Back to Journals » Research and Reports in Urology » Volume 14
Ischemic Priapism During Severe SARS-CoV-2 Infection: A Case Report and Literature Review
Authors De Rose AF, Ambrosini F, Genova Gaia L, Mantica G, Terrone C
Received 3 April 2022
Accepted for publication 4 June 2022
Published 23 June 2022 Volume 2022:14 Pages 259—263
DOI https://doi.org/10.2147/RRU.S369221
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Panagiotis J Vlachostergios
Aldo Franco De Rose, Francesca Ambrosini, Luca Genova Gaia, Guglielmo Mantica, Carlo Terrone
IRCCS Ospedale Policlinico San Martino, Genova, Italy
Correspondence: Francesca Ambrosini, Department of Urology - Policlinico San Martino Hospital, University of Genoa, Largo Rosanna Benzi, 10, Genoa, 16132, Italy, Tel +39 3480497079, Email [email protected]
Purpose: Literature on priapism as a concomitant manifestation of COVID-19 infection is scarce since less than 10 cases are reported. It is crucial to determine whether priapism in a COVID-19 patient is related to the infection itself or to the ongoing therapy, especially in those critically ill. Our study aims to create an alert for all physicians faced with the management of priapism in SARS-CoV-2 patients. We tried to explore any potential leading factors presenting a case of priapism arising during COVID-19 pneumonia, and we reviewed the current literature available on this topic.
Case Presentation: We reported the case of a 62-year-old man with severe COVID-19 pneumonia complicated by acute respiratory distress syndrome who developed ischemic priapism during his stay in intensive unit care. Corporal aspiration was performed with injection of 200 μg of intracavernosal phenylephrine resulting in detumescence. After recovery, the patient reported complete erectile dysfunction.
Conclusion: The etiopathogenetic mechanism of priapism remains not completely clear. The most frequently hypothesized cause is the prothrombotic state associated with the infection. Further elements including the drugs administered during the infection may play a crucial role. Further studies are needed to obtain stronger evidence.
Keywords: priapism, erectile dysfunction, COVID-19, respiratory distress syndrome
Introduction
The pandemic caused by SARS-CoV-2 continues to be one of the most serious medical emergencies in recent history affecting millions of people worldwide. The spectrum of symptoms and signs related to the syndrome of the COVID-19 disease is extremely variable.
Among the various clinical manifestations, priapism is certainly rare. Although the definitions of priapism and its outcomes are inconsistent, 1 it is generally accepted to define priapism as a full or partial erection that persists for more than four hours despite cessation of sexual stimulation or unrelated to sexual stimulation.1,2
According to the latest EAU Guidelines,1 priapism can be classified as ischemic (low-flow or veno-occlusive), non-ischemic (high-flow or arterial), and stuttering (recurrent or intermittent), on the basis of the etiology, pathophysiology, and clinical presentation. Ischemic priapism is the most common subtype of priapism, accounting for more than 95% of all episodes,3 and an urgent intervention is mandatory due to the potentially irreparable damage leading to erectile dysfunction with fibrosis of the corpora cavernosa.1
Literature on this topic is scarce since less than 10 cases of priapism in patients with concomitant COVID-19 infection are reported.4–9
Considering the limited evidence available, any attempt to draw clinically meaningful conclusions about aetiology and pathogenesis is challenging. It is crucial to determine whether priapism in a COVID-19 patient is related to the infection itself or to the ongoing therapy, especially in those critically ill.
One of the most corroborated hypotheses is that the prothrombotic state associated with COVID-19 infection10,11 plays a crucial role in the pathogenetic mechanism for ischemic priapism.
We reported a case of ischemic priapism in a patient with severe COVID-19 pneumonia complicated by acute respiratory distress syndrome. We tried to explore any potential leading factors, and we reviewed the current literature available on this topic.
A written informed consent was provided by the patient to have the case details published. Approval from the institutional review board was not required.
Case Report
The case presented is a 62-year-old man, sexually active with the occasional intake of Tadalafil 5mg. His past medical history was unremarkable. In particular, he did not have any thromboembolic risk factors. He had a normal body mass index (BMI), and he did not have a smoking habit.
He presented to the emergency department of our Institution for severe dyspnoea, fatigue, and dry cough. On presentation, his temperature was 39°C, his heart rate was 75 beats/min, respiratory rate was 25/min, blood pressure was 130/75, and SpO2 was 78%. A nasopharyngeal swab specimen was obtained showing SARS-CoV-2 infection.
Due to worsening hypoxia despite the supplemental oxygen, an attempt to continuous positive airway pressure (CPAP) was carried out. A chest CT scan showed diffuse and bilateral ground-glass thickening, negative for pulmonary thrombus embolism. SARS-CoV-2-related pneumonia was diagnosed.
The patient’s condition continued to deteriorate, and he was subsequently treated with supplemental oxygen via a heated high-flow nasal cannula.
