Back to Journals » Open Access Journal of Contraception » Volume 12
Knowledge and Associated Factors of Postpartum Contraceptive Use Among Women in the Extended Postpartum Period in Gondar City, Northwest Ethiopia
Authors Mekonnen BD , Gelagay AA, Lakew AM
Received 4 November 2020
Accepted for publication 23 December 2020
Published 25 January 2021 Volume 2021:12 Pages 7—15
DOI https://doi.org/10.2147/OAJC.S290337
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Igal Wolman
Birye Dessalegn Mekonnen,1 Abebaw Addis Gelagay,2 Ayenew Molla Lakew3
1Department of Nursing, Teda Health Science College, Gondar, Ethiopia; 2Department of Reproductive Health, Institute of Public Health, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia; 3Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
Correspondence: Birye Dessalegn Mekonnen Email [email protected]
Background: The choice of a postpartum contraceptive method and the timing of its initiation depend on the woman’s knowledge regarding postpartum contraceptives use. Also, women’s perception towards family planning is reliant on good knowledge and has a great influence on their attitudes and practices. There is limited information on the knowledge and associated factors of postpartum contraceptive use among women. Therefore, the aim of this study was to assess the knowledge and associated factors of postpartum contraceptive use among women in the extended postpartum period.
Methods: An institutional-based cross-sectional study was conducted from November 5, 2018 to December 5, 2018 among postpartum women in six health institutions in Gondar city, northwest Ethiopia. A systematic random sampling technique was used to select the study participants. Data were analyzed using SPSS version 20. Bivariable and multivariable logistic regression models were fitted to identify the determinants of knowledge of postpartum contraceptive use. Adjusted odds ratio (AOR) with their 95% confidence intervals (CI) were calculated. P-values less than 0.05 were considered to indicate statistical significance.
Results: Out of 403 participants, 299 (74.2%) had good knowledge on postpartum contraceptive use. Being urban residents (AOR=2.95, 95% CI=1.34– 6.48), previous modern contraceptives use (AOR=5.15, 95% CI=1.16– 22.88), health facility delivery (AOR=4.10, 95% CI=1.20– 13.98), and counseling about family planning during PNC (AOR=3.80; 95% CI=1.52– 9.51) were significantly associated with good knowledge.
Conclusion: This study showed that the knowledge of women regarding postpartum contraceptives was relatively low. Therefore, increasing institutional delivery service and counseling about family planning during the postpartum period should get more focus to address the knowledge gap of postpartum mothers.
Keywords: knowledge, postpartum, contraceptives use, Ethiopia
Introduction
Postpartum family planning (PPFP) is fundamental to prevent mistimed and closely spaced pregnancies following childbirth;1 as closely spaced pregnancies increase the risks of maternal morbidity and poor infant outcomes including preterm birth, low birth weight and small-for-gestational-age.2 Research shows that maternal death increases as the number of children (parity) per woman rises.3 A recent study revealed that contraceptive use could avert more than two-fifths of maternal mortality.4
The benefits of contraceptive utilization accrue to women themselves, their children, and community.5–7 Additionally, contraceptive use during the postpartum period plays a great role in improving the lives of women and their families.8,9 Women have an opportunity for accessing the healthcare system during the postpartum period which further increased their motivation to avoid another pregnancy using contraceptives.10 Following childbirth, pregnancy can occur within 45 days of giving birth, even before menses resumes.11,12 Thus, late initiation of contraceptive use in the postpartum period could increase the risk of unintended pregnancy.13 The World Health Organization (WHO) recommended initiation of postpartum contraceptive utilization within 6 weeks after delivery.14
In order to make choices about family planning (FP) women need to have adequate information about the availability of different contraceptive methods.15 In addition, the choice of contraceptive method and its timing initiation in the postpartum period depend on a woman’s knowledge about contraceptives.16 As well, women’s perception towards FP is reliant on good knowledge and has a great influence on their attitudes and practices.17,18
Access to timely utilization of modern contraceptives in the postpartum period is dependent on good knowledge of women regarding family planning.19 Evidence has indicated that the lowest contraceptive utilization was observed in sub-Saharan African countries, mainly due to low level of knowledge.20 Other evidence has revealed that lack of knowledge on contraceptive methods and their accessibility are barriers that exist in developing countries.21
Knowledge of women on the role of contraceptive use in family life is indispensable to good health.22 Given that, good knowledge increases intent to use contraceptives, which can then lead to increased postpartum modern contraceptive uptake. Hence, investigation of knowledge and its determinants of PPFP utilization will help to design and implement evidence-based interventions. However, there is limited evidence on levels of knowledge and its associated factors of postpartum contraceptive use, particularly in northwest Ethiopia. Therefore, this study aimed to fill the research gap by assessing the knowledge and its associated factors of postpartum contraceptive use among women in the extended postpartum period in Gondar city, northwest Ethiopia. The finding will help to design appropriate interventional strategies that could fight against the unsatisfactory potential demand of family planning services. Moreover, it will have a big contribution in reduction of maternal and infant mortality as well as morbidity rates.
