Back to Journals » International Journal of Nanomedicine » Volume 17
Insights on the Dynamic Innovative Tumor Targeted-Nanoparticles-Based Drug Delivery Systems Activation Techniques
Authors Hamdy NM , Eskander G , Basalious EB
Received 21 August 2022
Accepted for publication 23 November 2022
Published 7 December 2022 Volume 2022:17 Pages 6131—6155
DOI https://doi.org/10.2147/IJN.S386037
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yan Shen
Nadia M Hamdy,1,* Georgette Eskander,2,* Emad B Basalious3,*
1Biochemistry Department, Faculty of Pharmacy, Ain Shams University, Cairo, 11566, Egypt; 2Faculty of Pharmacy, Ain Shams University, Postgraduate Student, Cairo, Egypt; 3Department of Pharmaceutics and Industrial Pharmacy, Faculty of Pharmacy, Cairo University, Cairo, 11562, Egypt
*These authors contributed equally to this work
Correspondence: Emad B Basalious; Nadia M Hamdy, Email [email protected]; [email protected]
Abstract: Anti-cancer conventional chemotherapeutic drugs novel formula progress, nowadays, uses nano technology for targeted drug delivery, specifically tailored to overcome therapeutic agents’ delivery challenges. Polymer drug delivery systems (DDS) play a crucial role in minimizing off-target side effects arising when using standard cytotoxic drugs. Using nano-formula for targeted localized action, permits using larger effective cytotoxic doses on a single special spot, that can seriously cause harm if it was administered systemically. Therefore, various nanoparticles (NPs) specifically have attached groups for targeting capabilities, not seen in bulk materials, which then need activation. In this review, we will present a simple innovative, illustrative, in a cartoon-way, enumeration of NP anti-cancer drug targeting delivery system activation-types. Area(s) covered in this review are the mechanisms of various NP activation techniques.
Keywords: intrinsic-activation, extrinsic-activation, NPs, nanoparticles, DDS, drug delivery systems, cancer biology, nano-bio-medicine
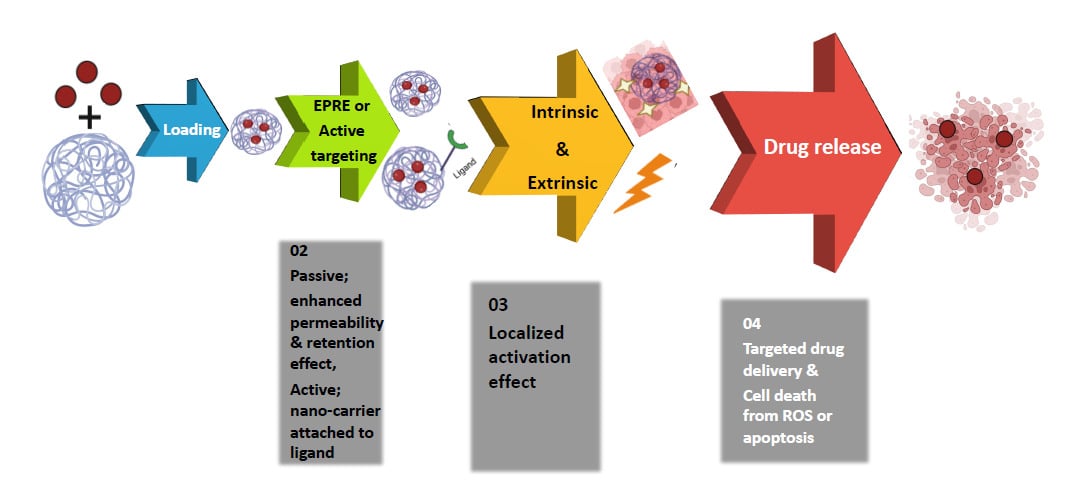
Graphical Abstract:
Introduction
Cancer is one of the major health problems that leads to death, worldwide.1 Many conventional therapeutic approaches have been conducted in order to treat different types of tumors, including surgery, radiation therapy, immunotherapy, chemotherapy, targeted therapy, and hormone therapy.2 Chemotherapy possesses an efficient cytotoxic effect,3 as reported 100 years ago by Paul Ehrlich the first scientist who discovered chemotherapy as the “magic bullet” for treating cancer patients.4 However, chemotherapy is often paired with terrible side effects ranging from skin disorders and suppression of bone marrow to fatigue.5 These side effects are all attributed to the lack of cytotoxic drugs targeting cancer cells.
