Back to Journals » Patient Preference and Adherence » Volume 13
Lay People’s Ethical Attitudes To Placebo Treatment: A Q-Methodology Study
Authors Hammami MM , Hammami S, Aboushaar R, Aljomah AS
Received 21 May 2019
Accepted for publication 6 September 2019
Published 27 September 2019 Volume 2019:13 Pages 1599—1617
DOI https://doi.org/10.2147/PPA.S216565
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Video abstract presented by Hammami et al.
Views: 172
Muhammad M Hammami,1,2 Safa Hammami,3 Reem Aboushaar,4 Ahmed S Aljomah1
1Clinical Studies and Empirical Ethics Department, King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia; 2Alfaisal University College of Medicine, Riyadh, Saudi Arabia; 3St. Mary Medical Center, San Francisco, CA, USA; 4MS IV, Florida Atlantic University, Boca Raton, FL, USA
Correspondence: Muhammad M Hammami
Clinical Studies and Empirical Ethics Department, King Faisal Specialist Hospital and Research Centre, P O Box # 3354 (MBC 03), Riyadh 11211, Saudi Arabia
Tel +966-1-442-4527
Fax +966-1-442-7894
Email [email protected]
Background: Placebo-treatment acceptability is debated among ethicists, mostly due to conflict between respect-to-autonomy and beneficence principles. It is not clear how lay people balance these and other ethical principles.
Methods: One hundred and eighty-seven respondents rank-ordered 42 opinion statements covering various ethical aspects of placebo-treatment, according to a 9-category symmetrical distribution. We analyzed statements’ scores using averaging-analysis and by-person factor analysis (Q-methodology).
Results: Respondents’ mean (SD) age was 34.6 (10.6) years, 54% were women, 40% healthcare-related, 68% Muslims (31% Christians), and 39% received general education in Saudi Arabia (24% in the Philippines). On averaging-analysis, the most-agreeable statements were “Acceptable if benefit to patient large” and “Acceptable with physician intent to benefit patient”. The most-disagreeable statements were “Acceptable with physician self-benefit intent” and “Acceptable with large harm to other patients”. Muslims gave a higher rank to “Giving no description is acceptable”, “Acceptable with small benefit to patient”, and “Acceptable with physician intent to benefit patient” and a lower rank to “Acceptable to describe as inactive drug”, “Acceptable with physician intent to please patient caring relative”, and “Acceptable with moderate harm to other patients” (p<0.01). Q-methodology detected several ethical attitude models that were mostly multi-principled and consequentialism-dominated. The majority of Christian and Philippines-educated women loaded on a “relatively family and deception-concerned” model, whereas the majority of Muslim and Saudi Arabia-educated women loaded on a “relatively common-good-concerned” model. The majority of Christian and healthcare men loaded on a “relatively deception-concerned” model, whereas the majority of Muslim and non-healthcare men loaded on a “relatively motives-concerned” model. Of nine intent-related statements, ≥2 received extreme rank on averaging-analysis and in 100% of women and men models.
Conclusion: 1) On averaging-analysis, patient’s beneficence (consequentialism) followed by physician’s intent (virtue ethics) were more important than deception (respect-to-autonomy). 2) Q-methodology identified several ethical attitude models that were mostly multi-principled and associated with respondents’ demographics.
Keywords: lay people attitude, placebo treatment, virtue, common good, principlism, Q-methodology
Background
Placebo treatment appears to be commonplace.1–8 A 2009 systematic review of placebo use in 12 countries found that 17% to 80% of general medicine practitioners used pure placebos (interventions with no pharmacologically active ingredients) and 54% to 57% impure placebos (interventions pharmacologically inert for the condition they are prescribed for but not otherwise) at least once in their career.7 Further, a deception checklist to help doctors decide when deception is morally acceptable has been published,9 a placebome to examine genetic correlates of placebo response has been proposed,10 and placebo smartphone apps have been developed (several are available at Google Play).
Placebo treatment is used for various reasons, including complying with patient/family expectations, satisfying their demands, and avoiding confrontation;11 exercising kindness and compassion, avoiding risk of addiction, managing clinical uncertainty, benefiting the carer, and feeling able to do something;12 and taking advantage of the placebo effect in reducing suffering. The placebo effect,13 not to be confused with non-specific passive changes and statistical artefacts, such as natural course of the condition and regression to the mean, respectively,14,15 is associated with both pharmacologically active and placebo interventions. It works by manipulating expectations, consciously, through personal experience, observational learning, obtaining information, and/or unconsciously through classical conditioning. It may alter patient perceptions of symptoms and/or the physiological systems modulated by pharmacologically active agents.16 Interestingly, the placebo effect has been shown to interact with the effect of pharmacologically active agents.17–19 In fact, due to demonstrated effectiveness, the conceptual soundness of the term “placebo” has been challenged.20
Placebo treatment usually involves some degree of deception and thus conflicts with the ethical principle of respect to person (right to autonomy, right to be treated with dignity, the “right to know”). In addition, placebo treatment may erode patients’ trust in their physicians11,21 and the medical profession as a whole, is not compatible with the shared decision-making model of clinical practice,22 may increase the probability of deceiving again and/or in other situations, may have a nocebo effect (the effect of negative expectations), which has similar effect size to the placebo effect,23 may encourage over medicalization of minor illnesses, and has monetary cost.8,12 Further, the adverse effects of placebo treatment may extend to other patients (such as when antibiotics use for viral infections spreads antibiotics resistance) and to community at large (cost of placebo treatment, cost of trust loss).
Deception is not a single construct. It can be divided into outright lying and non-lying deception and it may or may not be followed by full disclosure. In non-lying deception, A causes B to be misled, not necessarily through communicating with B or through using a believed-false statement; whereas in outright lying, A informs B a believed-false statement.24 However, both are scalar phenomena, allowing for a number of intermediate states.25
Ethicists have debated whether outright lying and non-lying deception can be justified in placebo treatment and whether there is a moral difference between the two acts.24,26–29 Does patients’ trust in physicians mean to provide all relevant information or to do the best for their health? Are physicians bound by the same constraints as everyone else, or is deception morally justified by the therapeutic privilege?30 Is disclosing that placebos are pharmacologically inert incidental information (akin to disclosing the biochemical ingredients of pharmacologically active drugs) that does not increase informedness and, thus, shouldn’t influence patients’ decisions?20,31
Although not mentioned in the Hippocratic Oath, fundamental to most medical associations’ ethics is that a physician should not deceive their patients.9 There are few studies that explored patients and lay people attitudes to placebo treatment.21,32–34 Placebo treatment was acceptable, especially with deception rather than outright lying and when there is a serious or persistent condition,21,32 with the intent to benefit the patient and when there is no alternative treatment,34 and with benefit certainty and transparency.33 Further, contrary to theoretical analysis, patients appear to accept a paternalistic approach more than physicians,21,35 who also believe that it is ethically permissible to prescribe placebos.6,8 These studies have not explored the thinking process underlying the ethical acceptance or unacceptance of placebo treatment. Further, they used independent rating of options followed by averaging-analysis, which may obscure individual differences. Q-methodology has the advantage of unmasking thinking patterns by statistically grouping like-minded people based on their sorting of a selection of opinion statements.36–39 It involves construction of an appropriate concourse of opinion statements, selection of statements to form a Q-set, respondents’ sorting of the Q-set along a continuum, by-person factor analysis, and factors’ interpretation”.
The main aim of this study was to explore lay people ethical attitudes toward the acceptability of treating conditions that have no or inadequate therapy, by physician-prescribed placebos. Specifically, using averaging-analysis and Q-methodology, we explored how lay people balance the ethical principles of respect for autonomy, beneficence, non-maleficence, and justice40–42 and how other ethical approaches, such as familism,43 communitarianism,44 and virtue45 shape their attitude.
Methods
This exploratory cross-sectional study is part of a series of studies designed to model lay people’s ethical decision-making on controversial medical issues. It was conducted in accordance with the ethical principles contained in the Declaration of Helsinki after approval of the Research Ethics Committee (REC) of the King Faisal Specialist Hospital and Research Center (KFSH&RC); all respondents provided written informed consent.
