Back to Journals » Infection and Drug Resistance » Volume 9
Lemierre’s syndrome: current perspectives on diagnosis and management
Authors Johannesen K, Bodtger U
Received 4 July 2016
Accepted for publication 4 August 2016
Published 14 September 2016 Volume 2016:9 Pages 221—227
DOI https://doi.org/10.2147/IDR.S95050
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Video abstract presented by Katrine M Johannesen.
Views: 4079
Katrine M Johannesen,1 Uffe Bodtger1–3
1Department of Lung Medicine, Naestved Hospital, Naestved, 2Institute for Regional Health Research, University of Southern Denmark, Odense, 3Department of Pulmonology, Zealand University Hospital, Roskilde, Denmark
Abstract: This is a systematic review of cases with Lemierre’s syndrome (LS) in the past 5 years. LS is characterized by sepsis often evolving after a sore throat or tonsillitis and then complicated by various septic emboli and thrombosis of the internal jugular vein. Symptoms include sepsis, pain, and/or swelling in the throat or neck, as well as respiratory symptoms. Laboratory findings show elevated infectious parameters and radiological findings show thrombosis of the internal jugular vein and emboli in the lungs or other organs. The syndrome is often associated with an infection with Fusobacterium necrophorum. We found a total of 137 cases of LS, of which 47 were infected with F. necrophorum and others with Staphylococcus and Streptococcus. Complications of this rare but severe disease included osteomyelitis, meningitis, and acute respiratory distress syndrome. Mortality was extremely high in the pre-antibiotic era but has diminished with the advent of antibiotics. This review showed a mortality rate of only 2% of which none of the cases involved fusobacteria. Duration of treatment varied; a 4–6-week course of carbapenem or piperacillin/tazobactam in combination with metronidazole was optimum. Other treatment options included anticoagulants in 46% of cases, which is unwarrantedly high, as to date, no evidence of the positive effects of anticoagulants in LS exists. Only two cases had ligation of the internal jugular vein performed. This review confirms the rare, but severe aspects of LS. Mortality from LS in this day and age appears to be low, however the syndrome is difficult to recognize, and still requires the full attention of the clinician.
Keywords: Lemierre’s syndrome, fusobacteria, postanginal sepsis
Definition
Lemierre’s syndrome (LS) takes its name after the French bacteriologist André-Alfred Lemierre, who first described the syndrome in 1936.1 The syndrome is defined by a pharyngeal infection, complicated by septicemia and internal jugular vein thrombosis followed by septic emboli. Due to the introduction of antibiotics, LS has aptly been referred to as “the forgotten disease”. The most commonly involved bacteria is Fusobacterium necrophorum but other bacteria such as fusobacteria, Streptococcus, Staphylococcus, and Enterococcus are commonly found in cultures.2 Other bacteria, such as Klebsiella Pneumoniae have rarely been described in middle-aged persons with newly diagnosed type 2 diabetes.3
Patients with LS present with a prolonged sore throat, neck pain, and often with fever.4 Patients are often young (age 16–30 years) and otherwise healthy, but appear acutely ill with tachycardia, tachypnea, hypotension, and a poor saturation (often <95%).2,3,5,6 Laboratory findings showed leukocytosis with dominating neutrocytosis and elevated C-reactive protein as well as signs of organ failure, such as elevated liver enzymes. Imaging of the internal jugular vein showed thrombosis.2,5
Complications to this severe syndrome include a mortality rate as high as 10%,3 especially when antibiotic treatment is delayed.7 Other less severe complications include metastatic infections in joints, internal organs (often lungs), and/or the brain.6
Fusobacterium necrophorum has a reputation for being resistant to penicillin, thus the drugs of choice have primarily been β-lactamase-resistant β-lactams, such as piperacillin–tazobactam, even though many strains are sensitive to penicillin in combination with metronidazole.4,7
The syndrome remains difficult to diagnose due to its low incidence and absence of pathognomonic symptoms. Thus, symptoms mimic other common diseases. Botros et al8 have described this dilemma in an excellent manner.
