Back to Journals » Clinical Ophthalmology » Volume 17
Investigating the Ocular Surface Microbiome: What Can It Tell Us?
Authors Peter VG, Morandi S C, Herzog EL, Zinkernagel MS, Zysset-Burri DC
Received 1 October 2022
Accepted for publication 10 January 2023
Published 19 January 2023 Volume 2023:17 Pages 259—271
DOI https://doi.org/10.2147/OPTH.S359304
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Virginie G Peter,1 Sophia C Morandi,1,2 Elio L Herzog,1– 3 Martin S Zinkernagel,1,2 Denise C Zysset-Burri1,2
1Department of Ophthalmology, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland; 2Department for BioMedical Research, University of Bern, Bern, Switzerland; 3Graduate School for Cellular and Biomedical Sciences, University of Bern, Bern, Switzerland
Correspondence: Virginie G Peter, Department of Ophthalmology, Inselspital, Bern University Hospital, University of Bern, Freiburgstrasse 15, Bern, 3010, Switzerland, Email [email protected]
Abstract: While pathogens of the eye have been studied for a very long time, the existence of resident microbes on the surface of healthy eyes has gained interest only recently. It appears that commensal microbes are a normal feature of the healthy eye, whose role and properties are currently the subject of extensive research. This review provides an overview of studies that have used 16s rRNA gene sequencing and whole metagenome shotgun sequencing to characterize microbial communities associated with the healthy ocular surface from kingdom to genus level. Bacteria are the primary colonizers of the healthy ocular surface, with three predominant phyla: Proteobacteria, Actinobacteria, and Firmicutes, regardless of the host, environment, and method used. Refining the microbial classification to the genus level reveals a highly variable distribution from one individual and study to another. Factors accounting for this variability are intriguing - it is currently unknown to what extent this is attributable to the individuals and their environment and how much is artifactual. Clearly, it is technically challenging to accurately describe the microorganisms of the ocular surface because their abundance is relatively low, thus, permitting substantial contaminations. More research is needed, including better experimental standards to prevent biases, and the exploration of the ocular surface microbiome’s role in a spectrum of healthy to pathological states. Outcomes from such research include the opportunity for therapeutic interventions targeting the microbiome.
Keywords: ocular surface, ocular surface microbiome, 16s rRNA gene sequencing, whole metagenome shotgun sequencing
Introduction
The role of the ocular surface microbiome (OSM) in health and disease of the underlying tissue is increasingly receiving attention, and knowledge in the field is expanding rapidly.1 Among others, following features were identified that warrant further attention. (1) In humans and selected model organisms, the ocular surface (OS) microbiota may play a role in shaping local and systemic immune responses.2,3 (2) There seems to be a resident OSM.4 (3) The OS microbiota participates in the defense against pathogenic invaders through nutrient and niche competition.5 (4) The OSM composition could be influenced by host, environmental and iatrogenic factors; OSM disbalance, called dysbiosis, seems to be associated with a variety of OS and systemic disorders.6 (5) This offers the opportunity to modulate the OSM homeostasis to improve ocular health.7–9 Today, we are still at an early stage in OSM research and these questions are subject to active investigation. This review provides an up-to-date picture of the knowledge on OSM composition, with emphasis on bacterial, viral, and fungal diversity at the conjunctiva as well as encountered technical challenges. Microbiome research has made impressive advances in recent years. It was in the 1670s that bacteria living in humans were observed and described as “little living animalcules” for the first time. Compared to other human microbiomes of the gut, skin, vagina, oral and nasal cavities, the OSM is unique due to its sparse microbial colonization, which makes it particularly challenging to analyze. The first reports about the presence of an OSM are based on culture-dependent methods.10–13 Technological advances, especially modern sequencing technologies have enabled a high-throughput and broad characterization of microbiomes. The term microbiome refers to all microbes, including bacteria, viruses, archaea and eukaryotes, and their genetic material in a defined environment. This term should be distinguished from microbiota, which describes the microbes present in a defined niche.
The OS as a Microbial Niche and Its Microhabitats
The OS is continuously exposed to the environment, to microbes and microparticles with potential infectious, toxic or allergenic effects. Yet it hosts an unusually low microbial load compared to other barrier surfaces and mucosae. This highlights the presence of efficient protection mechanisms at the OS in homeostasis, with balanced immune responses and autoimmunity. Initial mechanical protective mechanisms include blinking and the tear reflex, as well as chemical defense provided by antimicrobial molecules in the tear film.14 These antimicrobial tear proteins, including lysozyme, lactoferrin, mucins, defensins, interleukins and other antimicrobial peptides, act through various mechanisms such as lethal or growth inhibitory antimicrobial activity and immunomodulatory effects. An additional line of defense is mediated by the conjunctiva-associated lymphoid tissue (CALT). CALT harbors a diverse repertoire of immune cells including immune competent cells, secretory Immunoglobulin A and lymphocytes.15,16 Additionally, recent findings indicate that resident bacteria on the OS could inhibit the growth of invading pathogens through mutual regulation, as has been observed in other mucosal niches as well.5,17,18 As previously reviewed, there are dedicated anatomical structures and mechanisms to prevent excessive immune reactions.6 A key feature seems to be the physical barrier separating microbes from the host’s exposed surface, the epithelium, which itself is a pivotal activator of innate and adaptive immune responses. Structures involved in this barrier include the tear film mucus, antimicrobial peptides, secreted immunoglobulins and immune cells. At the OS, different microhabitats with specific anatomical and physiological properties can be distinguished, which may also harbor different flora: the cornea; the limbal, bulbar, tarsal, and fornical conjunctiva; and the lid margin.19,20 In summary, the OS composed of separate microhabitats, has evolved specific protective mechanisms that exert significant selection pressure on the resident microbiota. This raises the question of whether the OS microbiota have specific properties to survive and outcompete other invading microbes. Consequently, the conjunctiva cannot be simplified as a sparse version of other mucosae; instead, an inherent microbial population of OS is to be expected.