Instrument Development And Validation
The study instrument was developed by the authors and was subjected to two cycles of pilot testing, validation, and revision. First, a Q-concourse was constructed based on reviewing the literature and logically structured into the following major ethical domains: consequentialism (including ethics of care/familism and common good), justice, rights, and virtue. Second, a representative set of statements (Q-set) was chosen with the aim of maximizing comprehensiveness and balance and minimizing redundancy. Third, pilot testing identified statements that were uninformative (having especially small variance), unclear, or leading. It also evaluated the Q-set, through focused probing in an interview session following Q-sorting, asking sorters to assume certain extreme points of view before sorting, studying correlation of statements scores among individuals who assumed the same extreme point of view, and test–re-test assessment (with intervening Q-sorting while assuming extreme points of view and with random re-numbering of statements). Intra-person correlation of statements’ scores was consistently more than 0.77.
The final Q-set is presented in Supplementary File 1, Q-set statements. It is composed of 42 opinion statements divided into four major parts: 1) Consequentialism: a) to patient (four statements covering harm and graded benefit), b) to family (three statements covering graded benefit), and c) to other patients/common good (six statements covering graded benefit and harm to other patients). 2) Justice: a) distributive (one statement, which can also be classified under consequences to other patients), and b) cost bearing (six statements). 3) Rights: a) informed consent/deception (seven statements covering various degrees of deception), and b) vulnerability (six statements covering various vulnerable groups). 4) Virtue: a) motives (nine statements covering various physicians’ motives). The statements were assigned random numbers and presented to respondents on separate cards along with a set of instructions and sorting sheet (Supplementary File 2, Instructions and sorting sheet). The sorting sheet had nine categories (from 1 = strongly disagree to 9 = strongly disagree) with a symmetrically distributed number of slots: categories 1 and 9, three slots each, categories 2 and 8, four slots each, categories 3 and 7, five slots each, and categories 4, 5, and 6, six slots each.
Instrument Administration
The instrument was self-administered. Respondents’ instructions included the following information: For the purpose of this study, we define placebos as interventions that do not have ingredients known to be pharmacologically active for the condition being treated. These include pure and the so-called impure placebos. Pure placebos are interventions, such as sugar pills, that have no pharmacologically active ingredients. Impure placebos are interventions, such as prescribing antibiotics for viral infections, that have pharmacologically active ingredients for certain conditions, but are prescribed for unrelated conditions. Placebo treatment has been shown in numerous studies to be active and produce a specific placebo effect. It works through modulating patient’s expectations, consciously and subconsciously. Patients experience a placebo effect because they expect that they will benefit from the treatment. We exclude from the placebo effect changes in patient status that would occur regardless of any intervention (such as the spontaneous cure of influenza) as well as changes due to other aspects of the doctor–patient relationship. We stipulate that the effect of placebo would be strongest if the patient believed it is pharmacologically active. We further stipulate that placebos are prescribed by the physician for conditions that have no or inadequate therapy. Thus, we are interested in studying the ethical acceptance of placebo treatment in the absence of, or in addition to, standard therapy rather than instead of it. We are interested in the ethical acceptability of prescribing placebos rather than what the physician should do (the morally best course of action) or what you prefer for yourself or your family/friend.
Respondents were instructed to rank the Q-set statements and then comment on their extreme choices. Completeness of sorting (ie, each statement is sorted, and only once) was checked by study coordinators and respondents were asked to self-correct any identified mistakes in copying statements’ numbers onto the sorting sheet before leaving the study site. The following data were also collected: sex, age, degree of general education, place of general education, ethics education (formal, informal), nationality, major religious affiliation, occupation (healthcare, non-healthcare), and time spent in Q-sorting.
Sample Size And Sampling
Consistent with Q-methodology exploratory nature, sample size was based on convenience and practicality. Respondents were recruited by advertising throughout the KFSH&RC and other public places. Adults with at least high school education who were able to understand the purpose and procedures of the study were eligible.
Analysis
We used PCQ for Windows (PCQ Software, Portland, OR, USA) to conduct Q-methodology analysis. Analysis was performed separately for men’s and women’s Q-sorts, due in part to the 120 Q-sorts limit of the program. Extracted factors were subjected to graphical rotation. The program used definer Q-sorts (Q-sorts with significant (p<0.01) loading of ≥0.40 on a factor) to create a model Q-sort for each factor (represents how a hypothesized respondent with 100% loading on the factor would have ordered the 42 statements). We interpreted the factors (ethical attitude models) based on identifying the seven most agreeable and seven most disagreeable statements for each factor, respondents’ post-sorting comments, and comparison of statement scores across factors; taking into account the entire factor. On averaging-analysis, statements were considered “neutral” if their mean ranking score was ≥4 and ≤6. For Q-methodology, the statements were considered strongly agreed with if they were assigned a score of 9 or 8, and strongly disagreed with if they were assigned a score of 1 or 2. In order to explore the association between attitude models and respondents’ demographics and because of the relatively small number of definer Q-sorts, respondents who loaded significantly (or more significantly, if compounded) on one of the identified factors were considered as one group. The groups were compared using Analysis of Variance (ANOVA) and Fisher Exact test. Finally, independent t-test was used to compare individual statements’ mean ranking scores; p˂0.01 was considered significant. Two-tailed p-value and 95% confidence interval are reported. Statistical analysis was performed with IBM SPSS Statistics version 21 software.
Results
The mean (SD) age of the 187 respondents was 34.6 (10.6) years and the mean sorting time was 28.2 (10.2) minutes. Fifty-four percent were women. Almost all respondents were Muslims or Christians, and most had their general education in Saudi Arabia or the Philippines, to a large degree, reflecting the institution’s visitors/employees (Table 1).
 |
Table 1 Demographics of study respondents |
Averaging-Analysis
Respondents force-ranked 42 placebo treatment-related, opinion, statements (full length statements along with abbreviated statements are available in Supplementary File 1, Q-set Statements) on a 9-point scale (1=strongly disagree, 9=strongly agree) following a systematic distribution (Supplementary File 2, Instructions and Sorting Sheet).
Mean (SD) scores of the 42 statements are shown in Figure 1. Nine statements were assigned a mean ranking score of ˃6, with mean (SD) scores ranging from 7.9 (1.9) to 6.1 (2.1). The three most agreeable statements were, in descending order, “2. Acceptable if benefit to patient large”, “26. Acceptable with physician intent to benefit patient”, and “31. Acceptable if no harm to patient”. Seven statements were assigned a mean ranking score of <4, with mean (SD) scores ranging from 3.0 (2.1) to 3.9 (1.8). The two most disagreeable statements were, in ascending order, “15. Acceptable with physician self-benefit intent” and “36. Acceptable with large harm to other patients”. The data show the overall primacy of beneficence/non-maleficence and motives.
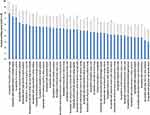 |
Figure 1 Forced-ranking scores of 42 placebo treatment-related opinion statements, arranged according to mean assigned ranks. Bars and error bars represent the mean and SD of ranking scores on a scale of 1 (strongly disagree) to 9 (strongly agree). For a full description of the statements, see Supplementary File 1, Q-set Statements. |
Figure 2 groups the 42 statements according to the most relevant underlying ethical principle. It shows that the perceived importance of the various moral interests is graded and somewhat overlapping.
 |
Figure 2 Forced-ranking scores of 42 placebo treatment-related opinion statements, arranged according to the most relevant underlying ethical approach. Bars and error bars represent the mean and SD of ranking scores on a scale of 1 (strongly disagree) to 9 (strongly agree). For a full description of the statements, see Supplementary File 1, Q-Set statements. |
Mean ranking scores of some statements were significantly associated with respondents’ demographics. Healthcare respondents assigned a higher rank to “40. Acceptable with moderate benefit to patient” (6.8 (1.7) vs 5.9 (1.9) in non-healthcare respondents, mean (95% confidence interval) difference=0.9 (0.4–1.4), p=0.001). Further, respondents who reported formal ethics education assigned a lower rank to “35. Giving no description is acceptable” (3.9 (2.4) vs 4.9 (2.4) by their counterparts, mean difference=−1.1 (−1.9 to −0.3), p=0.009).
