Back to Journals » Clinical Optometry » Volume 12
Knowledge of Childhood Blindness and Associated Factors Among Parents or Guardians in Maksegnit Town, Northwest Ethiopia
Authors Assefa NL , Tolessa KG, Ferede AT
Received 1 August 2020
Accepted for publication 23 September 2020
Published 9 October 2020 Volume 2020:12 Pages 175—182
DOI https://doi.org/10.2147/OPTO.S275071
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Mr Simon Berry
Natnael Lakachew Assefa, Kalkidan Getahun Tolessa, Ayanaw Tsega Ferede
Department of Optometry, School of Medicine, College of Medicine and Health Sciences and Comprehensive Specialized Hospital, University of Gondar, Gondar, Ethiopia
Correspondence: Natnael Lakachew Assefa
University of Gondar, PO Box 196, Gondar, Ethiopia
Tel +251-9-10-08-89-03
Email [email protected]
Introduction: Childhood blindness is defined as a group of eye diseases occurring in childhood or early adolescence. Good parental knowledge of childhood blindness is important for early detection and management of the lifelong burden.
Purpose: This study aimed to assess knowledge of childhood blindness and associated factors among parents or guardians.
Materials and Methods: A community-based cross-sectional study was conducted. Systematic random sampling was used to select the study participants. Data were collected by interview using a pre-tested semi-structured questionnaire. The collected data were analyzed by SPSS version 20. Multivariate logistic regression was used to identify the determinant factors, and p-values less than 0.05 were considered as statistically significant.
Results: A total of 524 participants were enrolled in the study, with a 98.49% response rate. The proportion of good knowledge of childhood blindness was 39.1% (95% CI: 34.9– 43.3%). Being male (AOR=2.32, 95% CI: 1.4– 3.87), higher educational status (AOR=6.47, 95% CI: 2.4– 17.3), knowing where the child eye care center is (AOR=2.68, 95% CI: 1.5– 4.7) and participation in eye care campaigns (AOR=1.95, 95% CI: 1.26– 3.0) had statistically significant associations with knowledge of childhood blindness.
Conclusion: Less than half of the study participants had good knowledge about childhood blindness. Being male, having higher educational status, knowing about the child eye care center and participation in eye care campaigns were positively associated with knowledge of childhood blindness.
Keywords: childhood blindness, knowledge, Maksegnit, Ethiopia
Introduction
The World Health Organization (WHO) refers to childhood blindness as
a group of eye diseases occurring in childhood or early adolescence, which (if left untreated) may result in severe visual impairment or blindness that is likely to be untreatable later in life.1,2
It can also be defined as best corrected visual acuity in the better eye of less than 3/60 in those less than 16 years of age.3 Globally, childhood blindness accounts for 4% of cases of blindness and 1% of visual impairment.4 Based on the WHO 2017 report, childhood blindness was estimated at 1.14 million across the world, with more than 80% of these children living in developing countries.5 The prevalence of blindness in children varies with the socio-economic level of countries, ranging from 0.3 to 1.5 per 1000 in high-income and low-income countries, respectively.6,7 In Ethiopia, childhood blindness is estimated at 0.1–6% of the total cases of blindness.8
Globally, there is a wide variation in the causes of childhood blindness, based on the income level of the society, and more than 75% of these causes are avoidable.9,10 The common causes associated with childhood blindness in the poorest countries of Africa are corneal scarring due to vitamin A deficiency, measles infection, ophthalmia neonatorum and the use of harmful traditional eye remedies, which account for 47% of cases of blindness. Retinopathy of prematurity, non-preventable hereditary eye disease and cortical blindness are common in middle- and high-income countries.9,11 In all the WHO regions, corneal opacity, cataract and retinopathy of prematurity are the leading causes of visual impairment and childhood blindness.6 A study conducted in Ethiopia reported that refractive error was the leading cause of childhood blindness.12
Childhood blindness has a great impact at the individual level, with a negative effect on personal development and educational performance, placing an economic burden on the family and the country at large.6,13 According to the primary health care strategy of the WHO, the first aim is health promotion by providing health education targeting mothers and women of child-bearing age, teachers, and religious and community leaders.7 Adequate early childhood interventions are essential for detecting eye health problems in children and providing timely treatment to prevent the consequence of development of amblyopia and irreversible lifelong blindness.6,14
In most of the initiatives aiming to prevent childhood blindness, information regarding the knowledge held by parents and care givers about childhood blindness is essential.15 Since children, especially preverbal ones, cannot complain of poor vision, it is up to the parents and care givers to detect it and ensure that children receive the help they need.14
Studies conducted in developing countries report that the proportion of good knowledge of childhood blindness was 23% in Ghana,15 43.9% in Swaziland16 and 28.1% in Ethiopia.17 Studies report that many factors affect people’s knowledge of childhood blindness. Higher educational status,3,18 age,19 media exposure and knowledge of a child eye care center17,19 were significant factors associated with good knowledge of childhood blindness.