Technical Challenges in Characterizing the Low Abundant OSM
Culture-based methods represent a long established and well-described procedure for the identification of commensal bacteria and fungi.10–13,21 Cultures have the advantage of isolating living microbes only.22 In contrast, they have the major drawback of being time-consuming and unfit to describe and quantify the vast composition of complex microbiomes.23 Indeed, bacterial cultures were initially developed to grow specific pathogens and generate pure cultures for further investigations. A majority of environmental bacteria, though, are not easily cultured, making this method inadequate for the characterization of novel microbiomes being continuously exposed to the environment.24–27 The advent of modern sequencing technologies has enabled more extensive microbiome characterization. 16s rRNA gene sequencing has been the most used sequencing technology in microbiome research so far. With regard to low abundance microbiomes, this method has the advantage of selecting and amplifying the input material by PCR before sequencing, namely the 16s rRNA gene found in bacteria. This amplification step has the drawback of introducing biases to an extent that depends on the initial template concentration, DNA extraction method and number of PCR cycles used.28–33 Sequencing of the 16s rRNA gene is aimed to target only bacteria, thus omitting other kingdoms, which represents another limitation. Whole metagenome shotgun sequencing is an emerging sequencing technology. Compared to 16s rRNA gene sequencing, it provides a more comprehensive picture of the taxonomic composition and offers the possibility to study functional profiles of microbiomes. Whole metagenome shotgun sequencing consists of parallel sequencing of a sample’s fragmented DNA, whose sequences are then assembled into longer reads and mapped to a database of reference sequences. This method bypasses some of the issues of 16s rRNA gene sequencing since there is no target gene amplification, although a global amplification step may be included in cases of low input DNA content. Its major benefit is the sequencing of DNA regardless of its origin, thus enabling detection of viruses, archaea and eukaryotes, in addition to bacteria. Furthermore, whole metagenome shotgun sequencing increases taxonomic resolution and provides deeper genomic information.34,35 The broader distribution of marker sequences in target genomes has the drawback of increasing the sensitivity of this method to short random DNA contaminations. This might result in artifactual identification of microbial species, especially in low abundance microbiomes.36 Both 16s rRNA gene sequencing and whole metagenome shotgun sequencing do not provide absolute quantification of microbial DNA. This can instead be obtained by qPCR of unspecific 16s rRNA genes, enabling an absolute quantification of bacterial load.37,38 Meta-analyses are essential for understanding the highly variable results from studies on low abundant microbiomes, but the lack of standardized procedures in such studies make these analyses very difficult.33 Well-designed controls are necessary to eliminate false positive results and to detect biases introduced during the sampling, DNA extraction and sequencing steps. Negative controls should be included to control sterile working conditions. It seems that contamination originating from the extraction kits represents, among others, an important source of false positive results, especially when working with DNA at low concentrations. It was shown that DNA extraction kits contain a “kitome”-A term describing the genetic material originating from DNA extraction kits, library preparation kits and their solutions, which differs from one production lot to another.36 To account for systematic biases, positive controls with known microbial composition would be beneficial. Such controls recently became commercially available and include among others a standard from ZymoBiomics comprising fungal and bacterial DNA from a range of gram-positive and gram-negative bacteria with varying GC content (ZymoBiomics Microbial Community Standard, Zymo Research Corp., Irvine, CA, United States). To our knowledge, there is no microbial community standard available containing bacterial, fungal, as well as viral DNA. However, the latter would be relevant since viruses have been detected on the OS as well.4,39,40 In samples with a small amount of target DNA, host DNA depletion or microbiome enrichment should be considered.41,42 Host DNA depletion aims to increase the relative concentration of target DNA as well as to eliminate free DNA originating from dead cells. One study addressed the efficiency of different target DNA enrichment methods and found an up to ten-fold increase in relative bacterial DNA content by selective host cell lysis.43 An increase in target DNA compared to host DNA improves sequencing read quality and decreases sequencing cost by reducing the total amount of reads needed. In summary, research on low-abundance microbiomes progresses with the introduction of modern sequencing technologies but lacks experience and standardization. Well-designed experiments including positive and negative controls, host DNA depletion and absolute quantification of microbial DNA are needed in future studies to improve reproducibility and comparability.
Microbial Flora at the Ocular Surface
A core microbiome is generally described as a set of microbial taxa that are characteristic of a specific host or environment, although its definition and quantification is still subject to debate.6,44 The exact composition of the ocular microbiota of the healthy eye is difficult to characterize due to the technical and analytical challenges mentioned earlier, leading to varying results depending on the methods and protocols used. In addition, host and environmental factors can influence the composition of the microbial flora, complicating the standardization of studies in humans. Here we attempt to highlight some constant and variable features of the OSM from recent studies published in the scientific literature. First, the scientific community tends to agree that the OS contains fewer microbes than other human microbial niches. The term “paucimicrobial” has been used to describe this sparse microbial colonization, although it lacks a precise definition. Traditional culture techniques originally identified few bacteria and fungi on the OS.45–47 More recently, a study measured the bacterial mass at the conjunctiva, facial skin and buccal mucosa in healthy adults using 16s gene quantitative PCR. It was reported that 0.05 bacteria were detectable per conjunctival cell, corresponding to less than 40 bacteria per conjunctival swab. In comparison, there were approximately 150-fold more bacteria on the facial skin or buccal mucosa than at the conjunctiva. Furthermore, there were approximately 2 times more bacteria present at the lower than at the upper conjunctiva. In terms of bacterial load, there were no statistically significant differences between men and women, right and left eye, and subjects younger than 30 years and older than 60 years old.4 To get an overview of the major kingdoms detected on the OS, we searched the literature using PubMed for studies that performed whole metagenome shotgun sequencing of the OSM in which numerical data were available on the relative abundance of major kingdoms at the OSM of healthy subjects. Five studies matching these criteria show that bacteria account for the great majority of the OSM (average 91%, median 93%, range [78–98%]), followed by viruses (average 5%, median 1%, range [1–7%]), and fungi or other eukaryotes (average and median 4%, range [0.02–20%]) (Figure 1).39,48–51 Of note, bacterial DNA was detected in all participants in these studies, while fungi and viruses were not. For instance, in one study, fungi and viruses were detected in 35% and 41% of subjects, respectively.49 For comparison, the skin is mainly colonized by bacteria, followed by viruses (< 1/4) and eukaryotes (< 1/10), with frequencies varying by anatomical location and individual.52
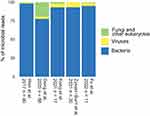 |
Figure 1 Relative composition of major kingdoms on human conjunctiva (% of microbial reads), based on 5 studies using the metagenomic shotgun technique, showing an abundant number of bacterial reads (average 91%, median 93%, range [78–98%]), less viral reads (average 5%, median 1%, range [0–20%]), and minimal fungal or other eukaryotic reads (average 4%, median 4%, range [1–7%]). References: Fu et al 2022;51 Zysset−Burri et al 2021;39 Kang et al 2021;49 Deng et al 2020;48 Wen et al.50 |
Bacterial Composition of the OSM
To get an overall picture of the most abundant bacterial taxa on the OS, we performed a literature search in PubMed that included studies on OSM using sequencing (16s rRNA gene or whole metagenome shotgun sequencing) and in which numerical data on the relative abundance of bacterial taxa were available. Studies including fewer than 11 individuals were excluded. 