Back to Journals » Patient Preference and Adherence » Volume 11
Lay health educators within primary care practices to improve cancer screening uptake for South Asian patients: challenges in quality improvement
Authors Lofters AK , Vahabi M, Prakash V, Banerjee L, Bansal P, Goel S, Dunn S
Received 9 November 2016
Accepted for publication 17 January 2017
Published 8 March 2017 Volume 2017:11 Pages 495—503
DOI https://doi.org/10.2147/PPA.S127147
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
AK Lofters,1–4 M Vahabi,5 V Prakash,6 L Banerjee,7 P Bansal,8 S Goel,7,8 S Dunn1,2,9
1Department of Family and Community Medicine, 2Dalla Lana School of Public Health, University of Toronto, 3Department of Family and Community Medicine, 4Centre for Urban Health Solutions, St Michael’s Hospital, 5Daphne Cockwell School of Nursing, Ryerson University, Toronto, 6Screening Saves Lives Program, Canadian Cancer Society, Mississauga, 7Wise Elephant Family Health Team, Brampton, 8Mississauga Halton Central West Regional Cancer Program, Mississauga, 9Women’s College Research Institute, Women’s College Hospital, Toronto, ON, Canada
Background: Cancer screening uptake is known to be low among South Asian residents of Ontario. The objective of this pilot study was to determine if lay health educators embedded within the practices of primary care providers could improve willingness to screen and cancer screening uptake for South Asian patients taking a quality improvement approach.
Materials and methods: Participating physicians selected quality improvement initiatives to use within their offices that they felt could increase willingness to screen and cancer screening uptake. They implemented initiatives, adapting as necessary, for six months.
Results: Four primary care physicians participated in the study. All approximated that at least 60% of their patients were of South Asian ethnicity. All physicians chose to work with a preexisting lay health educator program geared toward South Asians. Health ambassadors spoke to patients in the office and telephoned patients. For all physicians, ~60% of South Asian patients who were overdue for cancer screening and who spoke directly to health ambassadors stated they were willing to be screened. One physician was able to track actual screening among contacted patients and found that screening uptake was relatively high: from 29.2% (colorectal cancer) to 44.6% (breast cancer) of patients came in for screening within six months of the first phone calls. Although physicians viewed the health ambassadors positively, they found the study to be time intensive and resource intensive, especially as this work was additional to usual clinical duties.
Discussion: Using South Asian lay health educators embedded within primary care practices to telephone patients in their own languages showed promise in this study to increase awareness about willingness to screen and cancer screening uptake, but it was also time intensive and resource intensive with numerous challenges. Future quality improvement efforts should further develop the phone call invitation process, as well as explore how to provide infrastructure for lay health educator training and time.
Keywords: quality improvement, cancer screening, ethnicity, health equity, health promotion, primary care
Introduction
The province of Ontario, Canada’s most populous province with 13 million people, has well-established screening disparities for breast, cervical, and colorectal cancer, particularly for people of low socioeconomic status and people who are foreign-born.1–10 Ontarians of South Asian ethnicity, that is those from India, Pakistan, Bangladesh, and Sri Lanka, have been identified as an immigrant group particularly vulnerable to underscreening for all three cancers.8,11–13 Despite generally having good access to primary care, and better access than many other immigrant groups, South Asian Ontarians appear to be the most underscreened group for all three cancers.3,5,8
Ontario has organized screening programs for these three cancers, which include invitations, information about test results, and reminders for when it is time to repeat screening sent directly to residents of the province who are eligible for screening.14–16 However, cancer screening is still fundamentally embedded in primary care, suggesting that primary care providers could be key to addressing underscreening for South Asian patients.
