Back to Journals » Open Access Journal of Contraception » Volume 6
Knowledge, non-use, use and source of information on contraceptive methods among women in various stages of reproductive age in rural Lagos, Southwest Nigeria
Authors Afolabi BM, Ezedinachi E, Arikpo I, Ogunwale A, Ganiyu DF, Abu R, Ajibade A
Received 9 January 2015
Accepted for publication 23 February 2015
Published 20 May 2015 Volume 2015:6 Pages 65—75
DOI https://doi.org/10.2147/OAJC.S80683
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Igal Wolman
Video abstract presented by Bamgboye M Afolabi
Views: 1130
Bamgboye M Afolabi,1 Emmanuel NU Ezedinachi,2 Iwara Arikpo,2 Abiodun Ogunwale,3 Damilola Fatimah Ganiyu,1 Rashidat A Abu,1 Adewunmi A Ajibade1
1Health, Environment and Development Foundation, Yaba, Lagos, Nigeria; 2Institute of Tropical Disease and Research, University of Calabar, Calabar, Nigeria; 3Project Hope, Washington, DC, USA
Background: Contraceptives are advocated to be used against unwanted pregnancy and sexually transmitted diseases as unsafe abortion contributes to high maternal mortality in Nigeria while unwanted pregnancies have terminated the educational development of many females.
Objective: This questionnaire-based survey aimed to describe the knowledge, nonuse, and use of various contraceptive methods among women in different child-bearing age groups in rural Lagos, Nigeria.
Materials and methods: Between 2012 and 2013, 816 females in rural communities within Lagos State were surveyed for their knowledge, source of information, and use of contraceptives. They were grouped into early, mid, and late reproductive age. Statistical analysis of data harvested from respondents was carried out using STATA 13 software.
Results: In all, 816 females in different stages of reproductive age were involved in the study, among whom 19% were single, 78% married, 3% divorced, and 0.5% widowed. About 6% had no formal education, while the majority (81%) were of the Yoruba ethnic group. Married respondents were approximately thrice more likely to know of contraceptives than single respondents (χ2=29.9, P=0.000, odds ratio =2.9, 95% confidence interval =1.9, 4.2). Condom use was the most widely known and used method of contraceptive regardless of marital status and reproductive age status. Information about contraceptives was mainly from health facilities among married and divorced women and from school or educational institution among singles. Overall prevalence of contraceptive use was 51.9%. Nonuse of contraceptives was 43% among married women and 67% among singles. Knowledge of contraceptive method was negatively associated with marital status (t=-2.24, P=0.025) but positively associated with source of information on contraceptives (t=20.00, P=0.000). Use of contraceptives was positively associated with stage of reproductive age (t=1.94, P=0.05) and source of information on contraceptives (t=11.22, P=0.000), but negatively associated with marital status (t=-2.79, P=0.005) and religious belief (t=-1.89, P=0.05).
Conclusion: Knowledge and use or nonuse of contraceptives could be pivotal in designing adequate prenatal care to prevent unwanted pregnancy and consequently illegal abortion or possible adverse pregnancy outcomes such as low birth weight, preterm birth, and conditions such as small for gestational age. Data from this study can also be used to design penetrating health education on making pregnancy safer or living a healthy female reproductive life.