Even though childhood blindness is considered a priority in the WHO initiative of “VISION 2020: The Right to Sight”, there have been limited studies conducted regarding childhood blindness in the study area. By considering the critical role of parents and care givers in the early detection of childhood blindness, studies should be conducted to assess the level of knowledge of childhood blindness. Therefore, the aim of this study was to estimate the level of parents’ or guardians’ knowledge of childhood blindness. The results may be beneficial to health authorities to enable them to plan strategies for the prevention of childhood blindness in Ethiopia.
Materials and Methods
Study Setting, Design and Sampling
A community-based cross-sectional study was conducted in Maksegnit town. Maksegnit town is located in North Gondar, Amhara Regional State, 40 km from Gondar town, Ethiopia. It has a total population of 11,444 (5544 males and 5900 females) living in 3580 households. There is only one health center in the town, but there are no allied eye care professionals (2007 unpublished data from Maksegnit town health extension workers’ monthly vital statistics). All parents or guardians had lived in the town for at least 6 months and had at least one child under 16 years.
Sample size was determined with the single population proportion formula:  (n=sample size, Z=value of the z statistic at 95% confidence level=1.96, P=proportion of good knowledge 28.1% =0.28117, d=maximum tolerable error (marginal error) 4%=0.04, n=485). By adding a 10% non-response rate, the final sample size was estimated at 532. A systematic random sampling method was employed to select the households using an interval of constant (k=7, where k was calculated as the total households [3580] divided by the sample size [532]).
(n=sample size, Z=value of the z statistic at 95% confidence level=1.96, P=proportion of good knowledge 28.1% =0.28117, d=maximum tolerable error (marginal error) 4%=0.04, n=485). By adding a 10% non-response rate, the final sample size was estimated at 532. A systematic random sampling method was employed to select the households using an interval of constant (k=7, where k was calculated as the total households [3580] divided by the sample size [532]).
After selecting the first household with the lottery method among the first seven houses, the next house was selected by adding 7. If the first selected household did not have children, the next immediate household was selected, and the sampling fraction was added to find the next household. If more than one eligible parent or guardians was found in the selected household, a lottery method was used to recruit the sample.
Definition of Knowledge
Knowledge
Knowledge was assessed by asking 14 questions (five questions about the causes of childhood blindness, sixquestions about prevention of childhood blindness and three questions about treatment of childhood blindness) (Table 1).Correct answers were given a score of 1 and incorrect answers a score of 0. The median was calculated from the total score, which was 12. Participants with a score on or above the median on the knowledge questions were said to have a good knowledge, while those with a score below the medianhad a poor knowledge.
 |
Table 1 Proportion of Knowledge of Causes, Prevention and Treatment of Childhood Blindness Among Parents or Guardians in Maksegnit Town (n=524, n=Sample Size) |
Participation in Eye Care Campaign
Study participants who had participated at least once in any eye care community outreach service by either organizing or providing other services in the campaign were counted as having participated in an eye care campaign.
