Back to Journals » Clinical Ophthalmology » Volume 10
Interactive navigation-guided ophthalmic plastic surgery: navigation enabling of telescopes and their use in endoscopic lacrimal surgeries
Authors Ali MJ , Singh S, Naik MN , Kaliki S , Dave TV
Received 5 August 2016
Accepted for publication 29 August 2016
Published 21 November 2016 Volume 2016:10 Pages 2319—2324
DOI https://doi.org/10.2147/OPTH.S119055
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mohammad Javed Ali,1 Swati Singh,1 Milind N Naik,1 Swathi Kaliki,2 Tarjani Vivek Dave1
1The Institute of Dacryology, 2The Operation Eyesight Universal Institute for Eye Cancer, L.V. Prasad Eye Institute, Hyderabad, India
Purpose: The aims of this study were to report the preliminary experience of using telescopes, which were enabled for navigation guidance, and their utility in complex endoscopic lacrimal surgeries.
Methods: Navigation enabling of the telescope was achieved by using the AxiEM™ malleable neuronavigation shunt stylet. Image-guided dacryolocalization was performed in five patients using the intraoperative image-guided StealthStation™ system in the electromagnetic mode. The “look ahead” protocol software was used to assist the surgeon in assessing the intraoperative geometric location of the endoscope and what lies ahead in real time. All patients underwent navigation-guided powered endoscopic dacryocystorhinostomy. The utility of uninterrupted navigation guidance throughout the surgery with the endoscope as the navigating tool was noted.
Results: Intraoperative geometric localization of the lacrimal sac and the nasolacrimal duct could be easily deciphered. Constant orientation of the lacrimal drainage system and the peri-lacrimal anatomy was possible without the need for repeated point localizations throughout the surgery. The “look ahead” features could accurately alert the surgeon of anatomical structures that exists at 5, 10 and 15 mm in front of the endoscope. Good securing of the shunt stylet with the telescope was found to be essential for constant and accurate navigation.
Conclusion: Navigation-enabled endoscopes provide the surgeon with the advantage of sustained stereotactic anatomical awareness at all times during the surgery.
Keywords: telescope, endoscope, image guidance, navigation, lacrimal surgery, powered endoscopic DCR
Introduction
The use of telescopes has revolutionized endoscopic surgeries, and lacrimal procedures are not an exception.1,2 With constant advances in instrumentation and techniques, the results of primary and revision endoscopic dacryocystorhinostomy (DCR) are now comparable to those of external approaches.3,4 The use of navigation guidance is quickly gaining foothold in complex endoscopic lacrimal surgeries.5–7 The advantages of navigation guidance include accurate target localization, reduced risk of complications and enhanced safety. However, routine navigation localization would require placing the navigation seeker or instrument at multiple anatomical points and at multiple times during a given surgery. It would be desirable to have the tip of the endoscope navigable, which would offer several advantages. This can be achieved using either the optical technique or the electromagnetic technique. The optical technique has been reported in one case of orbital foreign body to navigate the tip of the endoscope.8 In this series, we report the use of the neuronavigation stylet and the telescope as one instrument for constant endoscopic navigation using the electromagnetic technique, thereby eliminating the need for separate trackers as well as the optical technology. The authors of the present study report their preliminary experiences with navigation-enabled telescope and its utility in guidance for complex powered endoscopic DCRs.
Methodology
Institutional review board approval was obtained from L.V. Prasad Eye Institute. All patients provided written informed consent. Navigation enabling of the telescope was achieved by using AxiEM™ malleable neuronavigation shunt stylet (Medtronic, Minneapolis, MN, USA). Image-guided dacryolocalization was performed using the intraoperative image-guided StealthStation™system in the electromagnetic mode using the noninvasive dynamic reference frame with the AxiEM technology. The “look ahead” protocol software was used to assist the surgeon in assessing the intraoperative geometric location of the endoscope and what lies ahead in real time. Five consecutive patients with complex secondary acquired nasolacrimal drainage obstruction were included in this study. All the patients underwent navigation-guided powered endoscopic DCR by a single surgeon (MJA). The utility of uninterrupted navigation guidance throughout the surgery with the endoscope as the simultaneous viewing and navigating tool was noted.