Furthermore, compared to Christians, Muslims assigned a higher rank to “35. Giving no description is acceptable” (5.1 (2.5) vs 3.6 (2.2), mean difference=1.5 (0.8–2.3), p<0.001), “9. Acceptable with small benefit to patient” (5.6 (2.0) vs 4.7 (2.2), mean difference=1.0 (0.3–1.6), p=0.003), and “26. Acceptable with physician intent to benefit patient” (7.6 (1.8) vs 6.7 (2.2), mean difference=0.9 (0.3–1.5), p=0.005); and a lower rank to “19. Acceptable to describe as inactive drug” (5.0 (2.5) vs 6.0 (2.3), mean difference=−1.0 (−1.8 to −0.3), p=0.009), “39. Acceptable with physician intent to please patient caring relative” (3.9 (1.9) vs 4.9 (2.0), mean difference=−0.9 (−1.5 to −0.3), p=0.003), and “20. Acceptable with moderate harm to other patients ” (3.6 (1.8) vs 4.4 (1.8), mean difference=−0.9 (−1.4 to −0.3), p=0.004).
There was a significant association (p˂0.001) between place of general education (Saudi Arabia vs the Philippines) and religious affiliation (Muslims vs Christians). Therefore, the differences in ranking scores of statements 35, 9, 26, 19, 39, and 20 between respondents who had their general education in Saudi Arabia vs the Philippines were in the same direction as Muslims vs Christians, and most were also significant (statements 9, 26, 39, and 20). In addition, respondents who had general education in Saudi Arabia (vs the Philippines) assigned a higher rank to “16. Acceptable with large benefit to other patients” (6.6 (2.1) vs 5.3 (2.2), mean difference=1.3 (0.5–2.1), p=0.002) and a lower rank to “3. Acceptable if harm to other patients small” (4.2 (1.8) vs 5.2 (2.1), mean difference=−1.0 (−1.7 to −0.3), p=0.009). The differences in ranking these two statements between Muslims and Christians were in the same direction and of borderline significance (p=0.03 and p=0.02).
Q-Methodology Analysis
Using the 101 women Q-sorts and the 86 men Q-sorts, we extracted six factors (centroids) for women and six for men. Extracting a higher number did not importantly improve the percent variance explained and complicated factor interpretation. The extracted factors were subjected to graphical rotation in order to reduce confounding (loading significantly on more than one model) and negative loading.
Ethical Attitude Models In Women
The six-factor solution accounted for 47% of the total variance and 62 (61%) of the Q-sorts. Twenty Q-sorts did not have significant loading on any of the factors (models) and 19 were confounded. Correlation of the scores of the 42 statements between the six models ranged from 0.11 (models C and E) to 0.54 (models D and F). Model A had six defining Q-sorts, an eigenvalue of 4.9, and explained 5% of the variance. Model B had nine defining Q-sorts, an eigenvalue of 8.3, and explained 8% of the variance. Model C had seven defining Q-sorts, an eigenvalue of 5.5, and explained 5% of the variance. Model D had 22 defining Q-sorts, an eigenvalue of 15.5, and explained 15% of the variance. Model E had nine defining Q-sorts, an eigenvalue of 5.6, and explained 6% of the variance. Finally, model F had nine defining Q-sorts, an eigenvalue of 7.6, and explained 8% of the variance.
The six program-generated model Q-sorts (the program assigns an idealized score for each of the 42 statements to represent how a hypothesized respondent with 100% loading on a factor would have ordered the statements) are presented in Table 2. There were three consensus statements, “2. Acceptable if benefit to patient large” (ranked 9 in all models), “12. Acceptable if patient covers cost” (ranked 3–4), and “31. Acceptable if no harm to patient” (ranked 8–9). There was one differentiating statement, “35. Giving no description is acceptable” (ranked 4, 2, 2, 5, 1, and 9 in models A–F, respectively). Figure 3 shows the idealized statement scores for the six models along with mean statements’ score for the entire women cohort, with the statements grouped according to the most relevant underlying ethical principle.
 |
Table 2 Factor scores for six placebo-treatment, ethical attitude models in women |
 |
Figure 3 Placebo treatment-related ethical attitude models in women. Data represent mean or program-generated idealized ranking scores on a scale of 1 (strongly disagree) to 9 (strongly agree) of 42 placebo treatment-related statements, arranged according to the most relevant underlying ethical approach. (A) Models A (gray triangle, “relatively justice and motives-concerned”) and B (light brown circle, “relatively family and deception-concerned”). (B) Models C (dark blue square, “relatively outright lying-concerned”) and D (dark brown circle, “relatively common good-concerned”). (C) Models E (green diamond, “relatively patient benefit and vulnerability-concerned”) and F (red circle, “relatively outright lying and common good-concerned”). For reference, mean scores for the entire women cohort are represented by the light blue plus symbol in A, B, and C. For a description of the resolution models see the text. For a full description of the statements, see Supplementary File 1, Q-set statements. |
None of the models was mono-principled. As indicated above, all six models assigned rank 9 to “2. Acceptable if benefit to patient large” and ranks 8 or 9 to “31. Acceptable if no harm to patient” indicating a strong consequentialist orientation that emphasized the patient’s (rather than other parties) beneficence and non-maleficence. However, varying the degree of benefits and harms revealed that the strength of this orientation is different among the models. Ranking of “40. Acceptable with moderate benefit to patient” ranged from 9 (model E) to 5 (models A and C) and ranking of “9. Acceptable with small benefit to patient” ranged from 8 (model E) to 3 (models A and C). Interestingly, “42. Acceptable with large benefit to caring relative” was among the seven most agreeable statements only for model B and “16. Aceptable with large benefit to other patients” was among the most agreeable statements only for model D, suggesting different scope of application of the beneficence principle among the models. On the other hand, five models (all except model E) strongly agreed with “26. Acceptable with physician intent to benefit patient” and all models strongly disagreed or disagreed with “15. Acceptable with physician self-benefit intent”, indicating an overall importance of motives, and a virtue orientation in addition to the strong consequentialist perspective.
Women model A was unique in strongly agreeing with “33. Acceptable if available to similar patients” and “13. Acceptable if informed State covers cost”, indicating a distributive justice inclination. On the other hand, it was unique in strongly disagreeing with “5. Acceptable with physician intent to prove patient wrong” and it strongly disagreed with “6. Acceptable with physician intent to get rid of patient”. We interpreted this as virtue (rather than rights) orientation because the statements are about intent and because model A was also unique in strongly disagreeing with “19. Acceptable to describe as inactive drug”, and it strongly agreed with “23. Acceptable to describe as active drug” (both statements were justified in post-sorting comments based on effectiveness). Relative to other models, it can be classified as “relatively justice and motives-concerned”.
Women model B was unique in strongly agreeing with “42. Acceptable with large benefit to caring relative” (ranked 9), “34. Acceptable with moderate benefit to caring relative”, and “29. Acceptable with physician intent to benefit caring relative”. It also assigned relatively more weight to small benefit to caring relatives (Figure 3A). On the other hand, it strongly disagreed with “6. Acceptable with physician intent to get rid of patient”, “17. Acceptable to describe as active drug with delayed disclosure”, “23. Acceptable to describe as active drug”, and “35. Giving no description is acceptable”. It can be classified as “relatively family and deception-concerned”.
Women model C was unique in strongly agreeing with “8. Acceptable with delayed disclosure without early description”. It also strongly agreed with “19. Acceptable to describe as inactive drug” and “14. Acceptable to describe as drug that may help with delayed disclosure”, but strongly disagreed with “23. Acceptable to describe as active drug”. It gave relatively less weight to benefiting other patients (Figure 3B). It can be classified as “relatively outright lying-concerned”.
Women model D was unique in strongly agreeing with “16. Acceptable with large benefit to other patients” and in strongly disagreeing with “11. Acceptable with economically disadvantaged patient”. It also strongly disagreed with “20. Acceptable with moderate harm to other patients” and gave relatively more weight to benefiting other patients (Figure 3B). It can be classified as “relatively common good-concerned”.
