuticals Inc., Parsippany, NJ, USA) was approved in 2011 for administration into the surgical site to produce postsurgical analgesia.10
In randomized, double-blind, controlled studies across a range of surgical models, liposomal bupivacaine has been found to reduce pain intensity scores and postsurgical opioid consumption, and to extend the time to first use of rescue analgesics, compared with placebo or bupivacaine HCl.11 A pooled analysis of data from ten clinical studies of liposomal bupivacaine showed that liposomal bupivacaine doses ≤266 mg were well tolerated, with rates of adverse events and serious adverse events that were lower than for bupivacaine HCl and comparable with placebo.12 In an open-label exploratory study of patients undergoing robotic laparoscopic prostatectomy, liposomal bupivacaine 266 mg administered via TAP infiltration was associated with low pain intensity scores (mean pain intensity scores remained ≤3 beginning at 6 hours postsurgery) and low opioid requirements (mean of ≈0.7 oxycodone 5 mg/acetaminophen 325 mg tablets consumed per day through day 10).13
The objective of this small cohort study was to evaluate the analgesic efficacy and safety of liposomal bupivacaine infiltration into the TAP in patients undergoing open abdominal umbilical hernia repair.
Patients and methods
This was a prospective, single-arm cohort study (ClinicalTrials.gov identifier NCT01801124) conducted at Maimonides Medical Center, Brooklyn, NY, USA, from July to December 2012. The protocol was reviewed and approved by the institutional review board at Maimonides Medical Center and the study was conducted in accordance with the International Conference on Harmonisation Guidelines for Good Clinical Practice. All patients provided their written informed consent prior to participation.
The study included adult male and female patients, 18–75 years of age, undergoing open abdominal umbilical hernia repair under general anesthesia, with an incision length of 3–12 cm and American Society of Anesthesiologists physical classification status of 1–3.
Short-acting analgesics, such as fentanyl, were permitted during surgery; intraoperative use of other analgesics was not permitted. Liposomal bupivacaine was administered at the end of surgery prior to the end of general anesthesia using a standardized infiltration protocol, with an identical syringe size, needle gauge, needle placement, and infiltration rate for all patients. Using ultrasound guidance, the TAP was identified using hydrodissection. Once the TAP was identified, 5 mL of preservative-free 0.9% sodium chloride (normal saline) was injected followed by 15 mL of diluted liposomal bupivacaine; a total of 266 mg of liposomal bupivacaine was used bilaterally (original volume of 20 mL diluted with normal saline to a total volume of 30 mL was infiltrated bilaterally, 15 mL on each side, into the TAP). After surgery, all patients were provided access to supplemental (rescue) analgesics.
The primary outcome measure was postsurgical analgesia, assessed by reviewing patient-reported pain intensity based on an 11-point numeric rating scale (NRS; 0= no pain, 10= worst possible pain) prior to liposomal bupivacaine infiltration (time 0) and at 2, 4, 8, 12, 24, 48, 72, 96, and 120 hours, and approximately 10±5 days after infiltration. Other outcome measures included time to first administration of supplemental analgesia after TAP infiltration; incidence of opioid-related adverse events (defined as somnolence, respiratory depression, hypoventilation, hypoxia, dry mouth, nausea, vomiting, constipation, urinary retention, sedation, confusion, pruritus, and ileus); and overall satisfaction with postsurgical analgesia (patient-reported, using a 5-point Likert scale whereby 1= not at all satisfied and 5= extremely satisfied) at hospital discharge and 10 days after surgery. All data were summarized and reported using descriptive statistics. Adverse events and serious adverse events were monitored and reported through postsurgical day 30.