The present study is a review of the publications in the past 5 years concerning LS. A PubMed search was carried out using the MeSH terms “Lemierre Syndrome/classification”, “Lemierre Syndrome/diagnosis”, “Lemierre Syndrome/etiology”, and “Lemierre Syndrome/therapy”. Inclusion criteria were: studies published in English language, dealt with human subjects, and apublication date within the last 5 years. The search elicited 121 papers, of which the abstracts were read, and 18 papers were excluded as they did not concern LS. The full text of 103 papers was read, after which seven were excluded, since they did not include any data on patients/cases. A total of 137 cases were included for this review (Figure 1).
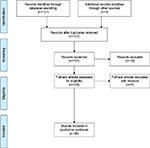  | Figure 1 Lemierre’s syndrome review: study inclusion and exclusion flow diagram. Notes: Figure created using PRISMA 2009 flow diagram software from Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097 doi: 10.1371/journal.pmed.1000097. For more information, visit www.prisma-statement.org.94 |
Diagnosis
A definite diagnosis of LS should be made based on the following findings:7,9
- a recent pharyngeal illness,
- complicated by septic emboli,
- as well as either thrombosis of the internal jugular vein or findings of F. necrophorum in blood cultures.
Clinical
This review yielded at total number of 137 cases2,3,5,6,8,10–90 including both case reports and minor reviews. The major clinical characteristics of LS are reported in Table 1. Twenty-four percent of the cases were presented with a complaint in the pharyngeal area (tonsillitis, pharyngitis, common sore throat), whereas a few came with an initial complaint of a swelling of the neck,37,61,64–66,73,82 due to either the thrombus itself or an abscess located in the neck region. Only eleven cases were described with initial difficulties in the dental region,6,16,18,42,46 the otogenic region,18,19,68,77 or the central nervous system.29,45 Atypical presentations included seizures90 and blindness.60,63 Half the cases were presented with sepsis at their first evaluation in the hospital, and at least 17 cases were intubated (not reported in all articles), underlining the severity of LS. Interestingly, the location of the primary infection is an important prognostic factor: infection in the oropharyngeal location (compared to other sites) was associated with a higher risk of longer intensive care unit stays due to complications such as respiratory problems.18 At least 37 of the cases in this review were not in the age group usually associated with LS, rather they were older than 30 years or younger than 15 years. Eleven were children younger than 15 years, who presented with a variety of symptoms, including pharyngitis59 and/or pneumonia43 and also more severe symptoms such as meningitis45 or febrile seizures.58 None of the children in this review died. In the older age group too, common complaints such as pneumonia40 dominated, but also here more severe symptoms/illnesses were seen, such as multiple emboli.38 It had previously been found that other diseases underlie LS in these older patients, such as diabetes or cancer.91
  | Table 1 Common clinical characteristics of Lemierre’s syndrome Abbreviation: CNS, central nervous system. |
The overall mortality was 2%, death was reported only in two of 137 cases. This is considerably less than previously reported.91 Briefly, no fusobacteria were cultured in the following two cases: 1) a diabetic patient with tonsillitis and peritonsillar abscess (K. pneumoniae positive culture)3 and 2) a 79-year old with tonsillitis and multiple septic emboli in lungs, liver, heart, kidney, and joints (Streptococcus anginosus positive culture).38 In a previous study, we presented morbidity and mortality in patients with positive cultures in blood, sputum, or pleural effusion with fusobacteria versus Staphylococcus aureus and showed that infections with fusobacteria were associated with a significantly lower 1-year mortality.92 Only one patient in the fusobacteria group in that study had LS,49 but generally mortality in the fusobacteria group was due to comorbidity and not due to severity of the infection itself. It could be speculated that publication bias plays an important role when trying to estimate the mortality in this rare syndrome. It could go both ways: fatal cases with a lesser likelihood to be published due to the simple fact that these cases could be missed and not diagnosed at all; or fatal cases could have a higher likelihood to be published due to the interest in why these cases become fatal.