Keywords: knowledge, nonuse, use, source of information, contraceptive methods, reproductive age, rural Lagos, Nigeria
Introduction
Putting an end to the silent pandemic of unsafe abortion is an urgent public-health and human-rights imperative. Probably due to lack of access to safe and effective contraceptive use, unsafe abortion threatens women throughout the developing world. Every year, about 19–20 million abortions are done by individuals without the requisite skills or in environments below minimum medical standards, or both, leading to unsafe abortion, mostly (97%) in developing nations.1 Over 200 million women of reproductive age would prefer to defer subsequent pregnancy or permanently prevent pregnancy, after having enough children, though the majority of them still depend on traditional methods of contraceptives or are not using any contraceptives at all.2 The unreliability, in certain instances, of the traditional/calendar method of contraceptive often results in unwanted pregnancy and either legal or illegal abortion with unpleasant consequences. Women may not use any contraceptive method to prevent unwanted pregnancy because they have no access or they confront various barriers such as “lack of awareness, lack of access, cultural factors, religion, opposition to use and fear of health risks and side effects of contraceptives”.3
The World Health Organization (WHO) refers to safe, legal abortion as a “fundamental right of women, irrespective of where they live”.1 Goal 5 of the Millennium Development Goals – Improving Maternal Health – aimed to achieve global access to reproductive health by 2015.4 In the past decade, progress has been recorded or statistics remained stable in contraceptive prevalence rate, adolescent birth rate, antenatal care coverage, and unmet need for family planning in developed countries, though Sub-Saharan Africa, the part of the world with the poorest reproductive health indices, did not achieve improvements in most, if not all, of these indicators.4 The United Nations agreed that contraceptive prevalence rate should be one of the indicators to be monitored for worldwide progress toward achieving global access to reproductive health.5 Within the same period, approximately 55% of women had no access to adequate antenatal care, while 24% did not have access to family planning services.6
Meanwhile, sexual health is described as “a state of physical, emotional, mental and social well-being in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity”.7 One of the most important but often overlooked themes in the WHO’s definition of health is that females and males, at appropriate age, have the ability to be in charge of their own fulfilling and harmless sex life; the capability to reproduce; and, most important of all, the liberty and sovereignty to choose if, when, and at what frequency to have safe sex.8 Both men and women therefore need to gain information about and access to safe, effective, affordable, and acceptable methods of birth control. Worldwide, contraceptive use is higher and women have fewer children where family planning services are more widely available. Will reports that rates of contraceptive use in the world are highest in China (84.6%) among women who are currently married or in union, compared to the United States (78.6%) and Japan, with 54.3% prevalence. Toward the end of the last decade (2009), about 13 million abortions were performed in China, 62% of which were among women aged 20–29 years while most were single.9 Pills, tubal ligation, and condoms are the most widely used methods of contraceptives among American women, with sterilization more prominent among Black Americans and Hispanics and pills among White American women.10
For many decades now, decline has been observed by demographers concerning fertility rates in Asia and Latin America, though there is uncertainty about fertility rates in Sub-Saharan Africa.11 The high fertility rates prevailing in Sub-Saharan Africa reflect demand for children: a demand premised on the costs and benefits associated with the birth of additional children versus the cost of preventing a birth.12 In 2012, 2.8 million women in Tanzania used modern contraceptive methods, thus preventing 120,000 un safe abortions.13 In Kenya, condoms (35%), pills (33%), injection (19%), and intrauterine contraceptive devices (IUDs) (4%) are the most commonly used contraceptive methods.14 In Nigeria, contraceptive use has increased slightly, from 3.5% among married women within the age bracket 15–49 years using modern contraceptive methods in 1990, to 8.2% in 2003, and 9.7% in 2009.15 Studies have shown that many women with unwanted pregnancies resolve to terminate them by abortion,16 contributing to 20%–40% of maternal deaths in Nigeria.17–19 However, the majority of studies have been conducted either in tertiary health facilities20–23 or in urban areas,24,25 making data on contraceptive use in rural Nigeria scanty and skewing information on contraceptive use in Nigeria toward metropolitan consumption.
This study was conducted with the aim of determining the overall approach to contraceptives in rural Lagos, Nigeria. Its objectives are to 1) determine the extent of knowledge of contraceptive methods among rural women at different stages of reproductive age; 2) describe the pattern of nonuse and use of contraceptive methods among them; and 3) document their sources of information on contraceptive methods.
