Back to Journals » Transplant Research and Risk Management » Volume 14
Kidney Transplant Recipients with JC Virus Infection Have Decreased Function of the Transplanted Kidney
Authors Trung Hieu H , Sỹ BT
Received 1 August 2022
Accepted for publication 28 September 2022
Published 20 October 2022 Volume 2022:14 Pages 53—61
DOI https://doi.org/10.2147/TRRM.S384595
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Qing Yi
Ho Trung Hieu,1 Bùi Tiến Sỹ2
1Department of Nephrology and Dialysis, 108 Military Central Hospital, Hanoi, Vietnam; 2Department of Microbiology Department, 108 Military Central Hospital, Hanoi, Vietnam
Correspondence: Ho Trung Hieu, Department of Nephrology and Dialysis, 108 Military Central Hospital, No. 1 Tran Hung Dao Str., Hai Ba Trung District, Hanoi, 100000, Vietnam, Tel +84 985989675, Fax +84 2438213229, Email [email protected]
Purpose: We conducted a survey on the status of patients after kidney transplantation infected with JC virus (JCV), at 108 Military Central Hospital (108MCH), Vietnam, combining research on the effects of JCV infection on transplanted kidney function and understanding the risk factors for JCV infection in kidney transplant recipients.
Patients and Methods: A single-center cohort study was conducted in the period from March 2021 to July 2022, using a combination of retrospective and prospective methods, with longitudinal follow-up of 94 eligible kidney transplant patients who agreed to participate, at the Department of Nephrology and Dialysis, 108MCH, Vietnam. Patients undergo monthly health checks and have their blood and urine tested by a real-time PCR method, with TaqMan probes (BioRad, USA). If at least one of the two specimens (blood or urine sample) is positive for JCV (when JCV is quantified in blood or urine samples at > 250 copies/mL), the patient is confirmed to have JCV infection in any part or tissue of the body. Factors of JCV infection, such as age, gender, donor source, and immunosuppressive therapy, along with demographic and clinical data and JCV infection status, were analyzed using multivariable Cox-regression analysis. The estimated glomerular filtration rate (eGFR) was selected as an indicator of kidney function, and the difference in eGFR between JCV-infected patients and non-infected patients was compared using the t-test. This study was approved by the Research Ethics Committee.
Results: JCV was detected in 71.3% of kidney transplant patients. Differences in eGFR were observed between the JCV-infected and non-infected patient groups (64.47± 25.70 and 70.89± 28.80 mL/min/1.73 m2 for each group; independent t-test; t=− 6.079; p=0.00). Factors such as kidney donor (HR=0.086; 95% confidence interval [CI]: 0.008– 0.936; p=0.04), tacrolimus trough level (HR=1.083; 95% CI: 1.069– 1.097; p=0.00), mycophenolate dose (HR=1.002; 95% CI: 1.002– 1.001; p=0.00) and prednisone dose (HR=1.001; 95% CI: 1.000– 1.001; p=0.00) in the trio of immunosuppressants tacrolimus + mycophenolate mofetil (MMF) + prednisone (multivariable Cox-regression analysis) are potential risk factors for JCV infection in renal transplantation. JCV infection in kidney transplant patients lowers the eGFR, leading to decreased transplant kidney function (independent t-test, p=0.00).
Conclusion: The level of JCV infection in kidney transplant patients in our study is quite high (71.3%). Using an immunosuppressive regimen that uses the trio of immunosuppressants tacrolimus + MMF + prednisone, and having a donor source element are potential risk factors for JCV infection in renal transplantation. The function of the transplanted kidney is reduced by JCV infection in kidney transplant patients in the short term. The timely diagnosis and treatment of JCV can ensure the stable and long-term function of transplanted kidneys in kidney transplant patients.