Similar to other jurisdictions, Ontario primary care providers practice in a wide variety of practice structures (eg, solo practitioners and large multidisciplinary teams). These structures have varying degrees of infrastructure and support to take on initiatives aimed at improving quality of care for particular at-risk groups, which suggests that primary care–based initiatives cannot be too prescriptive. Successful implementation of primary care–based initiatives for this patient population will also have to incorporate cultural considerations. A previous Ontario study identified several key barriers to cancer screening for South Asians, including health education programs not offering materials that are easy to understand, limited knowledge among patients, patients’ beliefs and fears, and the health system not accommodating South Asian culture.17
Quality improvement is a systematic approach to making changes in health care that aims to produce better outcomes for patients and stronger performance of the health care system.18,19 Key components of quality improvement are developing and conducting rapid tests of change within practice settings, recognizing that what works well for one physician or practice might need adaptation for another, consistently evaluating change for success and failure, adapting approaches, and spreading successful change.18–21 Quality improvement is becoming part of the primary care culture in Canada and internationally. Ontario’s interprofessional team-based primary care organizations are now required to submit annual quality improvement plans.22
The objective of this pilot study was to determine if primary care provider–led quality improvement initiatives could improve willingness to screen and cancer screening uptake for South Asian patients. This study describes the experiences of four primary care providers who embedded lay health educators within their practices taking a quality improvement approach.
Materials and methods
Study setting
The study took place within the Peel Region of Ontario. Peel Region, with a population of 1.3 million people and growing, has lower cancer screening uptake for breast, cervical, and colorectal cancers than the provincial average.10 Screening rates are especially and consistently low in areas of the region inhabited by a large number of South Asians.10 Peel Region has a sizeable South Asian population, with 28% of Peel residents having South Asian ancestry as compared to 6.6% for the province of Ontario as a whole.10,23 India and Pakistan are the top two source countries for immigrants in Peel, and Punjabi and Urdu are the top two non-official languages.23
Participant recruitment
We aimed to recruit a minimum of four primary care provider participants for this pilot study. To recruit participants, we presented the study to primary care groups in the region and also used a snowball sampling technique. Participants were deemed appropriate if they self-identified as 1) having their primary care practice based in Peel Region and 2) having at least 20% of their patient population as South Asians. A screening questionnaire also queried potential participants about gender and ethnicity in order to document demographics.
We recruited four family physicians for this study (Table 1). Three physicians volunteered after hearing about the study, and Physician #4 agreed to participate after she was approached. No physicians declined to participate. All physicians had strong preexisting interests in improving their patients’ cancer screening uptake and all identified as being of South Asian ethnicity themselves. Two physicians (one male and one female) practiced together in the same interprofessional team-based primary care organization where remuneration is primarily by capitation. Two physicians (one male and one female) practiced in more traditional family practice models where remuneration is primarily fee-for-service. All four physicians were in family practice models that made them eligible for preventive care bonuses from the provincial government if they met minimum cancer screening thresholds. All four participants approximated that at least 60% of their patient population was of South Asian ethnicity. The provincial cancer care agency routinely provides Ontario family physicians with breast, cervical, and colorectal cancer screening rates for their individual practices as well as names and ages of overdue patients. Screening rates for participating physicians prior to study initiation varied and are presented in Table 1.
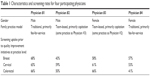  | Table 1 Characteristics and screening rates for four participating physicians |
This study was approved by the St Michael’s Hospital Research Ethics Board and all participating physicians provided written informed consent for this study.
Training workshop
An initial half-day workshop was held with participants. The workshop provided them with relevant background information on current provincial cancer screening guidelines,14,16,24 cancer screening rates in Peel Region and among South Asians in particular, and patient- and provider-focused evidence-based initiatives to increase cancer screening. They received information on Plan-Do-Study-Act (PDSA) cycles, a quality improvement methodology consisting of a rapid succession of small tests. Each test tries out different variations of an idea for improvement and incorporates results from the previous test.20,21 These small tests of change take into account the diversity of settings in which physicians function and that what works well for one physician might need significant adaptation for another.