Three days after admission, due to worsening respiratory dynamics, the patient required orotracheal intubation after sedation with etomidate, fentanyl, and rocuronium. PCMV (pressure-controlled mechanical ventilation) and prono-supination cycles were started, and sedation was maintained with propofol and fentanyl.
After 21 days, an attempt to extubation failed and a percutaneous tracheostomy was performed.
During the long hospitalization, amine support with norepinephrine had to be set up several times. Moreover, multiple cycles of target antibiotic therapies were administered.
The patient underwent cycles of conventional continuous venovenous hemodiafiltration due to his critical status with acute kidney failure.
From a cardiological point of view, echocardiology showed slight septal hypertrophy with neither pathological dilatation nor valvulopathy nor pulmonary hypertension, normal contractility, and preserved global systolic function.
The patient required blood transfusions and on one occasion a reaction with erythema and hypertensive elevation was recorded.
During the patient stay in intensive unit care (ICU), he was noted to have an erection of unknown duration.
On urological examination, the corpora were approximately 70–80% rigid, without glans tumescence.
At the time of the urological consultation, the patient’s blood tests showed moderate leukocytosis (11.59 x109/l) with neutrophilia (10.20 x109/l), hemoglobinemia 101.0 g/l, hematocrit 29.9%, albuminemia 29.9 g/l, PCR 154.0 mg/l, procalcitonin 9.08 µg/l. The ionogram was regular except for a slight hypermagnesemia (2.9 mg/dl); coagulation tests showed a slight decrease in prothrombin time and aPTT, fibrinogen 6.84 g/l and D-dimer 5600 µg/L.
Ongoing therapy included midazolam 3mg/h, propofol 80mg/h, enoxaparin 4000UI twice a day, fentanyl 0.5 µg/kg/h, rocuronium 5mL/h, furosemide 60mg die to have a diuresis of 150mL/h.
Initial corporal blood gas was consistent with ischemic priapism with pH 7.142, partial pressure of carbon dioxide (PaCO2) 81.8 mmHg, and 19 partial pressure of oxygen (PaO2).
Subsequently, 16-gauge needles were placed in bilateral corpora cavernosa with trans-glandular access, and other 2 blood gas analysis of the corpora cavernosa were carried out (Table 1).
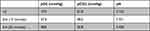 |
Table 1 Cavernosal Blood Gas Analysis |
Corporal aspiration was performed with injection of 200 μg of intracavernosal phenylephrine resulting in detumescence.
Throughout his hospitalization, he experienced no further thromboembolic complications, and priapism did not reoccur.
After 98 days of hospitalization, the patient was discharged with a rehabilitation program and clinical follow-up.
The patient reported complete erectile dysfunction. A dynamic penile US was performed showing normal echogenicity of the corpora cavernosa and regular response to extracavernous injection of Alprostadil 5 mcg, with the satisfactory erection of approximately 40 minutes.
The patient currently achieves a satisfactory erection by taking as needed a phosphodiesterase type 5 inhibitor at minimal dosage.
Hormonal status was assessed demonstrating luteinizing hormone 5.37 U/L, follicle-stimulating hormone 20.5 U/L, testosterone 352 ng/dL.
Discussion
Priapism is a rare entity and the literature lacks strong evidence since most of the data available result from retrospective, heterogeneous, incomplete, and limited cohorts of patients. The etiological causes of priapism are extremely varied.
The knowledge regarding priapism during COVID-19-infection is currently limited, accounting for less than 10 cases reported in the literature.
In our case, the patient presented with ischemic priapism as in all the other reports available.
All the Authors reported the diagnosis of ischemic priapism by penile blood gas analysis and in some cases penile US.5,8,12 In one case, no laboratory or radiological methods were used, and the diagnosis was made on clinical examination.4
There is still considerable controversy regarding the pathophysiology of priapism during the COVID-19 infection. One of the most plausible hypotheses involves the prothrombotic state associated with the SARS-CoV-2 which can partly justify the onset of ischemic priapism.
The alteration in the thrombotic/fibrinolytic balance due to the pro-inflammatory cytokine storm triggered by the infection leads to endothelial dysregulation. Thus, thrombotic complications are frequent and may involve both the arterial and venous beds in multiple anatomical areas.11
In the reports available in the literature, most of the authors suggested this theory to justify priapism.4,7–9,12
Carreno et al reported a case of ischemic priapism in a 29-year-old male, with obesity and a severe Covid-19 clinical presentation. The authors hypothesize that even the propofol administration during the hospitalization in the intensive care unit may be a leading factor to priapism, as in the experience of Vesta et al.12,13
Moreover, it is worthwhile noting that most of the cases reported in the literature had severe Covid-19 disease, requiring admission to the intensive care unit.4–8,12 Some patients suffered exitus during hospitalization.4,8,12
On the contrary, in one case, the patient had an asymptomatic SARS-CoV-2 infection except for anosmia, with no other risk factor for priapism.9 His medical history was unremarkable, and he did not habitually use any pharmacological treatment.9
Considering our patient’s sedation during his ICU stay, we could not assess the presence of pain, which is typically present in ischaemic priapism.