Microbiological
In this review, 96 cases reported a causative microbiological agent; the majority of the cases were infections with F. necrophorum (41), Fusobacterium nucleatum (6), and unspecified fusobacteria (3), others were infections with microbiological agents such as Streptococcus (17), including methicillin-resistant S. aureus, and S. aureus (six cases) (Figure 2). These findings suggest that F. necrophorum is still the major microbiological agent in LS, but it could also be due to reporting bias, as clinicians and/or editors only approve “the forgotten disease” when fusobacteria is present in relevant cultures. Fusobacterium necrophorum (and other fusobacteria) is an obligate anaerobic bacterium and is notoriously difficult to culture, requiring a longer incubation period than other bacteria.92 A large proportion of the cases did not report a microbiological agent (n=40). As with other bacteria, cultures can be false negative if antibiotics are administered before sample collection. Whether the cases without a positive culture of F. necrophorum (or other fusobacteria) are true cases of LS is debatable. In the review by Riordan,9 it was suggested that F. necrophorum is in fact present in all patients with LS but goes undetected due to various circumstances and that the bacteria detected would be unable to cause LS on its own. However, this quite stern conclusion has not been accepted as a common rule in the clinical community, and so far a clinical diagnosis of LS is still valid if the bacteria either go undetected or turn out to be Streptococcus or some other known pathogenic bacteria.
  | Figure 2 Distribution of bacterial agent. Abbreviation: MRSA, methicillin-resistant Staphylococcus aureus. |
Imaging
Concerning the diagnosis of the infectious thrombosis, the optimal imaging tool is still debated. Ultrasonography is a radiation-free and easily available bedside tool, but it has the disadvantage of being less sensitive for recently formed thrombosis material, with a lesser echogenicity, as well as difficulties in the deeper tissue areas around the clavicle and mandible.93 Magnetic resonance imaging (MRI) is an excellent method for visualizing all anatomic structures as well as the thrombosis and/or septic emboli. However, MRI is expensive and usually not readily available. Computed tomography (CT) scans are cheaper and available in most hospitals, but it involves radiation exposure. In this review, the vast majority of cases (95%) with thrombophlebitis of the internal jugular vein were diagnosed by CT scans. Ultrasonography was used by the remaining cases, but none used MRI.
In total, ten cases (7%) had no or unknown thrombus during their disease. The majority of cases (84%) had thrombosis of the internal jugular vein, while a few (9%) cases had thrombosis of other veins, such as the facial vein, sinus transversus, or vena ophthalmicus.47,60
A larger proportion of cases (71 cases) had septic emboli in the lungs, but septic emboli were also seen in other organs, such as the liver,12,38,87 spleen,81 joints,38,70 heart,38 and the central nervous system,29,31 even though in smaller numbers.
Management
Antibiotics
All but a few rare cases received antibiotic treatment during their hospital stay. Multiple different regimens of the antibiotic of choice were used. Resistance to penicillin was not found at an increased frequency. However, carbapenem and piperacillin/tazobactam were commonly used, either as monotherapy or in combination with metronidazole, and 98% of the cases (mortality n=2) were treated successfully. The mean duration of antibiotic treatment was 4 weeks, but it ranged from 10 days to 8 weeks. The reason for the choice of a particular duration was not explained in any of the included papers. Riordan9 highlights the features of metronidazole and also recommends it as monotherapy, which was not seen in any of the cases in this review. He especially praises metronidazole for its profound activity against all strains of Fusobacterium spp., its good penetration within the tissue, and its good oral availability. Regarding treatment duration, Riordan9 and others have, similar to this review, found a wide range of treatment duration; however, it seems that there is no justified reason for prolonged intravenous treatment in cases of LS, and thus, if the patient responds well to treatment, he/she could be switched to oral treatment after the first 2 weeks of intravenous antibiotics.9
Anticoagulation
Anticoagulation is still a controversial issue, with no proper studies carried out on the issue. In this review, we found that 87 cases (64%) received anticoagulation treatment, often with low-molecular-weight heparin. Treatment duration varied between 2 weeks and 6 months. A few (n=2) patients suffered from side effects (hemorrhage or disseminated intravascular coagulation) and were treated accordingly without serious adverse effects.32,87 In the review by Riordan and also previous reviews, the frequency of patients treated with anticoagulants was 21%–23%. The high prevalence in this study might be due to the widespread, unconfirmed hypothesis regarding the positive effects of anticoagulants, which seem to have gained a favorable position in the clinic. Also, within this review, we have not subdivided the patients receiving anticoagulation treatment regarding thrombosis solely in the jugular vein and thrombosis involving sinus cavernosus. The latter is a more severe situation and thus requires a more aggressive treatment strategy.