Materials and methods
This cross-sectional descriptive study took place in the Elegushi community in the Ibeju-Lekki Local Government Area (population 120,247) and the Ijede community in the Ikorodu Local Government Area (population 832,388) of Lagos State, Nigeria, between October 2012 and March 2013. Each of these bigger communities is divided into wards which are further divided into family groups. The approximate populations of these two rural communities of study were 30,500 and 88,000, respectively, consisting mainly of homogeneous people in different clustered compounds. The target population was women in different stages of childbearing age residing in these communities. It is estimated that 25% of the population in these communities were women of childbearing age (WCBA). The independent variables in the study were marital status, highest level of education, religion, and ethnic group. The dependent variables were knowledge and use of contraceptives. Knowledge was assessed by asking if the participants knew what contraceptives are, while use was determined by asking the women the type of contraceptive they use. Epi Info 7 was used to calculate the sample size for the projected WCBA population of each site of study, using 30% as an expected frequency of contraceptive use in each of the communities, a confidence limit of 5%, and confidence level set at 95%. The calculated sample size was 641 (319 for Ibeju-Lekki and 322 for Ikorodu). For contingencies, especially the considerations of attrition, nonresponse, and increase in representativeness, the sample size was inflated by 30%, bringing it to 833. Systematic random sampling was used, in which the starting point was the first house on a popular street in a particular direction and then every fourth house was selected for the study. If a selected house did not have any WCBA, then the next house was visited to replace it for a respondent. All the WCBA (15–49 years) who agreed to participate were interviewed. None of them was pregnant when the interview took place.
Mobile data capturing device
Questionnaires were electronically prepared in a mobile data capturing device. The electronic questionnaire was divided into six parts, consisting of administrative information; demographic information; knowledge of HIV/tuberculosis/malaria; contraceptive use; self-assessment of individual health; and, in the last part of the electronic questionnaire, the reports of testing for hemoglobin concentration, malaria parasitemia, and HIV. It took roughly 45 minutes to complete a questionnaire. Six field workers were trained in administering the electronic questionnaire. Once data were captured, the questionnaires were electronically sent to a central location where they were automatically recorded in an Excel spreadsheet.
Statistical analysis
The collected data were analyzed using STATA 13. Frequency tables were used for categorical variables. Cross-tabulations and chi-square tests were used for appropriate variables. Appropriate cross-tabulations and test statistics were applied and the P-value set at P<0.05
Ethical considerations
Ethical considerations included taking verbal informed consent from all the participants. The confidentiality of the data was ensured and clearance was obtained from the State Government ethics committee. The survey was anonymous in order to preserve the privacy of study subjects.
Definitions
Respondents were divided into three age groups and categorized into three corresponding stages of reproductive age. As shown in Figure 1, respondents below the age of 25 years were classified as early reproductive age (ERA), those between 25 and 34 years as mid reproductive age (MRA), and those 35 years and above as late reproductive age (LRA). Marital status was defined as “single” if the participant had never had a conjugal relationship or “married” if there had been or still was a conjugal relationship.
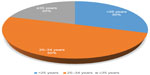  | Figure 1 Stages of reproductive age of respondents. |
Results
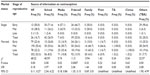
A total of 816 females of childbearing age, whose ages ranged from less than 15 to more than 45 years, fully responded to the questionnaire assessing their knowledge and use of contraceptives and the type of contraceptive they use mostly. Nine out of the initial 833 anticipated respondents traveled out of the study communities, five refused to respond further based on either religious or cultural beliefs, and three refused to participate at all, giving a response rate of 98.0%. Among the respondents, 244 (29.9%) were aged <25 years, among whom there were 107 (43.9%) single and 137 (56.1%) married women, and 405 were aged between 25 and 34 years, consisting of 44 (10.9%) single and 361 (89.1%) married women. Among those 35 years and older, only five (3.0%) were single while the rest (162, 97.0%) were married (Table 1; Figure 1). Table 1 also shows that 6.3% of all respondents had no formal education, while the majority (81.7%) of them had at least secondary education. The majority (470, 57.6%) of the respondents were Christians, while 41.9% were Moslems and only 0.5% were traditionalists. The Yoruba ethnic group was dominant (662, 81.1%), as is expected in this part of the country.
  | Table 1 Demographic characteristics of respondents relative to age group |
Overall, 99 (63.5%) single respondents (60.7% in ERA, 70.5% in MRA, 60.0% in LRA) and 547 (82.9%) married respondents (22.1% in ERA, 53.9% in MRA, and 24.0% in LRA) indicated awareness of female contraceptives (Table 2). The proportion of married women who knew about contraceptive methods (547, 82.9%) was significantly higher (χ2=28.8, P=0.0000, odds ratio [OR] =2.79, confidence interval [CI] =1.90, 4.09) compared to singles. Married respondents were about thrice more likely to have knowledge of contraceptives than singles.