Therefore, inventing or finding a drug delivery system (DDS) that has the ability to carry the chemotherapeutic drug directly to the target site with minimal leakage to normal cells is of great concern in the oncology field. This is achieved via nano-bio-medicine research to improve cancer treatment efficiency and decrease mortality rates as well.6
Nanocarriers (NCs) provide a golden solution for off-target side effects, through targeting mechanisms involving either passive targeting, where the nanoparticles (NPs) accumulate at the tumor site by the enhanced permeability and retention (EPR) effect that arises due to the leaky vasculature around the cancer cells from angiogenesis over-activation, with lack of lymphatic drainage that facilities anti-cancer drugs diffusion.7 Or, nanocarriers (NCs) may provide an active receptor-mediated tumor-targeted drug delivery vehicle,8 where the anti-cancer drug is surfing to the target receptor, carried over a NC, being functionalized by a ligand that might be an antibody, aptamer or peptide. As illustrated in Figure 1A, where a boy (drug) is carried over the floating board (NC) surfing the sea to reach the beach/island (tumor target destination) using a rope (ligand).
Many activation techniques are practically conducted to release most of the cytotoxic drug(s) carried on NC, to the tumor target site. These activation techniques are grouped into two categories, intrinsic-activation, that takes advantage of differences in some properties between healthy and cancerous cells, including pH, enzymatic, and concentration-dependent activation9 or extrinsic-activation where an external factor outside the tumor cell is encountered for activation, such as ultrasound, magnetic, light, and X-ray activation.10
Intrinsic-Activation
Being rich in some substances or different in certain features from healthy cells, cancerous cells are presented in Figure 1B, where healthy cells have normal levels of these features, being presented, here, as a poor man with no money. In contrast, the tumor cells are rich and have a lot of money due to an altered tumor cell metabolism and/or different gene expression level, arising from an uncontrolled cell division.11
Intrinsic-activation differs from extrinsic-activation, where in the latter the tumor is subjected to damage using external factor(s) as sketched in Figure 1C, where the tumor (house) is vulnerable to external factors (humor).
pH-Dependent Intrinsic-Activation
Nano-systems can be constructed where changes in acidity triggers drug release from its nano-formula, so pH differences between healthy and malignant cells can result in organ-specific release, tissue-specific release or cell-specific release, as clarified in Figure 2.
Organ-Specific Release
The gastrointestinal tract pH environment is rapidly changing, to assist maintaining its regular function, from the stomach acidic pH (1.5–3.5) to the intestinal alkaline pH (5.1–7.8).12 Using nano-bio-medicine is considered an advanced technique in which orally delivered medications can be targeted to specific parts of the gastrointestinal tract (GIT), for example it can be used for localized treatment of stomach cancer and colorectal malignancies.13 Generally, oral drug absorption occurs at the intestine, especially the ileum, owing to the large surface area provided by epithelial folding and the villous structures. Unfortunately, the acidic pH of the stomach hindered this process, by causing drug denaturation, with decreased effective drug concentration reaching the ileum, and consequently, drug resistance occurs.14,15 In contrast, using pH activated NPs protects the cargo, controlling its release, mainly, at the target site (ileum).16 Indeed, it seems like hiding the drug to escape from the stomach acidic pH, like a policeman and thief (Figure 2A). So, the drug release from the NPs commences only in the intestinal alkaline pH. This facilitates oral delivery of anti-tumor substances with efficient concentration using pH-sensitive polymers such as poly lactic-co-glycolic-acid (PLGA)17 and poly acrylic acid (PAA).18 As reported by Tian et al oral administration of doxorubicin (DOX) by PAA coated mesoporous silica NPs (MSNPs) occurs when the nano-system reaches the colon's high pH, then PAA degrades, releasing the drug.18
A self-micro-emulsifying DDS was used to increase the solubility and adsorption rate of natural anti-cancer drugs suffering from low bioavailability, such as curcumin. Through pH responsive release in the gastrointestinal tract, curcumin carried on this NC, its bioavailability increased. This system carrying curcumin showed a 21 nm average particle size when diluted in water with an increased rate of adsorption of >90% within 12 h as compared with only 20% of the free curcumin.19
Tissue-Specific Release