Keywords: urinary tract infection, polyomavirus, JC polyomavirus, kidney transplant, Vietnam
Introduction
JC virus (JCV) was first identified in 1971 after propagation of the virus in glial cell cultures inoculated with brain extracts from a progressive multifocal leukoencephalopathy (PML) patient, and named after initials of the donor;1 since then, a variety of human polyomaviruses have been identified.2,3 The impact of JCV on nephropathy was shown in a few cases.4 However, there is evidence showing that JCV nephropathy occurs at both early and late stages after renal transplantation.5,6 In immunocompetent individuals, JCV infection usually presents as asymptomatic infection or mild respiratory symptoms.4,7 The reduction of immune function, especially cell-mediated changes in immune function, can lead to the reactivation of polyomaviruses and cause serious clinical consequences in immunosuppressed patients.8 The hallmark of JCV infection is asymptomatic primary infection occurring almost universally in childhood, from which time, the virus remains latent in the human host. Viral reactivation, as evidenced by the presence of viral DNA in the urine or less frequently in the blood, can occur intermittently throughout life, but rarely causes disease in the otherwise immunocompetent host, whereas occasional cases of JCV-associated disease are seen in the profoundly immunosuppressed, susceptible host.9 Reactivation of polyomavirus infection with shedding of infected urothelial cells (decoy cells) is estimated to occur in 10–60% of renal transplant recipients, but clinically significant disease occurs in less than 5%. The use of more powerful maintenance immunosuppression regimens incorporating mycophenolate mofetil (MMF) and tacrolimus has probably contributed to a rise in the incidence of clinically significant polyomavirus infection. The management of this condition is difficult and primarily involves progressive reduction in the immunosuppressive burden in an attempt to augment host mechanisms of viral clearance. The long-term outlook for graft survival is often poor.10 JCV belongs to the same branch as human polyomavirus (PyV),11 and has been shown to be associated with PyV-associated nephropathy12 and PyV-associated PML, caused by PyV JC.13 Since 35–90% of healthy adults are seropositive for BK virus and JCV, serological assays are rarely used for diagnosing ongoing PyV-associated diseases.14,15 In recent years, the correlation between JCV and postoperative complications of kidney transplantation has gradually been evaluated.
The purpose of our study is to determine the rate of JCV infection in kidney transplant recipients during the study period, initially to determine the causes as well as potential risk factors for JCV infection in patients after surgery kidney transplantation, and then to assess the effect of JCV in kidney transplant patients and determine strategies to prevent and treat JCV.
In this study, features such as age, gender, donor source, immunosuppressive therapy, and demographic and clinical data, and correlations between the effect of JCV infection on transplanted kidney function and JCV infection factors, and between JCV and immunosuppressive doses and immunosuppressive drug levels, were reviewed with a view to providing a reference for the appropriate adjustment of the immunosuppressive regimen for kidney transplant patients.
Materials and Methods
Subjects
This single-center cohort study was performed at the Department of Nephrology and Dialysis, 108 Military Central Hospital (108MCH), Vietnam. Patients who underwent renal transplantation between December 2016 and July 2022 were included in the study. Patients who were no longer undergoing therapy at the center were excluded from the study. We ended up enrolling 94 patients who received their first kidney transplant and underwent full participation in therapeutic therapy in this study. Five kidney transplant patients were followed up for 3 months or less after kidney transplant surgery, six kidney transplant patients were followed up for over 61 months, and 83 kidney transplant patients were followed up for 6 months or more. Clinical characteristics and transplant-related data, as well as several episodes of urinary tract infections that developed during the first year after transplantation, were examined retrospectively. Basiliximab was used as the standard inducer, while anti-thymocyte globulin (ATG) was administered to patients receiving kidneys from brain-dead donors. The patients were started on a triple-drug immunosuppressive regimen typically consisting of calcineurin inhibitors (tacrolimus), mycophenolate mofetil (MMF), and corticosteroids (prednisone). Corticosteroids were progressively tapered to 5 mg/day over 3 months after kidney transplant surgery. Induction regimens and maintenance immunosuppressive drugs at follow-up were also recorded.