An option of eight different types of contraceptive methods was presented to respondents to determine which they were more familiar with. As illustrated in Table 3, there was no statistically significant difference in the proportion of single and married women who were familiar with most of the different types of contraceptives. However, the proportion of married women with knowledge of injectables was significantly higher than that of single women (χ2=13.70, P=0.0002, OR =0.50, CI =0.34, 0.72), while the proportion of single women with knowledge of the abstinence method was significantly higher (χ2=11.96, P=0.0005, OR =2.48, CI =1.46, 4.22) than that of married women. Single women in the study had more knowledge of condoms (94, 60.3%), pills (76, 48.7%), and withdrawal (49, 31.4%) than other methods, while married women had more knowledge of condoms (413, 62.6%), pills (340, 51.5%), and injectables (311, 47.1%). There was very low knowledge of diaphragms/cervical caps/spermicide (13, 8.3%; 59, 8.9%) and tubal ligation (11, 7.1%; 27, 4.1%) among single and married women, respectively. Distribution of knowledge of contraceptives according to reproductive stage is also illustrated in Table 3.
Schools/educational institutions were the major sources of contraceptive information among the singles (42, 26.9%), while health facilities were the major sources of such information among married (352, 53.3%) respondents (Table 4). Married women were about six times more likely to source information on contraceptive use from health facilities (χ2=68.22, P=0.000, OR =5.71, CI =3.65, 8.94), while single women were about four times more likely to source such information from schools and educational institutions (χ2=40.59, P=0.000, OR =3.97, CI =2.54, 6.22); about thrice more likely to source it from other sources, such as traditional birth attendants (χ2=22.57, P=0.000, OR =3.08, CI =1.90, 4.99); and about twice more likely to source it from friends and colleagues (χ2=11.5, P=0.0007, OR =2.06, CI =1.35, 3.15).
In all, 424 WCBA admitted using contraceptives, giving an overall prevalence of 52.0% (Table 5). Among these 424, 51 (12.0%) were single women while 373 (88.0%) were married women. In the study population of single women, however, 32.7% admitted using contraceptives while, among the population of married women, 56.6% claimed using contraceptives. The proportion of married women using contraceptives was significantly higher than that of single women, and married women were about thrice more likely to use contraceptives than single women (χ2=28.70, P=0.000, OR =2.68, CI =1.85, 3.87). This may indicate that married women in rural areas, who already have children, are not yet ready for a next pregnancy or that they do not want to have children anymore. Table 5 also shows the distribution of contraceptive use in the different reproductive age groups.
Table 6 shows that condom use is the most common method of contraceptive among single women (35, 22.4%) and among married women (176, 26.7%), showing no significant difference in the proportion of single and married women using this commodity (χ2=1.18, P=0.23, OR =1.26, CI =0.83, 1.90). Married women were about four times more likely to use injectable contraceptives (χ2=13.47, P=0.0002, OR =4.31, CI =1.85, 10.02); almost thrice more likely to use the pill method (χ2=11.06, P=0.0007, OR =2.80, CI =1.51, 5.21); and two-and-a-half times more likely to use the withdrawal method (χ2=6.20, P=0.01, OR =2.52, CI =1.19, 5.32) when compared to single women in the study. Figure 2 illustrates that there are varying gaps between knowledge and use of some contraceptive methods among WCBA in rural Lagos. For example, although 60.3% of single women and 62.6% of married women claimed knowledge of condoms, only 22.4% of single women and 26.7% of married women actually use them, and although 30.8% of single and 47.1% of married women have knowledge of injectable contraceptives, only 3.8% of single women and only 14.7% of married women claimed they actually use injectable contraceptives.