17 publications featuring 18 cohorts of healthy individuals, including 2 pediatric, met these criteria.4,39,49,51,53–65 Of the available data, relative abundances were reported in at least 2 different cohorts for 20 genera, as shown in Figure 2A. Data from conjunctival samples in one study were provided to us by one of the present co-authors.39 Note that in most papers but not all, data were available if bacterial taxa were detected with a relative frequency of > 1%; for convenience, we excluded those with a relative frequency of < 1%. To give a measure to the most abundant bacterial taxa, we calculated weighted average and median values considering the frequency with which different taxa were reported, thus accounting for possible “outliers” like bacterial taxa that are very abundant in a minimal number of studies.1 In the following, the weighted average and median (WA and WM) therefore refer to average and median values multiplied by the proportion of datasets in which a given taxon is reported with an abundance of > 1% among the 18 cohorts considered. Globally, the most abundant genera were Corynebacterium (data availability 17/18, average and WA 11%, median and WM 9%) and Pseudomonas (data availability 9/18, average 19%, WA 10%, median 18%, WM 9%), followed by Staphylococcus (data availability 13/18, average 6%, WA 5%, median 6%, WM 4%), Streptococcus (data availability 9/18, average 7%, WA 4%, median 4%, VM 2%), Acinetobacter (data availability 10/18, average 6%, WA 3%, median 6%, WM 3%), Propionibacterium (data availability 7/18, average 8%, WA 3%, median 5%, WM 2%), Bacillus (data availability 5/18, average 10%, WA 3%, median 8%, WM 2%), Agrobacterium (data availability 2/18, average 17%, WA 2%, median 17%, WM 2%), Sphingomonas (data availability 5/18, average 4%, WA 1%, median 3%, WM 1%), Cutibacterium (data availability 3/18, average 7%, WA 1%, median 5%, WM 1%), and Enhydrobacter (data availability 3/18, average 6%, WA 1%, median 4%, WM 1%). Less abundant genera that have been reported in at least two cohorts include, by order of abundance, Chryseobacterium, Rothia, Massilia, Moraxella, Neisseria, Paracoccus, Ralstonia, Pedobacter, and Prevotella. At the phylum level, Proteobacteria (data availability 15/15, average 45%, median 52%, range [15–65%]), Actinobacteria (data availability 15/15, average 23%, median 17%, range [5–60%]), and Firmicutes (data availability 15/15, average 19%, median 17%, range [2–45%]) were the most prevalent phyla identified in all studies regardless of the sequencing method (Figure 2B). Other common phyla are Bacteroidetes (data availability 12/15, average 6%, median 5%), Cyanobacteria (data availability 5/15, average 3%, median 1%), and Deinococcus Thermus (data availability 4/15, average 1%, median 1%). Although there is currently no consensus regarding the presence of a core OSM, it appears from these data that the genus Corynebacterium is systematically detected in the studies and is quite abundant on average, although it is not ubiquitously detected when individual subjects are considered. In a study that included negative environmental controls, Corynebacterium was also the taxon that showed the highest enrichment in the conjunctiva when compared with the environmental controls, followed by Propionibacteria, Staphylococcus, and Streptococcus among others.4 Among the 18 datasets, Pseudomonas appeared to be very abundant only in a subset of the studies (55%). When compared to environmental negative controls, Pseudomonas displayed a poor conjunctival enrichment in one study.4 Previous culturing studies commonly isolated Coagulase-negative Staphylococci species (predominantly S. epidermidis and S. aureus), as well as Propionibacterium, Corynebacterium, and Streptococcus.12,45,47,66–70 These genera were also detected by sequencing, although the results obtained by culturing differed in that a vast majority of coagulase-negative Staphylococci were isolated, which does not appear to be the case from sequencing studies. This difference highlights one of the drawbacks of culturing, that facilitates the growth of bacteria adapted to the given culture conditions. However, data from culturing provide an important additional layer of evidence for those bacteria whose growth was previously demonstrated, as culturing has the advantage of isolating viable bacteria. To compare the OSM depending on its sampling location, two studies compared the bacterial composition of the conjunctiva with that of the lid margin and periocular skin, which revealed significant differences in microbial community structure. Indeed, Proteobacteria were present at all sites and predominated at the conjunctiva, whereas Firmicutes were more prevalent and predominant on the periocular skin (45%) and at the lid margin (53%).19,71 Moreover, the Shannon diversity index, a metric used to characterize the overall species diversity, differed significantly between sites and was highest at the skin and lowest at the conjunctiva. One of these studies further addressed the difference between two conjunctival sites: limbus and fornix, showing no significant differences in bacterial community.19 In summary, based on the studies characterizing the composition of the OSM so far in up to 89 healthy subjects, there is currently no definition of the core ocular microbiota. Further studies with large sample sizes under standardized conditions are required to validate the current findings and account for this high variability. Furthermore, the OSM from healthy individuals may be compared to the OSM from patients with eye diseases. However, this topic lies outside the scope of this review and the data are still limited.
 |
Figure 2 The relative abundance of ocular surface bacteria in healthy individuals at (A) Genus and (B) Phylum-level, as reported in 18 datasets from 17 publications. The classification of bacterial taxa is indicated with different colors. Two pediatric cohorts are included. At Genus level, Corynebacterium was most frequently reported with a relative frequency of > 1% (17/18), followed by Staphylococcus (13/18), Acinetobacter (10/18), Pseudomonas (9/18), and Streptococcus (9/18). At the Phylum level, the relative abundance of Actinobacteria (15/15), Proteobacteria (15/15), and Firmicutes were available in all datasets; those of Bacteroidetes (12/15), Cyanobacteria (5/15), and Deinococcus Thermus (4/15) were only available in a subset of the datasets. References: Fu et al 2022;.51 Zysset−Burri et al 2021;39 Kang et al 2021;49 Zhang et al 2021;64 Liang et al 2021;60 Andersson et al 2021;53 Dong et al 2019;55 Li et al 2019 (n= 54);59 Li et al 2019 (n= 23);58 Yau et al 2019;62 Butcher et al 2017;54 Ham B et al 2018;56 Ozkan et al 2017;61 Zhang et al 2017;63 Doan et al 2016;4 Huang et al 2016;57 Zhou et al 2014 (adult and paediatric cohorts).65 |
Viruses at the OS
Virus is the second most detected kingdom on the healthy OS so far.39,48–51 Yet there is little information on the composition and function of the OS virome, a term referring to the set of all viruses in a community and their genetic material. An important increase of interest on this topic has occurred during the SARS-CoV-2 pandemic as conjunctivitis was the most diagnosed ophthalmic disease among COVID-19 patients.72 Studies searching for the presence of SARS-CoV-2 virus in tears have yielded widely variable results, with positive rates ranging from 0% to 72%, and the question whether ocular transmission of SARS-CoV-2 is possible is still debated.73,74 Additionally, it has been shown that resident viruses of the OS were involved in the pathogenesis of ocular adnexal neoplasia. The Human papilloma virus (HPV) associated with conjunctival papilloma and squamous cell carcinoma is a typical example; another is Merkel cell polyomavirus (MCV) associated with Merkel cell carcinoma.75,76 It appears that the OS virome may be important not only in disease but also in maintaining OSM homeostasis. In the studies summarized below, the three methods used for viral detection include whole metagenome shotgun sequencing, Biome representational in silico karyotyping (BRiSK) and viral-directed PCR. It is important to note that none of these three techniques can detect RNA viruses; this requires RNA sequencing, which has not been addressed in studies to date. Microbial interactions are crucial for the sustainability of various ecosystems, including the interplay between species not only within the same kingdom but also between different kingdoms.77 For instance, interactions between viruses and bacteria lead to the modulation of the antiviral immune response and thus influence the viral infectivity.78 On the other hand, bacteria-infecting viruses, called bacteriophages (phages), are one of the main regulators of bacterial population density and distribution. A review states that every 48 hours 50% of all bacteria on earth are killed by phages.79 This efficiency to control bacterial population by phages highlights their relevance in ecosystems and makes phages attractive for therapy, for instance as alternative to antibiotics.80 Recent results in gut microbiome research suggests that the relationship between phages and their bacterial hosts might be rather mutualistic than competitive.79 As phages depend on the survival of their bacterial host, they can contribute to bacterial fitness through various mechanisms through phage “morons”. Morons are independent DNA elements within the phage genomes introduced through horizontal gene transfer.81,82 There is evidence that phages are present at the OS as well. Indeed, in one study applying whole metagenome shotgun sequencing to healthy conjunctival samples from 17 individuals, phages of the genera Siphoviridae were among the 15 microbial genera detected with a relative abundance of more than 1%.49 In this study, the relative abundance of viruses was on average 5% and the positive rate for viruses 41%. Two other viral genera were Anelloviridae and Alphatorquevirus. The family Anelloviridae include the genus Alphatorquevirus, to which the Torque teno virus (TTV) genotypes belong.49 Interestingly, occurrence of TTV in vitreous fluid has been associated with seasonal hyper acute pan uveitis, and another study indicates that TTV triggers an adaptive immune response.83,84 In one study, TTV was also identified in all seven culture-negative endophthalmitis samples versus 57.1% of the fourteen culture-positive samples, whereas no TTV was found in the control group of seven subjects with non-inflamed eyes.40 Another study also detected TTV in 86.3% of 80 healthy conjunctival samples using BRiSK and confirmed for 65% of the samples by directed quantitative PCR. As TTV was the predominant virus found in this study, it was hypothesized that TTV may be an overlooked or unknown resident virus of the OS. Two other viruses, namely the Multiple Sclerosis–associated retrovirus and Human Endogenous Retrovirus K were found in 86.3% of all samples with BRiSK.4 The clinical significance of this result is unclear, as these represent known human endogenous retroviruses and thus likely originated from sequencing of host DNA.85 Following three viruses were identified with a very low positive rate (2/80 samples) and their significance is unclear: MCV, HPV, and Abelson murine leukemia virus. Another study detected elevated levels of MCV, TTV, and HPV in healthy anophthalmic conjunctiva compared to the conjunctiva in healthy eyes.86 According to the researchers, these results suggest that enucleation and prosthesis placement may affect the OS viral microbiome. Due to the oncogenic nature of MCV, understanding the mechanisms by which the OS regulates this virus may have clinical importance. In general, deciphering the viral and fungal as well as bacterial constituents of the healthy OS may be crucial for understanding OSM homeostasis. The pathogenic and oncogenic characteristics of certain microbes found on the healthy OS underline the clinical relevance of this research.