Tumor tissue exhibits lower microenvironmental pH than normal cells. This is attributed to the “Warburg” effect or “aerobic glycolysis” taking place in the tumor tissue, where the glycolytic product pyruvate is reduced by lactate dehydrogenase (LDH) enzyme into lactic acid, instead of undergoing oxidation in the Krebs cycle, to give ATP.20–22 This could be used to render smart nano-sized pH-activated systems to release cargo, only after accessing tumor tissue in a slightly acidic environment (pH ~ 6.0–6.5). Qian et al designed a nano micelle encapsulating anti-cancer drug system containing two peptides on its surface together with an aggregation-induced emission moiety, where those peptides are pH-responsive peptides and the system remains intact till reaching the tumor acidic pH, where it releases the cytotoxic drug to commence apoptosis. Now, the aggregation-induced emission moiety is released to give fluorescence upon apoptosis induction, as a monitor for the therapeutic effect.23 Moreover, Ko et al designed a pH-responsive block copolymer encapsulating DOX and under aqueous conditions this copolymer forms nano-sized self-assembled micelles. On reaching the tumor acidic microenvironment, a pH-dependent micellization-demicellization behavior takes place, with controlled drug release at the tumor site. This formula was found to suppress tumor growth in B16F10 tumor-bearing mice and prolonged survival vs using free DOX.24 Similarly, Lee et al used a pH-sensitive micelle copolymer containing DOX and using biotin as a ligand which is hidden, normally, by the micelle formula at normal pH conditions (normal cells). At the acidic tumor conditions, biotin enters cancer cells via biotin receptor-mediated endocytosis in a short time period, to allow specific drug release at the tumor tissue. It is noteworthy to mention that this formula gives a chance to make use of endosomal membrane disruption by the micelle components.25
Cell-Specific Release
Knowing that on the cellular level there is a great difference between cancerous and normal cells' pH, attributed to the lysosomal machinery that give the cancerous cells the feature of responsive release.26 Normal cells pH is maintained by the lysosomes in the acidic range (4.5–6.5), whereas, lysosomes keep acidic pH in cancerous cells below 4.5.27–29 This variation in the acidic pH level provides a good environment for localizing drug release from pH-sensitive nanomaterials that act as a body guard to protect their cargo from lysosomal enzymes as RNA interference (RNAi) for example which is a lysosome-sensitive cargo30 as illustrated in Figure 2B where Spike, the dog, protects Jerry, the mouse, from being attacked by Tom, the cat, till reaching his destination. α-Cyclodextrin nano-valves complexed with an aniline-based stalk on the surface within MSNPs, when, after entering the tumor cell, the lysosomal acidic pH activates these nanovesicles by weakening the link between the stalk and the cyclodextrin, allowing the anti-cancer drug release31 as shown in Figure 2C α-cyclodextrin nano-valves complexed with an aniline-based stalk is represented as a cap of a bottle that is being decomposed only by the action of tumor cell acidic pH releasing the cytotoxic drug. Muniswamy et al reported a drug delivery vehicle consisting of PLGA NPs with an outer layer of dendrimer-cationized albumin and encapsulated with DOX. In malignant cells, PLGA is degraded at a pH from 4.5 to 5.5 and releases the drug. This system, fortunately, can cross the blood brain barrier being beneficial for glioblastoma treatment.32 A pH-responsive polymeric micelle was formed by hydrophilic methyl ether poly (ethylene glycol) self-assembly and pH-responsive/biodegradable poly(beta-amino ester) copolymers carrying a fluorescence dye (tetra methyl rhodamine isothiocyanate) which is used for cancer imaging or carrying camptothecin for cancer therapy. Once the formula reaches the tumor site, the drug or the dye is released after copolymer degradation at the tumoral acidic pH (6.4).33
Gas-Generating pH-Sensitive Nano-System
It is noteworthy that using this system has a great effect in improving nano system efficiency, where CO2 gas generated from bicarbonate HCO3− in an acidic medium can aid in rupturing the pH-sensitive NP polymer, releasing the chemotherapeutic drug. Kim et al encapsulated sodium bicarbonate in PLGA NPs which decomposed to produce CO2 under acidic condition, releasing an imidazoquinoline-based synthetic toll-like receptor 7/8 agonist into tumor cells giving a great cytotoxic effect.34
pH-Responsive Metallic Nano-Materials
Titanium peroxide (TiOx) and Titanium dioxide (TiO2) have been widely used in nano-bio-medicine due to their biocompatibility and optical functionalities at neutral pH.35 This is due to the same idea as “secret ink” where the cytotoxic drug is nearly invisible at neutral pH, but becomes visible and produces an effect only under acidic pH as the releasing condition.