The workshop also highlighted existing local and provincial initiatives aimed at increasing cancer screening in primary care. One program of particular focus was the Canadian Cancer Society’s Screening Saves Lives program, a preexisting lay health educator program that was focusing on South Asians in the region. Lay health educators in the program, referred to as health ambassadors, were of South Asian ethnicity themselves. Most health ambassadors were foreign-trained physicians who were not practicing medicine in Canada, but some were non-physician members of the South Asian community with strong social networks. Health ambassadors were trained to share screening messages with their peers and social networks.
As part of the Screening Saves Lives program (and independent of this pilot study), the volunteers recruited for the role of health ambassador underwent a four-session training program. The first session introduced the Canadian Cancer Society and the Screening Saves Lives program. This session also included key cancer statistics to highlight the need for screening of colon, breast, and cervical cancers. The second session focused on cancer screening guidelines for these three cancers in Ontario and practical considerations for screening. The third session focused on motivations and the barriers to screening and the transtheoretical model stages of change.25 The training concluded with a final session on administrative duties of the health ambassadors. The content and activities were designed to be flexible to the cultural needs and facilitating styles of the participants.
Quality improvement initiatives
After the workshop, physicians were asked to test quality improvement initiatives of their choosing for a minimum of six months. They were encouraged to pursue initiatives that had low long-term costs, that were feasible to implement and maintain in the long term, and those that did not require onerous effort in the long term by providers and office staff.20,26 They were also encouraged to pursue quality initiatives that had some evidence for improving cancer screening, for example, providing one-on-one education, reducing structural barriers, small media (pamphlets and brochures), sending patient reminders.27–29 Physicians were asked to reflect on results at the end of each test of change conducted, including whether success was achieved, what was learned at the end of each test, and what would be used to plan the next test.
Interviews
Brief structured interviews were conducted with participants prior to study initiation and after six-month period. Interviews assessed anticipated and experienced barriers and facilitators to implementation of quality improvement initiatives. All interviews were tape-recorded and transcribed. A content analysis approach was used to identify themes from the transcripts, using a line-by-line analysis of responses to produce a summary of themes.30
Results
Anticipated barriers and facilitators for physicians
Prior to implementation, the physicians noted several anticipated barriers to implementation of their quality improvement initiatives, many of which were at the patient level. Key themes were resource restraints, patients’ lack of knowledge of screening, and structural barriers:
I will have to get approval from my colleagues as I feel there may be some hesitation as office resources will be used. [Physician #1, male, traditional family practice model]
People say they will come and they don’t. Second is reluctance, people don’t understand the importance of these tests and even this is common among educated South Asians. [Physician #2, female, interdisciplinary family health team]
One of the barriers is you have to have booked appointments. [Physician #3, male, interdisciplinary family health team]
… lack of knowledge among patients, lack of means of transportation … [Physician #4, female, traditional family practice model]
Physicians universally noted that supportive office staff could be a facilitator to implementing their screening initiatives, including staff able to contact patients and staff who spoke South Asian languages.
Chosen initiatives and tests of changes
Tables 2–4 summarize the chosen quality improvement initiatives for the participating physicians. All physicians chose to work with the Screening Saves Lives’ Health Ambassador program in some capacity. One or two health ambassadors volunteered at each office for a total of three to five hours per week. Working together with the Screening Saves Lives program, physicians chose to look at the number of patients reached and willingness to screen as feasible outcome measures, with health ambassadors taking on core roles of tracking and documenting, again for feasibility. Considering the relatively short time frame, it was deemed unlikely that physicians would be able to see a meaningful change in screening rates within the six-month time frame of the study.
  | Table 2 Quality improvement initiatives for Physician #1 |
  | Table 3 Quality improvement initiatives for Physicians #2 and #3 |
  | Table 4 Quality improvement initiatives for Physician #4 |
For Physicians #1–3, working with the lay health educator program ultimately involved health ambassadors telephoning overdue patients, making use of their knowledge of South Asian languages, to educate them about screening. These three physicians went through three change cycles in the study period. Further, Physicians #2 and #3 allowed health ambassadors to directly book screening appointments at the time of telephone calls. In the fourth physician’s office, health ambassadors spoke to patients in the waiting room throughout the study period. For all physicians, ~60% of South Asian patients overdue for screening reported willingness to be screened after speaking directly with a health ambassador (Tables 2–4).