Fungi at the OS
Only a minor proportion of the OSM is attributed to eukaryotes, most of which are fungi.39,48–51 Since fungi are pathogens in ocular diseases like blepharitis, conjunctivitis, keratitis and endophthalmitis,87 several studies about fungi at the ocular surface exist. However, only a limited number of studies have attempted to investigate the fungal OSM in healthy human eyes. Attention has been brought to this matter by the discovery that individuals developing fungal keratitis have an altered bacterial composition not only at the surface of the affected eye but also at the fellow non-affected eye when compared to healthy subjects’ eyes. This observation suggests that bacterial composition influences susceptibility to fungal infection.88 Here we focus on fungi possibly associated with the healthy conjunctiva and review the first attempts to define a core fungal microbiome. Although other eukaryotes are known to cause OS disease such as Acanthamoeba, studies in this regard are very limited.89 Traditional culture techniques and sequencing methods (whole metagenome shotgun sequencing and amplicon sequencing) have led to discordant results about the composition and function of the fungal microbiome. For fungal amplicon sequencing, the internal transcribed spacer (ITS) region is used as a sequencing target.52 When compared to sequencing, the culture-dependent method identifies a reduced spectrum of fungi, as many fungi are not cultivable.90 Cultivation also shows a lower positivity rate (proportion of samples in which fungi are detected) than sequencing. Two studies compared the results obtained from cultivation to ITS2 amplicon sequencing in the same healthy individuals. In these studies, cultivation detected only 1 to 4 genera with a positivity rate of 8.90% to 12.50%, whereas amplicon sequencing detected 65 to 94 genera with a positivity rate of 40% to 73.50%.91,92 Overall, the positivity rate for fungi at the OS based on the culture technique varies between 3% to 28% in different studies.92 The identification of fungi by the sequencing method also has its limitations as many fungi are under-represented in the databases and therefore remain unclassifiable.93 Secondly, confirming that a fungus identified by sequencing is not artifactual at the investigated site is difficult. Furthermore, discordant results are obtained from the two different sequencing methods (whole metagenome shotgun sequencing and amplicon sequencing), implying that an accurate representation of the true fungal composition at the OS is not attained.49 A study using whole metagenome shotgun sequencing showed a lower positivity rate for fungi compared to amplicon sequencing (35% vs 40% to 73.50%) and detected only two phyla (Ascomycota and Basidiomycota) out of four that had been found on the OS with ITS2 so far.49 It has been hypothesized that this difference is due to the short read lengths generated by whole metagenome shotgun sequencing which makes the eukaryotic genome challenging to assemble, as it is larger, more complex, and richer in repeats compared to prokaryotic genomes.94 These issues should be considered in future whole metagenome shotgun sequencing studies of the OSM. ITS has been formally proposed for adoption as the primary fungal barcode marker to the Consortium for the Barcode of Life and might currently be the best method to specifically capture the ocular surface fungal core and transient microbiota.95 Fungi that have been identified at the OS using cultivation include Alternaria sp., Fusarium sp., Aspergillus niger, Aspergillus flavus, Curvularia sp., Penicillium sp., Helminthosporium sp., Candida albicans, Candida guilliermondii, Candida parapsilosis, Saccharomyces cerevisiae, Hormodendrum sp., and Rhodotorula rubra.91 In a study using ITS2 amplicon sequencing to characterize fungi on the eyes of 17 healthy adults living in the southern part of India, 12 to 24 genera per microbiome were identified, making a total of 65 distinct genera. The two dominant phyla were Ascomycota (mean abundance (MA): 47.74%) and Basidiomycota (MA: 26.87%) followed by Zygomycota (MA: 0.08%) (in two eyes). The 4 genera Aspergillus (MA: 21.05%), Setosphaeria (MA: 14.97%), Malassezia (MA: 7.37%) and Hematonectria (MA: 2.73%) were present in all eyes in which fungi were detected. There was no difference in alpha diversity between the left and the right eye and sex had no influence, whereas alpha diversity was altered by age.91 Using the same method, another study on healthy eyes including 45 healthy adults from an urban community in the Shandong Province in China detected 4 phyla, the most abundant being Basidiomycota (MA: 78.67%) and Ascomycota (MA: 19.54%), followed by Zygomycota (MA: 0.13%) and Neocallimastigomycota (MA: 0.01%). In total, 94 genera were identified, among which 51 were identified in at least two individuals, while the remaining 43 were detected only once. Overall, only Malassezia accounted for a relative abundance >1% in each individual. Malassezia is a major component of the skin microbiome.96 “Core” fungal taxa of the healthy OS, defined by an abundance of at least 0.01% in more than 80% of the participants, included Basidiomycota and Ascomycota at the phylum level and Malassezia (MA: 74.65%), Rhodotorula (MA: 1.93%), Davidiella (MA: 1.89%), Aspergillus (MA: 1.25%) and Alternaria (MA: 0.61%) at the genus level.92 Taken together, Basidiomycota and Ascomycota were the most abundant phyla on healthy eyes according to studies using sequencing, despite variable abundances. Relative abundance and distribution of the dominant genera varied significantly among individuals within and in between the studies. More studies will be necessary to confirm our knowledge about commensal and transient ocular surface fungal microbiome composition and function, as well as influencing factors such as sex, age, occupation, environment, season and geographic location.