Methods
Study Design and Setting
An institutional-based cross-sectional study was conducted in six public health institutions of Gondar city, northwest Ethiopia, 750 km from Addis Ababa, the capital of Ethiopia. The data were collected from November 5 to December 5, 2018. According to the Gondar city Health department office, the city has a population of approximately 78,546 women in the reproductive age group, and the estimated number of postpartum women was 10,360. The study site consists of eight governmental health centers and 14 rural health posts that are providing maternal and other health services to the community.
Study Population and Sampling
A total of 405 participants were determined using the single population proportion formula assuming the proportion of women who had a good knowledge on postpartum contraceptive in a previous study to be 60.1%,23 confidence level 95%, margin of error 5%, and 10% non-response rate. A systematic random sampling technique was used to select the study participants. The proportional allocation was made for six health facilities providing immunization service at Gondar city. Finally, every third woman who brought their child for immunization was included in the study. Women who gave birth in the last 12 months and attended immunization for their children at a public health facility in Gondar city were included in the study.
Data Collection Procedure
Data were collected by a structured and pretested questionnaire via face-to-face interview at the health institutions. The questionnaire and consent documents were first developed in English, then translated into Amharic by a language expert, and finally retranslated into English to check the consistency. The questionnaire was adapted from EDHS and other published literature.24–27 The questionnaire includes socio-demographic, reproductive health, and obstetric factors, source of information, and knowledge of modern postpartum contraceptives. Six female diploma midwives were assigned as data collectors and two Bsc nurses as supervisors. Training was given for data collectors and supervisors before the actual data collection.
Variables of the Study
Extended postpartum period: The first 12-month period after a live birth.
The dependent variable for this study was knowledge (good, poor). It was defined as follows: each question had a group of answer points; one point was awarded for each correct answer. Correct responses were summed up to get a total knowledge scores for each participant. Total score for all questions reached 16 grades. The knowledge scores were classified into Good knowledge (≥50%) and 50% was considered as Poor knowledge.28
The independent variables were socio-demographic factors: age, religion, marital status, educational level, residence, occupation, husband education, wealth status; reproductive health factors: number of live children, birth interval, menstrual resumption, fertility desire, breast feeding status, abortion history; and health service-related factors: antenatal care visits, postnatal care visit, place of delivery, family planning counseling during antenatal care, and family planning counseling during postnatal care.
Data Quality Control
Data quality was controlled through the provision of training for the data collectors and supervisors about the overall data collection procedures and the techniques of interviewing. To establish face validity, a pre-test was done on 5% of the sample questionnaire before the actual data collection to ensure the clarity of the questionnaire and necessary corrections were made based on the pre-test. Moreover, it was assumed to check the wording and to confirm the logical sequence of the questions with a population of postpartum women presumed to have similar sociodemographic characteristics to the population of the study area. The collected data were checked for completeness, consistency, accuracy, and clarity by the co-authors and the principal investigator on a daily basis.
Data Processing and Analysis
Data were entered into Epi Info version 7.2.2.2 statistical software and then exported to SPSS version 20 for further analysis. Frequencies and cross-tabulations were used to summarize descriptive statistics. Both bivariable and multivariable logistic regression was used to identify independent variables associated with knowledge of women on postpartum contraceptive use. Variables having a P-value≤0.2 in the bivariable analysis were included in the multivariable logistic regression model. The strength and presence of association was interpreted using the adjusted odds (AOR) ratio with their 95% confidence interval (CI). The criterion for statistical significance was set at a P-value of 0.05.