Technique
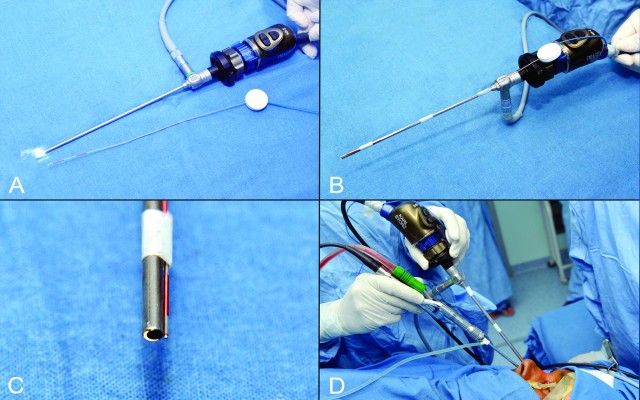
The AxiEM malleable neuronavigation shunt stylet is a flexible tracker with a length of 23 mm and diameter of 1.2 mm (Figure 1A). It has unique miniaturized electromagnetic coils near its tip that allow for accurate and real-time tracking. The routinely used 4 mm, 0° telescopes (Hopkins®; Karl Storz, Tuttlingen, Germany) were employed for navigation enabling (Figure 1A). The stylet was anchored securely to the surface of the telescope with the help of multiple adhesive dressings (Figure 1B). The tip of the stylet was in line with the edge of the telescope mirror (Figure 1C). Alternatively, if single point localization was desired, the tip was advanced a little beyond the edge of the telescope. However, this has potential for causing inadvertent tissue damage if left in that position. The authors routinely kept the tip on the same plane as that of the telescopic mirror and occasionally advanced it only when single point localization was desired. The instrument was then technically ready for an endoscopic lacrimal surgery (Figure 1D).
For intraoperative navigation, contiguous computerized tomography scans of 1 mm thickness were performed from the superior aspect of the horizontal portion of the mandible to the vertex as per the manufacturer’s guidelines. Various scans were then uploaded to the StealthStation’s workstation. The patient locations were then registered and software with the “look ahead” features was utilized. This unique software has the ability to show the anatomical structures that would be encountered at defined points in the trajectory of the endoscope. A typical “look ahead” screen has four windows showing axial cuts of computerized tomography scans (Figure 2). The first window shows the current location of the tip of the stylet or, in this study, the tip of the telescope. The subsequent three windows show anatomical structures at 5, 10 and 15 mm, respectively, from the current location trajectory. Hence, the surgeon would have a very good idea of what lies ahead of his/her endoscope at those defined points.
Results
The use of navigation-enabled telescope provided continuous navigation guidance during all phases of the powered endoscopic DCRs. The endoscope was able to track the anatomical structures in real time in its direction of trajectory. The location of the bony nasolacrimal duct becomes important in posttraumatic nasolacrimal drainage obstruction and this was found to be accurately achieved in all cases intraoperatively by placing the endoscope at different locations near the lateral wall of the nose and in different trajectories. In the case exemplified, the bony nasolacrimal duct can be localized and would be found 15 mm ahead in the same direction from the current location of the endoscope (Figure 3).
Scarring of the soft tissues can be a hurdle in accurate localization of the lacrimal sac in cases of revision DCRs or following lacrimal trauma. Precise identification of the scarred lacrimal sac from adjacent scarred tissues was possible when the endoscope was in the vicinity of scarred tissues (Figures 4 and 5). There were no line of sight interruptions. In one case, the position of the probe changed due to constant endoscopic maneuvering during the powered superior osteotomy and the radiological orientation was lost. The endoscope was retrieved back, the stylet was anchored back with adhesive dressings and navigation could be reinitiated without the need for a re-registration.
The “look ahead” features could accurately alert the surgeon of anatomical structures that existed at 5, 10 and 15 mm in front of the endoscope. No complications were noted and all the surgeries could be completed uneventfully. Good securing of the shunt stylet with the telescope was found to be essential for constant and accurate navigation.
Discussion
The current study presents our preliminary report on image-guided lacrimal surgeries using navigation-enabled telescopes. All the illustrated scenarios reflect the utility of this technique to provide constant intraoperative geometric orientation and the advantage of knowing what anatomical structures lie ahead at defined points, which would be encountered subsequently.
Neuronavigation endoscopic techniques are increasingly used in complex neurosurgeries in an attempt to be more minimally invasive, able to use pinless fixations in pediatric patients, enhance surgical safety and reduce morbidity.9–12 The uses of AxiEM neuroendoscopic navigation with shunt stylet have been reported in a few pediatric studies.12,13 All of them used neuroendoscopy with simultaneous working channels. The navigation stylet was inserted through one of the working channels beyond the tip of the endoscope and was used as the localizing instrument under endoscopic visualization. The current study used the routine ENT Hopkins telescopes (Karl Storz), which do not have working channels and hence the stylet was anchored separately on the surface of the telescopes, and found them to be effective in accurate localization.