Women model E was unique in strongly agreeing with “9. Acceptable with small benefit to patient”. It was also unique in strongly disagreeing with “8. Acceptable with delayed disclosure without early description”. Further, it strongly disagreed with “35. Giving no description is acceptable” and strongly agreed with “10. Acceptable to describe as drug that may help” and “23. Acceptable to describe as active drug”. The last four statements were justified in post-sorting comments based on effectiveness. Furthermore, it also strongly disagreed with “39. Acceptable with physician intent to please patient caring relative” and “21. Acceptable with physician intent to benefit other patients”, suggesting strong prominence of patient benefits. On the other hand, model E was unique in strongly agreeing with “27. Acceptable with educated patient” and it strongly disagreed with “22. Acceptable with uneducated patient”. It can be classified as “relatively patient benefit and vulnerability-concerned”.
Finally, women model F was unique in strongly agreeing with “35. Giving no description is acceptable” (a differentiating statement for this model). It strongly agreed with “19. Acceptable to describe as inactive drug”, strongly disagreed with “17. Acceptable to describe as active drug with delayed disclosure”, and disagreed with “23. Acceptable to describe as active drug”, indicating outright lying (rather than deception) concern. On the other hand, it was unique in strongly disagreeing with “3. Acceptable if harm to other patients small”, and it gave relatively more weight to harm to other patients in general (Figure 3C). It can be classified as “relatively outright lying and common good-concerned”. Compared to model D, the concern of model F in regard to the common good was restricted to the negative impact of placebo treatment.
Ethical Attitude Models In Men
The six-factor solution accounted for 45% of the total variance and 57 (66%) of the Q-sorts. Twenty two Q-sorts did not have significant loading on any of the factors and seven were confounded. Correlation of the scores of the 42 statements between the six factors ranged from 0.10 (factors A and F and factors B and D) to 0.60 (factors B and C). Ethical resolution model A had 11 defining Q-sorts, an eigenvalue of 5.9, and explained 7% of the variance. Model B had 16 defining Q-sorts, an eigenvalue of 9.9, and explained 12% of the variance. Model C had 15 defining Q-sorts, an eigenvalue of 8.7, and explained 10% of the variance. Model D had four defining Q-sorts, an eigenvalue of 3.4, and explained 4% of the variance. Model E had seven defining Q-sorts, an eigenvalue of 5.9, and explained 7% of the variance. Finally, model F had four defining Q-sorts, an eigenvalue of 4.0, and explained 5% of the variance.
The six program-generated model Q-sorts are presented in Table 3. There was one consensus statement, “2. Acceptable if benefit to patient large” (ranked 9 in all models). There were two differentiating statements, “17. Acceptable to describe as active drug that may help with delayed disclosure” (ranked 1, 5, 8, 5, 8, 6 in models A–F, respectively) and “26. Acceptable with physician intent to benefit patient” (ranked 9, 8, 9, 3, 9, and 7 in models A–F, respectively). Figure 4 shows the idealized statement scores for the six models along with mean statements’ score for the entire male cohort, with the statements grouped according to the most relevant underlying ethical principle.
 |
Table 3 Factor scores for six, placebo-treatment, ethical attitude models in men |
 |
Figure 4 Placebo treatment-related ethical attitude models in men. Data represent mean or program-generated idealized ranking scores on a scale of 1 (strongly disagree) to 9 (strongly agree) of 42 placebo treatment-related statements, arranged according to the most relevant underlying ethical approach. (A) Models A (gray triangle, “relatively utility and vulnerability-concerned”) and B (light brown circle, “relatively deception-concerned”). (B) Models C (dark blue square, “relatively motives-concerned”) and D (dark brown circle, “relatively pure consequentialist”) (C) Models E (green diamond, “relatively conditionally patient-centered and outright lying-concerned”) and F (red circle, “relatively patient benefit-concerned”). For reference, mean scores for the entire men cohort are represented by the light blue plus symbol in A, B, and C. For a description of the resolution models see the text. For a ull description of the statements, see Supplementary File 1, Q-set statements. |
Similar to women’s models, all six models assigned a rank of 9 to “2. Acceptable if benefit to patient large” and all but one assigned a rank of 8–9 to “31. Acceptable if no harm to patient”. Similarly, ranking of “40. Acceptable with moderate benefit to patient” ranged from 9 (model B) to 5 (model A) and ranking of “9. Acceptable with small benefit to patient” ranged from 7 (models B and C) to 1 (model A), again indicating an overall consequentialist orientation of varying strength among the models. Further, “42. Acceptable with large benefit to caring relative” was among the seven most agreeable statements for model A, but was disagreeable to models C and F, and “16. Acceptable with large benefit to other patients” was among the most agreeable statements only for models A, B, and C; again suggesting a different scope of application of the beneficence principle. Of note, only four male models strongly agreed with “26. Acceptable with physician intent to benefit patient” and only four male models strongly disagreed with “15. Acceptable with physician self-benefit intent”.
Men model A was unique in strongly agreeing with “42. Acceptable with large benefit to caring relative” and “33. Acceptable if available to similar patients”. It also strongly agreed with “16. Acceptable with large benefit to other patients”. Further, it was unique in strongly disagreeing with “9. Acceptable with small benefit to patient” and it strongly disagreed with “7. Acceptable with small benefit to other patients”, indicating a strong utilitarian view (the greatest benefit to the greatest number). In the same vein, it was unique in strongly disagreeing with “17. Acceptable to describe as active drug with delayed disclosure” (differentiating statement for this model). The justifications given in post-sorting comments included, “the placebo would lose its benefit“ and “physicians would lose their patients’ trust”. Consistently, this model assigned similarly weak positive ranking to “19. Acceptable to describe as inactive drug” and “23. Acceptable to describe as active drug” and similarly weak negative ranking to “8. Acceptable with delayed disclosure without early description” and “14. Acceptable to describe as drug that may help with delayed exposure”. On the other hand, it was unique in strongly agreeing with “27. Acceptable with educated patient” (it weakly disagreed with “22. Acceptable with uneducated patient”) and in strongly disagreeing with “24. Acceptable with child patient” (it weakly agreed with “4. Acceptable with adult patient”), indicating a concern about vulnerability. It can be classified as “relatively utility and vulnerability concerned”.
Men model B was unique in strongly agreeing with “19. Acceptable to describe as inactivedrug” and in strongly disagreeing with “35. Giving no description is acceptable”, “23. Acceptable to describe as active drug”, and “18. Acceptable if uninformed State covers cost”. It also disagreed with “41. Acceptable if uninformed insurance covers cost”. It can be classified as “relatively deception-concerned”.
Men model C was unique in strongly disagreeing with “39. Acceptable with physician intent to please patient caring relative”. It also strongly disagreed with “6. Acceptable with physician intent to get rid of patient” and “32. Acceptable with physician intent to get rid of patient insisting relative”, but strongly agreed with “26. Acceptable with physician intent to benefit patient”. On the other hand, it equally strongly agreed with “10. Acceptable to describe as drug that may help”, “17. Acceptable to describe as active drug with delayed disclosure”, and “23. Acceptable to describe as active drug”, and disagreed with “19. Acceptable to describe as inactive drug”, emphasizing intent over rightness of action. It can be classified as “relatively motives-concerned”.
Men model D was unique in strongly agreeing with “5. Acceptable with physician intent to prove patient wrong” and “25. Acceptable with physician intent to please patient”. Further, it also strongly agreed with “6. Acceptable with physician intent to get rid of patient” and, strangely, it disagreed with “26. Acceptable with physician intent to benefit patient” (a differentiating statement for this model), suggesting a strong disregard to underlying motives (or deranged perspective). On the other hand, it was unique in strongly agreeing with “22. Acceptable with uneducated patient” (justified as “should be available for everybody, especially uneducated”, in post-sorting comments) and unique in strongly disagreeing with “19. Acceptable to describe as inactive drug” (justified as “the patient would suffer”, in post-sorting comments) and “10. Acceptable to describe as drug that may help” (justified as “it indicates that the doctor is not sure”, in post-sorting comments), indicating emphasis on consequences over motives and rightness of action. It can be classified as “relatively pure consequentialist”.