Results
Socio-Demographic Characteristics of Study Participants
A total of 403 participants responded completely to the study, making a response rate of 99.5%. The mean age of the respondents was 28.2 years (±5.3 SD); and more than half (221, 54.8%) of them were in the age group of 25–34. Out of the total study participants, 357 (88.6%) were urban dwellers. The majority (390, 96.8%), of the respondents were married and 374 (86.1%) orthodox in religion. One-third (149, 37%) of them had attended secondary school in their education. Of the respondents’ husbands, 178 (45.6%) had attended higher education. One hundred and fifty-eight (39.2%) of the respondents were found in the lowest economic status (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Study Participants in Gondar City, Northwest Ethiopia, 2019 (n=403) |
Reproductive Health and Obstetric Characteristics of Participants
The average number of living children per woman was 2.1, with a minimum of one and a maximum of ten children. Among the study participants, 33 (8.2%) had experienced abortion in their past. Three hundred and ninety-five (98%) of the study participants had an ANC visit for their recent pregnancy. Three hundred and seventy-nine (94%) mothers gave birth to their current children in government health institutions. The majority (377, 93.5%) of the current births were planned. Regarding reproductive plan, more than two thirds (68.9%) of the respondents wanted to have one to two children. Of the respondents, 329 (81.6%) attended postnatal care; of them, 299 (90.9%) received family planning counseling at postnatal care sessions. The majority (378, 93.8%) of participants had a history of previous contraceptive use, and nearly half (48.9%) were using contraceptives currently. Three hundred and eighty-eight (96.3%) respondents were currently breastfeeding their infant (Table 2).
 |
Table 2 Reproductive Health and Obstetric Characteristics of Study Participants in Gondar City, Northwest Ethiopia, 2019 (n=403) |
Knowledge of Postpartum Contraceptive Use
The findings of this study showed that 299 (74.2%) women had good knowledge regarding postpartum contraceptive use. Almost all (99.5%) of the study participants had heard about postpartum contraception. The most mentioned sources of contraceptive methods were health personnel 387 (96%) (Figure 1).
 |
Figure 1 Source of information about postpartum contraceptive use in Gondar town, northwest Ethiopia, 2019. |
The main advantages of contraceptive use mentioned by the study participants were to space between child births (372, 92.3%), followed by to prevent unwanted pregnancy (364, 90.3%), and to limit the number of children (276, 68.5%). Some of the respondents mentioned more than one advantage. Women were asked whether they knew about any contraceptives, and 398 (98.8%) and 367 (91.1%) of the respondents knew of injectable and pills methods, respectively (Figure 2).
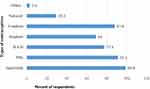 |
Figure 2 Type of contraceptives women know during extended postpartum period in Gondar town, northwest Ethiopia, 2019. |
It was observed that 273 (67.8%) women cited that the best time to start postpartum contraceptive was after 42 days following childbirth. One hundred and two (25.3%) of the respondents had discussed modern contraceptives with their partners (Table 3).
 |
Table 3 Knowledge-Related Characteristics and Partner Involvement of Study Participants in Gondar City, Northwest Ethiopia, 2019 (n=403) |
Factors Associated with Knowledge of Postpartum Contraceptive Use
In the multivariable logistic regression analysis, factors that were found to be significantly associated with knowledge of postpartum contraceptive use among women in the extended postpartum period were place of residence, modern contraceptive ever use, place of delivery, and FP counseling during PNC. Urban dwellers were about 3-times more likely to have good knowledge on postpartum contraceptive use than rural dwellers (AOR=2.95, 95% CI=1.34–6.48). The odds of those mothers who ever used contraceptive methods were 5.15-fold more knowledgeable than those mothers who did not use previously (AOR=5.15, 95% CI=1.16–22.88).
Postpartum women who gave birth to their current child in the governmental health institutions were 4.1-times more likely to have good knowledge regarding postpartum contraceptive use compared to those who gave birth at home (AOR=4.10, 95% CI=1.20–13.98). Similarly, counseling service on family planning during the postpartum period were found to be statistically significant in determining the knowledge of postpartum women about postpartum contraceptives use. Those mothers who were counseled during PNC were almost 4-times more likely to have good knowledge compared to those mothers who were not counseled (AOR=3.80; 95% CI=1.52–9.51) (Table 4).