Physician #1 was able to maintain a list of all patients who had been telephoned, and after the study period was over, he opted to look at screening uptake among these patients. A health ambassador who had not previously been involved in the pilot study reviewed electronic medical records in July 2016 for patients who had been called. Screening uptake among those who had received a phone call was 29.2% (colorectal cancer), 36.3% (cervical cancer), and 44.6% (breast cancer) (Table 2).
Actual barriers and facilitators for physicians
At the conclusion of the six-month process, participating physicians described the barriers and facilitators they had experienced in increasing screening uptake for their South Asian patients. Key themes for barriers included increased workload and no-shows for patients who had booked screening appointments:
The number of people I had that went for screening after talking to the Health Ambassadors was not that was expected. I was expecting 1 in 4 or 5 but it was not. I would say it was 1 in 10 who followed up … The barriers were still cultural, that people did not want to do the screening due to various reasons … this process is time consuming and requires a lot of effort and is more than the benefits. [Physician #1]
… finding space for the HAs to conduct telephone calls and have a private area was a kind of limitation … I think that reaching out to the patients during the day was a barrier as everybody was not at home … what mostly surprises me is when more people don’t show up … [Physician #2]
I think the main barriers are the patients who need the test don’t come to the office … it’s difficult to reach them …all of these are time consuming and more staff and more work load has been added to the clinic … [Physician #3]
Even if you push them to do it, they still don’t do it. [Physician #4]
Despite these barriers, the participating physicians viewed working with the health ambassadors very positively. Key facilitators were the health ambassadors themselves and the quality improvement framework:
I think that having the Health Ambassador was excellent. I think she is interested, she is motivated …. Having someone who could speak multiple languages and someone who could reach out to them was of great help … [Physician #1]
I think, the education piece by HAs was sort of a key, much more valuable and people were more receptive to that …. [Physician #2]
What helped was that we had a dedicated person …. [Physician #3]
Number one is Health Ambassadors who educated and informed our patients and staff …. [Physician #4]
The quality improvement approach was also explicitly noted by Physician #1 as a facilitator:
… for the average family physician, you have to have someone with a framework, help them implement it and have regular feedback. The idea of giving somebody a boxed solution to do it is likely not going to end up in success. [Physician #1]
Physicians #2–4 reported that they planned to continue with their initiatives past the study period.
Discussion
In this pilot study, four family physicians undertook quality improvement initiatives to improve cancer screening for South Asian patients in their primary care practices. All four physicians made use of an existing lay health educator program and integrated these lay health educators, or health ambassadors, directly into their practice settings. Making phone calls to patients to invite them for screening had the most reach and the most appeal for participating physicians. For all physicians, ~60% of South Asian patients who were overdue for cancer screening and who spoke directly to health ambassadors stated they were willing to be screened. One physician was able to track actual screening among contacted patients and found that screening uptake was relatively high: from 29.2% (colorectal cancer) to 44.6% (breast cancer) of patients came in for screening within six months of the first phone calls. However, the screening uptake among South Asian patients is unknown and this same physician reported being unlikely to continue with initiatives, because of the significant amount of time and resources required.
In the transtheoretical model, change is viewed as a process that consists of progress through several stages.25 It is possible that speaking to the health ambassadors, people who sometimes spoke their own language and were from their same ethnocultural group, helped to move South Asian patients along these stages in this study. A willingness to be screened, which many patients reported, suggests they were at least in a contemplative stage and perhaps even a preparatory stage. We know at least some patients went on to action and were actually screened. Time will tell if these patients will maintain screening.