Men model E was rather difficult to interpret. It was unique in strongly disagreeing with “29. Acceptable with physician intent to benefit caring relative.” The justification in post-sorting comments was that the physician should be concerned about benefiting the patient only. Consistently, it strongly disagreed with “30. Acceptable with small benefit to caring relative” and disagreed with “39. Acceptable with physician intent to please caring relative” and “7. Acceptable with small benefit to other patients”. On the other hand, it strongly disagreed not only if there is large harm to other patients but also if there is moderate or small harm (statements 36, 20, and 3). This suggests a view that placebos should be given only to benefit the patient and only if there is no harm to others. In addition, model E strongly agreed with “14. Acceptable to describe as drug that may help with delayed disclosure” and “17. Acceptable to describe as active drug with delayed disclosure”. Further, although it disagreed with “23. Acceptable to describe as active drug”, it agreed with “35. Giving no description is acceptable” and was neutral with “19. Acceptable to describe as inactive drug”, suggesting an outright lying concern. Finally, although it was unique in strongly disagreeing with “11. Acceptable with economically disadvantaged patient”, it also disagreed with “37. Acceptable with not economically disadvantaged patient”, making it difficult to interpret. It can be classified as “relatively conditionally patient-centered and outright lying-concerned”.
Finally, men model F was unique in strongly disagreeing with “22. Acceptable with uneducated patient” and “27. Acceptable with educated patient”. This was justified as “education has nothing to do with it”, in post-sorting comments. Interestingly, it also equally disagreed with “11. Acceptable with economically disadvantaged patient”and “37. Acceptable with not economically disadvantaged patient”, indicating a view of disconnection between placebo treatment and socioeconomic status of patients. It strongly agreed with “10. Acceptable to describe as drug that may help”, “14. Acceptable to describe as drug that may help with delayed disclosure”, and “23. Acceptable to describe as active drug”. It agreed with “8. Acceptable with delayed disclosure without early description” and was rather negative with “19. Acceptable to describe as inactive drug”, indicating that for this model beneficence takes precedence over honesty. It was also unique in strongly disagreeing with “34. Acceptable with moderate benefit to caring relative” and it strongly disagreed with “32. Acceptable with physician intent to get rid of patient insisting relative”, “30. Acceptable with small benefit to caring relative”, and “21. Acceptable with physician intent to benefit other patients”, suggesting a focus on patient benefit. It can be classified as “relatively patient benefit-concerned”.
Association Between Ethical Attitude Models And Respondents Characteristics
In women, the number of Q-sorts that loaded on model A, B, C, D, E, or F only or with higher loading were 7, 13, 7, 32, 9, and 9, respectively (four were confounded and 20 did not have significant loading on any model). In men, the number of Q-sorts that loaded on model A, B, C, D, E, or F only or with higher loading were 11, 17, 16, 4, 9, and 5, respectively (two were confounded and 22 did not have significant loading on any model).
In women, there was a significant association between model type and major religious affiliations (Islam vs Christianity, p=0.009) and place of education (Saudi Arabia vs the Philippines, p=0.005) but not nationality (Saudi vs Filipinos, p=0.07) or occupation (healthcare-related vs non-healthcare-related, p=0.50). The majority of Q-sorts by Muslims (53%) loaded on model D, ie, “relatively common good-concerned” (compared to 23% of Q-sorts by Christians), and the majority of Q-sorts by Christians (27%) loaded on model B, ie, “relatively family and deception-concerned” (compared to 11% of Q-sorts by Muslims). The majority of Q-sorts by respondents who completed their general education in Saudi Arabia (54%) loaded on model D (compared to 19% by their counterpart), and the majority of Q-sorts by respondents who completed their general education in the Philippines (31%) loaded on model B (compared to 7% by their counterpart). Similarly, the majority of Q-sorts by Saudis (41%) loaded on model D, whereas 32% and 26% of Q-sorts by Filipinos loaded on model D and B, respectively. Finally, the majority of the Q-sorts by healthcare respondents (44%) and non-healthcare respondents (37%) loaded on model D. There was no significant association between ethical attitude models and mean age (p=0.93) or mean Q-sorting time (p=0.55).
In men, there was no significant association between model type and religious affiliations (p=0.17), place of education (p=0.40), nationality (p=0.45), or occupation (p=0.65). However, the majority of Q-sorts by Muslims (31%) loaded on model C, ie, “relatively motives concerned” (compared to 8% of Q-sorts by Christians), and the majority of Q-sorts by Christians (33%) loaded on model B, ie, “relatively deception-concerned” (compared to 27% of Q-sorts by Muslims). The majority of Q-sorts by respondents who completed their general education in Saudi Arabia loaded on model B or C (31% vs 29% and 31% vs 21% by their counterpart, respectively), and the majority of Q-sorts by respondents who completed their general education in the Philippines loaded on model A, ie, “relatively utility and vulnerability-concerned” or B (29% vs 10% and 29% vs 31% by their counterpart, respectively). Similarly, the majority of Q-sorts by Saudis (39%) loaded on model C (compared to 20% of Q-sorts by Filipinos), and the majority of Q-sorts by Filipinos loaded on model A (27% vs 13% of Q-sorts by Saudis) or model B (27% vs 22% of Q-sorts by Saudis). Finally, the majority of Q-sorts by healthcare respondents (38%) loaded on model B (compared to 25% of Q-sorts by non-healthcare respondents), and the majority of Q-sorts by non-healthcare respondents (27%) loaded on model C (compared to 19% of healthcare respondents). Again, there was no significant association between ethical attitude models and age (p=0.08) or Q-sorting time (p=0.77).
Using Ethical Principles Other Than The Four Principles Of Principlism
It has been argued that four principles, namely respect for autonomy, beneficence, non-maleficence, and justice, are the only ethical principles required for ethical resolution of medical dilemmas (principlism).40–42 We explored whether this applies to lay person and placebo treatment. Figure 2 links the 42 statements to various ethical approaches, including those that are fundamental to the four principles (rights: respect for autonomy, consequentialism: beneficence and non-maleficence, and justice).
Two or more of nine intent-related statements received extreme ranks (model rank ˃7 or <3) in 100% of the women and men models. In addition, one statement, “26. Acceptable with physician intent to benefit patient” received high extreme rank, and two statements, “15. Acceptable with physician self-benefit intent” and “32. Acceptable with physician intent to get rid of patient insisting relative” received low extreme ranks on averaging-analysis, indicating the importance of motives (and a virtue approach) for at least some of our respondents.
In addition, although none of the three statements related to family benefit or familism (statements 30, 34, 42) received extreme ranks on averaging-analysis, one or more received high extreme rank in one women model (model B, “relatively family and deception-concerned”) and one men model (model A, “relatively utility and vulnerability-concerned”) and low extreme ranks in two men models (model E, “relatively conditionally patient-centered and outright lying-concerned” and model F, “relatively patient benefit-concerned”).
Further, one or more of the six statements related to common good or communitarianism (statements 1, 7, and 16 related to other patients’ benefit, and statements 3, 20, and 36 related to other patients’ harm) received high extreme ranks in one women model (model D) and four men models (models A, B, C, and D) and low extreme ranks in five women models (models A, B, C, D, and F) and five men models (models A, B, C, D, and E). In addition, one statement (16) received high extreme rank and two statements (20 and 36) received low extreme ranks on averaging-analysis.
Averaging-Analysis Vs Q-Methodology
Out of the 30 statements that had a neutral score on averaging-analysis (defined as mean ranking score ≥4 and ≤6, which excludes the five most agreeable and the seven most disagreeable statements), only six (20%) and five (17%) were neutral (defined as idealized score ≥3 and ≤7, which excludes the seven most agreeable and the seven most disagreeable statements) in all six women (Table 2) and all six men (Table 3) models, respectively.
On the other hand, out of the seven most agreeable and the seven most disagreeable statements for women’s models A–F, 64%, 36%, 64%, 29%, 64%, and 57%, respectively, were neutral on averaging-analysis (Table 2). The corresponding percentages for men’s models A–F were 71%, 50%, 50%, 79%, 43%, and 64%, respectively (Table 3).
Finally, there was only one statement that was neutral on averaging-analysis and in all women and men models: “28. Acceptable if informed insurance covers cost”.