 |
Table 4 Factors Associated with Knowledge of Postpartum Contraceptive Use During the Extended Postpartum Period in Gondar City, Northwest Ethiopia, 2019 |
Discussion
This study was conducted to assess the knowledge of women on postpartum contraceptive use and its associated factors among mothers in the extended postpartum period. Accordingly, the overall knowledge of women regarding postpartum contraceptive use was found to be 74.2% (95% CI=70–78.2). This finding is lower than the studies carried out in Aksum town, Tigray region,29 Hossana town,30 and southern Karnataka, India31 which reported the knowledge of women on contraceptive use among postpartum mothers was 95.8%, 96.5%, and 88% respectively. However, this finding is higher than those studies done in East Gojam Zone, northwest Ethiopia (60.1%),23 Kebribeyah Town, Somali Region, Eastern Ethiopia (68.2%),32 and Zambia (59%).33 The reason for this variation might be due to differences in reproductive health services and accesses to information, education, and counseling regarding postpartum contraceptive utilization. Furthermore, the difference could be due to differences in women’s access to mass media. Evidence has revealed that mass media plays a vital role in improving awareness of women on reproductive health including contraception.34
This study has identified that urban residence was associated with knowledge of women on postpartum contraceptive use. Women who were urban residents were about 3-times more likely to have good knowledge on postpartum contraceptive use than rural dwellers. This study is supported by cross-sectional studies conducted in Nigeria26 and India.16 The reason could be due to the fact that women in the urban areas are more likely to be more educated, and they have better access to information, education, and health facilities than rural women. Furthermore, the availability of major sources of family planning information, such as television and newspapers, are still very limited in rural areas.
Previous history of modern contraceptive use was found to be a determinant factor for knowledge of women on postpartum contraceptives use in which those mothers who had ever used modern contraceptive methods were about 5-times more knowledgeable than those mothers who had never used. This may be explained by the fact that previous exposure to contraceptives may give the opportunity to know the benefits and side-effects of contraceptives.
Postpartum women who gave birth to their current child at the Health facilities were about 4-times more likely to have good knowledge regarding postpartum contraceptive use than those who delivered at home. Similar findings were reported in a study conducted in India.35 The reason could be that women who delivered at a health facility might get an opportunity for comprehensive counseling about the modern contraceptives and lactational amenorrhea methods during their maternal health services utilization. Moreover, this finding suggests that facility delivery remains an important window of opportunity to provide access to family planning messages and to offer women various contraceptive methods.
Furthermore, postpartum mothers who were counseled during their postnatal care visit were nearly 4-times more likely to have good knowledge on postpartum contraceptive use compared to those mothers who were not counseled. This finding is supported by reports from Nigeria24 and India.35 This is because women who received family planning counseling during PNC might have adequate information regarding the source, benefit, side-effect, of contraceptives, and the place where they could find contraceptives.
While nearly three-quarters of women had good knowledge, which could increase their intent to use postpartum modern contraceptive uptake, a substantial number of women still had poor knowledge. This implies the need to improve the awareness of the women on the use of postpartum contraception through counseling, education, and social communication with a collaborative effort of policy-makers, program managers, health professionals, and other stakeholders.
Limitations of the Study
Though the study made its attempt to identify factors associated with knowledge of women on postpartum contraceptive use in the study setting, it is not free from some limitations. The study does not include data on the qualitative information of study participants, and it mainly focuses on individual level factors; and factors related to the health system and the service providers were not investigated. Furthermore, the measurements of knowledge tools are operationally defined according to our setting and from other similar findings, and these tools are not validated.
Conclusion
This study demonstrated that the knowledge of postpartum women regarding postpartum contraceptive use was relatively low. Women’s residence, contraceptive ever use, place of delivery, and FP counseling during PNC were factors significantly associated with knowledge of postpartum contraceptive use among postpartum women. Therefore, increasing institutional delivery service and counseling about modern family planning during the postpartum period should get more focus to address the knowledge gap on postpartum contraceptive utilization. There is also a great need to prioritize the provision of information and education for women in rural areas to empower them to create awareness regarding postpartum family planning.
Abbreviations
AOR, adjusted odds ratio; ANC, antenatal care; CI, confidence Interval; FP, family planning; PPFP, postpartum family planning; PNC, postnatal care; SPSS, Statistical Package for Social Science.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author.