There were several significant challenges to successful implementation of the health ambassador–focused quality improvement initiatives that warrant discussion. First, the initiatives were quite resource intensive, especially as this quality improvement work was additional to, not instead of, usual clinical duties. For instance, Physician #4 had very positive views of the health ambassadors but ultimately did not have the capacity to try more than one initiative in her office due to a busy clinical workload. Although the health ambassadors were volunteers and took on a good amount of the work, a considerable amount of time still needed to be spent preparing them to do their tasks, for example, training on use of electronic medical records, training on clinic procedures, preparing and finalizing privacy/confidentiality agreements, and finding workspace. Some process and outcome measures could not be tracked as neither the physicians nor the volunteers had the capacity. Having more office staff available to liaise with health ambassadors was noted to be a facilitator to initiatives. However, this suggests that family physicians practicing in settings with few office staff may have even greater difficulty initiating similar quality improvement initiatives. The participating physicians were highly motivated, and it is likely that the time and resources required would be a significant roadblock for an average, busy primary care physician.
A second and related challenge was that the health ambassadors were originally recruited and trained to include the screening messages in their day-to-day life. They were not originally required to commit specific times for the volunteer role. The health ambassadors, therefore, had other competing duties and could not visit a particular clinic more than a few hours per week. This limited the ability to reach a larger number of patients within each office. Although immediate costs are very low, the sustainability of volunteer-led initiatives is a challenge. This is particularly true when the volunteers are ultimately hoping to move on to paid work in their profession or are already working full time. We found two US studies that used lay health educators within primary care practices.31–33 In both cases, the researchers were able to pay these workers and thus were able to have much more dedicated time toward their initiatives and to provide much more intensive outreach to patients. Percac-Lima et al31 conducted a randomized trial to evaluate the impact of patient navigation for cancer screening among low-income and racial minority patients within a US primary care practice. Paid patient navigators telephoned patients in their own languages and provided intensive outreach to help with cancer screening. Patients randomized to navigation had significantly higher screening rates for breast, cervical, and colorectal cancer screening over eight months (23.4%, 14.4%, and 13.7%, respectively). Of note, despite these successes, 19% of patients could not be reached, and many declined to participate. Collinsworth et al32 embedded paid Spanish-speaking community health workers within five Texas community clinics to reduce disparities in diabetes care.32,33 The program consisted of educational sessions and clinical assessments. Patients who participated in the program had significant reductions in glycosylated hemoglobin levels and blood pressure after one year.
Third, and as noted with the Percac-Lima et al’s study, the majority of patients were not able to be reached directly by telephone.31 Telephone calls seemed to hold the most promise as a way of reaching patients in this pilot study and have been used successfully for cancer screening.34–36 However, future initiatives should strive to ensure accurate contact information at the onset, flexibility on the timing of calls so that they could be made in the evenings and/or on weekends, and should seek to address privacy issues and concerns. Health ambassadors noted that patients could be suspicious on the telephone of who they were, how they had obtained their contact information, and how they were affiliated with the physicians’ offices.
Fourth, patients expressing willingness to be screened need not necessarily equate to patients actually getting screened, and the capacity for these physicians to track screening was limited. More than 60% of South Asian patients overdue for screening reported willingness to be screened, but for three physicians’ practices, we were unable to determine how many patients actually went on to be screened. No-shows were also a noted issue for physicians. Social desirability bias might have led patients to say they were willing to be screened when that was not actually the case.37 Patients might have been willing to be screened but still may have faced barriers to actually following through with screening. In one physician’s office (#4), only 21% of patients approached in the waiting room admitted to being overdue for at least one type of screening. This was despite her overall percentages of patients overdue for screening for her practice at the onset being 43%, 47%, and 59% for breast, cervical, and colorectal cancers, respectively. Although patients coming in to the office may have been more likely to be up-to-date on screening, this finding of 21% still seemed incongruent with her experience and further suggests that social desirability bias may have been at play. Tracking actual screening uptake among individual patients was resource intensive, raised issues around data privacy, and was ultimately only feasible in one office. Although it cannot be proven that this was a direct result of the phone calls, screening uptake among telephoned patients was relatively high in that office.