Calcium-based materials, such as calcium phosphate and calcium carbonate (CaCO3), can be used in treatment and diagnosis in conjugation with an anti-cancer drug due to their pH sensitivity and biodegradability with the ability to be functionalized by a ligand for targeting. Dong et al used DOX and Mn2+chelated chlorin e6 (Ce6(Mn)) as a photosensitizer both carried on CaCO3 NPs coated by poly-ethylene glycol (PEG). Once it arrives at the malignant acidic pH, it releases the drug. The NP photosensitizer has two advantages, first to enhance the magnetic resonance imaging (MRI) signal, which provides continuous monitoring for drug release. Second, NP photosensitizer provides a photodynamic therapy. Thus, this system presents a combinatorial chemo and photodynamic therapy.36 Likewise, iron oxide NPs have been very promising pH-trigger release anti-cancer drug carriers, as proposed by Yue et al. Iron oxide nano-tubes were used in an acidic pH-activated release of paclitaxel, solving its low solubility at 4.5 pH.37
Enzyme-Dependent Intrinsic-Activation
Enzymes dysregulation plays an important role in cancer pathogenesis, since they are responsible for many biological and metabolic activities.38 By synthesizing ligand-conjugated nano systems having high affinity to attach tumor-overexpressed enzymes (endogenous enzymatic-dependent activation) or using exogenous enzymes to contribute specific targeted nano system activation in tumor cells (exogenous enzyme dependent activation); enzymes have a great role in cancer treatment.
Endogenous Enzymatic-Dependent Intrinsic-Activation
Enzyme expression levels in tumor cells is higher than in normal cells.39 These enzymes include cathepsins, matrix metallo-proteinases (MMPs), hyaluronidase (HAase), glycosyl hydrolases, NAD(P)H-quinone oxidoreductase-1 (NQO1), protein tyrosine kinase-7 (PTK-7), and telomerase, as summarized in Table 1.
 |
Table 1 Enzyme-Dependent Intrinsic-Activation of Anti-Cancer Drug's NPs |
Table 1 enumerates enzyme-dependent intrinsic-activation of anti-cancer drugs in NP form.
Each of these enzymes have the ability to attach to a certain substrate, thus, by conjugating a chemotherapeutic drug to the enzyme substrate, activation occurs massively at the tumor site, where the enzyme is located there, with minimal side effects to normal cells.11 This is sketched in Figure 3A, where the substrate attached to the anti-cancer drug (the rat holding cheese) is directed toward the overexpressed enzymes (trap) to get more cheese and once the rat is captured the free drug is released (cheese) at the tumor site, thus specific targeting is achieved.
Cathepsins
DOX was incorporated into gold nano-rods and coated by poly-L-lysine hydrobromide (PLL), when this nano-system reaches the tumor site, PLL is digested by cathepsins and subsequently, the drug is released. Villar-Alvarez et al reported that less than 50% of cancer cells were killed by the same concentration of DOX compared to the invented nano-system aided by cathepsin enzyme.40 Similarly, two protease degradable amphiphilic copolymers were proposed by Yildiz et al consisting of PLGA-PLL copolymers attached to PLA-PEG copolymers and were conjugated to NIR fluorophore used for tumor imaging without tissue invasion, in addition to carrying a cytotoxic drug. This system was degraded by cathepsin's high concentration at the tumor site releasing the anti-cancer drug.41
Matrix Metallo-Proteinases (MMPs)
There are 23 types of MMPs, some of them are used as potential biomarkers for cancer treatment as MMP-2 and MMP-14.42 While MMP-9 has the ability to dissolve gelatin/polyvinylpyrrolidone (PVP) giving the chance for responsive release. As a proof of concept, MMPs were incorporated in the presence of PVP enclosing mesoporous NPs containing dying molecules. After PVP was enzymatically degraded by MMPs, the colored molecules were released 10 times more than the other test group.43 Cyclic peptide inhibitor CTTHWGFTLC was used as a targeting peptide inhibiting MMP-2 and MMP-9. This peptide facilitates anti-cancer drug localization. It was observed that this peptide enhances liposomes and protein nanocages delivery in vivo in murine cancer models.44,45 Celina et al proposed a drug delivery vehicle composed of superparamagnetic iron oxide NPs ferumoxytol encapsulating azademethylcolchicine to suppress tumor angiogenesis. This vehicle is linked to an MMP-activatable peptide that, upon reaching the tumor site, the peptide is broken releasing free drug selectively in the tumor cells with much higher concentration than normal cells.46
Hyaluronidase (HAase)