Other forms of treatment
A substantial number of cases (n=17) had abscesses in various anatomical locations: lungs, liver, epidura, and neck. Generally, accessible abscesses were treated by drainage. Rarely, other surgical procedures were performed: tooth extraction,84 craniotomy,69 and ligation of the occluded vein,18,65,68 in order to prevent further septic emboli. Common for these cases were severe illness, and all other treatment modalities were already initiated, ligation seems to be reserved exclusively for extremely ill patients.
Conclusion
Given that we identified only 30 case reports from 2012, 27 from 2014, and ten from 2015, it does not seem that the incidence of LS is increasing. However, these are speculations, and evidently publication bias is unavoidable, and the “market” might be saturated with case reports on the subject. The syndrome still deserves the name “the forgotten disease”, and most fusobacterial infections are not LS. A fatal outcome is rare.
Diagnosing LS still requires thorough clinical examination and awareness of the association between current acute medical illness and a recent pharyngeal infection; yet, there is a need for studies on the diagnostic outcomes when LS is suspected.
Furthermore, early collection of blood samples and microbiology cultures in severely ill patients are required to establish a microbiological diagnosis. Symptoms of possible thrombosis need evaluation by an early CT scan or ultrasonography. The former has a better diagnostic capability, including intrathoracic vessels and septic emboli.
Treatment is efficacious and follows the general principles: systemic antibiotics, drainage of abscesses, and, perhaps, anticoagulation. Antibiotic treatment is crucial and should be corrected according to microbiological results on drug resistance. Penicillin, carbapenem, or piperacillin/tazobactam – often in combination with metronidazole – is efficacious. The optimal duration of treatment is not established, but 2 weeks of intravenous antibiotics with a total of 4–6 weeks seems sufficient. However, duration needs individualization according to disease severity and follow-up results, including imaging and serological inflammatory markers.
Based on the current evidence, it is still unknown whether anticoagulation therapy is mandatory. There were no apparent differences in mortality or course between the 64% cases treated with anticoagulants versus the 36% who were not. However, confounding by indication is most likely. Unfortunately, no randomized studies on this controversy are available.
Overall, LS is characterized by the absence of large-scale studies, but hopefully the future will witness a pragmatic multicenter approach to address the various controversies of this intriguing disease.
Disclosure
The authors report no conflicts of interest in this work.
References
Lemierre A. On certain septicemias due to anaerobic organisms. Lancet. 1936;1:701–703. | ||
Noh HJ, Freitas CA, Souza Rde P, et al. Lemierre syndrome: a rare complication of pharyngotonsillitis. Braz J Otorhinolaryngol. 2015;81(5):568–570. | ||
Chuncharunee A, Khawcharoenporn T. Lemierre’s syndrome caused by Klebsiella pneumoniae in a diabetic patient: a case report and review of the literature. Hawaii J Med Public Health. 2015;74(8):260–266. | ||
Riordan T, Wilson M. Lemierre’s syndrome: more than a historical curiosa. Postgrad Med J. 2004;80(944):328–334. | ||
Tromop-van Dalen C, Mekhail AM. Lemierre syndrome: early recognition and management. CMAJ. 2015;187(16):1229–1231. | ||