  | Figure 2 Gaps between knowledge and use of some contraceptive methods among women of childbearing age in rural Lagos, Nigeria. |
On the contrary, as shown in Table 7, all the single women in the study claimed they do not use diaphragms/cervical caps/spermicide or tubal ligation, while 77.6%, 92.3%, and 96.2% claimed not using condoms, pills, and injectables, respectively. While 99.4%, 96.1%, and 98.3% of married women acknowledged not using tubal ligation, abstinence, and diaphragms/cervical caps/spermicide, respectively, 484 (73.3%) of them also claimed nonuse of condoms. Single women were more than four times likely not to use injectables (χ2=13.47, P=0.0002, OR =4.31, CI =1.85, 10.02); about thrice more likely not to use pills (χ2=11.06, P=0.0007, OR =2.80, CI =1.51, 5.21); and about two-and-a-half times more likely not to use the withdrawal method (χ2=6.20, P=0.01, OR =2.52, CI =1.19, 5.32).
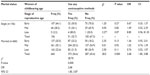
There was a negative but significant association between marital status and knowledge of contraceptives (t=−2.24, P=0.025) and a positive and significant association between knowledge of contraceptives and source of information on contraceptives (t=20.00, P=0.000) (Table 8). Multivariate analysis also showed that there was a positive and significant association between the use of contraceptives and the respondent’s stage of reproductive age (t=1.94, P=0.05) as well as the source of information (t=11.22, P=0.000), and a negative association between use of contraceptives and marital status (t=−2.79, P=0.005) as well as respondent’s religion (t=−1.89, P=0.05) (Table 9).
  | Table 8 Multivariate analysis on association between the dependent variable, knowledge of contraceptives, and other independent variables |
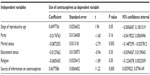  | Table 9 Multivariate analysis on use of contraceptives as the dependent variable and other independent variables |
Discussion
A national survey on contraceptive use among WCBA in Nigeria ought to be conducted every 4 years, as this would appear to be the best source of information on contraceptive use because it can reach a wide target population. Like other studies,17,26–28 the response rate in our study was quite high, probably due to the interest of women in topical issues such as contraceptive use. The majority of the respondents had at least a secondary level of education, while 6.1% had a higher degree of education. Of the total respondents, only 6.3% had no formal education, a relatively low figure compared to the 51.3% reported in Pakistan.29 Level of education is a key factor in a woman’s reproductive life. Some of the contributory factors to infant mortality include, for example, low female literacy and low access to and utilization of quality health services by women.30 The 1990 World Conference on Education for All (EFA) recognized improving access to quality education for girls and women as “the most urgent priority”, which was reaffirmed by over 100 countries at the April 2000 Dakar World Education Forum.31 Data from the current study show that knowledge of contraceptive methods was generally high among the respondents, ranging from 62% among singles to 83% among married respondents, just as reported by Abiodun and Balogun18 and Ezechi et al.28 In particular, knowledge of condoms was most prevalent among divorced (65.2%) respondents followed by married (62.7%) and by single (60.3%) respondents, respectively, corresponding with findings in another study.32 Condom use was also the most prevalent method of contraception among single and married respondents in this study, which accords with findings in Nigeria,33 Ghana,34 and the Democratic Republic of the Congo.35 The reason male condoms are preferred is probably because the female condom is not easily available and, even where available, its application is internal with uncertain effectiveness, while the male condom is external with a moderate degree of effectiveness. Male condoms are usually advertised in print and electronic media, and the commodity is occasionally distributed free, especially at rallies and in most hospitality establishments. In addition, they can be purchased cheaply at almost any corner patent medicine store as an over-the-counter item. Furthermore, male condoms have no apparent side effect which could harm the user, and it is believed that they not only prevent unwanted pregnancy, but also protect against sexually transmitted diseases. The nonuse of contraceptives was higher (67.3%) among single women compared to married (43.4%) respondents. Interestingly, among the single women, nonuse of contraceptives was highest (70.0%) among those in ERA. The inverse relationship between high knowledge of contraceptive methods and low contraceptive use, on one hand, and low contraceptive use and high sexual