Finally, we have no details about the demographics of patients who were approached. Factors such as education level, socioeconomic status, and years of stay in Canada could all affect willingness to screen and we were unable to track those variables in this study. Patients did not self-report ethnicity, which is considered the gold standard for race/ethnicity identification.38 Similar work in the future may consider a brief demographic survey for participating patients. Some primary care practices are now routinely collecting sociodemographic information from patients.39
Despite these challenges, our findings suggest that the utility of ethnoculturally specific lay health educators embedded within primary care to educate patients on screening and motivate them to be screened should be further explored, with modification. All physicians had positive views of working with the health ambassadors, three of four physicians planned to continue to work with health ambassadors, and more than 60% of South Asian patients reported a willingness to be screened. In one physician’s office, screening uptake was high after phone calls, higher than that seen in other studies involving cancer screening outreach and higher than the numbers seen in the Percac-Lima et al’s study.31,40,41 Interestingly, screening uptake was also higher than that physician had predicted after participating in the study. Future work should continue to adapt this resource-intensive initiative to maximize benefits. For example, telephoning during evening and weekend hours, providing the opportunity for patients to book an appointment on the spot, mailing out colon cancer screening kits to patients who agree, and providing reminder phone calls close to the time of appointments might be important next steps to consider.
Importantly, future work should also consider providing paid positions or having office staff take on the health ambassador role. Being able to pay lay health educators may allow for a greater time commitment, time for rigorous training, more intensive outreach, and tracking of actual screening rates. In turn, this might make this study more feasible for physicians who are not as highly motivated as our study participants were. However, this would require financial resources, which may be feasible in some large team-based models, but would be particularly challenging for physicians working in traditional fee-for-service models and smaller practices.
Conclusion
Quality improvement work within community primary care practices is hard work. Using ethnoculturally specific lay health educators within primary care practices to telephone patients in their own languages showed some promise in this study for increasing awareness about cancer screening and screening uptake. However, it was also quite time intensive and resource intensive and had numerous challenges. Future quality improvement efforts should focus on further developing the phone call invitation process, including exploring how to provide infrastructure for lay health educator training and time, and for monitoring of processes and outcomes.
Acknowledgment
This study was funded by a Canadian Cancer Society Research Institute Knowledge to Action grant.
Disclosure
Dr Lofters was supported by a Canadian Cancer Society Research Institute Career Development Award in Cancer Prevention. Dr Lofters and Dr Dunn received salary support from the University of Toronto Department of Family and Community Medicine.
The other authors report no conflicts of interest in this work.
References
Fernandes KA, Sutradhar R, Borkhoff CM, et al. Cross-sectional small area variation study of cancer, glucose, and cholesterol screening in Ontario: data to motivate community and primary care strategies to improve participation. CMAJ Open. 2015;3(4):E373–E381. | ||
Borkhoff CM, Saskin R, Rabeneck L, et al. Disparities in receipt of screening tests for cancer, diabetes and high cholesterol in Ontario, Canada: a population-based study using area-based methods. Can J Public Health. 2013;104(4):e284–e290. | ||