Zhang et al designed a DDS that has a promising effect in treating cancer in which an MSNP enclosing DOX from the inside and with hyaluronic acid and desthiobiotin–SA complex on the outside blocking the pores. When reaching cancer cells, the MSNP-HA/DOX system enters tumor cells by receptor mediated endocytosis, then hyaluronic acid is degraded by overexpressed HAase releasing DOX.47 Similarly, in gene therapy Choi et al reported that RNAi can be delivered in a pH-responsive nano formula that protects the cargo. Concerning targeted delivery, the formula is functionalized by hyaluronic acid to enter cancer cells by receptor mediated endocytosis. The genetic delivery system is modified by engineered RNA receptor Zn(II)-dipicolylamine as it binds RNA via phosphate binding, in addition to an enhanced targeting, where a calcium phosphate coating was added to protect the phosphate binding from decomposition by ions in the blood stream or cell culture (in vivo or in vitro, respectively). At the tumor site the NPs undergo further decomposition by HAase to release the drug.48
Glycosyl Hydrolases
These enzymes have a role in catalyzing the hydrolysis of glycosidic bonds in complex sugars.49 Dzamukova et al proposed nano-tubes encapsulating a cytotoxic drug while using dextrin as the tube stopper, with glycosyl hydrolases overexpressed in cancer cells; dextrin will be degraded, so the cytotoxic drug was found at higher levels in tumor cells than normal cells, which proved targeting.50
Protein Tyrosine Kinase (PTK)
Huang et al reported a nano-particulated aptamer-lipid-PLGA hybrid that can administer paclitaxel and DOX, simultaneously. The aptamers used in this method can bind to PTK-7, expressed on the tumor cell membrane, then its structure changes and DOX is released.51
Nicotinamide Adenine Dinucleotide Phosphate Dehydrogenase (NAD(P)H: Quinone Oxidoreductase-1
Shin et al have conducted a novel nanoprobe named prodrug 1 which is a theragnostic system (therapeutic and diagnostic) which consists of 7-ethyl-10-hydroxycamptothecin (SN-38) as the anti-cancer drug, hydroquinone which helps in enzyme activation, with biotin being a targeting moiety, when the system is decomposed by NQO1 at the tumor site released (SN-38) which act by inhibiting topoisomerase I in the cell nucleus resulting in cell apoptosis.52,53
Telomerase
A novel DNA shell, called a hairpin, is attached to gold nanoparticles and has been developed with 3’ telomere primers that could be stretched by tumor cell's telomerase enzyme. Elongation of 3’ regions cause aptamer deconstruction, resulting in the release of the anti-cancer medication DOX and fluorescent carboxy fluorescein label within the aptamer,54 this stretching appears like peeling a banana as simplified in Figure 3B. In another study, gold NPs encapsulate oligonucleotide inhibitors for telomerase to stop its action, this system was decorated by a peptide to enhance penetration. Enhanced drug uptake and high drug concentration was seen in telomerase-positive cells, but not telomerase-negative cells, thus an anti-proliferative effect was maximized.55
Dual Enzyme-Intrinsic-Activation
It is possible to make use of the synergistic effects that can be applied by targeting two enzymes, by the dual enzyme activation method. This increases efficiency, accuracy, and circulation time. A gemcitabine-PEG coated CdSe/ZnS quantum dots nano-system interacts with both MMP-9 and cathepsin B to treat pancreatic cancer.56 DOX loaded nano-capsules were functionalized by folic acid to mediate active targeting by receptor mediated endocytosis, upon reaching the tumor site; the system disintegrates only in the presence of trypsin enzyme or hyaluronidase enzyme, or both, which is overexpressed in tumor cells.57
Exogenous Enzyme-Loaded NPs Intrinsic-Activation
A new approach was proposed to introduce an exogenous enzyme, other than those normally found in the human body. An organic silica-based nano-system was constructed to carry the hypoxia-sensitive prodrug (AQ4N) and glucose oxidase enzyme (exogenous enzyme). A high glutathione concentration in cancer cells degrades a silica nano-system releasing the AQ4N prodrug. Hypoxic tumor condition, induced by glucose oxidase through consuming oxygen for oxidizing glucose, will now activate this chemotherapeutic prodrug58 as shown in Figure 4A. Simply, the glucose oxidase enzyme, introduced in the silica-NPs, acts like the hand which removes the oxygen mask (oxygen environment surrounding drug) generating a hypoxic condition which activates the chemotherapeutic prodrug (the boy) as illustrated in Figure 4B. Similarly, silica NPs encapsulate the peroxidase enzyme (exogenous enzyme) and indole-3-acetic acid prodrug forming a pH-responsive system upon reaching tumor cells, the cargo released with the peroxidase activates the prodrug to active cytotoxic peroxyl radicals causing tumor cell death.59
Concentration-Dependent Intrinsic-Activation
The abnormal behavior of cancerous cells arising from either gene expression or altered cell metabolism, leads to differences in the concentration of some released bio-molecules either membrane proteins or soluble molecules, as listed in Table 2, which both will cause intrinsic activation of the nano-system treatment applied.
