Back to Journals » International Medical Case Reports Journal » Volume 13
Juvenile Xanthogranuloma: Case Report and Literature Review
Authors Vahabi-Amlashi S , Hoseininezhad M, Tafazzoli Z
Received 26 November 2019
Accepted for publication 14 February 2020
Published 25 February 2020 Volume 2020:13 Pages 65—69
DOI https://doi.org/10.2147/IMCRJ.S240115
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas

Sadegh Vahabi-Amlashi, Masoumeh Hoseininezhad, Zahra Tafazzoli
Cutaneous Leishmaniasis Research Center, Mashhad University of Medical Sciences, Mashhad, Iran
Correspondence: Zahra Tafazzoli
Department of Dermatology, Imam Reza Hospital, Ibn e Sina Street, Mashhad, Iran
Tel +98 91 51885344
Fax +98 51 38583845
Email [email protected]
Abstract: Juvenile Xanthogranuloma (JXG) is a relatively uncommon non-Langerhans cell histiocytosis, which often occurs at an early age and is usually asymptomatic. Herein, we present the case of a 17-year-old man with numerous asymptomatic yellow-brown papulonodular lesions with a symmetric distribution on upper and lower extremities, face, and trunk, developed over the past 4 years. In the histopathologic examination, histiocytes with a Touton-like appearance were observed in favor of xanthogranuloma. The patient was treated with isotretinoin 20 mg daily for 2 months, which surprisingly led to the progression of lesions and thus was discontinued. Although JXG may cause severe morbidities in some circumstances, it is a self-limiting benign disorder and patients should be assured regarding the benign self-regressive nature of the disease.
Keywords: non-langerhans-cell histiocytosis, isotretinoin, adult, Juvenile Xanthogranulomas
Introduction
Juvenile Xanthogranuloma (JXG) is a relatively uncommon non-Langerhans cell histiocytosis disorder.1 The lesions usually present as asymptomatic yellow-brown papules and nodules that are mostly self-limited. JXG can present anywhere in the body but primarily occurs as a solitary lesion on the head, the neck, or upper trunk.1 Biopsy of the lesions can reveal the definitive diagnosis. Systemic involvement is rare, which includes the eyes and the lungs and very rarely other organs such as the liver, the spleen, lymph nodes, bones, and gastrointestinal tract.2
JXG with multiple lesions, characterized by more than five lesions, is an uncommon presentation whos lesions usually regress within 1–5 years.3,4 Therefore, the patient should be assured. However, due to the possibility of systemic involvement, it is advisable to perform routine ophthalmologic evaluations.5 Treatments are indicated in case of cosmetic problems or systemic involvement, although their efficacy is still under controversy. These treatments include surgical excision, degenerative lasers, systemic treatments such as retinoid, isotretinoin, cyclosporine, oral corticosteroids, methotrexate, vinblastine, and mercaptopurine.3,6-9 Herein, we present the case of a young man with multiple generalized xanthogranulomas that progressed after isotretinoin treatment.
Case Presentation
A 17-year-old male with a 4-year history of multiple asymptomatic skin lesions was referred to our dermatology clinic. He claimed that the lesions had started form the lower limb, and then gradually spread to other areas of the skin. The patient had no relevant familial or personal medical history.
In examination of the skin, he had numerous asymptomatic yellow-brown, well-defined, soft to stiff, pedunculated papulonodular lesions with variable sizes (up to 15 mm in diameter) and some subcutaneous patterns. The lesions were nearly symmetrically distributed almost all over the body, especially on upper and lower extremities, face, and trunk (Figure 1).
 |
Figure 1 Yellow-brown papulonodular asymptomatic lesions of juvenile xanthogranuloma, at the right leg (A), face (B), right arm (C) before the treatment and left leg (D) after the treatment. |
The examination of mucous membranes, palms, and soles revealed normal findings. However, a pigmented patch with increased hair growth was found on the patient’s back. Ophthalmologic assessment, abdominal ultrasonography, and chest X-ray were obtained, but no extra-cutaneous involvement was detected. However, during physical examination, he appeared to have a marked kyphosis. The initial findings brought up four differential diagnoses: histiocytosis, neurofibromatosis, sarcoidosis, and xanthoma.
A punch biopsy was obtained from a lesion on patient’s arm, which revealed an atrophic epidermis. In addition, in the upper and lower dermis, there were giant histiocytes, mainly of Touton type, as well as some foamy histiocytes with mixed lymphocytic infiltrations, which was extended to subcutaneous tissue (Figure 2). According to the histopathologic findings, the diagnosis of JXG was confirmed for the patient.