Based on the pathophysiology, we hypothesize that coagulopathy secondary to COVID-19 infection may have led to obstruction of draining venules, resulting in low-flow priapism. Moreover, we hypothesized that propofol and enoxaparin may have played a role, as reported in previous studies.13,14
In particular, some authors believed that either a possible formation of heparin-related anti-platelet antibodies or incomplete prophylaxis of thromboembolism, especially in severe SARS-CoV-2 infection, may lead to the development of ischemic priapism.4,5
Intravenous dexmedetomidine administration could be a protective factor for the onset of priapism given its selective α2-adrenoreceptor agonist action, although further studies are needed.2,15
Our report has important limitations. First, the knowledge on this topic is severely limited, and further prospective multicentric studies would be needed to draw stronger conclusions. Furthermore, the patient received a timely urological intervention, but the exact time of priapism onset was not available, probably impacting on clinical outcomes.
Conclusion
Our study aims to create an alert for all physicians faced with the management of priapism in SARS-CoV-2 patients. In the SARS-CoV-2 patient, the most frequently hypothesized cause is the prothrombotic state associated with the infection. Further elements including the drugs administered during the infection may play a crucial role. Further studies are needed to strengthen the evidence.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Consent for Publication
The patient signed a specific informed consent with permission to use clinical and instrumental data for research publication.
Acknowledgments
We thank the multidisciplinary teams of our Institutes for their expertise and assistance throughout all aspects of our study.
Funding
The authors have no financial support.
Disclosure
The authors have no conflict of interest to declare in this work.
References
1. EAU guidelines [Internet]; 2021. Available from: http://uroweb.org/guidelines/compilations-of-all-guidelines/.
2. Bivalacqua TJ, Allen BK, Brock G, et al. Acute ischemic priapism: an AUA/SMSNA guideline. J Urol. 2021;206(5):1114–1121. doi:10.1097/JU.0000000000002236
3. Broderick GA, Kadioglu A, Bivalacqua TJ, Ghanem H, Nehra A, Shamloul R. Priapism: pathogenesis, epidemiology, and management. J Sex Med. 2010;7(1 Pt 2):476–500. doi:10.1111/j.1743-6109.2009.01625.x
4. Lam G, McCarthy R, Haider R, Peculiar A. Case of priapism: the hypercoagulable state in patients with severe COVID-19 infection. Eur J Case Rep Intern Med. 2020;7(8):001779. doi:10.12890/2020_001779
5. Grimberg DC, Tejwani R, Allkanjari A, Forrester MT, Kraft BD, Kaye DR. Ischemic priapism due to coagulopathy of severe COVID-19 infection. J Clin Urol. 2021;27:205141582110259. doi:10.1177/20514158211025914
6. Addar A, Al Fraidi O, Nazer A, Althonayan N, Ghazwani Y. Priapism for 10 days in a patient with SARS-CoV-2 pneumonia: a case report. J Surg Case Rep. 2021;2021(4):rjab020. doi:10.1093/jscr/rjab020
7. Lamamri M, Chebbi A, Mamane J, et al. Priapism in a patient with coronavirus disease 2019 (COVID-19). Am J Emerg Med. 2021;39:
8. Silverman ML, VanDerVeer SJ, Donnelly TJ. Priapism in COVID-19: a thromboembolic complication. Am J Emerg Med. 2021;45:
9. Giuliano AFM, Vulpi M, Passerini F, et al. SARS-CoV-2 infection as a determining factor to the precipitation of ischemic priapism in a young patient with asymptomatic COVID-19. Case Rep Urol. 2021;2021:9936891. doi:10.1155/2021/9936891
10. Ali MAM, Spinler SA. COVID-19 and thrombosis: from bench to bedside. Trends Cardiovasc Med. 2021;31(3):143–160. doi:10.1016/j.tcm.2020.12.004
11. Libby P, Lüscher T. COVID-19 is, in the end, an endothelial disease. Eur Heart J. 2020;41(32):3038–3044. doi:10.1093/eurheartj/ehaa623
12. Carreño BDV, Perez CP, Vasquez D, Oyola JA, Suarez O, Bedoya C. Veno-occlusive priapism in COVID-19 disease. Urol Int. 2021;105(9–10):916–919. doi:10.1159/000514421
13. Vesta KS, Martina SD, Kozlowski EA. Propofol-induced priapism, a case confirmed with rechallenge. Ann Pharmacother. 2006;40(5):980–982. doi:10.1345/aph.1G555
14. Lin PH, Bush RL, Lumsden AB. Low molecular weight heparin induced priapism. J Urol. 2004;172(1):263. doi:10.1097/01.ju.0000132155.38285.8e
15. Guler G, Sofikerim M, Ugur F, Aksu R, Boyaci A. Intravenous dexmedetomidine for treatment of intraoperative penile erection. Int Urol Nephrol. 2012;44(2):353–357. doi:10.1007/s11255-011-0023-x
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