 |
Table 2 Differences in the Concentration of Bio-Molecules Released by Cancerous Cells in Relation to Anti-Cancer Drugs Activation from NPs |
Table 2 addresses the differences in the concentration of bio-molecules released by cancerous cells, in relation to anti-cancer drugs activation from its NPs package.
Membrane Proteins
Transferrin (Tf)
Transferrin is an iron-binding glycoprotein. With an increased tumor cell proliferation rate, there has been an increased demand for iron.83 Tf acts like a (taxi) which transports iron ions to Tf receptors (TfRs) placed on the tumor cell surface (garage) as depicted in Figure 5A. Thus, targeting TfRs using Tf as the ligand, is a good way to direct most anti-cancer drugs to the tumor site. Targeting efficiency is highly dependent on NPs concentration, ligand density, dosing time, and cell surface receptor expression level.84 Zhang et al used this mechanism in targeting nano sonosensitizers in tumor cells, this system is composed of protoporphyrin IX (PpIX) NPs which is a sonosensitizer (activated by ultrasound to give a cytotoxic effect) and conjugated to human holo-Tf as a ligand. Active targeting was achieved by entering the system using receptor mediated endocytosis into tumor cells. Once applying ultrasound on the tumor cells PpIX is activated releasing ROS and inducing apoptosis. Active targeting and improved penetration were detected by PpIX fluorescence in the tested groups that exceeded control groups.60 Similarly, using Tf as a ligand conjugated to chitosan-PEG NPs achieved active targeting for paclitaxel delivery, providing a high cytotoxic effect with almost no harm to normal cells.61 Interestingly, it has been reported that Tf-conjugated NPs have the ability to cross the blood brain barrier, giving a great chance to treat brain tumors.85,86
Epidermal Growth Factor Receptor (EGFR)
Epidermal growth factor receptor (EGFR) overexpression on tumor cell membranes is related to multi-drug resistance (MDR)87,88 and a poor cancer prognosis.89 To treat such resistance, an antibody drug conjugate (ADC) is used, such as cetuximab which is an EGFR-monoclonal antibody.90 Unfortunately, ADC was accompanied by limited carrying capacity for anti-cancer drugs.91 Roncato et al successfully solved this issue by conjugating cetuximab with avidin-nucleic-acid-nano-assemblies (ANANAS) that actually carried a higher concentration of DOX as ANANAS consists of around 50 avidin and 1200 biotin-binding sites that enhance targeting. Therefore, this system had a more powerful lethal effect in treating breast cancer than ADC alone or pure DOX; where it shows 70% killing of cancer cells compared to only 40% killing achieved by ADC using the same DOX concentration. Moreover, this system was tested in non-obese diabetic/severe combined immunodeficiency mice, where the tumor growth suppression was significantly higher than the control group, ADC group and pure DOX.62 Zhou et al proposed a combination therapy using EGFR inhibitor as gefitinib and DOX as an anti-cancer drug, both incorporated in the same NC. For sequential delivery of gefitinib followed by DOX, gefitinib was physically encapsulated via ion pairing in a nano system made of DOX conjugated poly(L-lactide)-block-PEG.63
Prostate-Specific Membrane Antigen (PSMA)
Prostate-specific embrane ntigen (PSMA) is a membrane antigen which is overexpressed in prostate, lung, breast, and colon cancer.92 PSMA takes both advantage of achieving targeting and enhancing therapeutic agent(s) internalization through its internalization motif.93,94 Mangadlao et al described a system in which the PSMA receptor binding ligand (PSMA-1) and the fluorescent photodynamic treatment medication PC4 were combined to a nanoparticle. Accumulation of the nano-system was achieved by binding of the PSMA-1 ligand to the cancer cell membrane, then upon applying a laser, activation of the Pc4 molecule occurred, and this system killed most of the cancer cells.65 A10 is an RNA aptamer reported ligand with a high affinity to bind PSMA, facilitating active targeting. Aiming to prostatic cancer treatment in tumor bearing mice, a unimolecular micelle encapsulated DOX was synthesized and functionalized by the A10 aptamer for targeting tumor cells overexpressing PSMA. Targeted unimolecular micelles exhibited a much higher DOX accumulation and cellular uptake in PSMA positive than non-targeted unimolecular micelles in both in vitro and in vivo studies. Moreover, this nano system activated PARP and caspase 3 protein cleavage to induce apoptosis via upregulated Bax expression and down regulated Bcl2. These micelles increased cell cycle regulators p21 and p27 protein's expression.64