Oya M, Tanimoto T, Yamamoto T, Hakozaki Y. Lemierre’s syndrome associated with periodontal injury-derived odontogenic infection that did not respond to meropenem. Intern Med. 2015;54(14):1803–1808. | ||
Karkos PD, Asrani S, Karkos CD, et al. Lemierre’s syndrome: a systematic review. Laryngoscope. 2009;119(8):1552–1559. | ||
Botros J, Rencic J, Centor RM, et al. Anchors away. J Gen Intern Med. 2014;29(10):1414–1418. | ||
Riordan T. Human infection with Fusobacterium necrophorum (Necrobacillosis), with a focus on Lemierre’s syndrome. Clin Microbiol Rev. 2007;20(4):622–659. | ||
Turedi S, Turkmen S, Yadigaroglu M. An unusual cause of sore throat and neck swelling. Emerg Med J. 2015;32(8):625, 46. | ||
Wong AP, Duggins ML, Neil T. Internal jugular vein septic thrombophlebitis (lemierre syndrome) as a complication of pharyngitis. J Am Board Fam Med. 2015;28(3):425–430. | ||
Takano Y, Fukuda K, Takayasu H, et al. Liver abscessation and multiple septic pulmonary emboli associated with Lemierre’s syndrome: a case report. BMC Res Notes. 2015;8:65. | ||
Crowley ND, Verceles AC, Reed RM. Sore throat. don’t forget Lemierre’s syndrome. BMJ Case Rep. 2015;2015:bcr2014208225. | ||
Aslanidis T, Myrou A, Giannakou-Peftoulidou M. Management of a young female patient with Fournier’s gangrene and Lemierre’s syndrome. Pan Afr Med J. 2014;18:275. | ||
Agrafiotis M, Moulara E, Chloros D, et al. Lemierre syndrome and the role of modern antibiotics and therapeutic anticoagulation in its treatment. Am J Emerg Med. 2015;33(5):733.e3–733.e4. | ||
Shimada M, Morinaga Y, Kitazaki T, et al. A severe case of Lemierre Syndrome with Streptococcus constellatus infection. Jpn J Infect Dis. 2014;67(6):488–489. | ||
Olson KR. Case 36-2014: a woman with fever, pharyngitis, and double vision. N Engl J Med. 2015;372(6):581–582. | ||
Schubert AD, Hotz MA, Caversaccio MD, Arnold A. Septic thrombosis of the internal jugular vein: lemierre’s syndrome revisited. Laryngoscope. 2015;125(4):863–868. | ||
Davidoss N, Ha JF, Anderson JR, Rodrigues S. Lemierre’s syndrome – an unusual complication of otitis externa in a young, healthy female. J Laryngol Otol. 2015;129(suppl 1):S60–S62. | ||
Ledochowski S, Freichet M, Wallet F, et al. Lemierre’s syndrome: when a contralateral thrombosis stirs the debate. Intensive Care Med. 2015;41(2):329–330. | ||
Kempen DH, van Dijk M, Hoepelman AI, Oner FC, Verlaan JJ. Extensive thoracolumbosacral vertebral osteomyelitis after Lemierre syndrome. Eur Spine J. 2015;24(suppl 4):S502–S507. | ||
Takenouchi S, Kunieda T, Yamada R, et al. Lemierre syndrome caused by oral sex. J Formos Med Assoc. 2014;113(10):762–763. | ||
Asnani J, Jones S. Case review. Lemierre’s syndrome. J Fam Pract. 2014;63(4):193–196. | ||
Cardenas-Garcia J, Narasimhan M, Koenig SJ. A teenager with fever and sore throat. Diagnosis: lemierre syndrome. Chest. 2014;145(4):e10–e13. | ||
Murthy KA, Thippeswamy T, Kiran HS, et al. The ‘forgotten disease’ (or the never known). J Assoc Physicians India. 2013;61(10):754–757. | ||
Shook J, Trigger C. Lemierre’s Syndrome. West J Emerg Med. 2014;15(2):125–126. | ||
Behpour-Oskooee M, Karimi A, Sayyahfar S. Lemierre’s syndrome with double heterozygote status in the methylenetetrahydrofolate reductase gene. World J Pediatr. 2014;10(3):281–283. | ||
Gupta N, Kralovic SM, McGraw D. Lemierre syndrome: not so forgotten! American journal of critical care: an official publication. Am J Crit Care. 2014;23(2):176–179. | ||
