Back to Journals » International Medical Case Reports Journal » Volume 14
Late Dislocation of In-the-Bag Intraocular Lens in Three Patients with Multiple Chorioretinal Atrophy Associated with Sarcoidosis
Authors Ohta K, Sato A, Fukui E
Received 27 October 2020
Accepted for publication 15 December 2020
Published 16 February 2021 Volume 2021:14 Pages 95—100
DOI https://doi.org/10.2147/IMCRJ.S288270
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Kouichi Ohta, Atsuko Sato, Emi Fukui
Department of Ophthalmology, Matsumoto Dental University, Shiojiri, Nagano, Japan
Correspondence: Kouichi Ohta
Department of Ophthalmology, Matsumoto Dental University, 1780 Gobara, Hirooka, Shiojiri, Nagano, 399-0781, Japan
Tel/Fax +81-263-51-2210
Email [email protected]
Purpose: A late dislocation of an in-the-bag intraocular lens (IOL) is strongly associated with pseudoexfoliation and less with retinitis pigmentosa, prior vitreoretinal surgery, and uveitis. We present our findings of late in-the-bag IOL dislocation in three patients with multiple chorioretinal atrophy associated with sarcoidosis.
Methods: Observational study of three elderly female Japanese patients with a history of uveitis from sarcoidosis who presented with a late dislocation of an in-the-bag IOL.
Results: The late in-the-bag IOL dislocation occurred in the convalescent/quiescent stage of the sarcoidosis. Peripheral multifocal chorioretinal atrophy was the main manifestation in all patients who were diagnosed with definite or presumed sarcoidosis. The dislocated IOLs were successfully removed and new IOLs were implanted with scleral suture fixation followed by no remarkable active uveitis.
Conclusion: Clinicians should be aware that patients with peripheral multifocal chorioretinal atrophy associated with sarcoidosis can have a late in-the-bag IOL dislocation.
Keywords: late in-the-bag IOL dislocation, pigmented chorioretinal atrophy, sarcoidosis, uveitis
Introduction
Subluxation or dislocation of an in-the-bag implanted intraocular lens (IOL), an in-the -bag IOL dislocation, is an uncommon but potentially serious complication that can occur after the implantation cataract surgery. Early IOL dislocation generally is secondary to poor IOL fixation. Late dislocation, those occurring more than 3 months after cataract extraction, is a progressive condition caused by a weakening of the residual zonules after a cataract surgery.1 Two risk factors associated with a late IOL dislocation include zonular weakness and contraction of the capsular bag.1 The pseudoexfoliation syndrome is reported to be another cause of late IOL dislocation.1–3 Other risk factors include retinitis pigmentosa, prior vitrectomy, trauma, and uveitis.1–3 The incidence of late in-the-bag IOL dislocation in eyes with uveitis was reported to be 2 to 16%.1,2 In uveitis patients who had undergone cataract surgery, a late in-the-bag IOL dislocation was found in only 6 of 1056 (0.57%) eyes in one study4 and 10 of 581 (1.89%) eyes in another study.5 The majority of these eyes had intermediate uveitis.4,5
There have been a few cases of late in-the-bag IOL dislocation in eyes with sarcoidosis.1,2 However, the ocular findings in these cases of sarcoidosis were not described in detail. Thus, the purpose of this report is to present our findings in three cases of late in-the-bag IOL dislocation at the convalescent/quiescent stage of sarcoidosis. Peripheral multifocal chorioretinal atrophy was observed in all three cases.
Case Reports
Case 1
A-76-year-old Japanese woman complained of blurred vision in her left eye. She reported that she had undergone cataract surgery with an implantation of an IOL without any complications 8 years earlier. She also reported that she had been diagnosed with presumed sarcoidosis 15 years earlier in another University Hospital based on the Japanese diagnostic criteria. Although mild iritis, vitreous opacities, and peripheral multifocal chorioretinitis were present, the iritis was under control by topical steroids. She had undergone pars plana vitrectomy (PPV) with cataract surgery in an eye with mild vitreous opacities, an epiretinal membrane (ERM), and macular edema (ME) in another eye 12 years earlier. Since then, the ocular inflammation has been stable in both eyes.
