Back to Journals » Clinical Optometry » Volume 13
Keratoconus Epidemiology Presentations at Najran Province, Saudi Arabia
Authors Alzahrani K , Al-Rashah A, Al-Salem S, Al-Murdif Y, Al-Rashah A, Alrashah A, Al-Faify N , Ibrahim M
Received 9 March 2021
Accepted for publication 11 May 2021
Published 27 May 2021 Volume 2021:13 Pages 175—179
DOI https://doi.org/10.2147/OPTO.S309651
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Mr Simon Berry
Khaled Alzahrani,1 Ali Al-Rashah,2 Salem Al-Salem,2 Yahya Al-Murdif,2 Abdalaziz Al-Rashah,2 Alhassan Alrashah,2 Noura Al-Faify,3 Mohammed Ibrahim2
1Optometry Division, Ophthalmology Department, King Fahad Armed Forces Hospital, Jeddah, Saudi Arabia; 2Ophthalmology Department, King Khaled General Hospital, Najran, Saudi Arabia; 3Research Administration, Ministry of Health, Najran, Saudi Arabia
Correspondence: Khaled Alzahrani
Optometry Division, Ophthalmology Department, King Fahad Armed Forces Hospital, Jeddah, 21159, Saudi Arabia
Email [email protected]
Aim: Our study aims to produce an estimation of the keratoconus disease epidemiology and important demographic factors in disease presentation in Najran city in the south of Saudi Arabia.
Methods: Keratoconus patients between 9 and 29 years of age at the eye clinic of King Khaled General Hospital in Najran Province with a confirmed diagnosis of keratoconus were recruited over one year period. Visual acuity, keratometry, corneal thickness and demographic data were collected and analysed.
Results: The keratoconus prevalence in Najran Province was found to be 87.3 cases per 100,000 people with an incidence of 28.47 per 100,000 cases. The disease presented more frequently in male patients (67.9%) with a statistically significant difference in the mean age between genders (p=0.014). Most cases presented at a moderate stage, and almost half of the cases reported a family history of the disease. There were statistically significant differences in best visual acuity and corneal thickness between genders (p< 0.05). The majority of the cases were managed with contact lenses (56.08%).
Conclusion: Genetic and environmental factors could have a substantial role in the increased rate of keratoconus presentation in Najran Province. Screening programmes should dedicate more attention to late presentation to improve prevention and early detection. More studies on keratoconus epidemiology in Saudi Arabia are needed.
Keywords: keratoconus, incidence, prevalence, epidemiology, cornea
Introduction
Keratoconus (KC) is characterised as a non-inflammatory, ectatic disorder of the cornea.1 Typically, this disease is a progressive and bilateral yet asymmetric condition2 which predominantly impacts the inferior-central two-thirds of the cornea.3 During the early stages, stromal thinning results in a protruding conical shape, which induces “irregular” astigmatism and significant higher-order aberrations, both of which negatively impact visual performance.4 Existing literature indicates that KC tends to occur in adolescence,3 and the likely course of progression extends to the age of 30 or 40.5
The prevalence and incidence of KC has not yet been accurately determined. An early study has reported that the frequency of KC ranges from 50 to 230 cases per 100,000 individuals in the general population across North America.3 A more recent study has estimated the incidence of KC as 5 to 23 cases per 10,000 people and its prevalence as 5.4 per 10,000.6 Several analyses found on topographic data together with ocular slit-lamp examination which were conducted within the UK have demonstrated a KC frequency of 32 to 65 cases per 100,000 people.7–9 The prevalence of KC varies widely; the corneal ectatic disorder affects an approximate average of 1 in 2000 individuals in any population, is equally distributed between men and women10,11 and ranges from about 50 to 230 cases per 100,000 people.10 A recent study on its prevalence in Saudi Arabia produced a ratio of 1:21 people in the population.12 The disease is believed to be more common amongst Asians than Caucasians.13,14 There is significant interest in investigating this ratio in different areas in Saudi Arabia and especially in the southern region of the country.
The purpose of our study is to provide the first epidemiological analysis to produce an estimation of the prevalence of KCN in Najran city in the south of Saudi Arabia.
Participants and Methods
Data for this prospective, cross-sectional and observational study were obtained from a database of patients at the eye clinic of King Khaled General Hospital. The confidentiality and privacy of patients were maintained throughout the study. The study gained ethical approval from ministry of health-Saudi Arabia with IRB registration with KACST, KSA:H-11-N-081. The patients and parent or legal guardian of participants under 18 years of age provided informed consent. This study was conducted according to the declaration of Helsinki.