The OS Microbiome in the Context Its Host’s Immunity and Tear Proteome
Human microbiomes are diverse and vary from one host to another because of a series of factors. The gut microbiome, for instance, is influenced by host factors such as age, sex, genetics, and immune status, as well as by environmental factors such as diet and drugs. In turn, human microbiomes have an impact on the host’s health, including ocular health.97 Indeed, it was recently pointed out that compositional and functional alterations of the gut microbiome, in interaction with the immune system, were associated with ocular diseases.98–101 Moreover, it was shown that a healthy gut microbiome strengthens the ocular mucosal immune barrier through increasing immune effectors such as IgA and complement in the tear film of mice. Evidence suggests that the OSM is in a symbiotic relationship with the immune system and plays a role in the education, function, and induction of the immune system.2,3,102 A recent study demonstrated a causal relationship between the presence of Corynebacterium mastitidis at the OS and efficient defense against pathogens through activation of local immunity.2 Additional evidence was provided in mouse models demonstrating an increased susceptibility to keratitis when the ocular surface was depleted from commensal bacteria through lack of local recruitment of neutrophils usually induced by the resident bacteria.103 The OSM itself appears to be influenced by various host and environmental factors, whose role and importance are still elusive.65 A better understanding of the factors determining OSM composition and diversity could therefore substantially broaden the understanding of pathogenesis of OS diseases. One study has investigated the interplay between the healthy OSM and the tear proteome. This was the first investigation that found associations between taxonomical and functional features of the OSM and the tear proteome in humans.39 Analysis of the tear proteome with chromatography tandem mass spectrometry showed the 5 most abundant proteins to be lactotransferrin, albumin, lipocalin-1, lysozyme, and immunoglobulin A. Apart from albumin, these proteins all have antimicrobial activity. Functional classification based on Gene Ontology (GO) categories of the 2172 identified protein groups, revealed that 9% of the human tear proteins are involved in the biological process of antimicrobial humoral response. These results are consistent with previous knowledge that protection against pathogens is among the most important functions of the tear film.104 It has been hypothesized that antimicrobial components of the tear film may influence the OSM and vice versa. In line with this hypothesis, a disturbed tear film composition could favor dysbiosis of the OSM, lower protection against pathogens and ultimately lead to disease.39 Another study assessing the association between tear proteome and OSM in healthy eyes showed abundance of amino acid metabolism pathways (with the highest proportion being the tyrosine metabolism).49 Amino acids are naturally found in tears and have a positive effect on maintaining OS homeostasis, and it has been hypothesized that bacteria at the OS may play a role in the metabolism of tear film amino acids.105,106 Since Corynebacterium sub-species are known to produce amino acids, the Corynebacterium found on the OS may also be involved in amino acid metabolism.107 However, more research is needed to assess whether the healthy OSM contributes to the abundance of amino acids in tears and their potential beneficial effects. Kang et al detected microbial pathways involved in inorganic ion transport and metabolism as well as lipid metabolism and suggest further exploration whether the OSM affects tear film stability through these pathways.49
Discussion and Conclusions
The Human Microbiome Project108 aimed to characterize the microbiomes of the skin, gastrointestinal tract, oral cavity, nasal passages, and the urogenital tract to understand its role in health and disease. While there is evidence that microbes are involved in various host processes, a dysbiosis in the microbiota may be associated with several diseases including eye disease. Although the OS is continuously exposed to the environment including potentially pathogenic microbes, the OSM has not been characterized in the Human Microbiome Project. It has been much debated whether environmental microbes can adhere to and colonize the OS since host factors (mechanical barriers such as blinking and tear reflex as well as chemical defense such as anti-microbial tear proteins) create a harsh environment for microbes.109 Early traditional culture techniques showed the presence of bacteria at the conjunctiva of healthy subjects.12 However, these techniques are limited and biased since only cultivable species grow under the provided conditions and represent only a small proportion of the total microbial population in a sample. A more thorough characterization of the OSM has been provided by modern sequencing technologies. Using whole metagenome shotgun sequencing, it has been shown that in addition to bacteria, viruses (including bacteriophages) and eukaryotes (mainly fungi) colonize the human OS. While these techniques have been effective in identifying microbes in large biomass samples such as the gut, data inconsistencies (amplification bias, misidentification of microbial species) pose a problem in low microbial niches such as the OS. For this reason, there is a lack of reproducible data on taxonomic composition including diversity, abundance, and homeostasis of the OSM, thus the definition of a core microbiota is still missing. Nevertheless, it is important to mention that many different definitions of “core microbiota” have been used in microbiome studies so far and no consensus has been reached. After a detailed analysis of these definitions, the following description was proposed:
The core microbiota is a suite of members shared among microbial consortia from similar habitats, which is important for understanding stability, plasticity, and functioning across complex microbial assemblages.110
This may be of interest for further studies focused on determining the core and transient microbiome of the ocular surface. Another consideration with potential public health relevance regards the influence of environmental factors in OSM composition. Indeed, it is known that factors such as hygiene behavior, contact with young children, or seasonal and climatic conditions affect conjunctivitis incidence.111 In turn, the manner and extent to which external factors shape OSM structure is largely unknown. While few studies attempting to address this question have obtained interesting results, we are still humbled by the complexity of this matter.48,65
In conclusion, OSM research is still at an early stage and needs further investigation. It is of upmost importance to define a core microbiota in this niche with low microbial abundance. Indeed, this will provide the basis for understanding how the OSM shapes host physiology in health and disease, and ultimately developing microbial-based therapeutic approaches for the prevention and treatment of ocular diseases.
Abbreviations
OSM, ocular surface microbiome; OS, ocular surface, CALT, conjunctiva-associated lymphoid tissue; WA, weighted average; WM, weighted median; HPV, Human papilloma virus; MCV, Merkel cell polyomavirus; BRiSK, Biome representational in silico karyotyping; TTV, Torque teno virus; ITS, internal transcribed spacer; MA, mean abundance; GO, Gene Ontology.
Disclosure
VGP reports a grant from Peter Mayor Gedächtnis-Stiftung. MSZ reports grants from Foundation Bertarelli Catalyst Fund, EPFL (Ecole Polytechnique Fédérale de Lausanne) and Lausanne, Switzerland (CF10000044 – EPFL SCR0237812), during the conduct of the study. He also reports grants, personal fees from Bayer, personal fees from Novartis, non-financial support from Heidelberg Engineering, outside the submitted work. Dr Denise C Zysset-Burri reports grants from OPOS foundation, St. Gallen, Switzerland and Foundation Bertarelli Catalyst Fund, EPFL (Ecole Polytechnique Fédérale de Lausanne), Lausanne, Switzerland (CF10000044 – EPFL SCR0237812), during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Delbeke H, Younas S, Casteels I, Joossens M. Current knowledge on the human eye microbiome: a systematic review of available amplicon and metagenomic sequencing data. Acta Ophthalmol. 2021;99(1):16–25. doi:10.1111/aos.14508
2. St Leger AJ, Desai JV, Drummond RA, et al. An ocular commensal protects against corneal infection by driving an interleukin-17 response from mucosal gammadelta T cells. Immunity. 2017;47(1):148–158 e5. doi:10.1016/j.immuni.2017.06.014
3. Kugadas A, Gadjeva M. Impact of microbiome on ocular health. Ocul Surf. 2016;14(3):342–349. doi:10.1016/j.jtos.2016.04.004
4. Doan T, Akileswaran L, Andersen D, et al. Paucibacterial microbiome and resident DNA virome of the healthy conjunctiva. Invest Ophthalmol Vis Sci. 2016;57(13):5116–5126. doi:10.1167/iovs.16-19803
5. Miller D, Iovieno A. The role of microbial flora on the ocular surface. Curr Opin Allergy Clin Immunol. 2009;9(5):466–470. doi:10.1097/ACI.0b013e3283303e1b
6. Aragona P, Baudouin C, Benitez Del Castillo JM, et al. The ocular microbiome and microbiota and their effects on ocular surface pathophysiology and disorders. Surv Ophthalmol. 2021;66(6):907–925. doi:10.1016/j.survophthal.2021.03.010
7. Satokari R, Fuentes S, Mattila E, Jalanka J, de Vos WM, Arkkila P. Fecal transplantation treatment of antibiotic-induced, noninfectious colitis and long-term microbiota follow-up. Case Rep Med. 2014;2014:913867. doi:10.1155/2014/913867
8. Morgan XC, Segata N, Huttenhower C. Biodiversity and functional genomics in the human microbiome. Trends Genet. 2013;29(1):51–58. doi:10.1016/j.tig.2012.09.005
9. Joyce SA, Gahan CG. The gut microbiota and the metabolic health of the host. Curr Opin Gastroenterol. 2014;30(2):120–127. doi:10.1097/MOG.0000000000000039
10. Keilty RA. The bacterial flora of the normal conjunctiva with comparative nasal culture study. Am J Ophthalmol. 1930;13(10):876–879. doi:10.1016/S0002-9394(30)92437-3
11. Nolan J. Evaluation of conjunctival and nasal bacterial cultures before intra-ocular operations. Br J Ophthalmol. 1967;51(7):483–485. doi:10.1136/bjo.51.7.483
12. Perkins RE, Kundsin RB, Pratt MV, Abrahamsen I, Leibowitz HM. Bacteriology of normal and infected conjunctiva. J Clin Microbiol. 1975;1(2):147–149. doi:10.1128/jcm.1.2.147-149.1975
13. McNatt J, Allen SD, Wilson LA, Dowell VR. Anaerobic flora of the normal human conjunctival sac. Arch Ophthalmol. 1978;96(8):1448–1450. doi:10.1001/archopht.1978.03910060196020
14. Shovlin JP, Argüeso P, Carnt N, et al. 3. Ocular surface health with contact lens wear. Contact Lens and Anterior Eye. 2013;36:S14–S21. doi:10.1016/S1367-0484(13)60005-3
15. Knop N, Knop E. Conjunctiva-associated lymphoid tissue in the human eye. Invest Ophthalmol Vis Sci. 2000;41(6):1270–1279.