activity, on the other hand, might be strong factors for unplanned and unwanted pregnancies. The obvious sequel to unplanned and/or unwanted pregnancy is unsafe abortion, with high rates of pelvic inflammatory disease, intrauterine adhesions, secondary infertility, or maternal mortality. Studies have also documented high awareness of different methods of contraception, but low use.35,36 There are several possible reasons why single WCBA do not use contraceptives: 1) They may not have a male partner for sexual activity; 2) They may be ignorant about contraceptives; 3) They may want to experience a natural sexual sensation; 4) They may fear that they may not be able to give birth in the future due to side effects of some contraceptives; 5) Some may have experienced heavy menstrual bleeding after use of contraceptives such as IUDs. In other cases, single WCBA do not currently use contraceptives because they wish to get pregnant. This wish, sometimes dictated by a suitor, may have been delayed for a year or more after using hormonal implant. Documented reasons for nonuse of female contraceptives are 1) objections from male partner; 2) conflicts with religious beliefs; 3) objections from family members; 4) not thinking about using contraceptives; 5) abstaining from sex in order to avoid having a baby; and 6) unplanned sexual debut.36–38 Contrary to the data from our study, Lakew et al39 described living in rural areas and older age as factors negatively influencing modern contraceptive use.
Apparently, in some cases, non-use of contraceptives among single WCBA may suggest an indication of a wish to get pregnant.
Our study also shows that health facilities are the most frequent source of information dissemination on contraceptives among married (53.3%), and this rate is higher than that among single women (16.7%). This might be due to the relatively high level of education among women and mothers in southern parts of Nigeria.23 When marital status and source of information on contraceptives were regarded as independent variables and these were regressed against knowledge of contraceptives as a dependent variable, marital status and source of information were found to be significantly associated with knowledge of contraceptives. Meanwhile, stages of reproductive age, marital status, religion, and source of information on contraceptives were strongly associated with use of contraceptives.
Study limitations
The study has some limitations worth mentioning. First, the study was not based on nationally representative data, and the sample size may not be representative of all the females in Nigeria. Second, a questionnaire study may not be able to elicit all the information needed to arrive at a broad conclusion. Other qualitative techniques, such as focus group discussions, in-depth interviews, and observational studies, were not conducted. Third, stratification by marital status was skewed more toward the married than single, divorced, and widowed respondents. The sample size of widows in the study was negligible, and their views and perceptions may not be representative of other widows in the study area. Fourth, the study did not document participants’ knowledge of risk of not using contraceptives or of maternal mortality arising from nonuse of contraceptives. We also did not ask whether respondents were pregnant or not or whether they needed contraceptives at the time of interview. This was because we were of the opinion that external factors such as partner’s wish, pressure from family members, advise from friends and neighbors all could contribute to whether single women in child-bearing age determine to not use or to use contraceptive.
Conclusion
Knowledge and awareness of different methods of contraception was high among our study population. However, the high knowledge did not translate to high-frequency use of contraception, especially by unmarried respondents. Use of contraceptives was highest among the divorced and the married respondents, while nonuse was highest among the single respondents. Condom use was the most prevalent contraceptive method, and tubal ligation the least-accepted method. This study found that the prevalence of contraceptive use in general is higher than reported in another study,22 which may explain why maternal mortality might have reduced in Southwest Nigeria. It is therefore necessary for all levels of government and concerned organizations to carry out aggressive campaigns using print and electronic media, outreach programs, and rallies to achieve better awareness and use of modern, affordable, and acceptable contraceptive methods.
Acknowledgment
We would like to thank the Lagos State Honorable Commissioner for Health for giving us a rare opportunity to carry out this study.
Disclosure
The authors report no conflicts of interest in this work.