The routine daily clinical visit database was used to identify the KCN patients. The research analyses eye clinic visitors over a period of at least 6 to 12 months. The investigation is based on click study protocol.15
Recruitment extended to all patients of the Department of Ophthalmology at King Khaled General Hospital in Najran, Saudi Arabia between 2019 and 2020 who were suspected of having KC as well as patients who had been newly diagnosed with KC but were attending other tertiary hospitals in Najran Province. All subjects were examined for their case history, visual acuity, keratometry, refraction and ocular signs. Diagnoses were established based on changes in best-corrected visual acuity, familial KC, an irregular surface as evidenced by distorted corneal curvature, keratometry and corneal topography by means of a Pentacam (OCULUS, Wetzlar, Germany). There are many classifications to describe the severity of KC. For this research, we applied the keratometric classification, as it is a simple and applicable practice at our unit. According to average keratometric readings, eyes were sub-classified into mild (<48 dioptres), moderate (48–54 dioptres) or severe (>54 dioptres) KC, scissoring of the retinoscopy reflex, or irregularity in the red reflex on direct ophthalmoscopy. Clinical signs included at least one of the following: central corneal thinning, apical stromal scarring, Vogt’s striae, Fleischer’s ring and Munson’s sign. The sample excluded unusual cases for which a diagnosis could not be established with confidence. Continuous data are presented as mean ± standard deviation. Frequency and prevalence data are presented as n (%). Data normality was verified using a standard normality test, continuous data were compared using unpaired Student’s t-tests and categorical data were compared using chi-square tests. The results were analysed by using the package of SPSS23.
Results
According to a 2019 report by the General Authority for Statistics in Saudi Arabia, the total population of Najran Province was 608,467 people, of whom 210,739 were between 9 and 29 years of age. King Khaled General Hospital is the main hospital that provides eye care. Keratoconus was present in 312 eyes amongst 184 patients attending this hospital. The annual prevalence of KC in Najran was found to be almost 87.3 cases per 100,000 in the city’s population of individuals between 9 and 29 years of age. The incidence rate was found to be 28.47 cases per 100,0000 in the targeted population. This disorder affected 0.41% of patients at the eye clinic of King Khaled General Hospital (Table 1).
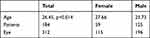 |
Table 1 Demographic Data for KC Patients |
Most of the KC patients were male (125; 67.9%), while 59 (32.0%) were female. The mean age was 26.45 years with a statistically significant age difference between genders (p=0.014).
LogMAR visual acuity results were found to decrease alongside an increase in disease severity. However, visual acuity was stronger in males than in females to a statistically significant degree (p=0.0018). There was no statistically significant difference between males and females in terms of corneal thickness pachymetry readings (p>0.05; Table 2). In addition, improvement to visual acuity per eye was achieved with spectacles in 123 cases (39.4%) and with soft or hard contact lenses in 175 cases (56.08%), and 14 cases (4.8%) were in need of a PKP procedure.
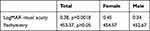 |
Table 2 Visual Acuity and Corneal Thickness Differences Between Males and Females in KC Cases |
A family history of KC was present in 89 patients (48.3%), whereas 95 patients (51.7%) reported no family history. Most of the cases were in the moderate stage. Based on keratometry results, which were graded according to the Zednik grading system, the average keratometry reading was 50.47 mm for disease severity, and statistically significant differences were observed between males and females (p=0.03; Table 3).