Antibiotic prophylaxis with a single dose of ceftriaxon of 2 g/day for 7–10 days was used in all patients after surgery. The ureteral stents placed during the transplant operation were removed 4 weeks after transplantation.
All kidneys were donated voluntarily with written informed consent, and this was conducted in accordance with the Declaration of Istanbul. The participants provided informed consent for this study;, and patients’ written informed consent was reviewed and approved by the Institutional Review Board in Biomedical Research of 108MCH (approval ID: 2021-1539/HDDD).
Study Design
We conducted a longitudinal study to follow up renal transplant patients, using retrospective data from December 2016 and prospective data from March 2021 to July 2022. Repeated monitoring of health status was conducted monthly, along with blood and urine testing by a real-time polymerase chain reaction (PCR) method every 3 months for the first year and every 6 months for the following years. Donor source, age, gender, etiology of end-stage renal disease, type of renal replacement therapy, induction therapy, duration of renal replacement therapy (RRT), time after kidney transplant, clinical complications after kidney transplantation, immunosuppressive therapy, estimated glomerular filtration rate (eGFR), dosage (tacrolimus, MMF, prednisone), and trough level (C0) of the immunosuppressant tacrolimus, along with JCV infection status, were also collected.
Detection of Infection Pathogens
To determine JCV infection status, blood and urine samples were analyzed by real-time PCR. DNA extraction procedures were performed using standardized urine samples and blood samples, comparing the resulting overall JCV DNA yields by quantitative PCR (qPCR). After identifying protocol modifications that increased DNA yields (lyticase/lysozyme digestion, bead beating, boil/freeze cycles, proteinase K treatment, and carrier DNA use), all modifications were combined for systematic confirmation of the optimal protocol conditions. This optimized protocol was tested against commercially available methodologies to compare overall DNA yields, community representation, and diversity by next-generation sequencing (NGS).
The procedure for the JCV viral load assay was as follows. DNA was extracted from a 200 µL or 1 mL urine sample or blood sample using the NucliSENS® easyMAG® reagents and platform (Biomérieux). DNA was eluted in a final volume of 25 µL. The presence of JCV DNA was determined by qPCR, utilizing the primer set JCT-1, JCT-2, and a TaqMan probe (BioRad, USA) designed to amplify the JCV large T (LTAg) gene fragment. To quantify the viral load, the targeted LTAg gene fragment was subcloned into a pMA backbone (Life Technologies). A 10-fold serial dilution of linearized plasmid DNA was prepared, covering a dynamic range of 10–108 calculated copy numbers per 5 µL. Another plasmid carrying the homologous BK virus LTAg gene fragment was prepared similarly and included as a negative control plasmid. For each sample, a 15 µL pre-PCR mixture was prepared, containing 10 µL LightCycler® Probe master (2×) (Roche), 0.06 µL primer JCT-1 (100 µM), 0.06 µL primer JCT-2 (100 µM), 0.04 µL probe JCT-1.1 (100 µM), and 4.84 µL PCR grade water. Then, 5 µL of DNA extracted from urine and blood, plasmid DNA, or PCR grade water was added. Samples were run in duplicate on the BioRad CFX 96 thermocycler with the following cycling conditions: 95°C for 5 min, followed by 40 cycles of 95°C for 10 s, 60°C for 10 s, and 72°C for 10 s. qPCR data were analyzed with the BioRad CFX Manager™ software version 2.1, and the quantitative level of JCV was calculated and expressed as log copies per mL urine sample and blood sample; if in at least one of the two specimens the quantitative level of JCV was >250 copies/mL then the patient has been infected with JCV. Based on this result, the clinician diagnosed the patient as having JCV infection (JCV infection status).