Lin HY, Liao KH, Jean SS, et al. Lemierre syndrome with cervical spondylodiscitis and epidural abscess associated with direct injection of heroin into the jugular vein. J Microbiol Immunol Infect. 2015;48(2):238–239. | ||
Azzopardi C, Grech R, Mizzi A. Lemierre syndrome: more than just a sore throat. BMJ Case Rep. 2013;2013:bcr2013201868. | ||
Ratnasingham Y, Kristensen LH, Gammelgaard L, Balslev T. Arterial ischemic stroke as a complication to disseminated infection with Fusobacterium necrophorum. Neuropediatrics. 2014;45(2):120–122. | ||
Horwitz M, Chaumoitre K, Grimaldi C, et al. Spontaneous regression of multiple Rasmussen aneurysms in a child with Lemierre syndrome and pulmonary abscesses. Pediatr Infect Dis J. 2013;32(11):1301–1302. | ||
Hawes D, Linney MJ, Wilkinson R, Paul SP. Lemierre’s syndrome: the importance of early detection. Br J Nurs. 2013;22(18):1075–1078. | ||
Morelli N, Rota E, Sacchini D, et al. Lemierre syndrome: more than “the forgotten disease”. Neurology. 2013;81(13):1179–1180. | ||
Golan E, Wong K, Alahmadi H, et al. Endoscopic sphenoid sinus drainage in Lemierre syndrome. J Clin Neurosci. 2014;21(2):346–348. | ||
Blessing K, Toepfner N, Kinzer S, et al. Lemierre syndrome associated with 12th cranial nerve palsy – a case report and review. Int J Pediatr Otorhinolaryngol. 2013;77(9):1585–1588. | ||
Abhishek A, Sandeep S, Tarun P. Lemierre syndrome from a neck abscess due to methicillin-resistant Staphylococcus aureus. Braz J Infect Dis. 2013;17(4):507–509. | ||
Righini CA, Karkas A, Tourniaire R, et al. Lemierre syndrome: study of 11 cases and literature review. Head Neck. 2014;36(7):1044–1051. | ||
Takeda K, Kenzaka T, Morita Y, Kuroki S, Kajii E. A rare case of Lemierre`s syndrome caused by Porphyromonas asaccharolytica. Infection. 2013;41(4):889–892. | ||
Kim BY, Yoon DY, Kim HC, et al. Thrombophlebitis of the internal jugular vein (Lemierre syndrome): clinical and CT findings. Acta Radiol. 2013;54(6):622–627. | ||
Litmathe J, Zardo P, Dickgreber N, May G, Sucker C, Fischer S. Severe ARDS induced by fusobacterial infections: a rare clinical presentation of Lemierre syndrome. Thorac Cardiovasc Surg. 2013;61(8):754–757. | ||
Boyd D, Paterson P, Dunphy L, Carton A, Hammersley N. A case report of Lemierre’s Syndrome associated with dental sepsis. Scott Med J. 2013;58(1):e24–e27. | ||
Mação P, Cancelinha C, Lopes P, Rodrigues F. An 11-year-old boy with pharyngitis and cough: lemierre syndrome. BMJ Case Rep. 2013;2013:bcr2012008527. | ||
Wahab D, Bichard J, Shah A, Mann B. Just a sore throat? Uncommon causes of significant respiratory disease. BMJ Case Rep. 2013;2013:bcr2013008739. | ||
DeGaffe GH, Murphy JR, Butler IJ, Shelburne J, Heresi GP. Severe narrowing of left cavernous carotid artery associated with Fusobacterium necrophorum infection. Anaerobe. 2013;22:118–120. | ||
Ghaly B, Bertram A, Naim A. Lemierre’s syndrome: a serious complication of a routine dental procedure. Aust Dent J. 2013;58(2):246–249. | ||
Gutzeit A, Roos JE, Portocarrero-Fah B, et al. Differential diagnosis of Lemierre’s syndrome in a patient with acute paresis of the abducens and oculomotor nerves. Korean J Ophthalmol. 2013;27(3):219–223. | ||
McGouran D, Keene A, Walklin R, et al. A complex case of bilateral Lemierre syndrome with suggestions on anticoagulation management. Intern Med J. 2013;43(6):728–730. | ||
Johannesen K, Bodtger U, Heltberg O. Lemierre’s syndrome: the forgotten disease. J Thromb Thrombolysis. 2014;37(3):246–248. | ||