Results
A total of 13 patients were enrolled, underwent surgery as planned, and completed 30 days of follow-up. All patients were included in the analysis, and their demographics and baseline characteristics are summarized in Table 1. All patients were younger than 65 years of age; most were Caucasian and had an American Society of Anesthesiologists physical classification status of 1 or 2. Eleven patients underwent intraperitoneal umbilical repair (ten with mesh and one without mesh) and two underwent preperitoneal umbilical repair (one with mesh and one without mesh). The mean surgical incision length was 4.9 (3–9) cm. Three patients were admitted to the hospital (one patient overnight and two patients for 2 days).
  | Table 1 Patient demographics and baseline characteristics (n=13) |
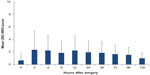
Mean patient-reported NRS scores for pain intensity remained below 2.3 from prior to liposomal bupivacaine infiltration (mean NRS score 0.6) through 120 hours after infiltration (mean NRS score 0.9; Figure 1) and decreased to 0.4 by day 10. TAP infiltration failed in the first patient, who reported no analgesia from the TAP block, experienced significant postsurgical pain, and was hospitalized overnight for pain control. Pain scores for this patient were recorded at the 2-hour and 24-hour pain intensity assessments only. Individual NRS scores of ≥5 were reported by three of the remaining 12 patients at one or more time points during the first 48 hours after surgery; thereafter, all observed scores were <5.
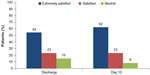
A total of ten patients (77%) required supplemental (rescue) analgesia during the first 72 hours postsurgery; the time to first postsurgical use of supplemental analgesia for these patients is shown in Figure 2. The median time to first use of supplemental analgesia was 11 (range <1 to 71) hours.
  | Figure 2 Time to first postsurgical use of supplemental analgesia for ten patients who requested rescue analgesia. Three patients (of 13) did not require supplemental analgesia. |
At the time of discharge, 54% of patients reported that they were extremely satisfied (a score of 5 on the 5-point Likert scale) with their postsurgical analgesia; at day 10, 62% reported that they were extremely satisfied (Figure 3). The mean patient-reported scores for satisfaction with postsurgical analgesia were 4.4 (maximum 5) at discharge and 4.6 at the day 10 postsurgical assessment. Of the three patients who were admitted for a hospital stay, two reported that they were “satisfied” with their postsurgical analgesia, and the third reported being “extremely satisfied”. There were no adverse events or serious (including opioid-related) adverse events reported during the study.
Discussion
Based on the postsurgical pain assessments that we used, ultrasound-guided TAP infiltration with liposomal bupivacaine appears to have provided good postsurgical analgesia in this exploratory study conducted in patients undergoing open abdominal umbilical hernia repair. Mean pain intensity scores remained low from the first postsurgical assessment (mean NRS score of 2.3 at the 2-hour assessment) through the 5-day and 10-day assessments (mean NRS scores of 0.9 and 0.4, respectively). Most patients were satisfied or extremely satisfied with their postsurgical analgesia at discharge and on day 10; and there were no opioid-related adverse events reported during the study.
Results from several recent systematic reviews and meta-analyses have shown TAP infiltration to provide good efficacy for postsurgical analgesia and a reduction in opioid use in various abdominal surgery settings,4,14–17 although there are only a few published studies in the setting of hernia repair.6–9 In a randomized, double-blind study (n=64), Salman et al8 compared a semi-blind approach to TAP infiltration using bupivacaine 0.25% with placebo infiltration in patients undergoing inguinal hernia repair. Compared with placebo, TAP infiltration was associated with a significant reduction in pain intensity scores (P<0.001), postsurgical opioid use (P<0.001), and intravenous acetaminophen use (P<0.02) during the 24-hour postsurgical period. Milone et al7 conducted a randomized study comparing ultrasound-guided TAP infiltration using levobupivacaine 0.5% plus conventional local anesthesia (n=50) with conventional local anesthesia alone (n=100). In their study, TAP infiltration significantly reduced VAS pain scores at rest and during movement at 6 hours and 12 hours postsurgery (P=0.001 at both assessments) but not at 24 hours postsurgery (P=0.1 for rest pain; P=0.07 for pain on movement). Significantly fewer patients in the TAP infiltration group required rescue analgesia with ketorolac compared with the control group (14% versus 32%; P=0.01).