16. Siebelmann S, Gehlsen U, Huttmann G, et al. Development, alteration and real time dynamics of conjunctiva-associated lymphoid tissue. PLoS One. 2013;8(12):e82355. doi:10.1371/journal.pone.0082355
17. Pamer EG. Immune responses to commensal and environmental microbes. Nat Immunol. 2007;8(11):1173–1178. doi:10.1038/ni1526
18. Cogen AL, Nizet V, Gallo RL. Skin microbiota: a source of disease or defence? Br J Dermatol. Mar. 2008;158(3):442–455. doi:10.1111/j.1365-2133.2008.08437.x
19. Ozkan J, Willcox M, Wemheuer B, Wilcsek G, Coroneo M, Thomas T. Biogeography of the human ocular microbiota. Ocul Surf. 2019;17(1):111–118. doi:10.1016/j.jtos.2018.11.005
20. St Leger AJ, Caspi RR. Visions of Eye Commensals: the Known and the Unknown About How the Microbiome Affects Eye Disease. BioEssays. 2018;40(11):e1800046. doi:10.1002/bies.201800046
21. Lagier JC, Hugon P, Khelaifia S, Fournier PE, La Scola B, Raoult D. The rebirth of culture in microbiology through the example of culturomics to study human gut microbiota. Clin Microbiol Rev. 2015;28(1):237–264. doi:10.1128/CMR.00014-14
22. Bonnet M, Lagier JC, Raoult D, Khelaifia S. Bacterial culture through selective and non-selective conditions: the evolution of culture media in clinical microbiology. New Microbes New Infect. 2020;34:100622. doi:10.1016/j.nmni.2019.100622
23. Benn A, Heng N, Broadbent JM, Thomson WM. Studying the human oral microbiome: challenges and the evolution of solutions. Aust Dent J. 2018;63(1):14–24. doi:10.1111/adj.12565
24. Deo PN, Deshmukh R. Oral microbiome: unveiling the fundamentals. J Oral Maxillofac Pathol. 2019;23(1):122–128. doi:10.4103/jomfp.JOMFP_304_18
25. Head I, Saunders J, Pickup RW. Microbial evolution, diversity, and ecology: a decade of ribosomal RNA analysis of uncultivated microorganisms. Microb Ecol. 1998;35(1):1–21. doi:10.1007/s002489900056
26. Hahn MW, Koll U, Schmidt J. Isolation and cultivation of bacteria. In: The Structure and Function of Aquatic Microbial Communities. Springer; 2019:313–351.
27. Pham VH, Kim J. Cultivation of unculturable soil bacteria. Trends Biotechnol. 2012;30(9):475–484. doi:10.1016/j.tibtech.2012.05.007
28. Acinas SG, Sarma-Rupavtarm R, Klepac-Ceraj V, Polz MF. PCR-induced sequence artifacts and bias: insights from comparison of two 16S rRNA clone libraries constructed from the same sample. Appl Environ Microbiol. 2005;71(12):8966–8969. doi:10.1128/AEM.71.12.8966-8969.2005
29. Brooks JP, Edwards DJ, Harwich MD, et al. The truth about metagenomics: quantifying and counteracting bias in 16S rRNA studies. BMC Microbiol. 2015;15:66. doi:10.1186/s12866-015-0351-6
30. Johnson JS, Spakowicz DJ, Hong BY, et al. Evaluation of 16S rRNA gene sequencing for species and strain-level microbiome analysis. Nat Commun. 2019;10(1):5029. doi:10.1038/s41467-019-13036-1
31. Kennedy K, Hall MW, Lynch MD, Moreno-Hagelsieb G, Neufeld JD, Wommack KE. Evaluating bias of illumina-based bacterial 16S rRNA gene profiles. Appl Environ Microbiol. 2014;80(18):5717–5722. doi:10.1128/AEM.01451-14
32. Hornung BVH, Zwittink RD, Kuijper EJ. Issues and current standards of controls in microbiome research. FEMS Microbiol Ecol. 2019;95(5). doi:10.1093/femsec/fiz045
33. Costea PI, Zeller G, Sunagawa S, et al. Towards standards for human fecal sample processing in metagenomic studies. Nat Biotechnol. 2017;35(11):1069–1076. doi:10.1038/nbt.3960
34. Quince C, Walker AW, Simpson JT, Loman NJ, Segata N. Shotgun metagenomics, from sampling to analysis. Nat Biotechnol. 2017;35(9):833–844. doi:10.1038/nbt.3935
35. Riesenfeld CS, Schloss PD, Handelsman J. Metagenomics: genomic analysis of microbial communities. Annu Rev Genet. 2004;38:525–552. doi:10.1146/annurev.genet.38.072902.091216
36. Salter SJ, Cox MJ, Turek EM, et al. Reagent and laboratory contamination can critically impact sequence-based microbiome analyses. BMC Biol. 2014;12(1):1–12. doi:10.1186/s12915-014-0087-z
37. Galazzo G, van Best N, Benedikter BJ, et al. How to count our microbes? The effect of different quantitative microbiome profiling approaches. Front Cell Infect Microbiol. 2020;10:403. doi:10.3389/fcimb.2020.00403
38. Tettamanti Boshier FA, Srinivasan S, Lopez A, et al. Complementing 16S rRNA gene amplicon sequencing with total bacterial load to infer absolute species concentrations in the vaginal microbiome. mSystems. 2020;5(2). doi:10.1128/mSystems.00777-19
39. Zysset-Burri DC, Schlegel I, Lincke JB, et al. Understanding the interactions between the ocular surface microbiome and the tear proteome. Invest Ophthalmol Vis Sci. 2021;62(10):8. doi:10.1167/iovs.62.10.8
40. Lee AY, Akileswaran L, Tibbetts MD, Garg SJ, Van Gelder RN. Identification of torque teno virus in culture-negative endophthalmitis by representational deep DNA sequencing. Ophthalmology. 2015;122(3):524–530. doi:10.1016/j.ophtha.2014.09.001
41. Marotz CA, Sanders JG, Zuniga C, Zaramela LS, Knight R, Zengler K. Improving saliva shotgun metagenomics by chemical host DNA depletion. Microbiome. 2018;6(1):42. doi:10.1186/s40168-018-0426-3
42. Marquet M, Zollkau J, Pastuschek J, et al. Evaluation of microbiome enrichment and host DNA depletion in human vaginal samples using Oxford Nanopore’s adaptive sequencing. Sci Rep. 2022;12(1):4000. doi:10.1038/s41598-022-08003-8
43. Heravi FS, Zakrzewski M, Vickery K, Hu H. Host DNA depletion efficiency of microbiome DNA enrichment methods in infected tissue samples. J Microbiol Methods. 2020;170:105856. doi:10.1016/j.mimet.2020.105856