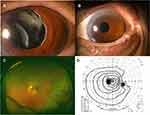
When she was referred to our hospital, her best-corrected visual acuity (BCVA) was 20/20 in the eye with the inferiorly subluxed IOL in her left eye (Figure 1A). The intraocular pressure (IOP) was 9 mmHg in the right eye and 10 mmHg in the left eye. Slit-lamp examination revealed no cells in the anterior chamber (AC). Pseudoexfoliation was not observed, but multifocal hyperpigmented chorioretinal atrophy was present in both eyes. After an increase of blurred vison to 20/25, she underwent 25-gauge pars plana vitrectomy in January 2011 during which the 3-piece acrylic IOL was displaced into a bed of intravitreal perfluorocarbon liquid (PFCL). The IOL was then removed through a 7.0-mm corneal scleral incision. A constriction of the capsule of the lens was not observed intraoperatively. A fornix-based conjunctival peritomy was made at 270 degrees followed by the construction of a partial thickness triangular limbal based scleral flaps 180 degrees apart. Then, a one-piece P336UV (Bausch and Lomb, Rochester, NY) was placed in the posterior chamber (PC) using the ab externo method6 with PAIR-PAKTM needles (Alcon Laboratory). Then, 10–0 polypropylene sutures were passed through the haptic eyelets and sutured to the sclera. The suture knots were buried under the scleral flaps, and scleral flaps were sutured with 8–0 vicryl sutures to avoid suture-related complications. Thereafter, the IOL was stable with minimal cells in the AC, and the BCVA has remained between 20/20 to 20/16 for 8 years (Figure 1B). Confluent pigmented chorioretinal atrophy was clearly observed postoperatively (Figure 1C). The visual field was constricted (Figure 1D).
Case 2
A-76-year old Japanese woman complained of blurred vision in her right eye. She had undergone cataract surgery with an IOL implantation without any complications 12 years earlier. She had also undergone PPV for an ERM and ME in both eyes 8 years earlier. She was diagnosed with sarcoidosis approximately 15 years earlier in another general hospital by a skin biopsy. Oral prednisolone (dose unknown) had been initially prescribed for the vitreous opacities and ME. After the PPV, the uveitis was controlled by topical steroids.
Her BCVA was 20/25, when she was referred to our hospital in March 2015. The IOP was 13 mmHg and 11 mmHg in the right and left eyes, respectively. Slit-lamp examination revealed no cells in the AC, but a superior subluxation of an in-the-bag IOL was detected (Figure 2A). No pseudoexfoliation or vitreous opacities were present, and pigmented chorioretinal atrophy was found in the peripheary. The foveal ellipsoid zone (EZ) was disrupted in the optical coherent tomographic (OCT) images.
She underwent 27-gauge PPV in May 2015. The dislocated 3-piece acrylic IOL was displaced into a pool of PFCL and cut into 3 pieces. The pieces were removed through a 3.5-mm corneal scleral incision. A foldable acrylic IOL (VA-70 AD, HOYA, Tokyo, Japan) was inserted and suture-fixed to the sclera with the ab externo technique as in Case 1. Although the PC-IOL was stable (Figure 2B) and the BCVA improved to 20/20 after the surgery, the BCVA decreased to the baseline value at 4 years due to mild macular chorioretinal atrophy. Peripheral pigmented chorioretinal atrophy and mild macular degeneration were clearly observed after the surgery (Figure 2C). A peripheral hypofluorescent lesion was also observed in the fundus autofluorescence images which corresponded with the pigmented lesion (Figure 2D).
Case 3
A-77-year old woman complained of blurred vision in her left eye. She had undergone cataract surgery with implantation of an IOL 13 years earlier without any complications. She had been diagnosed with presumed sarcoidosis about 15 years earlier, and the mild iritis had been controlled by steroid eyedrops.
Her BCVA at presentation was 20/30 in the left eyes. The IOP was 15 mmHg and 14 mmHg in the right and left eyes, respectively. Slit-lamp examination revealed no cells in the anterior chamber, but a nasally dislocated in-the-bag IOL was detected (Figure 3A). Slit-lamp examination showed no pseudoexfoliation or vitreous opacities, and ophthalmoscopy showed pigmented chorioretinal atrophy in the periphery. The subfoveal EZ was disrupted in the OCT images.