The studies by Salman et al8 and Milone et al7 compared TAP infiltration with placebo (or no TAP infiltration) in patients undergoing open hernia repair procedures and showed TAP infiltration to be associated with significant reductions in VAS pain scores and less use of rescue analgesia compared with controls. In both studies, mean VAS scores in the placebo/no TAP infiltration group appeared to peak at around 6 hours postsurgery and declined thereafter; between-group differences remained statistically significant through 24 hours after surgery in the study by Salman et al.8 The lack of a control group and small sample size in the current study limits the ability to compare our results with those of these controlled studies, but the pattern of VAS scores in the TAP infiltration groups in the controlled studies was broadly similar to those we observed.
In a randomized study of ultrasound-guided TAP infiltration using levobupivacaine 0.5% (n=134) compared with conventional ilioinguinal/iliohypogastric nerve block (n=139), Aveline et al6 found that patients in the TAP infiltration group had significantly less pain at rest at 4 hours, 12 hours, and 24 hours postsurgery, but there were no between-group differences on postsurgical days 1 or 2. Another randomized, active-controlled and placebo-controlled study conducted by Petersen et al9 compared ultrasound-guided TAP infiltration with ropivacaine 0.75% (n=29) versus ilioinguinal nerve block plus wound infiltration using ropivacaine 0.375% (n=30) or placebo (n=27). There were no significant differences between the three treatment groups with respect to cumulative VAS pain scores from 0 to 24 hours postsurgery; however, cumulative pain scores from 0 to 6 hours postsurgery were significantly lower in the iliohypogastric nerve block group versus the TAP and placebo groups. Postsurgical morphine use was similar between the TAP and ilioinguinal nerve block groups.
The studies by Aveline et al6 and Petersen et al9 compared TAP infiltration with conventional analgesic approaches (iliohypogastric nerve block or ilioinguinal nerve block plus infiltration). In the Aveline et al6 study, TAP infiltration provided significantly improved analgesia through 24 hours, but pain scores in the two groups converged over time so the differences were no longer significant on postoperative days 1 and 2. In the study by Petersen et al,9 use of TAP infiltration proved no better than ilioinguinal nerve block plus infiltration with respect to pain scores and postsurgical morphine use. The results of the study by Petersen et al9 appear to contradict the results observed in the other controlled studies, which demonstrated significantly improved analgesia with TAP infiltration compared with traditional analgesic approaches.4
Taken as a group, the four studies described above are consistent with respect to the pattern of pain following hernia repair; in the placebo/no TAP infiltration groups, pain intensity appeared to peak around 6–12 hours postsurgery and declined thereafter. Given this pattern and the short duration of action of local anesthetics, the analgesic efficacy we observed with liposomal bupivacaine in this small study is encouraging.
Important limitations to interpretation of our results include the lack of a control group and the small size of our study cohort. In addition, several of the studies described above measured pain at rest and during movement, which may be advisable for evaluation of pain following hernia repair surgery, although the accepted “movement” after ventral hernia repair is not standardized.
Conclusion
Although there were limitations, the positive results observed in this study (low postsurgical pain scores, high levels of patient satisfaction, and lack of opioid-related adverse events when used in open abdominal umbilical hernia repair), suggest that liposomal bupivacaine may hold promise for providing prolonged postsurgical analgesia when administered for TAP infiltration.
Disclosure
This study was funded by Pacira Pharmaceuticals Inc. DEF, PMG, NY, and EL have nothing to disclose. MK was a member of the liposomal bupivacaine steering committee for Pacira Pharmaceuticals Inc.; his honorarium was given to the Maimonides Medical Center Anesthesia Department’s Educational Fund. He is a current member of the Pacira Pharmaceuticals Inc. advisory board for liposomal bupivacaine. This work has been the subject of a previous presentation at the International Anesthesia Research Society Annual Meeting on May 4–7, 2013, San Diego, CA, USA. Editorial assistance was provided by Peloton Advantage, LLC, and supported by Pacira Pharmaceuticals Inc. The authors are fully responsible for the content, editorial decisions, and opinions expressed in this work, and did not receive an honorarium related to the development of this manuscript.