Data Collection Procedures
Data were collected using a pretested structured questionnaire through a face-to-face interview with the parent or guardian which contained socio-demographic factors and knowledge-related questions. The questionnaire was checked for reliability using a reliability test, with a Cronbach’s alpha value of 71%.
Statistical Analysis
All the collected data were entered, coded and cleaned in Epi Info 7 and then exported to SPSS version 20 and analyzed. Descriptive results were presented as frequencies, percentages, charts, tables, graphs and summary statistics. A binary logistic regression model was used to determine associations between visual impairment and independent variables. A multivariable binary logistic regression model was used to determine the factors adjusted for potential confounders. The adjusted odds ratio (AOR) and 95% confidence interval (CI) were used to show the strength of associations. Model fitness was checked by the Hosmer and Lemeshow goodness-of-fit test. Multicollinearity was checked by the variable inflation factor (VIF), which was less than 10 (all values were less than 1.84) and the tolerance was greater than 0.1 (all values were greater than 0.54). Finally, those factors with a p-value of less than 0.05 were considered as statistically significant.
Results
Socio-Demographic Characteristics of the Study Population
A total of 524 participants were enrolled in the study, with a 98.49% response rate. The median age of participants was 35 years (interquartile range: 30–41 years). Among the study participants, 328 (62.6%) were female; and 130 (28.2%) of the study participants were unable to read and write (Table 2).
 |
Table 2 Socio-Demographic and Socio-Economic Characteristics of the Study Participants in Maksegnit Town, Northwest Ethiopia (n=524, n=Sample Size) |
Ocular Examination-Related Characteristics of Study Participants
Among the study participants, 416 (79.4%) did not know where the child eye care center was and 276 (52.7%) had participated in an eye care campaign (Table 3).
 |
Table 3 Ocular Examination-Related Characteristics of Study Participants in Maksegnit Town, Northwest Ethiopia (n=524, n=Sample Size) |
Knowledge of Study Participants About Childhood Blindness
Among the study participants, 205 (39.1%; 95% CI: 34.9–43.3%) had a good knowledge of childhood blindness (Figure 1).
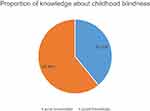 |
Figure 1 Knowledge of study participants of childhood blindness in Maksegnit town, northwest Ethiopia (n=524, n=sample size). |
Furthermore, 173 (33%) knew that glaucoma is a cause of childhood blindness and 199 (38) knew that facial cleanliness prevents childhood blindness (Table 1).
Factors Associated with Knowledge of Study Participants About Childhood Blindness
In multivariable analysis, being male, educational status, knowing where the childeye care center was and participation in an eye care campaign had statistically significant associations with knowledge of childhood blindness. Males were two times more likely to have a good knowledge of childhood blindness than females. Participants with an educational status of college or above were six times more likely to have a good knowledge of childhood blindness compared to those who were unable to read and write. Parents or guardians who knew where the child eye care center was three times more likely to have a good knowledge of childhood blindness than those who did not know where the child eye care center was. Participants who had participated in an eye care campaign were two times more likely to have a good knowledge of childhood blindness than those who had not participated (Table 4).
 |
Table 4 Factors Associated with Knowledge of Childhood Blindness Among Parents or Guardians in Maksegnit Town, Northwest Ethiopia (n=524, n=Sample Size) |
Discussion
The proportion of good knowledge of childhood blindness in this study was 39.1% (95% CI: 34.9–43.3%), which is higher than in other studies performed in Gondar rural districts (28.1%),17 in South Darfur state of Sudan (11.9%)20 and in rural Ghana (23%).15 The discrepancy between these studies and the present study may be due to the study participants’ educational status and residence. Half of the study participants (48.1%) in the study in Gondar rural districts were unable to read and write17 whereas in this study only 24.8% of the study participants were unable to read and write.15 Participants in the studies in Gondar rural district and rural Ghana were rural residents, while the present study participants were urban residents. In both situations, urban residents may have access to better information than rural residents, which may be the reason why they had good knowledge of childhood blindness.