Ethics Approval and Consent to Participate
Ethical clearance was obtained from the Institutional Review Board (IRB) of University of Gondar, College of Medicine and Health Sciences, Institute of Public Health. Formal letters of cooperation were written to the different health institutions in Gondar Town and Gondar Woreda Health Offices. The head of each health facilities also wrote a letter of permission to the immunization focal person. The ethical review committee of University of Gondar has identified the study procedure to cause less than very minimal risk after assessing the proposal document and, therefore, verbal consent was obtained from each woman for participation. Hence, verbal informed consent was approved by the IRB of University of Gondar. Moreover, the study was conducted in accordance with the Declaration of Helsinki. The benefit of the study was explained to the respondents. Participants were informed that they had the right to withdraw from the study at any time. The study participants were interviewed in a separate room keeping their privacy.
Consent to Publication
Not applicable.
Acknowledgment
The authors would like to acknowledge the Institute of Public Health, College of Medicine and Health Sciences, University of Gondar. The authors would also like to thank all health facility staff, data collectors, supervisors, and all mothers who participated in this study for their commitment in responding to the interviews.
Author Contributions
All authors (BDM, AAG, and AML) made substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Best practice in postpartum family planning. Royal College of Obstetricians and Gynaecologists. Best Practice Paper No. 1; 2015.
2. World Health Organization. Programming Strategies for Postpartum Family Planning. Geneva: WHO; 2013.
3. USAID. Healthy timing and spacing of pregnancies: A family planning investment strategy for improving the health and well-being of women and girls 2012. Available from: https://www.usaid.gov/sites/default/files/documents/1864/calltoaction.pdf.
4. Ahmed S, Li Q, Liu L, Tsui AO. Maternal deaths averted by contraceptive use: an analysis of 172 countries. The Lancet. 2012;380(9837):111–125. doi:10.1016/S0140-6736(12)60478-4
5. Ahmed S, Li Q, Liu L, Tsui AO. Maternal deaths averted by contraceptive use: an analysis of 172 countries. The Lancet. 2012;380(9837):111–125. doi:10.1016/S0140-6736(12)60478-4
6. Singh S, Darroch JE. Adding It Up: Costs and Benefits of Contraceptive Services. Guttmacher Institute and UNFPA; 2012:1269–1286.
7. Kozuki N, Walker N. Exploring the association between short/long preceding birth intervals and child mortality: using reference birth interval children of the same mother as comparison. BMC Public Health. 2013;13(S3):S6. doi:10.1186/1471-2458-13-S3-S6
8. Cleland J, Conde-Agudelo A, Peterson H, Ross J, Tsui AO. Contraception and Health. The Lancet. 2012;380(9837):149–156. doi:10.1016/S0140-6736(12)60609-6
9. Sonfield A, Hasstedt K, Kavanaugh ML, Anderson R. The Social and Economic Benefits of Women’s Ability to Determine Whether and When to Have Children. New York: Guttmacher Institute; 2013.
10. Control CfD, Prevention. Update to CDC’s US Medical Eligibility Criteria for Contraceptive Use, 2010: revised recommendations for the use of contraceptive methods during the postpartum period. MMWR Morb Mortal Wkly Rep. 2011;60(26):878.
11. Jackson EM, Glasier MPH, Anna MD. Return of ovulation and menses in postpartum nonlactating women: a systematic review. Obstet Gynecol. 2011;117(3):657–662. doi:10.1097/AOG.0b013e31820ce18c
12. Singh KK, Verma S, Tanti S. Contraceptive use among postpartum women in India. Asian Popul Stud. 2014;10(1):23–39. doi:10.1080/17441730.2013.827368
13. Singh KKVS, Tanti S. Contraceptive use among postpartum women in India. Asian Popul Stud. 2013;1–17.
14. Organization WH. WHO Recommendations on Postnatal Care of the Mother and Newborn. World Health Organization; 2014.
15. Gordon C, Sabates R, Bond R, Wubshet T. Women education and modern contraceptive use in Ethiopia. Int J Educ. 2011;3(1):1–23. doi:10.5296/ije.v3i1.622
16. Jyoti Vikas Rokade VRH, Hanji VR. Study of awareness of contraception in postnatal women. Int J Reprod Contracept Obstet Gynecol. 2018;7(6):2462–2466. doi:10.18203/2320-1770.ijrcog20182369
17. Morse JE, Rowen TS, Steinauer J, Byamugisha J, Kakaire O. A qualitative assessment of Ugandan women’s perceptions and knowledge of contraception. Int J Gynecol Obstetrics. 2014;124(1):30–33. doi:10.1016/j.ijgo.2013.07.014
18. Mashereni S, Miano M. Knowledge, Perception and Information That Kenyan Adolescents Have Regarding Use of Contraceptives. 2014.