Vahabi M, Lofters A, Kumar M, Glazier RH. Breast cancer screening disparities among immigrant women by world region of origin: a population-based study in Ontario, Canada. Cancer Med. 2016;5(7):1670–1686. | ||
Vahabi M, Lofters A, Kumar M, Glazier RH. Breast cancer screening disparities among urban immigrants: a population-based study in Ontario, Canada. BMC Public Health. 2015;15:679. | ||
Lofters AK, Hwang SW, Moineddin R, Glazier RH. Cervical cancer screening among urban immigrants by region of origin: a population-based cohort study. Prev Med. 2010;51(6):509–516. | ||
Lofters A, Glazier RH, Agha MM, Creatore MI, Moineddin R. Inadequacy of cervical cancer screening among urban recent immigrants: a population-based study of physician and laboratory claims in Toronto, Canada. Prev Med. 2007;44(6):536–542. | ||
Guilcher SJ, Lofters A, Glazier RH, Jaglal SB, Voth J, Bayoumi AM. Level of disability, multi-morbidity and breast cancer screening: does severity matter? Prev Med. 2014;67:193–198. | ||
Lofters AK, Ng R, Lobb R. Primary care physician characteristics associated with cancer screening: a retrospective cohort study in Ontario, Canada. Cancer Med. 2015;4(2):212–223. | ||
Lofters A, Guilcher S, Glazier RH, Jaglal S, Voth J, Bayoumi AM. Screening for cervical cancer in women with disability and multimorbidity: a retrospective cohort study in Ontario, Canada. CMAJ Open. 2014;2(4):E240–E247. | ||
Lofters AK, Gozdyra P, Lobb R. Using geographic methods to inform cancer screening interventions for South Asians in Ontario, Canada. BMC Public Health. 2013;13:395. | ||
Ahmad F, Cameron JI, Stewart DE. A tailored intervention to promote breast cancer screening among South Asian immigrant women. Soc Sci Med. 2005;60(3):575–586. | ||
Vahabi M, Lofters A, Kumar M, Glazier RH. Breast cancer screening disparities among immigrant women by world region of origin: a population-based study in Ontario, Canada. Cancer Med. 2016;5(7):1670–1686. | ||
Grewal S, Bottorff JL, Balneaves LG. A Pap test screening clinic in a South Asian community of Vancouver, British Columbia: challenges to maintaining utilization. Public Health Nurs. 2004;21(5):412–418. | ||
Cancer Care Ontario. About the Ontario breast screening program. Available from: https://www.cancercare.on.ca/pcs/screening/breastscreening/OBSP/. Accessed February 9, 2016. | ||
Cancer Care Ontario. Cervical cancer screening. Available from: https://www.cancercare.on.ca/pcs/screening/cervscreening/. Accessed February 9, 2016. | ||
Cancer Care Ontario. Ontario cancer plan IV 2015–2019; [updated June 29, 2009; July 16, 2009]. Available from: http://ocp.cancercare.on.ca/cms/One.aspx?portalid=14464%pageid=14471. Accessed February 9, 2016. | ||
Lobb R, Pinto AD, Lofters A. Using concept mapping in the knowledge-to-action process to compare stakeholder opinions on barriers to use of cancer screening among South Asians. Implement Sci. 2013;8:37. | ||
Health Quality Ontario. Learning Collaborative One: An Improvement Journey for Primary Healthcare Teams. Toronto: Health Quality Ontario. Available from: http://www.hqontario.ca/Portals/0/documents/qi/qi-report-learningcollaborative1-0909-en.pdf. Accessed October 28, 2015. | ||
Health Quality Ontario. Quality improvement in health care. Available from: http://www.hqontario.ca/quality-improvement. Accessed October 28, 2015. | ||
Speroff T, O’Connor GT. Study designs for PDSA quality improvement research. Qual Manag Health Care. 2004;13(1):17–32. | ||
Plan, Do, Study, Act (PDSA): NHS Institute for Innovation and Improvement. Available from: http://www.institute.nhs.uk/quality_and_service_improvement_tools/quality_and_service_improvement_tools/plan_do_study_act.html. Accessed October 28, 2015. | ||
Health Quality Ontario. Quality improvement plans: a commitment to improving quality for the year ahead. Available from: http://www.hqontario.ca/Quality-Improvement/Quality-Improvement-Plans?_ga=1.36309600.1145155389.1336601468. Accessed February 9, 2016. | ||