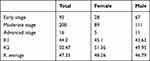 |
Table 3 Disease Severity Differences Between Males and Females Based on Keratometry Readings |
Discussion
The occurrence of KC varies widely at the global level according to the sample selection of patients, the location and the criteria for identification. Research has suggested an incidence and prevalence ranging from 0.3 cases per 100,000 people in Russia16 to 2300 cases per 100,000 in India.17 Only a few studies have explored KC in Saudi Arabia. For instance, Dr Assiri and his colleague have considered the incidence of KC in Asir Province in the south of Saudi Arabia and reported an estimation of 20 cases per 100,000 people.18 In addition, KC has been cited as the most common reason for not performing refractive surgery in Saudi Arabia, accounting for almost one-quarter of cases and occurring with a proposed incidence of 18.7%.19 Finally, recent reports have specified a higher rate of KC in children (1 case per 21) in Saudi Arabia compared to in other countries.20
Our study is the first report regarding KC epidemiology in Najran. Our results are comparable to those of other reports from several locations in the world. Although some studies have identified a higher prevalence amongst women, our study observes a higher prevalence amongst men.5,21 Family history also appears to be an important factor for the presentations of KC in Najran Province, which is consistent with studies that have suggested genetics as a factor22 with a high rate of consanguinity.7 However, the rate of KC presentation in our research exceeds that in comparable studies.23 Our study further agrees with previous findings concerning the occurrence of bilateral and asymmetric disease. The prevalence rates of KC in certain areas like Arab Gulf and Egypt could be higher than previously believed.24,25
Environmental factors might also be relevant, as the hot, dry weather in Najran Province may increase the prevalence of KC.18 In contrast, locations with colder temperatures exhibit lower incidences of KC.5,26 Furthermore, the presentation of KC may be associated with a diversity of influences, such as eye rubbing, Down’s syndrome, atopic disease, connective tissue disease, tapetoretinal degeneration and inheritance; nevertheless, its aetiology and pathogenesis are still indefinite.3
The average age for KC diagnosis in our study is relatively high considering that the disease emerged between the ages of 10 and 20 and progressed until the early 30s.9,27 Late presentation could be a prominent reason for requiring keratoplasty rather than other forms of management, as non-surgical KC management tools could be utilised when the disease is diagnosed early.3,28
Rapid changes in corneal curvature, diminished visual acuity and heightened irregular astigmatism are considered warning signs of KC. Timely action in response to these signs is imperative for early detection and management. Late presentation of patients to the eye care centre could be reduced by educating the population as well as empowering eye care specialists and optometrists in primary health care centres, as they have a heavy impact on early disease detection and can refer cases to more specialised centres when appropriate.
Our study was limited by the absence of certain key demographic information. The nature of the study was a further limitation, as it is expected that some cases were missed due to geographical difficulties and population awareness hindering access to eye health care services.
Our study suggested a national screening programme, which helps in reducing the late presentation rate for the KC cases. That will have effectively help at increase survival rate to avoid corneal transplant. Most of Saudi Arabia have similar habit in marriage; most of the cities have similarity in weather except some area. That increase the need of screening programme.
Conclusion
The prevalence and incidence of KC in Najran Province is high in comparison to figures reported in other studies. The presentation of KC in Najar could be influenced by numerous factors, including genetics and environmental aspects. In the majority of cases, patients presented to the hospital by 3rd decade, and the disease was more prevalent in males. Knowledge of the epidemiology of KC is important for treatment plans and management of the disease. Moreover, it is crucial for improving the ability of clinicians to detect early corneal changes. The data obtained from this study can act as a reference guide for government officials, clinicians and trainees.
Disclosure
The authors reported no conflicts of interest for this work.
References
1. Lawless M, Coster DJ, Phillips AJ, Loane M. Keratoconus: diagnosis and management. Aust N Z J Ophthalmol. 1989;17(1):33–60. doi:10.1111/j.1442-9071.1989.tb00487.x