Discussion
The aim of this study was to explore lay people ethical attitudes in regard to the acceptability of treating conditions that have no or inadequate therapy, by physician-prescribed placebos. We developed an instrument that covered various degrees of deception, benefits, and harms as well as various types of vulnerability, benefits, motives, and cost-bearing. Ipsative responses of a convenience sample of 101 women and 86 men were analyzed by averaging-analysis and, to explore the underlying thinking patterns, by Q-methodology.
Consequentialism Predominance
Consequentialism is a set of ethical theories, according to which the morality of an act is determined by its consequences. We found that, on averaging-analysis, consequentialism was the predominant attitude. “Acceptable if benefit to patient large”, “Acceptable if no harm to patient”, “Acceptable with moderate benefit to patient”, and “Acceptable with large benefit to other patients” were among the five most agreeable statements. This is consistent with the results of previous studies that, using different methodology and studying Western populations, showed acceptability of placebo treatment to patients and the general public,21,32,34,35 the philosophical approach used by some defenders of placebo treatment,24 the notion of good being more basic than the notion of right, and the precedence of “care/harm” as a psychological foundation of morality over other foundations.46
Consequentialists differ according to who counts and which consequence is best. Our respondents focused on the patient, with benefit to patient being clearly more important than benefits to caring relatives or to other patients, so familism, communitarianism, and utilitarianism (defined as the greatest good for the greatest number) as forms of consequentialist attitudes were on average not prominent. However, Q-methodology analysis revealed that the relative weights given to the various consequences differed among the ethical attitude models. For example, in women, model B was relatively family-concerned, models D and F relatively common good-concerned, and model E relatively patient benefit-concerned. In men, model A was relatively utility-concerned, model D relatively pure consequentialist, model F relatively patient benefit-concerned, and model E relatively patient benefit-concerned provided there is no harm to other patients.
Respect To Autonomy And Attitude Toward Deception
On averaging-analysis, the most agreeable act-related statements was “Acceptable to describe as drug that may help” followed by “Acceptable to describe as drug that may help with delayed disclosure”. Description as inactive drug, and giving no description or description as pharmacologically active drug with delayed disclosure were less acceptable (apparently because of reduced benefit), whereas description as pharmacologically active drug and giving no description were the least acceptable actions. The data are consistent with previous results32 and indicate that, for our respondents, the act itself is also important (although less important than its consequences), deception that creates false belief is worse than deception that negates or blocks true belief, and outright lying is different and worse than non-lying deception.
Deception is not a single construct. It can be achieved by equivocation, evasion, being economical with the truth, refraining from correcting a misunderstanding, or outright lying. The philosophical view that outright lying is morally worse than non-lying deception24,28 rather than morally equivalent29 argues that “to deceive”, unlike “to lie”, is a success-verb that gives the victim more chance to get things right, and that, in outright lying, the intend is not only to deceive but also to do so by lying, that crossing the lying–deception boundary by people who believe there is a boundary may have a negative moral effect on them,28 and that analogous to the distinction between killing and letting die, not-to deceive may not be as exceptionless as not-to-lie.47 Nevertheless, lying and deception may be scalar phenomena and may allow a number of intermediate states; they involve graded truth values (a statement may be only partly false) and graded beliefs (graded degree of confidence in the statement).25
Some ethicists find deception permissible only “at either end of the scale of importance” (ie, crisis or triviality).27 For our respondents, the acceptability of placebo treatment was rather proportional to benefits’ size.
It is to be noted that placebos could exert an effect without deception (open-label placebos), where positive expectations are induced by stating that placebos may have a powerful effect through mind-body self-healing processes. Although several studies have shown open-placebo effect,16,48–51 they were restricted to subjective symptoms and may have suffered from selection bias,52 and it is not known whether open-label placebos are as powerful as concealed placebos. In addition, beneficial outcomes could be induced without deception by changing patients mindsets and general expectations about health and illness (to expect the best outcome, diseases are curable, etc) rather than specific expectation from a specific intervention.53 Open-label placebos and changing general expectations were not addressed in our study.
It is not clear whether the different attitude to non-lying deception vs outright lying reflects a more general view about deception/lying, is specific to patient-physician relationship, or even specific to placebo treatment. The patient's right not to be deceived is a negative (liberty) right and thus theoretically has stronger moral weight than the positive (welfare) right of beneficence, and duty of care implies a duty to maintain trust. However, it may be that in the patient–physician relationship, trust is more related to “work in my interest” than to “tell me the whole truth”, in a way similar to the relationship between a conjuror and audience, where there is a welcome acceptance of deception. Compared to not disclosing bad news, placebo treatment does not imply disrespect to patients as incapable of understanding and controlling their situation. Further, it has been argued that even deontological arguments against deception may not preclude placebo treatment, because disclosing that placebos are pharmacologically inert is incidental information that does not increase “informedness” but could decrease it if the patient is in “the grip of a false picture” that placebos are inactive.20
Paternalism implies interference with another person, against their will, for their benefit (and potentially for the benefit of their long-run autonomy). In weak paternalism, it is legitimate to interfere with the means individuals choose to achieve their ends, if their means are likely to defeat their ends (rather than interfering to prevent them from achieving their ends). In pure paternalism, the person being benefited is identical to the person being interfered with. It appears that the attitude of our respondents toward placebo treatment was, in general, consistent with accepting weak, pure, medical paternalism. Nevertheless, Q-methodology revealed different attitudes in this regard. For example, women model B and men model B were deception-concerned compared to women models C and F and men model E, which were only outright lying-concerned. Further, impure paternalism was acceptable to some of our respondents; women models B and D accepted to prescribe placebo treatment to a patient in order to benefit the patient’s caring relatives or other patients, respectively (in contrast to women model E and men model F).
Finally, part of respect to autonomy is protection of vulnerable subjects, such as children and uneducated patients. In the current study, acceptability of placebo treatment was, on average, higher for educated and adult (and to some degree for not economically disadvantaged) patients compared to their counterparts, and Q-methodology showed that two of the 12 models were vulnerability-concerned (women model E and men model A). A focus group study of patients’ views showed that placebo treatment is acceptable if the recipient is a child.12
Motives And Adequacy Of Principlism
Advocates of principlism have argued that four principles (respect for autonomy, beneficence, non-maleficence, and justice) are sufficient for unversalisable normative morality40,42 and that although virtue ethics is important to instantiate and sustain the four principles in real life,40 motives and emotional and personal factors are not part of moral decision-making. Our empirical data show that motives were very important in judging the acceptability of placebo treatment. The mean rank of “Acceptable with physician intent to benefit patient” was second only to “Acceptable if benefit to patient large”, whereas “Acceptable with physician self-benefit intent” and “Acceptable with physician intent to get rid of patient insisting relative” received the lowest and fourth lowest ranks. Further, two or more of the nine intent-related statements received extreme rank in 100% of women and men models and Q-methodology was able to identify two motives-concerned models (women model A and men model C). This is consistent with the finding that for common people, judgments of wrongness/permissibility of an action rely in part on the mental state (intend=belief+desire) of the agent.54 In the same vein, since the 4th century, medical oaths and codes of practice have committed to virtuous behavior.55
The two motives-concerned models, within the overall picture of consequentialist orientation, are consistent with a version of utilitarianism that takes into account only intended consequences of actions. Interestingly, the majority of Muslim men loaded on the motives-concerned model; consistent with the view that Islam is a special consequentialist moral doctrine where motives are not irrelevant to the consequences (I call the motives to be the deed). However, this was not true for Muslim women.
One or more of three statements related to family benefit received high extreme ranks in two of the 12 women and men models, and one women model was classified by Q-methodology as family-concerned. Further, one or more of the six statements related to the common good received high extreme ranks in five of the 12 models, and Q-methodology classified two of the women models (models D and F) as common good-concerned. Together, the data suggest that, when it comes to lay people's moral attitude to placebo treatment, principlism is inadequate, and virtue, familism, and communitarianism may be important perspectives.