PeelRegion. Who Lives in Peel Region? 2010. Available from: http://www.region.peel.on.ca/health/health-status-report/chsr/pdfs/chap4.pdf. Accessed February 9, 2016. | ||
Ministry of Health and Long-Term Care. What is the ColonCancerCheck program? [updated November 6, 2012]. Available from: https://www.cancercare.on.ca/pcs/screening/coloscreening/cccworks/. Accessed February 9, 2016. | ||
Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38–48. | ||
Schuster RJ, Terwoord NA, Tasosa J. Changing physician practice behavior to measure and improve clinical outcomes. Am J Med Qual. 2006;21(6):394–400. | ||
Baron RC, Melillo S, Rimer BK, et al; Task Force on Community Preventive Services. Intervention to increase recommendation and delivery of screening for breast, cervical, and colorectal cancers by healthcare providers a systematic review of provider reminders. Am J Prev Med. 2010;38(1):110–117. | ||
Sabatino SA, Habarta N, Baron RC, et al; Task Force on Community Preventive Services. Interventions to increase recommendation and delivery of screening for breast, cervical, and colorectal cancers by healthcare providers systematic reviews of provider assessment and feedback and provider incentives. Am J Prev Med. 2008;35(1 Suppl):S67–S74. | ||
Baron RC, Rimer BK, Breslow RA, et al; Task Force on Community Preventive Services. Client-directed interventions to increase community demand for breast, cervical, and colorectal cancer screening a systematic review. Am J Prev Med. 2008;35(1 Suppl):S34–S55. | ||
Crabtree BF, Miller WL. Doing Qualitative Research. 2nd ed. London: Sage; 1999. | ||
Percac-Lima S, Ashburner JM, Zai AH, et al. Patient navigation for comprehensive cancer screening in high-risk patients using a population-based health information technology system: a randomized clinical trial. JAMA Intern Med. 2016;176(7):930–937. | ||
Collinsworth A, Vulimiri M, Snead C, Walton J. Community health workers in primary care practice: redesigning health care delivery systems to extend and improve diabetes care in underserved populations. Health Promot Pract. 2014;15(2 Suppl):51S–61S. | ||
Collinsworth AW, Vulimiri M, Schmidt KL, Snead CA. Effectiveness of a community health worker-led diabetes self-management education program and implications for CHW involvement in care coordination strategies. Diabetes Educ. 2013;39(6):792–799. | ||
Dietrich AJ, Tobin JN, Robinson CM, et al. Telephone outreach to increase colon cancer screening in medicaid managed care organizations: a randomized controlled trial. Ann Fam Med. 2013;11(4):335–343. | ||
Fortuna RJ, Idris A, Winters P, et al. Get screened: a randomized trial of the incremental benefits of reminders, recall, and outreach on cancer screening. J Gen Intern Med. 2014;29(1):90–97. | ||
Phillips L, Hendren S, Humiston S, Winters P, Fiscella K. Improving breast and colon cancer screening rates: a comparison of letters, automated phone calls, or both. J Am Board Fam Med. 2015;28(1): 46–54. | ||
Johnson TP, O’Rourke DP, Burris JE, Warnecke RB. An investigation of the effects of social desirability on the validity of self-reports of cancer screening behaviors. Med Care. 2005;43(6):565–573. | ||
Sandefur GD, Campbell ME, Eggerling-Boeck J. Racial and ethnic identification, official classifications, and health disparities. In: Anderson NB, Bulatao RA, Cohen B, editors. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Washington, DC: National Academies Press; 2004. | ||
Pinto AD, Glattstein-Young G, Mohamed A, Bloch G, Leung FH, Glazier RH. Building a foundation to reduce health inequities: routine collection of sociodemographic data in primary care. J Am Board Fam Med. 2016;29(3):348–355. | ||
Kearins O, Walton J, O’Sullivan E, Lawrence G. Invitation management initiative to improve uptake of breast cancer screening in an urban UK Primary Care Trust. J Med Screen. 2009;16(2):81–84. | ||
Escribà-Agüir V, Rodríguez-Gómez M, Ruiz-Pérez I. Effectiveness of patient-targeted interventions to promote cancer screening among ethnic minorities: a systematic review. Cancer Epidemiol. 2016;44:22–39. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