19. Akinlo ABA, Esimai O. Use of maternal health care as a predictor of postpartum contraception in Nigeria. Afr Popul Stud. 2014;27(2):288–300. 1011564/27-2-475
20. Moreland SSE, Sharma S. World Population Prospects and Unmet Need for Family Planning. Vol. 62. Washington, DC: Futures Group; 2010.
21. Nath JIF. A study on the knowledge, attitude and practice about contraception in postpartum. Women of North India Int J Sci Res. 2015;4(12):465–468.
22. Dixit R, Bandhani A. Contraceptive knowledge, practices among women in Garhwal region. Int J Community Med Public Health. 2019;6(2):793–796. doi:10.18203/2394-6040.ijcmph20190209
23. Gizaw WZF, Abuhay M, Bayu H. Extended postpartum modern contraceptive utilization and associated factors among women in Gozamen District, East Gojam Zone, Northwest Ethiopia. Insights Reprod Med. 2017;1:
24. Anaba R, Ugwa EA, Agbor IE, Nwali MI, Orji B. Knowledge, attitude, and contraceptive preferences among postpartum women in Izzi, Ezza South, and Ikwo local government Areas of Ebonyi State, Nigeria. Hosp Pract Res. 2018;3(1):11–15. doi:10.15171/hpr.2018.03
25. Central Statistical Agency, ICF International. Ethiopia Demographic and Health Survey; 2016.
26. Evelyn O. Knowledge, attitude and acceptance of modern family planning method among women attending Post–Natal Clinic in Ayeka Basic Health Centre in Okitipupa Local Government Area, Ondo State, Nigeria. Biomed J Sci Tech Res. 2017;1(4).
27. Singh A, Meena P, Radhakrishnan G, Rutela M. A knowledge, attitude and practice study on awareness and acceptance of contraception in postpartum women in a tertiary care hospital. Int J Reprod Contracept Obstet Gynecol. 2016;5:1921–1924. doi:10.18203/2320-1770.ijrcog20161691
28. Jose MJ, Fathima FN, Joseph ST, et al. Knowledge regarding reproductive health among women of reproductive age group in three sub-centre areas of a primary health center, Sarjapur, Bengaluru, Karnataka: a cross sectional study. Int J Commun Med Public Health. 2019;6(9):4082. doi:10.18203/2394-6040.ijcmph20194021
29. Teklehaymanot Huluf Abraha HS, Belay HS, Welay GM. Intentions on contraception use and its associated factors among postpartum women in Aksum town, Tigray region, northern Ethiopia: a community-based cross- sectional study. Reprod Health. 2018;15:188. doi:10.1186/s12978-018-0632-2
30. Gejo NG, Anshebo AA, Dinsa LH. Postpartum modern contraceptive use and associated factors in Hossana town. PLoS One. 2019;14(5):e0217167. doi:10.1371/journal.pone.0217167
31. Kripa S, Shetty H. Knowledge, attitude and practice of contraception among the postnatal women in a tertiary care hospital in a rural area in Southern Karnataka, India. Int J Reprod Contracept Obstetrics Gynecol. 2017;6(5):1821. doi:10.18203/2320-1770.ijrcog20171600
32. Nigussie ATGD, Tura G. Postpartum family planning utilization and associated factors among women who gave birth in the past 12 months, Kebribeyah Town, Somali Region, Eastern Ethiopia. J Women’s Health Care. 2016;5:340.
33. Chama Daniel KT, Webster M, Mumbi M, Ngoma CM. Contraceptive choices and use among postnatal women in selected Districts in Luapula Province, Zambia. Central Afr J Public Health. 2018;4:191–195. doi:10.11648/j.cajph.20180406.14
34. Zamawe CO, Banda M, Dube AN. The impact of a community driven mass media campaign on the utilisation of maternal health care services in rural Malawi. BMC Pregnancy Childbirth. 2016;16(1):21. doi:10.1186/s12884-016-0816-0
35. Nath J, Islam F. A study on the knowledge, attitude and practice about contraception in postpartum women of North India. Parity. 2015;35(45):45.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