44. Shade A, Handelsman J. Beyond the Venn diagram: the hunt for a core microbiome. Environ Microbiol. 2012;14(1):4–12. doi:10.1111/j.1462-2920.2011.02585.x
45. Ta CN, Chang RT, Singh K, et al. Antibiotic resistance patterns of ocular bacterial flora. Ophthalmology. 2003;110(10):1946–1951. doi:10.1016/S0161-6420(03)00735-8
46. Graham JE, Moore JE, Jiru X, et al. Ocular pathogen or commensal: a PCR-based study of surface bacterial flora in normal and dry eyes. Invest Ophthalmol Vis Sci. 2007;48(12):5616–5623. doi:10.1167/iovs.07-0588
47. Willcox MD. Characterization of the normal microbiota of the ocular surface. Exp Eye Res. 2013;117:99–105. doi:10.1016/j.exer.2013.06.003
48. Deng Y, Wen X, Hu X, et al. Geographic difference shaped human ocular surface metagenome of young han Chinese from Beijing, Wenzhou, and Guangzhou cities. Invest Ophthalmol Vis Sci. 2020;61(2):47. doi:10.1167/iovs.61.2.47
49. Kang Y, Lin S, Ma X, et al. Strain heterogeneity, cooccurrence network, taxonomic composition and functional profile of the healthy ocular surface microbiome. Eye Vis. 2021;8(1):6. doi:10.1186/s40662-021-00228-4
50. Wen X, Miao L, Deng Y, et al. The Influence of age and sex on ocular surface microbiota in healthy adults. Invest Ophthalmol Vis Sci. 2017;58(14):6030–6037. doi:10.1167/iovs.17-22957
51. Fu Y, Wu J, Wang D, et al. Metagenomic profiling of ocular surface microbiome changes in Demodex blepharitis patients. Front Cell Infect Microbiol. 2022;12:922753. doi:10.3389/fcimb.2022.922753
52. Byrd AL, Belkaid Y, Segre JA. The human skin microbiome. Nat Rev Microbiol. 2018;16(3):143–155. doi:10.1038/nrmicro.2017.157
53. Andersson J, Vogt JK, Dalgaard MD, Pedersen O, Holmgaard K, Heegaard S. Ocular surface microbiota in patients with aqueous tear-deficient dry eye. Ocul Surf. 2021;19:210–217. doi:10.1016/j.jtos.2020.09.003
54. Butcher RMR, Sokana O, Jack K, et al. Active trachoma cases in the Solomon Islands have varied polymicrobial community structures but do not associate with individual non-chlamydial pathogens of the eye. Front Med. 2017;4:251. doi:10.3389/fmed.2017.00251
55. Dong X, Wang Y, Wang W, Lin P, Huang Y. Composition and diversity of bacterial community on the ocular surface of patients with meibomian gland dysfunction. Invest Ophthalmol Vis Sci. 2019;60(14):4774–4783. doi:10.1167/iovs.19-27719
56. Ham B, Hwang HB, Jung SH, Chang S, Kang KD, Kwon MJ. Distribution and diversity of ocular microbial communities in diabetic patients compared with healthy subjects. Curr Eye Res. 2018;43(3):314–324. doi:10.1080/02713683.2017.1406528
57. Huang Y, Yang B, Li W. Defining the normal core microbiome of conjunctival microbial communities. Clin Microbiol Infect. 2016;22(7):643e7–643 e12. doi:10.1016/j.cmi.2016.04.008
58. Li S, Yi G, Peng H, et al. How ocular surface microbiota debuts in type 2 diabetes mellitus. Front Cell Infect Microbiol. 2019;9:202. doi:10.3389/fcimb.2019.00202
59. Li Z, Gong Y, Chen S, et al. Comparative portrayal of ocular surface microbe with and without dry eye. J Microbiol. 2019;57(11):1025–1032. doi:10.1007/s12275-019-9127-2
60. Liang X, Li Y, Xiong K, et al. Demodex infection changes ocular surface microbial communities, in which meibomian gland dysfunction may play a role. Ophthalmol Ther. 2021;10(3):601–617. doi:10.1007/s40123-021-00356-z
61. Ozkan J, Nielsen S, Diez-Vives C, Coroneo M, Thomas T, Willcox M. Temporal stability and composition of the ocular surface microbiome. Sci Rep. 2017;7(1):9880. doi:10.1038/s41598-017-10494-9
62. Yau JW, Hou J, Tsui SKW, et al. Characterization of ocular and nasopharyngeal microbiome in allergic rhinoconjunctivitis. Pediatr Allergy Immunol. 2019;30(6):624–631. doi:10.1111/pai.13088
63. Zhang H, Zhao F, Hutchinson DS, et al. Conjunctival microbiome changes associated with soft contact lens and orthokeratology lens wearing. Invest Ophthalmol Vis Sci. 2017;58(1):128–136. doi:10.1167/iovs.16-20231
64. Zhang Z, Zou X, Xue W, Zhang P, Wang S, Zou H. Ocular surface microbiota in diabetic patients with dry eye disease. Invest Ophthalmol Vis Sci. 2021;62(12):13. doi:10.1167/iovs.62.12.13
65. Zhou Y, Holland MJ, Makalo P, et al. The conjunctival microbiome in health and trachomatous disease: a case control study. Genome Med. 2014;6(11):1–10. doi:10.1186/s13073-014-0099-x
66. Grzybowski A, Brona P, Kim SJ. Microbial flora and resistance in ophthalmology: a review. Graefes Arch Clin Exp Ophthalmol. 2017;255(5):851–862. doi:10.1007/s00417-017-3608-y
67. Smith C. Bacteriology of the healthy conjunctiva. Br J Ophthalmol. 1954;38(12):719. doi:10.1136/bjo.38.12.719
68. Suto C, Morinaga M, Yagi T, Tsuji C, Toshida H. Conjunctival sac bacterial flora isolated prior to cataract surgery. Infect Drug Resist. 2012;5:37–41. doi:10.2147/IDR.S27937
69. Capriotti JA, Pelletier JS, Shah M, Caivano DM, Ritterband DC. Normal ocular flora in healthy eyes from a rural population in Sierra Leone. Int Ophthalmol. 2009;29(2):81–84. doi:10.1007/s10792-008-9196-4
70. Honda R, Toshida H, Suto C, et al. Effect of long-term treatment with eyedrops for glaucoma on conjunctival bacterial flora. Infect Drug Resist. 2011;4:191–196. doi:10.2147/IDR.S24250
71. Cavuoto KM, Banerjee S, Miller D, Galor A. Composition and comparison of the ocular surface microbiome in infants and older children. Transl Vis Sci Technol. 2018;7(6):16. doi:10.1167/tvst.7.6.16
72. Gregorczyk M, Roskal-Wałek J. Objawy oczne w zakażeniu SARS-CoV-2 [Ocular symptoms in SARS-CoV-2 infection]. Pol Merkur Lekarski. 2022;50(296):86–93. Polish.