Data Analysis
Statistical analysis was conducted using IBM SPSS Statistics software version 26.0. Categorical variables were presented as frequency (n) and percentage (%). Continuous variables (age, time of follow-up, eGFR, dose [tacrolimus, MMF, prednisone], and blood level of drug [tacrolimus]) were presented as mean and standard deviation. Multivariable Cox-regression analysis was performed to evaluate risk factors for the JCV infection. The eGFR was selected as an indicator of kidney function, and the difference in eGFR between JCV-infected patients and non-infected patients was compared using the t-test method. Comparison between age groups was performed by an ANOVA test. For all statistical analyses, a p-value <0.05 was considered significant.
Results
Characteristics of Study Subjects
The clinical characteristics and transplant-related data of the patients are illustrated in Table 1. Among 94 renal transplant patients included in the study (mean age 44.32±12.867 years, 74.5% male), 67 patients (71.3%) were infected with JCV, of whom 52 (55.3%) were male and 15 (16%) were female, and 27 patients (28.7%) were negative for JCV, of whom 18 (19.1%) were male and nine (9.6%) were female. Of the JCV-infected kidney transplant patients, 32 (34%) were under 40 years old, 52 (55.3%) were between 40 and 60 years old, and 10 (10.6%) were over 60 years old after kidney transplant surgery. The mean follow-up duration after renal transplantation was 30.16 months. These clinical features did not show a statistically significant difference in the prevalence of JCV (independent t-test, p>0.05). Donor sources were significantly different between groups (chi-squared test, p<0.05). The mean eGFR at baseline and endline showed a significant improvement in kidney graft (paired t-test, p<0.05). However, there was no significant difference in the comparison of the creatinine values. Antibiotic prophylaxis and immunosuppressive therapy, which included a calcineurin inhibitor (tacrolimus), an antimetabolite (MMF), and a corticosteroid (prednisone), were administered to all 94 renal transplant patients (100%). There was no significant difference in the type of induction therapy, either ATG or basiliximab, or immunosuppressive therapy (tacrolimus + MMF + prednisone).
 |
Table 1 Characteristics of Renal Transplant Recipients |
JCV Infection Status of Study Subjects
Overall, the prevalence of JCV in this study was quite high, accounting for 71.3% of the total number of patients in the study (on average, one patient was infected with JCV per month). The JCV infection status in the present study is illustrated in Table 2, which shows the number of patients with JCV infection present during the 61 months of the study. The number of kidney transplant patients infected with JCV was highest at 6 months after kidney transplant surgery, with 29 patients infected with JCV (30.8%), and this was also the time when the numbers of blood and urine samples positive for JCV were highest during the whole period of the study (nine blood samples positive for JCV, 40 urine samples positive for JCV). The time at which the number of JCV-infected kidney transplant patients was lowest was at 60 months after kidney transplant surgery, with one JCV-infected patient (one positive urine sample was obtained and all blood samples were negative for JCV).
 |
Table 2 Frequency, Proportion of Patients, Blood Samples, and Urine Samples Infected with JCV, by Months After Kidney Transplant Surgery |
Figure 1 shows the frequency of kidney transplant patients infected with JCV, mainly detected in urine samples. The positive rate in blood and urine samples was highest at 6 months post-transplant and then gradually decreased over time; and from the 42nd month after kidney transplant onward, JCV was no longer detectable in the blood samples. Urinary JCV infection was much higher than blood JCV infection: 245/690 (35.5%) urine samples were positive for JCV compared with 30/690 (4.3%) blood samples; in the month with the highest rate of infection (29 patients at the 6th month of kidney transplantation), there were 40 samples with JCV infection in the urine while only nine samples were infected with JCV in the blood.
 |
Figure 1 Frequency of JCV infection in blood samples and urine samples, and frequency of patients with JCV infection. |
Risk Factors for JCV Infection
Based on the results shown in Table 3, the potential risk factors that may be the cause of JCV infection in kidney transplant recipients included age, gender, donor, etiology of end-stage renal disease, hypertension, hematuria, proteinuria, and the triad of immunosuppressants, with concentrations of tacrolimus and doses of MMF and prednisone. In the last step, the fitting multivariable Cox regression showed only the significant variables.