References
Grimes DA, Benson J, Singh S, et al. Unsafe abortion: the preventable pandemic. Lancet. 2006;368(9550):1908–1919. | |
Singh S, Darroch JE, Vlassoff M, Nadeau J. Adding it Up: The Benefits of Investing in Sexual and Reproductive Health. New York, NY: The Alan Guttmacher Institute; 2003. Available from: www.guttmacher.org/pubs/AddingItUp2009.pdf. Accessed November 29, 2014. | |
Carr D, Khan M. The Unfinished Agenda: Meeting the Need for Family Planning in Less Developed Countries. Washington, DC: Population Reference Bureau; 2004. Available from: www.prb.org/pdf08/familyplanningadvocacytoolkit-resources.pdf. Accessed November 29, 2014. | |
Progress Report April 2008. Global Campaign for the Health Millennium Development Goals. Available from: http://www.who.int/pmnch/topics/mdgs/norad_progress_report.pdf. Accessed October 6, 2014. | |
Tracking the Millennium Development Goals: Improve Maternal Health [webpage on the Internet]. United Nations Development Programme; 2007. Available from: http://www.mdgmonitor.org/goal5.cfm. Accessed October 6, 2014. | |
What progress has been made on MDG 5? Geneva: World Health Organization. Available from: www.who.int/maternal_child_adolescent/topics/maternal/mdg/en/. Accessed October 6, 2014. | |
Lincetto O, Mothebesoane-Anoh S, Gomez P, Munjanja S. Antenatal Care. Available from: http://www.who.int/pmnch/media/publications/aonsectionIII_2.pdf. Accessed October 13, 2014. | |
Gender and human rights [webpage on the Internet]. Geneva: World Health Organization. Available from: http://www.who.int/reproductivehealth/topics/gender_rights/sexual_health/en/. Accessed October 15, 2014. | |
Brown HL, Fan YD, Gonsoulin WJ. Obstetric complications in young teenagers. South Med J. 1991;84:46–48. | |
Will R. Contraceptive use in China [webpage on the Internet]. US-China Today. USC US-China Institute; 2012. Available from: http://www.uschina.usc.edu/article@usct?contraceptive_use_in_china_18021.aspx. Accessed November 10, 2014. | |
Mosher WD, Jones J. Use of contraception in the United States: 1982–2008. Vital Health Stat 23. 2010(29):1–44. | |
Caldwell JC, Caldwell P. The cultural context of high fertility in sub-Saharan Africa. Popul De Rev. 1987;13(3):409–437. | |
van de Walle E, Foster AD. Fertility Decline in Africa: Assessment and Prospects. World Bank Technical Paper 125. Washington, DC: The World Bank; 1990. | |
Weinberger M. Contraceptive use reduces unsafe abortion in Tanzania [webpage on the Internet]. London: Marie Stopes International. Available from: http://mariestopes.org/data-research/infographics/contraceptive-use-reduces-unsafe-abortion-tanzania. Accessed October 6, 2014. | |
Okech TC, Wawire NW, Mburu TK. Contraceptive use among women of reproductive age in Kenya’s city slums. International Journal of Business and Social Science. 2011;2(1):22–43. | |
Federal Office of Statistics and IRD/Macro International, 1992; NPC and ORC Macro, 2004; NCP and ICF Macro, 2009. In: Goliber, Tom, Rachel Sanders, and John Ross. 2009. Analyzing Family Planning Needs in Nigeria: Lessons for Repositioning Family Planning in Sub-Saharan Africa. Washington, DC: Futures Group, Health Policy Initiative, Task Order 1. http://www.healthpolicyinitiative.com | |
Otoide VO, Oronsaye F, Okonofua FE. Why Nigerian adolescents seek abortion rather than contraception: evidence from focus-group discussions. Int Fam Plan Perspect. 2001;27(2):77–81. | |
Abiodun OM, Balogun OR. Sexual activity and contraceptive use among young female students of tertiary educational institutions in Ilorin, Nigeria. Contraception. 2009;79:146–149. | |
Oye-Adeniran BA, Adewole IF, Umoh AV, Ekanem EE, Gbadegesin A, Iwere N. Community-based survey of unwanted pregnancy in southwestern Nigeria. Afr J Reprod Health. 2004;8(3):103–115. | |