Paul SP, Beri R, Linney MJ. Lemierre’s syndrome: a sinister sore throat every clinician should remember. Turk J Pediatr. 2012;54(5):528–531. | ||
Soh T, Lim MH. Lemierre’s syndrome: an unusual cause of calf abscess. Ann Acad Med Singapore. 2013;42(1):52–54. | ||
Valesky W, Agoritsas K. Lemierre syndrome complicated by cerebral abscess. Am J Emerg Med. 2013;31(2):458.e1–458.e3. | ||
Dholakia S, Hashimi Y. Doctor, I have a sore throat. BMJ Case Rep. 2013;2013:bcr2012007736. | ||
Kumar M, Singh R, Sawlani KK, Kumar S. Atypical presentation of Lemierre syndrome: role of imaging. BMJ Case Rep. 2013;2013:bcr2012007647. | ||
Ji YQ, Wang J, Kong LQ, et al. Lemierre syndrome caused by Arcanobacterium haemolyticum. Chin Med J. 2013;126(2):391–392. | ||
Murata Y, Wada M, Kawashima A, Kagawa K. Early diagnosis of Lemierre’s syndrome based on a medical history and physical findings. Intern Med. 2013;52(2):285–288. | ||
Rodgaard JC, Niedvaraite R, Andersen GN. Lemierre’s syndrome in systemic lupus erythematosus: a report of two cases. Scand J Rheumatol. 2013;42(2):167–168. | ||
Khan A, Ganesan S, Arora M, Hussain N. Life threatening complication of sore throat: lemierre’s syndrome. Indian J Pediatr. 2013;80(12):1059–1061. | ||
Davies O, Than M. Lemierre’s syndrome: diagnosis in the emergency department. Emerg Med Australas. 2012;24(6):673–676. | ||
Akiyama K, Karaki M, Samukawa Y, Mori N. Blindness caused by septic superior ophthalmic vein thrombosis in a Lemierre Syndrome variant. Auris Nasus Larynx. 2013;40(5):493–496. | ||
Lim AL, Pua KC. Lemierre syndrome. Med J Malaysia. 2012;67(3):340–341. | ||
Iizuka T, Nagaya K, Sasaki D, et al. Atypical Lemierre syndrome, thrombophlebitis of the facial vein. Am J Emerg Med. 2013;31(2):460.e1–460.e3. | ||
Stauffer C, Josiah AF, Fortes M, Menaker J, Cole JW. Lemierre syndrome secondary to community-acquired methicillin-resistant Staphylococcus aureus infection associated with cavernous sinus thromboses. J Emerg Med. 2013;44(2):e177–e182. | ||
Phan T, So TY. Use of anticoagulation therapy for jugular vein thrombus in pediatric patients with Lemierre’s syndrome. Int J Clin Pharm. 2012;34(6):818–821. | ||
Murray M, Stevens T, Herford A, et al. Lemierre syndrome: two cases requiring surgical intervention. J Oral Maxillofac Surg. 2013;71(2):310–315. | ||
Tsai YJ, Lin YC, Harnnd DJ, Chiang RP, Wu HM. A Lemierre syndrome variant caused by Klebsiella pneumoniae. J Formos Med Assoc. 2012;111(7):403–405. | ||
Root RW, Barrett TW, Abramo TJ. A 10-month-old with Lemierre syndrome complicated by purulent pericarditis. Am J Emerg Med. 2013;31(1):274.e5–274.e7. | ||
Hile LM, Gibbons MD, Hile DC. Lemierre syndrome complicating otitis externa: case report and literature review. J Emerg Med. 2012;42(4):e77–e80. | ||
Teng HW, Chen CY, Chen HC, Chung WT, Lee WS. Fusobacterium septicemia complicated by cerebral subdural and epidural empyemas: a rare case of Lemierre syndrome. J Emerg Med. 2012;43(4):671–673. | ||
Chow BJ, Tupesis JP. Disseminated Lemierre syndrome presenting as septic arthritis. J Emerg Med. 2012;42(5):573–575. | ||
Kisser U, Gurkov R, Flatz W, Berghaus A, Reichel O. Lemierre syndrome: a case report. Am J Otolaryngol. 2012;33(1):159–162. | ||
Wingfield T, Blanchard TJ, Ajdukiewicz KM. Severe pneumonia and jaundice in a young man: an atypical presentation of an uncommon disease. J Med Microbiol. 2011;60(pt 9):1391–1394. | ||
Singhi S, Mathew J, Jindal A, Verma S. Clinical Pearls in pediatric infections. Indian J Pediatr. 2011;78(12):1536–1542. | ||