Since some lesions were similar to neurofibromatosis type 1 (NF1), the patient’s skin was carefully re-examined. There were no café-au-lait macules; however, a soft nodular lesion resembling a neurofibroma was observed on the back (Figure 3). Evaluation of the excisional biopsy taken from this lesion ruled out NF1 and confirmed the diagnosis of JXG.
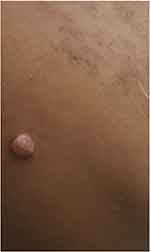 |
Figure 3 Soft nodular lesion resembling neurofibroma, which was observed on the back of the patient. |
Laboratory assessments, including routine hematological tests, liver and renal function tests, serum levels of lipids, erythrocyte sedimentation rate (ESR), and C-reactive protein were normal. Peripheral blood smear was normal.
The patient was treated with daily 20-mg doses of isotretinoin for two months, but ironically, the lesions progressed during the treatment period (Figure 1d). This and other adverse effects of isotretinoin treatment made the patient terminate the treatment. After a one-year follow-up, the patient still had some lesions, but there was a distinctive decline in the size and number of the lesions.
The patient provided written informed consent for publication of his details and images. In addition, no institutional approval was required to publish the case details.
Discussion
Skin lesions of JXG are categorized into the three main forms of small nodular/popular (2–5 mm), large nodular (5–20 mm), and giant xanthogranuloma (>20 mm).10 Lesions usually emerge as painless yellow-red papules that can enlarge up to 10 mm in diameter and develop into plaques.7 In most juvenile cases, lesions regress markedly by a year. However, as in the present case, spontaneous remission is uncommon in adults.11
Due to the potential association between the nodular form of JXG and neurofibromatosis, obtaining a biopsy to rule out the neurofibromatosis seems necessary.10 In our case, since we observed lesions similar to those of NF1 in the patient, we performed an excisional biopsy, which ruled out NF1 and confirmed the JXG diagnosis.
Multiple xanthogranuloma is more prevalent among men.9 It is commonly stated that the majority of JXG cases present with a single papulonodular lesion. However, some studies stated that the number of skin lesions is higher in JXG than in adult xanthogranuloma.6 As of our case, we observed about 15 lesions spread over face, trunk, as well as upper and lower extremities, especially over extensor surface of the joints.
In contrast to what we observed in our patient and in adults with xanthogranuloma, extracutaneous lesions in eyes, lungs, liver, kidneys, testis, gastrointestinal tract and pericardium is common in patients with JXG.3,7,9,12 The most commonly reported extracutaneous presentations of JXG were breast lumps, non-traumatic iritis, hyphema, and gait disturbances, respectively.7 Multiple xanthogranuloma has also been reportedly linked to hematologic disorders including thrombocytosis, B-cell lymphoma, chronic lymphocytic leukemia, and monoclonal gammopathy.13
The characteristic histopathological findings in JXG are Touton giant cells and histiocytes that are laden with lipid.1,14 Typically, a settled lesion represents a mixed pattern of cellular infiltration with histiocytes and white blood cells including lymphocytes, eosinophils, neutrophils, and plasma cells. Although subcutaneous involvement is frequent, epidermal lesions are scarce.7 It is worth mentioning that the Touton giant cells and histiocytes may not appear in the lesions at early stages of the disease, which makes the diagnosis difficult. Thus, an observation of the developed Touton giant cells is not mandatory when making the diagnosis.14 In our case, we observed giant histiocytes mainly of Touton type and some foamy histiocytes with mixed lymphocytic infiltration in the upper and lower dermis extended to the subcutaneous tissue.
Extracutaneous and visceral involvements are rare in multiple adult xanthogranuloma, so that no systemic or aggressive treatment is necessary.9 However, ocular and systemic involvements may regress by radiotherapy, chemotherapy or systemic steroids.6
Evidence suggests a variable response rate for systemic treatments and tumor suppressor drugs.14 Furthermore, due to the self-healing nature of cutaneous JXG lesions, treatment becomes controversial and only indicated for diagnostic or cosmetic purposes.7
However, as spontaneous regression is not common in adults with xanthogranuloma, some studies reported favorable outcomes of systemic retinoids on adult xanthogranulomas.6,15 Retinoids have major effects on cell growth and function, causing anchorage-independent growth, cell adhesiveness, and density-dependent growth.15 On the other hand, clinicians should be aware of their psychological side effects and their hazards for pregnant women.
Achar et al6 reported a 28-year-old male patient with multiple diffuse brown-yellow papulonodular eruptions on his body for one month. Histopathological examination of the skin biopsy specimen revealed features of xanthogranuloma and the patient was treated with isotretinoin 20 mg once daily, which resulted in most of the lesions being subsided or flattened within two months of treatment. However, as multiple adult xanthogranuloma has a good prognosis, the resolution might have been due to the disease trajectory.