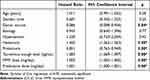 |
Table 3 Risk Factors for JCV Infection in Renal Transplantation |
Donor source (HR=0.086, p<0.05), hematuria (HR=1.405, p<0.01), proteinuria (HR=0.851, p<0.01), tacrolimus trough level (HR=1.083, p<0.01), dose of MMF (HR=1.002, p<0.01), and dose of prednisone (HR=1.001, p<0.01) were independent risk factors for JCV infection (Table 3).
Kidney Transplant Patients Infected with JCV Have Decreased Function of the Transplanted Kidney
The results in Table 4 show that the mean eGFR was different in JCV-infected kidney transplant patients and non-JCV-infected kidney transplant patients (64.47 vs 70.89 mL/min/1.73 m2; t=−6.079; p=0.00), and JCV-infected kidney transplant patients had lower mean eGFR than patients without JCV infection. These results indicate that JCV infection in kidney transplant patients will reduce both the eGFR and the function of the transplanted kidney (independent t-test, p=0.00). Therefore, timely diagnosis and treatment of JCV infection can ensure the stable and long-term function of the transplanted kidney in kidney transplant patients.
 |
Table 4 Relationship Between JCV Infection and Transplanted Kidney Function |
Discussion
JCV is inactive in healthy individuals but in immunosuppressed individuals may be reactivated and cause some related disorders.16 Kidney transplant recipients routinely undergo immunosuppressive treatments.16 Therefore, transplant recipients are often at risk of JCV infection. The rate of JCV infection in our study was 71.3%, which is higher than the rates found in other studies.17–19 The trend toward increasingly potent immunosuppressive drugs and higher drug concentrations in high-risk transplant patients in some Asian countries, which have a more tropical climate compared to other countries,20 may lead to a higher incidence of JCV. In our study, no significant difference was observed in the frequency of JCV in different sexes (independent t-test, p>0.05) or age groups (ANOVA, p>0.05), which is consistent with reports from Spain21 and Iran.22
Similarly to previous reports, the rate of viral infection in our study was highest at 6 months after kidney transplant surgery.23 The reason for this may be that in the first 6 months after kidney transplantation, the patient receives the highest dose of immunosuppressive therapy to prevent rejection of the graft after surgery, and the level of immunosuppression peaks at 6 months after kidney transplant surgery, so at this time, the patient’s immune system is at its weakest, which may facilitate JCV reactivation or a new infection.8,24 We also show that using the trio of immunosuppressants of tacrolimus + MMF + prednisone is one of the main causes of JCV infection in kidney transplant patients. This result is similar to reports of using this trio of immunosuppressants in kidney transplant recipients in previous studies.25,26 Therefore, appropriate adjustment of the dose of immunosuppressive drugs, under the guidance of Fulton and Markham,27 is an urgent goal in the prevention and treatment of JCV in kidney transplant patients.
Also in this study, we have shown that JCV infection in kidney transplant patients will reduce the eGFR, leading to a decrease in the function of the transplanted kidney (independent t-test, p<0.05). This result is similar to the findings of studies on polyomavirus infection in kidney transplantation and the role of immunosuppressive therapy.28 Reduced immunosuppression is associated with the stabilization of renal function when treated early. However, if the immunosuppressive dose is lower than required, the patient may experience significant kidney transplant damage and be at high risk of transplant rejection. The lack of effective antiviral therapy for JCV may limit the use of newer and more potent immunosuppressive drugs. Therefore, adjusting the level of immunosuppression for patients after surgery so that it can both meet the requirements of preventing damage and rejection of the transplanted kidney, and meet the requirements of immunity, is the acute goal, and is essential in immunosuppressive therapy after renal transplantation in renal transplant patients.