Folate Receptor (FR)
Folate receptors (FRs) are overexpressed in about 40% of human cancers, thus, using folate as a ligand conjugated to a NC-anti-cancer drug will aid in cancer treatment targeting strategies.95 Breast tumors are known to overexpress FRs, folate conjugated to DOX-loaded polymeric gold NPs (GNPs) in combination with supplemental laser photothermal therapy was used. The combined FR with laser photothermal therapy demonstrated superior therapeutic efficacy than simple DOX treatment.68 Targeting FR was seen in a study conducted by Singh et al using quantum dots conjugated to folic acid ligand and anti-HER2 antibody, where higher drug internalization was observed by confocal laser scanning microscopic studies and subsequently enhanced targeting and cytotoxic effect.66 Similarly, systemic administration of biodegradable polymeric micelles PEG-PLGA encapsulating DOX and conjugated to folate were prepared by Yoo and Park.67
Human Epidermal Growth Factor Receptor2 (HER2)
Human epidermal growth factor receptor2 (HER2) studies showed that it is overexpressed in cancer patients, especially breast cancer, where it plays an important role in MDR, tumor recurrence, and is related to a poor prognosis.96,97 Kumar Singh et al used liposome loaded capecitabine (CAP) and to reduce the off-target effects of traditional CAP, the surface of the CAP-loaded liposome was modified with chitosan and a tumor homing peptide (THP) for specific targeting of the HER2-positive cancer cells. The targeted chitosan-THP-modified CAP-loaded liposome (CTHP-CAP-LPs) showed approximately 71% greater cellular internalization efficiency than the non-targeted formulation. Additionally, CTHP-CAP-LPs caused notable cytotoxicity in comparison to the non-targeted formulation because of the former’s higher specificity and cellular absorption in cancer cells overexpressing the HER2 gene.69 Ghassami et al proposed a nano formulation consisting of polymeric NPs loading docetaxel and functionalized by aptamer to target HER2 to treat ovarian cancer. This formula minimized the off-target side effects and provided a higher drug concentration in tumor cells.70
Estrogen Receptors (ER)
There is a significant overexpression in estrogen receptors (ER) in breast cancer patients,98–101 where the estrogen binds to ER and plays a vital role in cancer development. Mamnoon et al proposed a drug delivery system involving targeted administration of DOX by hypoxia-responsive polymeric NPs functionalized with 17-estradiol (E2) in ER-positive breast cancer cells. This system was well taken up by ER-positive cancer cells and showed higher cytotoxicity than non-targeted formula.71
Cluster of Differentiation-44 (CD-44)
Cluster of ifferentiation-44 (CD-44) is a transmembrane glycoprotein, which has a role in cell–cell and cell–matrix interactions, and controls hyaluronic acid metabolism, lymphocyte activation, and cytokine release in healthy tissue.102,103 Numerous cancer types have greater CD-44 expression. The enhanced serum level of CD-44 is employed as a diagnostic marker for estimating the tumor burden in colon and stomach cancers.104 Moreover, CD-44 expression level rises in correlation with the grade and stages of an invasive breast tumor.105 Li et al attempted to target the CD-44-over expressed cancer cells using carbon dots loaded with DOX functionalized by hyaluronic acid. By using the acid sensitive linker 4-carboxybenzaldehyde to facilitate DOX release from the vehicle in an acidic environment, tumor volume reduction of 77-88% occurred in mice treated groups.72 In human colon carcinoma cell lines, diiodostyryl bodipy NPs photosensitizer was conjugated to hyaluronic acid as a ligand to specifically target overexpressed CD-44 on tumor cells. Hyaluronic acid increased hydrophilicity and biocompatibility of the photosensitizer. Upon light irradiation, ROS is generated which induce apoptosis and cancer cell death, in addition to fluorescence restoration which was not applicable with diiodostyryl bodipy alone, due to its aggregation. Results showed that this formula succeeded in achieving targeting and photodynamically label and treatment of colon cancer.73
αvβ3 Integrin