Similar to the discussed case, our young patient had multiple yellow-brown papulonodular lesions and received 20 mg of isotretinoin daily for 2 months. However, in stark contrast with the above-mentioned case, not only the lesions did not improve, but also they progressed and even new lesions appeared.
Conclusion
The case of JXG reported here, although typical in his histopathological findings and cutaneous lesions, was unusual for the number of lesions, the age of onset, and the response to treatment.
Since JXG is a self-healing disorder, dermatologists should be aware of the various forms of this disorder to select an appropriate treatment. However, its low incidence has made the diagnosis and management of JXG difficult. Detailed assessment for extracutaneous involvement and continuous follow-up is required, especially in cases with multiple lesions. In the limited form, patients should be assured regarding the benign self-regressive nature of the disease. Further studies are needed to evaluate the efficacy and safety of retinoids on dermatologic JXG lesions.
Disclosure
The authors have no conflicts of interest to disclose in this work.
References
1. Dehner LP. Juvenile xanthogranulomas in the first two decades of life: a clinicopathologic study of 174 cases with cutaneous and extracutaneous manifestations. Am J Surg Pathol. 2003;27(5):579–593. doi:10.1097/00000478-200305000-00003
2. Jezierska M, Stefanowicz J, Romanowicz G, Kosiak W, Lange M. Langerhans cell histiocytosis in children – a disease with many faces. Recent advances in pathogenesis, diagnostic examinations and treatment. Postepy Dermatol Alergol. 2018;35(1):6–17. doi:10.5114/pdia.2017.67095
3. Ferreira BR, Cardoso JC, Reis JP, Tellechea O. Multiple adult-onset xanthogranuloma, an uncommon diagnosis. An Bras Dermatol. 2017;92(2):294–295. doi:10.1590/abd1806-4841.20176216
4. Pradhan S, Chen S, Xiong L. Case reports on Juvenile Xanthogranuloma and brief review of literature. Science. 2017;6(5):82–85.
5. Meyer P, Graeff E, Kohler C, Munier F, Bruder E. Juvenile xanthogranuloma involving concurrent iris and skin: clinical, pathological and molecular pathological evaluations. Am J Ophthalmol Case Rep. 2018;9:10–13. doi:10.1016/j.ajoc.2017.09.004
6. Achar A, Naskar B, Mondal PC, Pal M. Multiple generalized xanthogranuloma in adult: case report and treatment. Indian J Dermatol. 2011;56(2):197–199. doi:10.4103/0019-5154.80416
7. Tan LC, Tan KB, Aw CW. Unusual presentation of adult xanthogranuloma: a case report. Singapore Med J. 2014;55(2):e25–e27. doi:10.11622/smedj.2013207
8. Wood AJ, Wagner MV, Abbott JJ, Gibson LE. Necrobiotic xanthogranuloma: a review of 17 cases with emphasis on clinical and pathologic correlation. Arch Dermatol. 2009;145(3):279–284. doi:10.1001/archdermatol.2008.583
9. Saad N, Skowron F, Dalle S, Forestier JY, Balme B, Thomas L. Multiple adult xanthogranuloma: case report and literature review. Dermatology. 2006;212(1):73–76. doi:10.1159/000089027
10. Caputo R, Grimalt R, Gelmetti C, Cottoni F. Unusual aspects of juvenile xanthogranuloma. J Am Acad Dermatol. 1993;29(5):868–870. doi:10.1016/0190-9622(93)70259-V
11. Lin SJ, Chiu HC. Adult multiple xanthogranulomas with spontaneous resolution. Acta Derm Venereol. 2003;83(2):157–158. doi:10.1080/00015550310007643
12. Mori H, Nakamichi Y, Takahashi K. Multiple Juvenile Xanthogranuloma of the eyelids. Ocul Oncol Pathol. 2018;4(2):73–78. doi:10.1159/000478101
13. Chisolm SS, Schulman JM, Fox LP. Adult xanthogranuloma, reticulohistiocytosis, and rosai-dorfman disease. Dermatol Clin. 2015;33(3):465–472. doi:10.1016/j.det.2015.03.011
14. Janssen D, Harms D. Juvenile xanthogranuloma in childhood and adolescence: a clinicopathologic study of 129 patients from the kiel pediatric tumor registry. Am J Surg Pathol. 2005;29(1):21–28. doi:10.1097/01.pas.0000147395.01229.06
15. Dion LD, Blalock JE, Gifford GE. Retinoic acid and the restoration of anchorage dependent growth to transformed mammalian cells. Exp Cell Res. 1978;117(1):15–22. doi:10.1016/0014-4827(78)90422-6
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