Conclusion
In the present study, patients infected with JCV accounted for a high percentage of patients following kidney transplant surgery. The donor source, hematuria, proteinuria, and the use of immunosuppressive regimens comprising the trio of immunosuppressants tacrolimus + MMF + prednisone can significantly increase the risk of JCV. Therefore, adjusting the dose of immunosuppressive drugs so that it can both meet the requirements of preventing injury and rejection of the transplanted kidney, and meet the immunological requirements, is a necessary acute goal in immunosuppressive therapy after kidney transplantation in kidney transplant patients. The function of the transplanted kidney is impaired by JCV infection in kidney transplant patients. Therefore, the timely diagnosis and treatment of JCV can ensure the stable and long-term function of the transplanted kidney in kidney transplant patients.
Acknowledgments
The authors acknowledge the members of the Division of Transplantation and the Department of Nephrology and Dialysis, 108MCH, for their efforts in continuing to deliver the best quality of care to the patients and their families.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Padgett B, Zurhein G, Walker D, Eckroade R, Dessel B. Cultivation of papova-like virus from human brain with progressive multifocal leucoencephalopathy. Lancet. 1971;297(7712):1257–1260. doi:10.1016/S0140-6736(71)91777-6
2. Atkinson A, Atwood W. Fifty years of JC polyomavirus: a brief overview and remaining questions. Viruses. 2020;12:969. doi:10.3390/v12090969
3. Mayberry CL, Maginnis MS. Taking the scenic route: polyomaviruses utilize multiple pathways to reach the same destination. Viruses. 2020;12(10):1168. doi:10.3390/v12101168
4. Delbue S, Ferraresso M, Ghio L, et al. A review on JC virus infection in kidney transplant recipients. Clin Dev Immunol. 2013;2013:1–7. doi:10.1155/2013/926391
5. Hildreth JE, Alcendor DJ. JC polyomavirus and transplantation: implications for virus reactivation after immunosuppression in transplant patients and the occurrence of PML disease. Transplantology. 2021;2(1):37–48. doi:10.3390/transplantology2010004
6. Safaei F, Mohebbi A, Hassanpour M, Razavi Nikoo H, Tabarraei A. Viruria of human BK virus and John Cunningham virus among renal transplant recipients and healthy control in Southeast of Caspian Sea. Intervirology. 2021;64(3):111–118. doi:10.1159/000513369
7. Chen Y, Bord E, Tompkins T, et al. Asymptomatic reactivation of JC virus in patients treated with natalizumab. N Engl J Med. 2009;361(11):1067–1074. doi:10.1056/NEJMoa0904267
8. Traylen CM, Patel HR, Fondaw W, et al. Virus reactivation: a panoramic view in human infections. Future Virol. 2011;6(4):451–463. doi:10.2217/fvl.11.21
9. De Gascun CF, Carr MJ. Human polyomavirus reactivation: disease pathogenesis and treatment approaches. Clin Dev Immunol. 2013;2013:1–27. doi:10.1155/2013/373579
10. Clarkson MR, Brenner BM, Magee C. Pocket Companion to Brenner and Rector’s the Kidney. Elsevier Health Sciences; 2010.
11. King AM, Adams MJ, Carstens EB, Lefkowitz EJ. Virus taxonomy: classification and nomenclature of viruses. Virus Taxonomy. 2012;2012:1327.
12. Baksh FK, Finkelstein SD, Swalsky PA, Stoner GL, Ryschkewitsch CF, Randhawa P. Molecular genotyping of BK and JC viruses in human polyomavirus [ndash] associated interstitial nephritis after renal transplantation. Am J Kidney Dis. 2001;38(2):354–365. doi:10.1053/ajkd.2001.26101
13. Cinque P, Dumoulin A, Hirsch HH. 24 diagnosis of polyomavirus infection, replication, and disease. Lennettes Lab Diagn Viral Infect. 2016;2016:401.