73. Zauli G, AlHilali S, Al-Swailem S, Secchiero P, Voltan R. Therapeutic potential of the MDM2 inhibitor Nutlin-3 in counteracting SARS-CoV-2 infection of the eye through p53 activation. Front Med. 2022;9:902713. doi:10.3389/fmed.2022.902713
74. Davis G, Li K, Thankam FG, Wilson DR, Agrawal DK. Ocular transmissibility of COVID-19: possibilities and perspectives. Mol Cell Biochem. 2022;477(3):849–864. doi:10.1007/s11010-021-04336-6
75. Verma V, Shen D, Sieving PC, Chan -C-C. The role of infectious agents in the etiology of ocular adnexal neoplasia. Surv Ophthalmol. 2008;53(4):312–331. doi:10.1016/j.survophthal.2008.04.008
76. Spurgeon ME, Lambert PF. Merkel cell polyomavirus: a newly discovered human virus with oncogenic potential. Virology. 2013;435(1):118–130. doi:10.1016/j.virol.2012.09.029
77. Kumar V, Baweja M, Singh PK, Shukla P. Recent developments in systems biology and metabolic engineering of plant–microbe interactions. Review. Front Plant Sci. 2016;7. doi:10.3389/fpls.2016.01421
78. Zárate S, Taboada B, Yocupicio-Monroy M, Arias CF. Human Virome. Arch Med Res. 2017;48(8):701–716. doi:10.1016/j.arcmed.2018.01.005
79. Shkoporov AN, Turkington CJ, Hill C. Mutualistic interplay between bacteriophages and bacteria in the human gut. Nat Rev Microbiol. 2022;20(12):737–749. doi:10.1038/s41579-022-00755-4
80. Kortright KE, Chan BK, Koff JL, Turner PE. Phage therapy: a renewed approach to combat antibiotic-resistant bacteria. Cell Host Microbe. 2019;25(2):219–232. doi:10.1016/j.chom.2019.01.014
81. Taylor VL, Fitzpatrick AD, Islam Z, Maxwell KL. The diverse impacts of phage morons on bacterial fitness and virulence. Adv Virus Res. 2019;103:1–31. doi:10.1016/bs.aivir.2018.08.001
82. Cumby N, Edwards AM, Davidson AR, Maxwell KL. The bacteriophage HK97 gp15 moron element encodes a novel superinfection exclusion protein. J Bacteriol. 2012;194(18):5012–5019. doi:10.1128/JB.00843-12
83. Smits SL, Manandhar A, van Loenen FB, et al. High prevalence of anelloviruses in vitreous fluid of children with seasonal hyperacute panuveitis. J Infect Dis. 2012;205(12):1877–1884. doi:10.1093/infdis/jis284
84. Chen T, Väisänen E, Mattila PS, Hedman K, Söderlund-Venermo M. Antigenic diversity and seroprevalences of Torque teno viruses in children and adults by ORF2-based immunoassays. J Gen Virol. 2013;94(Pt 2):409–417. doi:10.1099/vir.0.046862-0
85. Dewannieux M, Heidmann T. Endogenous retroviruses: acquisition, amplification and taming of genome invaders. Curr Opin Virol. 2013;3(6):646–656. doi:10.1016/j.coviro.2013.08.005
86. Siegal N, Gutowski M, Akileswaran L, et al. Elevated levels of Merkel cell polyoma virus in the anophthalmic conjunctiva. Sci Rep. 2021;11(1):15366. doi:10.1038/s41598-021-92642-w
87. Słowik M, Biernat MM, Urbaniak-Kujda D, Kapelko-Słowik K, Misiuk-Hojło M. Mycotic Infections of the Eye. Adv Clin Exp Med. 2015;24(6):1113–1117. doi:10.17219/acem/50572
88. Ge C, Wei C, Yang BX, Cheng J, Huang YS. Conjunctival microbiome changes associated with fungal keratitis: metagenomic analysis. Int J Ophthalmol. 2019;12(2):194–200. doi:10.18240/ijo.2019.02.02
89. Niederkorn JY. The biology of Acanthamoeba keratitis. Exp Eye Res. 2021;202:108365. doi:10.1016/j.exer.2020.108365
90. Hanson B, Zhou Y, Bautista EJ, et al. Characterization of the bacterial and fungal microbiome in indoor dust and outdoor air samples: a pilot study. Environ Sci Process Impacts. 2016;18(6):713–724. doi:10.1039/c5em00639b
91. Shivaji S, Jayasudha R, Sai Prashanthi G, Kalyana Chakravarthy S, Sharma S. The human ocular surface fungal microbiome. Invest Ophthalmol Vis Sci. 2019;60(1):451–459. doi:10.1167/iovs.18-26076
92. Wang Y, Chen H, Xia T, Huang Y. Characterization of fungal microbiota on normal ocular surface of humans. Clin Microbiol Infect. 2020;26(1):123.e9–123.e13. doi:10.1016/j.cmi.2019.05.011
93. Mitchell JI, Zuccaro A. Sequences, the environment and fungi. Mycologist. 2006;20(2):62–74. doi:10.1016/j.mycol.2005.11.004
94. Nowrousian M. Next-generation sequencing techniques for eukaryotic microorganisms: sequencing-based solutions to biological problems. Eukaryot Cell. 2010;9(9):1300–1310. doi:10.1128/ec.00123-10
95. Schoch CL, Seifert KA, Huhndorf S, et al. Nuclear ribosomal internal transcribed spacer (ITS) region as a universal DNA barcode marker for Fungi. Proce Natl Acad Sci. 2012;109(16):6241–6246. doi:10.1073/pnas.1117018109
96. Theelen B, Cafarchia C, Gaitanis G, Bassukas ID, Boekhout T, Dawson TL. Malassezia ecology, pathophysiology, and treatment. Med Mycol. 2018;56(suppl_1):S10–s25. doi:10.1093/mmy/myx134
97. Shi N, Li N, Duan X, Niu H. Interaction between the gut microbiome and mucosal immune system. Mil Med Res. 2017;4:14. doi:10.1186/s40779-017-0122-9
98. Zysset-Burri DC, Morandi S, Herzog EL, Berger LE, Zinkernagel MS. The role of the gut microbiome in eye diseases. Prog Retin Eye Res. 2022;101117. doi:10.1016/j.preteyeres.2022.101117
99. Zysset-Burri DC, Keller I, Berger LE, et al. Associations of the intestinal microbiome with the complement system in age-related macular degeneration. NPJ Genom Med. 2019;5(1):1.
100. Zinkernagel MS, Zysset-Burri DC, Keller I, et al. Association of the intestinal microbiome with the development of neovascular age-related macular degeneration. Sci Rep. 2017;7:40826. doi:10.1038/srep40826
101. Zysset-Burri DC, Keller I, Berger LE, et al. Associations of the intestinal microbiome with the complement system in neovascular age-related macular degeneration. NPJ Genom Med. 2020;5(1):1–11. doi:10.1038/s41525-020-00141-0
102. Horai R, Zárate-Bladés CR, Dillenburg-Pilla P, et al. Microbiota-dependent activation of an autoreactive T cell receptor provokes autoimmunity in an immunologically privileged site. Immunity. 2015;43(2):343–353. doi:10.1016/j.immuni.2015.07.014
103. Kugadas A, Christiansen SH, Sankaranarayanan S, et al. Impact of microbiota on resistance to ocular pseudomonas aeruginosa-induced keratitis. PLoS Pathog. 2016;12(9):e1005855. doi:10.1371/journal.ppat.1005855
104. Zhou L, Huang LQ, Beuerman RW, et al. Proteomic analysis of human tears: defensin expression after ocular surface surgery. J Proteome Res. 2004;3(3):410–416. doi:10.1021/pr034065n
105. Nakatsukasa M, Sotozono C, Shimbo K, et al. Amino Acid profiles in human tear fluids analyzed by high-performance liquid chromatography and electrospray ionization tandem mass spectrometry. Am J Ophthalmol. 2011;151(5):799–808 e1. doi:10.1016/j.ajo.2010.11.003
106. Rusciano D, Roszkowska AM, Gagliano C, Pezzino S. Free amino acids: an innovative treatment for ocular surface disease. Eur J Pharmacol. 2016;787:9–19. doi:10.1016/j.ejphar.2016.04.029
107. Liu G, Wu J, Yang H, Bao Q. Codon usage patterns in Corynebacterium glutamicum: mutational bias, natural selection and amino acid conservation. Comp Funct Genomics. 2010;2010:343569. doi:10.1155/2010/343569
108. Turnbaugh PJ, Ley RE, Hamady M, Fraser-Liggett CM, Knight R, Gordon JI. The human microbiome project. Nature. 2007;449(7164):804–810. doi:10.1038/nature06244
109. Kugadas A, Wright Q, Geddes-McAlister J, Gadjeva M. Role of microbiota in strengthening ocular mucosal barrier function through secretory IgA. Invest Ophthalmol Vis Sci. 2017;58(11):4593–4600. doi:10.1167/iovs.17-22119
110. Berg G, Rybakova D, Fischer D, et al. Microbiome definition re-visited: old concepts and new challenges. Microbiome. 2020;8(1):103. doi:10.1186/s40168-020-00875-0
111. Ramirez DA, Porco TC, Lietman TM, Keenan JD. Epidemiology of conjunctivitis in US emergency departments. JAMA Ophthalmol. 2017;135(10):1119–1121. doi:10.1001/jamaophthalmol.2017.3319
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