Ali and Naik7 coined the term “image-guided dacryolocalization” to encompass the use of stereotactic navigation in lacrimal disorders. They reported enhanced safety and precision while performing endoscopic DCR in patients with traumatic secondary acquired nasolacrimal duct obstructions. To the best of the authors’ knowledge, only three reports have been published on the use of navigation guidance in lacrimal surgeries and the current study is a step further in advancing the techniques and the knowledge database.
The advantages of a navigation-enabled telescope include eliminating the need for multiple localizing instruments, uninterrupted radiological orientation and sustained navigation guidance throughout the surgery. Since this can be performed only with the help of “look ahead” protocol software, numerous advantages of this technology as elucidated earlier get added to the surgery.
There are a few limitations of using navigation-enabled telescopes as compared to the routine navigation. The front end of the telescope cannot touch the tissues, as this would entail the risk of mucosal burns and tissue trauma. However, this limitation is negated to a large extent with the use of “look ahead” techniques. Alternatively, one can extend the tip of the navigation stylet beyond the edge of the telescope for point localization when desired; however, this has potential to cause inadvertent tissue trauma while maneuvering the endoscope. There would also be an additional cost of acquiring the neuronavigation stylet; hence, at present it is indicated only in complex endoscopic lacrimal surgeries, especially posttraumatic nasolacrimal duct obstructions. It should also be kept in mind that AxiEM systems utilize electromagnetic navigation and hence may interfere with communications of an implantable device or patient monitoring systems.
In conclusion, neuronavigation shunt stylet can help in achieving navigation-enabled telescopes for uninterrupted stereotactic guidance. This technique can provide useful anatomical and radiological clues while performing endoscopic DCRs in cases with secondarily acquired and complex nasolacrimal duct obstructions. Further large series, involving more varied etiopathologies, would help in formulating appropriate guidelines for intraoperative image guidance.
Disclosure
Mohammad Javed Ali received royalties from Springer for his text book “Principles and Practice of Lacrimal Surgery”. Swathi Kaliki received support from The Operation Eyesight Universal Institute for Eye Cancer, Hyderabad, India. The funders had no role in the preparation, review or approval of the manuscript. The other authors report no conflicts of interest in this work.
References
McDonogh M, Meiring JH. Endoscopic transnasal dacryocystorhinostomy. J Laryngol Otol. 1989;103:585–587. | ||
Wormald PJ. Powered endoscopic dacryocystorhinostomy. Otolaryngol Clin North Am. 2006;39:539–549. | ||
Ali MJ, Psaltis AJ, Bassiouni A, Wormald PJ. Long-term outcomes in primary powered endoscopic dacryocystorhinostomy. Br J Ophthalmol. 2014;98:1678–1680. | ||
Ali MJ, Psaltis AJ, Wormald PJ. Long-term outcomes in revision powered endoscopic dacryocystorhinostomy. Int Forum Allergy Rhinol. 2014;4:1016–1019. | ||
Day S, Hwang TN, Pletcher SD, Bhatki A, McCulley TJ. Interactive image-guided dacryocystorhinostomy. Ophthal Plast Reconstr Surg. 2008;24:338–340. | ||
Morley AM, Collyer J, Malhotra R. Use of an image-guided navigation system for insertion of Lester-Jones tube in a patient with disturbed orbito-nasal anatomy. Orbit. 2009;28:439–441. | ||
Ali MJ, Naik MN. Image-guided dacryolocalization (IGDL) in traumatic secondary acquired lacrimal duct obstructions (SALDO). Ophthal Plast Reconstr Surg. 2015;31:406–409. | ||
Feichtinger M, Zemann W, Kärcher H. Removal of the pellet from the left orbital cavity by image-guided endoscopic navigation. Int J Oral Maxillofac Surg. 2007;36:358–361. | ||
Mangano F, Limbrick D, Leonard J, et al. Simultaneous image-guided and endoscopic navigation without rigid cranial fixation: applications in infant; technical case report. Neurosurgery. 2006;58(4 suppl 2):ONS-E377. | ||
Karabatsou K, Hayhurst C, Buxton N, et al. Endoscopic management of arachnoid cysts: an advancing technique. J Neurosurg. 2007;106:455–462. | ||
Sangra M, Clark S, Hayhurst C, Mallucci C. Electromagnetic-guided neuroendoscopy in paediatric population. J Neurosurg Pediatr. 2009;3:325–330. | ||
McMillen JL, Vonau M, Wood MJ. Pinless, frameless electromagnetic image-guided neuro-endoscopy in children. Childs Nerv System. 2010;26:871–878. | ||
Choi YK, Seo BR, Kim JH, Kim SH, Kim TS, Lee JK. The usefulness of electromagnetic neuronavigation in paediatric neuroendoscopic surgery. J Korean Neurosurg Soc. 2013;53:161–166. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.