2. Zadnik K, Steger-May K, Fink BA, et al. Between-eye asymmetry in keratoconus. Cornea. 2002;21(7):671–679. doi:10.1097/00003226-200210000-00008
3. Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28(4):293–322. doi:10.1016/0039-6257(84)90094-8
4. Jinabhai A, Radhakrishnan H, Tromans C, O’Donnell C. Visual performance and optical quality with soft lenses in keratoconus patients. Ophthalmic Physiol Opt. 2012;32(2):100–116. doi:10.1111/j.1475-1313.2011.00889.x
5. Kennedy RH, Bourne WM, Dyer JA. A 48-year clinical and epidemiologic study of keratoconus. Am J Ophthalmol. 1986;101(3):267–273. doi:10.1016/0002-9394(86)90817-2
6. Romero-Jimenez M, Santodomingo-Rubido J, Wolffsohn JS. Keratoconus: a review. Cont Lens Anterior Eye. 2010;33(4):
7. Georgiou T, Funnell C, Cassels-Brown A, O’Conor R. Influence of ethnic origin on the incidence of keratoconus and associated atopic disease in Asians and white patients. Eye. 2004;18(4):379. doi:10.1038/sj.eye.6700652
8. Weed K, MacEwen C, Giles T, Low J, McGhee C. The Dundee University Scottish Keratoconus study: demographics, corneal signs, associated diseases, and eye rubbing. Eye. 2008;22(4):534–541. doi:10.1038/sj.eye.6702692
9. Pearson A, Soneji B, Sarvananthan N, Sandford-Smith J. Does ethnic origin influence the incidence or severity of keratoconus? Eye. 2000;14(4):625–628. doi:10.1038/eye.2000.154
10. Kuo IC, Broman A, Pirouzmanesh A, Melia M. Is there an association between diabetes and keratoconus? Ophthalmology. 2006;113(2):184–190. doi:10.1016/j.ophtha.2005.10.009
11. Mazzotta C, Traversi C, Baiocchi S, et al. Corneal healing after riboflavin ultraviolet-A collagen cross-linking determined by confocal laser scanning microscopy in vivo: early and late modifications. Am J Ophthalmol. 2008;146(4):
12. Netto MV, Mohan RR, Ambrósio R
13. Vellara HR, Patel DV. Biomechanical properties of the keratoconic cornea: a review. Clin Exp Optom. 2015;98(1):31–38. doi:10.1111/cxo.12211
14. De Sanctis U, Missolungi A, Mutani B, Richiardi L, Grignolo FM. Reproducibility and repeatability of central corneal thickness measurement in keratoconus using the rotating Scheimpflug camera and ultrasound pachymetry. Am J Ophthalmol. 2007;144(5):
15. Zadnik K, Barr J, Gordon M, Edrington T. Biomicroscopic signs and disease severity in keratoconus. Ophthalmic Lit. 1997;1(50):8.
16. Gorskova EN, Sevost’ianov EN. [Epidemiology of keratoconus in the Urals]. Vestn Oftalmol. 1998;114(4):38–40. (Russian).
17. Jonas JB, Nangia V, Matin A, Kulkarni M, Bhojwani K. Prevalence and associations of keratoconus in rural Maharashtra in central India: the central India eye and medical study. Am J Ophthalmol. 2009;148(5):760–765. doi:10.1016/j.ajo.2009.06.024
18. Assiri AA, Yousuf BI, Quantock AJ, Murphy PJ. Incidence and severity of keratoconus in Asir province, Saudi Arabia. Br J Ophthalmol. 2005;89(11):1403. doi:10.1136/bjo.2005.074955
19. Al-Amri AM. Prevalence of Keratoconus in a refractive surgery population. J Ophthalmol. 2018:5983530.
20. Torres netto EA, Al-Otaibi WM, Hafezi NL, et al. Prevalence of keratoconus in paediatric patients in Riyadh, Saudi Arabia. Br J Ophthalmol. 2018;102(10):1436–1441. doi:10.1136/bjophthalmol-2017-311391
21. Ameerh MAA, Al Refai RM, Al Bdour MD. Keratoconus patients at Jordan University Hospital: a descriptive study. Clin Ophthalmol. 2012;6:1895.
22. Millodot M, Shneor E, Albou S, Atlani E, Gordon-Shaag A. Prevalence and associated factors of keratoconus in Jerusalem: a cross-sectional study. Ophthalmic Epidemiol. 2011;18(2):91–97. doi:10.3109/09286586.2011.560747
23. Owens H, Gamble G. A profile of keratoconus in New Zealand. Cornea. 2003;22(2):122–125. doi:10.1097/00003226-200303000-00008
24. Saro AS, Radwan GA, Mohammed UA, Abozaid MA. Screening for keratoconus in a refractive surgery population of Upper Egypt. Delta J Ophthalmol. 2018;19:19–23. doi:10.4103/DJO.DJO_39_17
25. Al-Mahrouqi HH, Al-Shamli N, Mohan NR, et al. Clinical profile of Omani keratoconus patients: an experience from a tertiary referral centre in Muscat. Oman J Ophthalmol. 2018;11:259–264. doi:10.4103/ojo.OJO_203_2017
26. Nielsen K, Hjortdal J, Aagaard Nohr E, Ehlers N. Incidence and prevalence of keratoconus in Denmark. Acta Ophthalmol Scand. 2007;85(8):890–892. doi:10.1111/j.1600-0420.2007.00981.x
27. Godefrooij DA, de Wit GA, Uiterwaal CS, Imhof SM, Wisse RP. Age-specific incidence and prevalence of keratoconus: a nationwide registration study. Am J Ophthalmol. 2017;175:169–172. doi:10.1016/j.ajo.2016.12.015
28. Saini JS, Saroha V, Singh P, Sukhija JS, Jain AK. Keratoconus in Asian eyes at a tertiary eye care facility. Clin Exp Optom. 2004;87(2):97–101. doi:10.1111/j.1444-0938.2004.tb03155.x
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