She underwent 27-gauge PPV and the one piece in-the bag PMMA IOL was removed through a 7.5-mm corneal scleral incision without PFCL in September 2017. A CZ70BD IOL (Alcon, Texas, USA) was implanted and fixed with scleral sutures as in the other cases. Thereafter, the PC-IOL was stable (Figure 3B), and the BCVA has remained 20/30 for 2 years without obvious signs of iritis. The peripheral pigmented chorioretinal atrophy and mild macular degeneration could be clearly observed after the surgery (Figure 3C). The visual field was constricted due to the chorioretinal atrophy (Figure 3D).
Discussion
Intraocular lens dislocations of implanted IOLs are a serious complication. An early dislocation generally occurs secondary to poor fixation. In contrast, late in-the-bag IOL dislocations that occur >3 months after the cataract surgery are usually due to weakness of the zonular fibers.1–3 This weakness has been associated with pseudoexfoliation, retinitis pigmentosa, prior vitreoretinal surgery, trauma, high myopia, and uveitis.1–3 Although uveitis is one of the possible disorders associated with late in-the-bag IOL dislocation, it has a low incidence of 2 to 16%.1–3
In relatively large studies, 6 of 1056 patients with uveitis (0.57%)4 and 11 of 581 patients (1.89%)5 that underwent cataract surgery were reported to have a late dislocation of the IOL. Fuchs’ heterochronic uveitis, multifocal choroiditis, birdshot retinochoroiditis, chronic intermediate, chronic idiopathic pan uveitis, and sympathetic ophthalmitis were diagnosed in 6 of the 1056 patients who had an IOL dislocation.4 On the other hand, all 11 of the patients with intermediate uveitis had a dislocation.5 In another study, multifocal choroiditis was present in 2 of 5 uveitis patients with a late IOL dislocation.7
Our findings demonstrated that a late dislocation of an in-the-bag IOL can occur in female patients diagnosed with sarcoidosis. The ocular inflammation was detected as peripheral multifocal chorioretinal atrophy. Although all three patients were not examined in our hospital initially, the main findings at the active stage was reported to be peripheral multifocal chorioretinitis, mild vitreous opacities, mild ERM, and macular edema in Cases 1 and 2. Unfortunately, a complete record of the prior findings could not be obtained. In all cases, the ocular inflammation remained stable after the cataract surgery.
To the best of our knowledge, this is the first report describing a late dislocation of an in-the-bag IOL in patients with sarcoidosis with multifocal chorioretinal atrophy. Although IOL dislocations in patients with sarcoidosis have been reported, the ocular findings were not presented.1,2
Peripheral multifocal chorioretinitis has been reported to be associated with sarcoidosis in 39%8 to 47%9 of the examined eyes. In addition, the prevalence of multiple chorioretinal peripheral lesions is higher in Japan (57%) than other countries (45%).10 The majority of the patients have been elderly women, and the major complication was macular edema.8–10 Macular edema also occurred at the active stage in our Cases 1 and 2. Overall, it might have been expected that late in-the-bag IOL dislocation would occur in our patients associated with multifocal chorioretinal atrophy4,7 rather than with sarcoidosis. The chorioretinal atrophy in our cases were associated with sarcoidosis which frequently occurs in Japanese individuals.10
Because an extreme degree of capsular constriction was not observed, we suggest that a zonular weakness, one of the proposed mechanisms for in-the-bag IOL dislocation, was the mechanism in our cases.1–5,7 Jones et al discussed zonular damage during chronic uveitis, and they suggested that a weakening of the core fibrillin and subsequent dehiscence by enzymatic damage of collagen IV, an essential component of ligament, were the cause of the dislocations.11
Other possible mechanisms for the IOL dislocation should be considered for our cases. First, prior vitrectomy may be a possible cause in Case 2 although there were no complications during the surgery. Second, aging is a major factor for IOL dislocations. The cumulative incidence of late lens dislocation is 0.1% to 1.0% in the 10 years after surgery.12,13 In our small series, there was no convincing evidence for an association between the late in-the-bag IOL dislocation and peripheral chorioretinal atrophy and with the sarcoidosis. However, the possibility of zonular damage during chronic peripheral chorioretinal inflammation associated with sarcoidosis is not excluded.