Adekunle AO, Otolorin EO. Evaluation of the Nigerian population policy – myth or reality? Afr J Med Med Sci. 2000;29:305–310. | |
Adegbola O, Okunowo A. Intended postpartum contraceptive use among pregnant and puerperal women at a university teaching hospital. Arch Gynecol Obstet. 2009;280(6):987–992. | |
Aisien AO. Intrauterine contraceptive device (IUCD): acceptability and effectiveness in a tertiary institution. Afr J Med Med Sci. 2007;36(3):193–200. | |
Okunlola MA, Owonikoko KM, Roberts OA, Morhason-Bello IO. Discontinuation pattern among IUCD users at the family planning clinic, University College Hospital, Ibadan. J Obstet Gynaecol. 2006;26(2):152–156. | |
Abasiattai AM, Bassey EA, Udoma EJ. Profile of intrauterine contraceptive device acceptors at the University of Uyo Teaching Hospital, Uyo, Nigeria. Ann Afr Med. 2008;7(1):1–5. | |
Ekabua JE, Itam IH. The safety and complications of Norplant use in Calabar. Trop Doct. 2007;37(1):37–39. | |
Fawole AA, Aboyeji AP. Complications from unsafe abortion: presentations at Ilorin, Nigeria. Niger J Med. 2002;11(2):77–80. | |
Olugbenga-Bello AI, Abodunrin OL, Adeomi AA. Contraceptive practices among women in rural communities in south-western Nigeria. Global Journal of Medical Research. 2011;11(2). Available from: https://globaljournals.org/GJMR_Volume11/1-Contraceptive-Practices-Among-Women-in-Rural.pdf. Accessed October 23, 2014. | |
Ezechi OC, Gbajabiamilla TA, Gab-Okafor CV, Oladele DA, Ezeobi PM, Ujah IAO. Contraceptive behavior, practices and associated factors among Nigerian women living with human immunodeficiency virus infection. Journal of HIV and Human Reproduction. 2013;1:30–35. | |
Sadiq N, Waheed Q, Hussain M, et al. Factors affecting the utilization of antenatal care among women of reproductive age in Nurpur Shahan. J Pak Med Assoc. 2011;61(6):616–618. | |
Factors responsible for high infant and maternal mortality in Nigeria [webpage on the Internet]. Available from: http://articlesng.com/factors-responsible-high-infant-maternal-mortality-nigeria/. Accessed November 26, 2014. | |
Kyari GV, Ayodele J. The socio-economic effect of early marriage in North Western Nigeria. Mediterr J Soc Sci. 2014;5(14):582–592. | |
Monjok E, Smesny A, Ekabua JE, Essien EJ. Contraceptive practices in Nigeria: literature review and recommendation for future policy decisions. Open Access Journal of Contraception. 2010;1:9–22. | |
Nwachukwu I, Obasi OO. Use of modern birth control methods among rural communities in Imo State, Nigeria. Afr J Reprod Health. 2008;12(1):101–108. | |
Opoku B. Contraceptive use among ‘at-risk’ women in a metropolitan area in Ghana. Acta Obstet Gynecol Scand. 2010;89(8):1105–1107. | |
Kayembe PK, Fatuma AB, Mapatano MA, Mambu T. Prevalence and determinants of the use of modern contraceptive methods in Kinshasa, Democratic Republic of Congo. Contraception. 2006;74(5):400–406. | |
Oye-Adeniran BA, Adewole IF, Odeyemi KA, Ekanem EE, Umoh AV. Contraceptive prevalence among young women in Nigeria. J Obstet Gynaecol. 2005;25:182–185. | |
Amazigo U, Silva N, Kaufman J, Obikeze DS. Sexual activity and contraceptive knowledge and use among in-school adolescents in Nigeria. Int Fam Plan Perspect. 1997;23:28–33. | |
Okpani AO, Okpani JU. Sexual activity and contraceptive use among female adolescents – a report from Port Harcourt, Nigeria. Afr J Reprod Health. 2000;4:40–47. | |
Lakew Y, Reda AA, Tamene H, Benedict S, Deribe K. Geographical variation and factors influencing modern contraceptive use among married women in Ethiopia: evidence from a national population based survey. Reprod Health. 2013;10:52. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.