Ethical Attitude To Placebo Treatment Is Associated With Respondents’ Demographics
We noted the following associations. First, healthcare respondents, on average, put more weight on moderate benefit to the patient than their counterparts, and the majority of healthcare men loaded on a deception-concerned model, whereas the majority of non-healthcare men loaded on a motives-concerned model. This may be related to codes of medical practice,9 and is consistent with the observation that patients appear to accept a paternalistic approach more than physicians.21,35 Second, compared to Christians, Muslims, on average, put more weight on patient benefit, intent to benefit patient, and harm to other patients, and less weight on honesty and intent to please the patient’s caring relative. Consistently, the majority of Christian (and Filipino and Philippines-educated) women loaded on a family and deception-concerned model, the majority of Muslim (and Saudi and Saudi-educated) women loaded on a common good-concerned model, the majority of Christian (and Filipino) men loaded on a deception-concerned model, and the majority of Muslim (and Saudi) men loaded on a motives-concerned model.
The causes underlying the observed associations are likely multifactorial. People may hold the same values at different hierarchy, due in part to what values they were told to pay more attention to by families/friends. Alternatively, it may be due to analogical reasoning, where paradigm cases rather than ethical principles are the main sources of decision-making42 or to the fact that attitudes may be based on moral intuition rather than moral reasoning.56
Advantage Of Q-Methodology Over Averaging-Analysis
Averaging-analysis tends to have a depersonalizing effect, which is avoided in Q-methodology.36–39 This was apparent in the current study. Out of 30 statements that had neutral ranks on averaging-analysis, only 20% and 17% were neutral in all six women and all six men models, respectively. Further, out of the seven most agreeable and the seven most disagreeable statements for women or men models, 29% to 79% were neutral on averaging-analysis. Moreover, several of the attitude models that were revealed by Q-methodology would have been difficult to suspect looking only at averaging-analysis data.
Study Strengths And Limitations
This study has several methodological strengths, including the use of ipsative scores to minimize the tendency to respond in a general way, a shuffled set of statements to minimize the tendency to respond on basis other than items’ content (for example, due to the order effect or moral credentialing bias), and forced-distribution ranking to offset the tendency to attribute maximum importance to a large number of statements, assertiveness effect seen in complete rank-ordering, and categorizing proclivity seen in dichotomization.
The study has several limitations. First, the results may not be generalizable since a convenience sampling was used and only educated and committed individuals were recruited. Second, although responses to hypothetical scenarios likely reflect society’s internalized norms and beliefs, they may not be accurate predictors of real-life responses. Third, our Q-set did not cover all statements potentially relevant to placebo treatment. For example, we did not address open-label placebos, placebo treatment when pharmacologically active interventions are available and adequately effective, or the difference between pure and impure placebos. Fourth, although we provided our respondents with a clear explanation of placebos, they may have had variable or different understanding of the concept. Furthermore, respondents could have understood some of the statements differently. Fifth, the study was designed to explore the attitude toward the acceptability of placebo use in general; it did not specify whether it is from a prescriber, patient, or a third party point of view. Sixth, since Q-methodology is typically exploratory and not exhaustive, it is likely that there are other than the study-identified models, and the prevalence of the identified models among the larger population cannot be inferred from the study. Finally, there was some overlap among the identified models; a higher discrimination power would have been obtained by having more than nine sorting categories; however, this would be associated with more randomness in response.
Conclusions
Our data support four main conclusions. First, on averaging-analysis, patient’s beneficence and physician’s intent were more important than absence of deception. Second, it appears that in the setting of patient–physician relationship and placebo treatment, non-lying deception and outright lying are not on the same footing, and “information management” may be acceptable. A modified consequentialist perspective that takes into consideration intentions and the manner in which beneficial results are obtained seems to be preferred by most of our respondents. This raises a challenge to the prevailing formal convention against all deception in medical practice. Third, Q-methodology identified various ethical attitude models that were mostly multi-principled, partly associated with respondents’ demographics, and partly concealed in averaging-analysis. This indicates that lay people differ in how they balance the various ethical interests to reach individual points of ethical equilibrium, and that a one-size-fits-all approach may not be applicable in this context. Fourth, the four principles of principlism may not be adequate when it comes to characterizing lay people's attitude to placebo treatment.
The placebo effect contributes importantly to the success of both pharmacologically active and pharmacologically inactive interventions. The ways of ethical reasoning explored in the current study could be used to identify individuals who would accept placebo treatment and to improve the acceptability of placebo treatment for individuals who would not.
Abbreviations
ANOVA, Analysis of variance; KFSH&RC, King Faisal Specialist Hospital and Research Center; REC, Research Ethics Committee; SD, Standard deviation.
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki after approval of the Research Ethics Committee (REC) of the King Faisal Specialist Hospital and Research Center (KFSH&RC). All respondents provided written informed consent as approved by the REC.
Availability of data and materials
Additional data are available under Supplementary File 1 and Supplementary File 2. Raw data are available upon request from the corresponding author.
Acknowledgment
The authors would like to thank the staff of the Clinical Studies and Empirical Ethics Department for their help in collecting data.
Author contributions
MMH designed the study, performed data analysis, and wrote the manuscript. SH performed the literature review, managed data, co-analyzed data, and co-wrote the manuscript. RA and ASA contributed to the literature review, models interpretation, and manuscript drafting. All authors agree to be accountable for all aspects of the work and gave approval of the final version of the manuscript.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Hróbjartsson A, Norup M. The use of placebo interventions in medical practice – a national questionnaire survey of Danish clinicians. Eval Health Prof. 2003;26(2):153–165. doi:10.1177/0163278703026002002
2. Nitzan U, Lichtenberg P. Questionnaire survey on use of placebo. Bmj. 2004;329:944–946. doi:10.1136/bmj.38236.646678.55
3. Gray G, Flynn P. A survey of placebo use in a general hospital. Gen Hosp Psychiatry. 1981;3:199–203.
4. Thomson RJ, Buchanan WJ. Placebos and general practice: attitudes to, and use of the placebo effect. N Z Med J. 1982;95:492–494.