The proportion of good knowledge of childhood blindness in this study was lower than that reported in other studies from Ghana (76%)3 and India (78%).21 One possible reason for this difference may be that the study settings for the previous studies being hospital based, whereas the current study was community based. Participants who visit the hospital may have a good opportunity to access health professionals and obtain information about childhood blindness compared to participants in studies conducted at the community level.
The proportion of good knowledge of childhood blindness in this study was in line with other studies in Swaziland (43%)16 and Honduras (43%).22
In this study, being male was positively associated with good knowledge of childhood blindness, which was similar to the findings of other studies carried out in Ghana,15 Nigeria23 and Nepal.19 This may be due to the higher educational level observed in males and it may also be attributable to the working condition of males, which involves more social interaction. In addition, women are more likely to have less disposable income, which may result in less opportunity for visiting health services, which provide information on childhood blindness from health professionals.
Participants who had an educational status of college or above were positively associated with a good knowledge of childhood blindness, which was supported by studies conducted in Ghana,3 Gondar rural districts17 and Nepal.19 This may be because of educated parents being more likely to seek health facilities, thus obtaining information regarding childhood blindness from qualified personnel.
Participants who knew where the children’s eye care center was were positively associated with a good knowledge of childhood blindness, which was supported by other studies from Gondar rural districts17 and Nigeria.23 This may be due to those parents or guardians who know where the children’s eye care is located having a better practice of taking children to the eye clinics and receiving information from eye care practitioners.
Participation in eye care campaigns was positively associated with a good knowledge of childhood blindness. This association could be attributed to the study participants receiving health information from the professionals whom they encounter at their outreach visits.
This study may have some inherent limitations due to the cross-sectional study design and information bias due to the tools that were used to collect data on participation in an eye care campaign, meaning that subjects had participated at least once in any eye care community outreach service by either organized or other direct services.
Conclusion
Less than half of the study participants had good knowledge of childhood blindness. Being male, having higher educational status, knowledge of where the child eye care center is, and having participated in an eye care campaign were positively associated with knowledge of childhood blindness.
Data Sharing Statement
All the data supporting the findings are contained within the manuscript.
Ethics Approval and Informed Consent
Ethical approval was obtained from the Institutional Review Board (IRB) of University of Gondar, College of Medicine and Health Sciences, in accordance with the Declaration of Helsinki. A written letter of permission was obtained from Maksegnit town Administrative Office. Because the data were collected only by an interviewer-administrated questionnaire, verbal informed consent was obtained from each of the study participants. All study participants were informed about the purpose of the study, and their right to refuse and withdraw from the study at any time. Confidentiality was also maintained through an anonymous questionnaire by excluding identifiers and using codes. Moreover, personal data were secured by storing data in a password-protected computer not used by others, and the questionnaires were put in a locked cabinet.
Acknowledgments
We are deeply indebted to the University of Gondar, College of Medicine and Health Sciences for granting us ethical approval to conduct this research. We would also like to acknowledge the study participants for their cooperation and willingness during data collection.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Disclosure
All authors declare no potential conflict of interest with respect to the research, authorship, or publication of this article.
References
1. WHO. Blindness and vision impairment prevention. Priority eye diseases; 2018.
2. Ebeigbe JA, Emedike CM. Parents’ awareness and perception of children’s eye disease in Nigeria. J Optom. 2017;10(2):104–110. doi:10.1016/j.optom.2016.06.001
3. Kumah B, Abdulkabir M, Kobia-Acquah E, Amponsah M, Ablordeppey R. Knowledge of childhood blindness among mothers visiting a children’s Hospital in the Kumasi Metropolis, Ghana. Adv Ophthalmol Vis Syst. 2017;7(3):00221.
4. Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96(5):614–618. doi:10.1136/bjophthalmol-2011-300539
5. Gilbert C, Bowman R, Malik A. The epidemiology of blindness in children: changing priorities. Community Eye Health. 2017;30(100):74–77.