Ikemoto T, Kawasaki M, Kato T, et al. Dangerous cervical radiculopathy by Lemierre’s syndrome. J Orthop Sci. 2012;17(5):663–666. | ||
Dorfman A, Shokoohi H, Taheri MR. Lemierre’s syndrome and rapidly deteriorating respiratory failure in the emergency department. Am J Emerg Med. 2012;30(8):1658.e5–1658.e7. | ||
Price K, Wilson L, Tsegaye M. A case of craniocervical abscess with sinus thrombosis in Lemierre’s syndrome. Br J Neurosurg. 2012;26(3):426–428. | ||
Bababeygy SR, Almarzouki H, Buffenn AN. Isolated abducens nerve palsy secondary to Lemierre syndrome. J AAPOS. 2011;15(6):587–589. | ||
Lee WS, Wang FD, Shieh YH, et al. Lemierre syndrome complicating multiple brain abscesses caused by extended-spectrum beta-lactamase-producing Klebsiella pneumoniae cured by fosfomycin and meropenem combination therapy. J Microbiol Immunol Infect. 2012;45(1):72–74. | ||
Nisar MK, Kuttikat AV, Ramabhadran B, et al. Lemierre’s syndrome: a rare cause of septic polyarthritis. Rheumatol Int. 2013;33(3):817–818. | ||
Rehman HU. A woman with headache and ptosis. QJM. 2014;107(9):759–761. | ||
Kieran I, Lyttle M, Leroi M. Successful antibiotic stewardship: are we a victim of our own success? ANZ J Surg. 2011;81(6):488–489. | ||
Wasilewska E, Morris AD, Lee EY. Case of the season: lemierre syndrome. Semin Roentgenol. 2012;47(2):103–105. | ||
Klein NC, Petelin A, Cunha BA. Mycoplasma pneumoniae preceding Lemierre’s syndrome due to Fusobacterium nucleatum complicated by acute Epstein-Barr virus (EBV) infectious mononucleosis in an immunocompetent host. Heart Lung. 2013;42(1):74–76. | ||
Wu AY, Tseng HK, Su J, Liu CP. Lemierre’s syndrome in a patient with habitual toothpick usage. J Microbiol Immunol Infect. 2013;46(3):237–240. | ||
Chattopadhyay D, Mostafa ML, Carr M. Acute neck pain referred to the surgeon: lemierre’s syndrome as a differential diagnosis. Ann R Coll Surg Engl. 2012;94(3):e132–e133. | ||
Kroll D, Sendi P. Lemierre’s syndrome in the liver. Infection. 2012;40(4):477–478. | ||
Iwasaki T, Yamamoto T, Inoue K, Takaku K. A case of Lemierre’s syndrome in association with liver abscess without any other metastatic lesions. Intern Med. 2012;51(11):1419–1423. | ||
Molloy A, Towersey G, Shackleton D, et al. The changing face of an old disease: case report of nonclassical Lemierre’s syndrome caused by a Panton-Valentine leucocidin-positive methicillin-susceptible Staphylococcus aureus isolate. J Clin Microbiol. 2012;50(9):3144–3145. | ||
Pitsiou G, Kachrimanidou M, Papa A, et al. Lemierre’s syndrome presenting to the ED: rapidly fatal sepsis caused by methicillin-susceptible Staphylococcus aureus Staphylococcus protein A type t044. Am J Emerg Med. 2013;31(1):268.e5–268.e7. | ||
Krishna K, Diwan AG, Gupt A. Lemierre’s syndrome – the syndrome quite forgotten. J Assoc Physicians India. 2012;60:60–63. | ||
Hagelskjaer Kristensen L, Prag J. Lemierre’s syndrome and other disseminated Fusobacterium necrophorum infections in Denmark: a prospective epidemiological and clinical survey. Eur J Clin Microbiol Infect Dis. 2008;27(9):779–789. | ||
Johannesen K, Dessau R, Heltberg O, Bodtger U. Bad news itself or just the messenger? The high mortality of Fusobacterium spp. infections is related to disseminated malignancy and other comorbidities. Eur Clin Respir J. 2016;3:30287. | ||
Ungprasert P, Srivali N. Diagnosis and treatment of Lemierre syndrome. Am J Emerg Med. 2015;33(9):1319. | ||
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. Available from: www.prisma-statement.org. Accessed May 9, 2016. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