5. Sherman R, Hickner J. Academic physicians use placebos in clinical practice and believe in the mind-body connection. J Gen Intern Med. 2008;23:7–10. doi:10.1007/s11606-007-0332-z
6. Tilburt JC, Emanuel EJ, Kaptchuk TJ, Curlin FA, Miller FG. Prescribing “placebo treatments”: results of national survey of US internists & rheumatologists. Bmj. 2008;33:a1938. doi:10.1136/bmj.a1938
7. Fässler M, Meissner K, Schneider A, Linde K. Frequency and circumstances of placebo use in clinical practice–a systematic review of empirical studies. BMC Med. 2010;8:15. doi:10.1186/1741-7015-8-15
8. Howick J, Bishop FL, Heneghan C, et al. Placebo use in the United Kingdom: results from a national survey of primary care practitioners. PLoS One. 2013;8(3):e58247. doi:10.1371/journal.pone.0058247
9. Sokol DK. Can deceiving patients be morally acceptable? BMJ. 2007;334(7601):984–986. doi:10.1136/bmj.39184.419826.80
10. Wang RS, Hall KT, Giulianini F, Passow D, Kaptchuk TJ, Loscalzo J. Network analysis of the genomic basis of the placebo effect. JCI Insight. 2017;2(11):e93911. doi:10.1172/jci.insight.88864
11. Teasdale K, Kent G. The use of deception in nursing. J Med Ethics. 1995;21(2):77–81. doi:10.1136/jme.21.2.77
12. Bishop FL, Aizlewood L, Adams AE. When and why placebo-prescribing is acceptable and unacceptable: a focus group study of patients’ views. PLoS One. 2014;9(7):e101822. doi:10.1371/journal.pone.0101822
13. Moerman DE, Jonas WB. Deconstructing the placebo effect and finding the meaning response. Ann Intern Med. 2002;136(6):471–476. doi:10.7326/0003-4819-136-6-200203190-00011
14. Kienle GS, Kiene H. The powerful placebo effect: fact or fiction? J Clin Epidemiol. 1997;50(12):1311–1318. doi:10.1016/s0895-4356(97)00203-5
15. Fillingim RB, Price DD. What is controlled for in placebo-controlled trials? Mayo Clin Proc. 2005;80(9):1119–1121. doi:10.4065/80.9.1119
16. Zhou ES, Hall KT, Michaud AL, Blackmon JE, Partridge AH, Recklitis CJ. Open-label placebo reduces fatigue in cancer survivors: a randomized trial. Support Care Cancer. 2018. doi:10.1007/s00520-018-4477-6
17. Hammami MM, Al-Gaai EA, Alvi S, Hammami MB. Interaction between drug and placebo effects: a cross-over balanced placebo design trial. Trials. 2010;11:110. doi:10.1186/1745-6215-11-110
18. Hammami MM, Hammami S, Al-Swayeh R, Al-Gaai E, Farah FA, De Padua SJ. Drug*placebo interaction effect may bias clinical trials interpretation: hybrid balanced placebo and randomized placebo-controlled design. BMC Med Res Methodol. 2016;16(1):166. doi:10.1186/s12874-016-0269-1
19. Lund K, Vase L, Petersen GL, Jensen TS, Finnerup NB. Randomised controlled trials may underestimate drug effects: balanced placebo trial design. PLoS One. 2014;9(1):e84104. doi:10.1371/journal.pone.0084104
20. Glackin SN. Placebo treatments, informed consent and ‘the grip of a false picture’. J Med Ethics. 2015;41(8):669–672. doi:10.1136/medethics-2014-102332
21. Fassler M, Gnadinger M, Rosemann T, Biller-Andorno N. Placebo interventions in practice: a questionnaire survey on the attitudes of patients and physicians. B J Gen Pract. 2011;61(583):101–107. doi:10.3399/bjgp11X556209
22. Asai A, Kadooka Y. Reexamination of the ethics of placebo use in clinical practice. Bioethics. 2013;27(4):186–193. doi:10.1111/j.1467-8519.2011.01943.x
23. Petersen GL, Finnerup NB, Colloca L, et al. The magnitude of nocebo effects in pain: a meta-analysis. Pain. 2014;155(8):1426–1434. doi:10.1016/j.pain.2014.04.016
24. Jackson J. Telling the truth. J Med Ethics. 1991;17(1):5–9. doi:10.1136/jme.17.1.5
25. Marsili N. Lying as a scalar phenomenon. In: Cantarini S, Abraham W, Leiss E, editors. Certainty-uncertainty – And the Attitudinal Space in Between. John Benjamins Publishing, Amsterdam, The Netherlands; 2014
26. Alexander L, Sherwin E. Deception in Morality and Law. Cornell Law Faculty Publications; 2003:854. Available from: https://scholarship.law.cornell.edu/facpub/854.
27. Higgs R. On telling patients the truth. In: Lockwood M, editor. Moral Dilemmas in Modern Medicine. Oxford: Oxford University Press; 1985
28. Benn P. Medicine, lies and deceptions. J Med Ethics. 2001;27(2):130–134. doi:10.1136/jme.27.2.130
29. Bakhurst D. On lying and deceiving. J Med Ethics. 1992;18(2):63–66. doi:10.1136/jme.18.2.63
30. Chan TE. Regulating the placebo effect in clinical practice. Med Law Rev. 2015;23(1):1–26. doi:10.1093/medlaw/fwu026
31. Barnhill A, Miller FG. The ethics of placebo treatments in clinical practice: a reply to Glackin. J Med Ethics. 2015;41(8):673–676. doi:10.1136/medethics-2014-102651
32. Pugh J, Kahane G, Maslen H, Savulescu J. Lay attitudes toward deception in medicine: theoretical considerations and empirical evidence. AJOB Empir Bioeth. 2015;7(1):31–38. doi:10.1080/23294515.2015.10214948
33. Hull SC, Colloca L, Avins A. Patients’ attitudes about the use of placebo treatments: telephone survey. Bmj. 2013;347:f3757. doi:10.1136/bmj.f3757
34. Chen G, Johnson MH. Patients’ attitudes to the use of placebos: results from a New Zealand survey. N Z Med J. 2009;122(1296):35–46.
35. Lynöe N, Mattsson B, Sandlund M. The attitudes of patients and physicians towards placebo treatment: a comparative study. Soc Sci Med. 1993;36(6):767–774. doi:10.1016/0277-9536(93)90037-5
36. Hammami MM, Al Gaai E, Hammami S, Attala S. Exploring end of life priorities in Saudi males: usefulness of Q-methodology. BMC Palliat Care. 2015;14:66. doi:10.1186/s12904-015-0064-5
37. Hammami MM, Hammami S, Amer HA, Khodr NA. Typology of end-of-life priorities in Saudi females: averaging analysis and Q-methodology. Patient Prefer Adherence. 2016;10:781–794. eCollection 2016. doi:10.2147/PPA.S105578.
38. Hammami S, Farah FA, Hammami MM. Surrogate end-of-life decisions: projection or simulation? Gen Med (los Ngel). 2016;4. 247. doi:10.4172/2327-5146.1000247.
39. Hammami MM, Abuhdeeb K, Hammami MB, De Padua SJS, Al-Balki A. Prediction of life story narrative for end-of-life surrogate’s decision-making is inadequate: a Q-methodology study. BMC Med Ethics. 2019;20:28. doi:10.1186/s12910-019-0368-8
40. Gillon R. Ethics needs principles – four can encompass the rest – and respect for autonomy should be “first among equals”. J Med Ethics. 2003;29:307–312. doi:10.1136/jme.29.5.307
41. Gillon R. Medical ethics: four Principles plus attention to scope. Bmj. 1994;309:184. doi:10.1136/bmj.309.6948.184
42. Beauchamp T. Methods and principles in biomedical ethics. J Med Ethics. 2003;29:269–274. doi:10.1136/jme.29.5.269
43. Chan HM. Sharing death and dying: advance directives, autonomy and the family. Bioethics. 2004;18(2):87–103.
44. Callahan D. Principlism and communitarianism. J Med Ethics. 2003;29:287–291. doi:10.1136/jme.29.5.287
45. Campbell A. The virtues (and vices) of the four principles. J Med Ethics. 2003;29:292–296. doi:10.1136/jme.29.5.292
46. Graham J, Haidt J, Nosek B. Liberals and conservatives rely on different moral foundations. J Pers Soc Psychol. 2009;96(5):1029–1046. doi:10.1037/a0015141
47. Gillon R. Is there an important moral distinction for medical ethics between lying and other forms of deception? J Med Ethics. 1993;19(3):131–132. doi:10.1136/jme.19.3.131
48. Hoenemeyer TW, Kaptchuk TJ, Mehta TS, Fontaine KR. Open-label placebo treatment for cancer-related fatigue: a randomized-controlled clinical trial. Sci Rep. 2018;8(1):2784. doi:10.1038/s41598-018-20993-y
49. Kaptchuk TJ, Friedlander E, Kelley JM, et al. Placebos without deception: a randomized controlled trial in irritable bowel syndrome. PLoS One. 2010;5(12):e15591. doi:10.1371/journal.pone.0015591
50. Kelley JM, Kaptchuk TJ, Cusin C, Lipkin S, Fava M. Open label placebo for major depressive disorder: a pilot randomized controlled trial. Psychother Psychosom. 2012;81(5):312–314. doi:10.1159/000337053
51. Carvalho C, Caetano JM, Cunha L, Rebouta P, Kaptchuk TJ, Kirsch I. Open-label placebo treatment in chronic low back pain: a randomized controlled trial. Pain. 2016;157(12):2766–2772. doi:10.1097/j.pain.0000000000000473
52. Petrie KJ, Rief W. Psychobiological mechanisms of placebo and nocebo effects: pathways to improve treatments and reduce side effects. Annu Rev Psychol. 2019;70:599–625. doi:10.1146/annurev-psych-010418-102907
53. Zion SR
54. Cushman F. Crime and punishment: distinguishing the roles of causal and intentional analyses in moral judgment. Cognition. 2008;108:353–380. doi:10.1016/j.cognition.2008.03.006
55. Gardiner P. A virtue ethics approach to moral dilemmas in medicine. J Med Ethics. 2003;29:297–302. doi:10.1136/jme.29.5.297
56. Haidt J. The emotional dog and its rational tail: a social intuitionist approach to moral judgment. Psychol Rev. 2001;108(4):814–834.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