References
Warfield CA, Kahn CH. Acute pain management. Programs in US hospitals and experiences and attitudes among US adults. Anesthesiology. 1995;83:1090−1094. | |
Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003;97:534−540. | |
Gan TJ, Habib AS, White W, Miller T. Postoperative pain continues to be undermanaged. Abstract presented at the Annual Fall Pain Meeting and Workshops of the American Society of Regional Anesthesia and Pain Medicine, Miami Beach, FL, USA, November 15−18, 2012. | |
Johns N, O’Neill S, Ventham NT, et al. Clinical effectiveness of transversus abdominis plane (TAP) block in abdominal surgery: a systematic review and meta-analysis. Colorectal Dis. 2012;14:e635−e642. | |
Niraj G, Searle A, Mathews M, et al. Analgesic efficacy of ultrasound-guided transversus abdominis plane block in patients undergoing open appendicectomy. Br J Anaesth. 2009;103:601−615. | |
Aveline C, Le Hetet H, Le Roux A, et al. Comparison between ultrasound-guided transversus abdominis plane and conventional ilioinguinal/iliohypogastric nerve blocks for day-case open inguinal hernia repair. Br J Anaesth. 2011;106:380−386. | |
Milone M, Di Minno MN, Musella M, et al. Outpatient inguinal hernia repair under local anaesthesia: feasibility and efficacy of ultrasound-guided transversus abdominis plane block. Hernia. 2013;17:749−755. | |
Salman AE, Yetisir F, Yurekli B, et al. The efficacy of the semi-blind approach of transversus abdominis plane block on postoperative analgesia in patients undergoing inguinal hernia repair: a prospective randomized double-blind study. Local Reg Anesth. 2013;6:1−7. | |
Petersen PL, Mathiesen O, Stjernholm P, et al. The effect of transversus abdominis plane block or local anaesthetic infiltration in inguinal hernia repair: a randomised clinical trial. Eur J Anaesthesiol. 2013;30:415−421. | |
Exparel [package insert]. Parsippany, NJ, USA: Pacira Pharmaceuticals Inc.; 2012. | |
Bergese SD, Ramamoorthy S, Patou G, et al. Efficacy profile of liposome bupivacaine, a novel formulation of bupivacaine for postsurgical analgesia. J Pain Res. 2012;5:107−116. | |
Viscusi ER, Sinatra R, Onel E, Ramamoorthy SL. The safety of liposome bupivacaine, a novel local analgesic formulation. Clin J Pain. 2014;30:102−110. | |
Sternlicht A, Shapiro M, Robelen G, et al. Initial findings using EXPAREL® (bupivacaine liposome injectable suspension) via infiltration into the transversus abdominis plane (TAP) for postsurgical analgesia in robotic prostatectomy. Abstract presented at the Annual Fall Pain Meeting and Workshops of the American Society of Regional Anesthesia and Pain Medicine, Miami Beach, FL, USA, November 15−18, 2012. | |
Champaneria R, Shah L, Geoghegan J, et al. Analgesic effectiveness of transversus abdominis plane blocks after hysterectomy: a meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2013;166:1−9. | |
Abdallah FW, Halpern SH, Margarido CB. Transversus abdominis plane block for postoperative analgesia after Caesarean delivery performed under spinal anaesthesia? A systematic review and meta-analysis. Br J Anaesth. 2012;109:679−687. | |
Mishriky BM, George RB, Habib AS. Transversus abdominis plane block for analgesia after Cesarean delivery: a systematic review and meta-analysis. Can J Anaesth. 2012;59:766−778. | |
Charlton S, Cyna AM, Middleton P, Griffiths JD. Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. Cochrane Database Syst Rev. 2010;12:CD007705. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.