Although the exact mechanism for the IOL dislocation was not established in our cases, there were no postoperative complications, no further ME, or significant worsening of the uveitis. The sclera-sutured PC-IOL has remained stable after 8 (Case 1), 4 (Case 2), and 2 (Case 3) years after the surgery.
In conclusion, we suggest that patients with peripheral multifocal chorioretinal atrophy associated with sarcoidosis may have a risk of late in-the-bag IOL dislocation even in the convalescent stage of uveitis. However, the visual prognosis is fair to good after successfully removal and replacement of the IOL.
Statement of Ethics
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Ethics Approval and Consent to Participate
Ethics approval was obtained from the Institutional Ethics Committee at the Matsumoto Dental University, Shiojiri, Japan. A written informed consent was obtained from all the patients for publication of this case series and any accompanying images.
Acknowledgments
We thank Professor Emeritus. Duco Hamasaki of the Bascom Palmer Eye Institute for discussions and editing the manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors have no funding source to declare.
Disclosure
The authors have no conflicts of interest to declare.
References
1. Gross JG, Kokame GT, Weinberg DV. In-the-bag intraocular dislocation. Am J Ophthalmol. 2004;137:630–635. doi:10.1016/j.ajo.2003.10.037
2. Gimbel HV, Condon GP, Kohnen T, Olson RJ, Halkiadakis I. Late in-the-bag intraocular lens dislocation: incidence, prevention, and management. J Cataract Refract Surg. 2005;31:2193–2204. doi:10.1016/j.jcrs.2005.06.053
3. Davis D, Brubaker J, Espander L, et al. Late in-the-bag spontaneous intraocular lens dislocation. Evaluation of 86 consecutive cases. Ophthalmology. 2009;116:664–670. doi:10.1016/j.ophtha.2008.11.018
4. Steeples LR, Jones NP. Late in-the bag intraocular lens dislocation inpatients with uveitis. Br J Ophthalmol. 2015;99:1206–1210. doi:10.1136/bjophthalmol-2014-306437
5. Ganesh SK, Sharma HR. Late dislocation of in-the-bag intraocular lenses in uveitic eyes: an analysis of management and complication. Indian J Ophthalmol. 2017;65:148–154. doi:10.4103/ijo.IJO_938_16
6. Lewis JS. Ab externo sulcus fixation. Ophthalmic Surg. 1991;22:692–695.
7. Tao LW, Hall A. In-bag dislocation of intraocular lens in patients with uveitis: a case series. J Ophthalmic Inflamm Infect. 2015;5:10. doi:10.1186/s12348-015-0036-1
8. Ossewaarde-van Norel J, Ten Dam-van Loon N, De Boer JH, Rothova A. Long-term visual prognosis of peripheral multifocal chorioretinitis. Am J Ophthalmol. 2015;159:690–697. doi:10.1016/j.ajo.2015.01.005
9. Koop A, Ossewaarde A, Rothova A. Peripheral multifocal chorioretinitis. Acta Ophthalmol. 2013;91:492–497. doi:10.1111/j.1755-3768.2012.02483.x
10. Acharya NR, Browne EN, Rao N, Mochizuki M. Distinguishing features of ocular sarcoidosis in an international cohort of uveitis patients. Ophthalmology. 2018;125:119–126. doi:10.1016/j.ophtha.2017.07.006
11. Jones NP, Jalil A, Steeples LR. Management of subluxed and dislocated intraocular lenses in patients with uveitis: a practical approach. Ocul Immunol Inflamm. 2020;91–96. doi:10.1080/09273948.2020.1764592
12. Monestam EI. Incidence of dislocation of intraocular lenses and pseudophakodonesis 10 years after cataract surgery. Ophthalmology. 2009;116:2315–2320. doi:10.1016/j.ophtha.2009.05.015
13. Pueringer SL, Hodge DO, Erie JC. Risk of late intraocular lens dislocation after cataract surgery, 1980–2009: a population-based study. Am J Ophthalmol. 2011;152:618–623. doi:10.1016/j.ajo.2011.03.009
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.