6. Borrel A, Dabideen R, Mekonen Y, Overland L. Child eye health in Africa. The status and way forward. The African Child Policy Forum Cape Town, South Africa: ORBIS Africa; 2013.
7. Durnian J, Cheeseman R, Kumar A, Raja V, Newman W, Chandna A. Childhood sight impairment: a 10-year picture. Eye. 2010;24(1):112. doi:10.1038/eye.2009.32
8. Berhane Y, Worku A, Bejiga A, Adamu L, Alemayehu W, Bedri A. Prevalence and causes of blindness and low vision in Ethiopia. Ethiop J Health Dev. 2007;21(3):204–210.
9. Steinkuller PG, Gilbert C, Foster A, Collins ML, Coats DK. Childhood blindness. J AAPOS. 1999;3(1):26–32. doi:10.1016/S1091-8531(99)70091-1
10. Balarabe AH, Hassan R, Fatai OO. Eye health seeking habits and barriers to accessing curative services among blind beggars in an urban community in Northern Nigeria. Ann Afr Med. 2014;13(4):184. doi:10.4103/1596-3519.142289
11. Gilbert C, Foster A. Childhood blindness in the context of VISION 2020: the right to sight. Bull World Health Organ. 2001;79:227–232.
12. Yared AW, Belaynew WT, Destaye S, Ayanaw T, Zelalem E. Prevalence of refractive errors among school children in Gondar town, northwest Ethiopia. Middle East Afr J Ophthalmol. 2012;19(4):372. doi:10.4103/0974-9233.102742
13. Scheiman M, Amos C, Ciner E. Pediatric eye and vision examinations. Optometric clinical practice guideline; 2002:1–57.
14. Courtright P, Hutchinson AK, Lewallen S. Visual impairment in children in middle and lower income countries. Arch Dis Child. 2011;96(12):1129–1134. doi:10.1136/archdischild-2011-300093
15. Rami D, Pulisetty T. Maternal and care giver perception to childhood eye care in Ghana. Int J Epidemiol. 2013;11(1).
16. Sukat VN, Moodley VR, Mashige KP. Knowledge and practices of parents about child eye health care in the public sector in Swaziland. Afr J Prim Health Care Fam Med. 2018;10(1):1–3.
17. Zeleke BM, Taye BW, Ayele TA, Wolde YA. Knowledge and practice on childhood blindness among communities in Northwest Ethiopia: implications to blindness prevention programs. JOECSA. 2013;17(2):2–21.
18. Muhit MA, Shahjahan M, Hassan A, Wazed A, Ahmed N. Parental knowledge, attitude and practice related to blindness of children in some selected Upazilla of Bangladesh. Mymensingh Med J. 2011;20(4):671–679.
19. Shrestha MK, Guo CW, Maharjan N, Gurung R, Ruit S. Health literacy of common ocular diseases in Nepal. BMC Ophthalmol. 2014;14(1):2. doi:10.1186/1471-2415-14-2
20. Alrasheed SH, Naidoo KS, ClarkeFarr PC. Childhood eye care services in South Darfur State of Sudan: learner and parent perspectives. Afr Vision Eye Health. 2016;75(1):1–3.
21. Paranjpe R, Mushtaq I, Thakre A, Sharma A, Dutta D, Iqbal B. Awareness of childhood blindness in parents attending paediatrics ophthalmology outpatient department. Med J DY Patil Univ. 2016;9(4):451–454. doi:10.4103/0975-2870.186057
22. Ramai D, Elliott R, Goldin S, Pulisetty. T. A cross-sectional study of pediatric eye care perception in Ghana, Honduras and India. J Epidemiol Glob Health. 2014;5(2):133–142. doi:10.1016/j.jegh.2014.06.004
23. Amiebenomo O, Achugwo D, Abah I. Parental knowledge and attitude to children’s eye care services. Niger J Paediatr. 2016;43(3):215–220. doi:10.4314/njp.v43i3.11
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