14. Bodaghi S, Comoli P, Bösch R, et al. Antibody responses to recombinant polyomavirus BK large T and VP1 proteins in young kidney transplant patients. J Clin Microbiol. 2009;47(8):2577–2585. doi:10.1128/JCM.00030-09
15. Egli A, Dumoulin A, Köhli S, Hirsch HH. Polyomavirus BK after kidney transplantation: role of molecular and immunological markers. Trends Transplant. 2009;3:85–102.
16. Ferenczy MW, Marshall LJ, Nelson CD, et al. Molecular biology, epidemiology, and pathogenesis of progressive multifocal leukoencephalopathy, the JC virus-induced demyelinating disease of the human brain. Clin Microbiol Rev. 2012;25(3):471–506. doi:10.1128/CMR.05031-11
17. Yin W-Y, Lu M-C, Lee M-C, Liu S-C, Lin T-Y, Lai N-S. A correlation between polyomavirus JC virus quantification and genotypes in renal transplantation. Am J Surg. 2010;200(1):53–58. doi:10.1016/j.amjsurg.2009.03.017
18. Boukoum H, Nahdi I, Sahtout W, Skiri H, Segondy M, Aouni M. BK and JC virus infections in healthy patients compared to kidney transplant recipients in Tunisia. Microb Pathog. 2016;97:204–208. doi:10.1016/j.micpath.2016.06.015
19. Atyabi SR, Bouzari M, Kardi MT. John cunningham (JC) virus genotypes in kidney transplant recipients, rheumatoid arthritis patients and healthy individuals in Isfahan, Iran. J Med Virol. 2017;89(2):337–344. doi:10.1002/jmv.24626
20. Vanichanan J, Udomkarnjananun S, Avihingsanon Y, Jutivorakool K. Common viral infections in kidney transplant recipients. Kidney Res Clin Pract. 2018;37(4):323. doi:10.23876/j.krcp.18.0063
21. Lopez V, Gutierrez C, Burgos D, et al. Prospective Study of Infection and Nephropathy Due to BK and JC Polyomavirus in 76 Kidney Transplant Recipients. Elsevier; 2008:2927–2929.
22. Taheri S, Kafilzadeh F, Shafa M, et al. Comparison of polyomavirus (BK virus and JC viruses) viruria in renal transplant recipients with and without kidney dysfunction. J Res Med Sci. 2011;16(7):916.
23. Alangaden GJ, Thyagarajan R, Gruber SA, et al. Infectious complications after kidney transplantation: current epidemiology and associated risk factors. Clin Transplant. 2006;20(4):401–409. doi:10.1111/j.1399-0012.2006.00519.x
24. Karpas A, Lowdell M, Jacobson SK, Hill F. Inhibition of human immunodeficiency virus and growth of infected T cells by the immunosuppressive drugs cyclosporin A and FK 506. Proc Natl Acad Sci. 1992;89(17):8351–8355. doi:10.1073/pnas.89.17.8351
25. Mele TS, Halloran PF. The use of mycophenolate mofetil in transplant recipients. Immunopharmacology. 2000;47(2–3):215–245. doi:10.1016/S0162-3109(00)00190-9
26. Balal M, Demir E, Paydas S, Sertdemir Y, Erken U. Uncommon side effect of MMF in renal transplant recipients. Ren Fail. 2005;27(5):591–594. doi:10.1080/08860220500200171
27. Fulton B, Markham A. Mycophenolate mofetil. Drugs. 1996;51(2):278–298. doi:10.2165/00003495-199651020-00007
28. Barri YM, Ahmad I, Ketel BL, et al. Polyoma viral infection in renal transplantation: the role of immunosuppressive therapy. Clin Transplant. 2001;15(4):240–246. doi:10.1034/j.1399-0012.2001.150404.x
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