αvβ3 Integrin is a member of the family of cell adhesion molecules involved in contacts between cells and the extracellular matrix (ECM). Integrin is essential for cell shape, motility, mitosis, cytokinesis, migration, and phagocytosis.106–108 MMP-2 and plasmin activation by integrin in tumor cells contribute to the destruction of the interstitial matrix and the basement membrane, which could hasten tumor invasion and metastasis.109 Yadav et al developed a DDS consisting of chitosan incorporating raloxifene and ligand for targeting. Increased cellular internalization and excellent encapsulation efficiency for raloxifene and high stability at acidic pH was utilized by this delivery system and increased the drug's lethal effect on cancer cells.74 The iRGD moiety can be used as a ligand as it binds preferentially to the integrin receptor, so, it has high penetration and targetability action. A protein NPs conjugated to the iRGD ligand was used and loaded with paclitaxel. Results demonstrated an enhanced drug uptake by cancer cells due to integrin-mediated endocytosis and a better antiproliferation effect.75
Biotin Receptor
Biotin is one member of vitamin B complex, that can bind and help in a cell's growth and development. The rapid proliferating cancer cells need to increase biotin uptake via overexpressing biotin receptors. Human serum albumin NPs (HSNs) functionalized with biotin molecules were disclosed by Taheri et al for the selective delivery of methotrexate (MTX) to breast cancer cells. More biotin molecules may have enabled more precise recognition of biotin-specific receptors on breast cancer cells, allowing for greater cellular internalization of MTX and an improved therapeutic response. MTX-HSNs with more biotin demonstrated remarkable tumor growth inhibition (about ten times lower in tumor volume than the non-targeted formulation).76
Luteinizing Hormone Releasing Hormone (LHRH) Receptor
Luteinizing hormone releasing hormone (LHRH) receptor is overexpressed in many tumors including breast, ovarian, endometrial, and prostate tumors.110,111 In an animal model of breast cancer Li et al used the LHRH peptide as a targeting moiety and investigated its targeting effectiveness and biodistribution using modified cisplatin-loaded micellar NPs. An improved internalization, cytotoxicity, and decrease of the tumor volume with minimum systemic toxicity were observed.77
Lectin
Lectin is a protein which binds to carbohydrates attached to protein molecules (glycan) which is overexpressed in cancer cells and is correlated with the neoplastic transformation and metastasis. Lectin has been used in treating colon cancer by targeting colon cancer cells.112 NPs can be conjugated to lectin to target cancer cells via lectin receptors. This is known as the “lectin-targeting pathway”. In contrast, carbohydrate moieties attached to NPs can be used to target cancer cell lectins in what is called a “reverse-lectin targeting pathway”.78 To confirm the drug's conjugate ability for enhancing targeting, either in primary or metastatic liver cancers, Phase I/II clinical trials have been completed using reverse-lectin targeting in which the targeting moiety “galactosamine” was attached to the polymer backbone encapsulating DOX, therefore, specific targeting and liver specific release was achieved.79
Soluble Molecules
Glutathione (GSH) concentration in cancerous cells is 1.7–7 fold higher than in normal cells.113 Nano-system's selectivity was enhanced using the difference in GSH concentration between cells. High GSH concentration causes degradable dendritic mesoporous organo-silica NPs (DDMON) disintegration via reducing the disulphide bond, together with the therapeutic drug release, with high selectivity to cancerous cells.80 In other words, as shown in Figure 5B high GSH concentration is like the fire that causes the bomb explosion (DDMON) and releases what is inside (the anti-cancer drug). Furthermore, a glutathione (GSH)-responsive NP was synthesized using a GSH-cleavable disulfide bond containing polyurethane to disintegrate upon being subjected to high GSH concentration at the tumor site, providing controlled and targeted release of cisplatin.81 To achieve a controlled release of paclitaxel used for treating lung cancer, a GSH-triggered NPs was synthesized showing 35% or 95% drugs release in response to high GSH concentration at the tumor site compared to 10% cumulative drug release (in 3 days) in normal cells (with normal GSH concentration), this formula gives a double recognition and targeted technique for both cancerous cells and tumor associated macrophages; providing a better chemotherapeutic effect.82
Dual stimuli responsive systems were used to treat prostate cancer cells, by incorporating the naturally-derived anti-cancer drug's Strigolactones analogues MEB55 and ST362, in GSH/pH-responsive nano sponges. At the tumor site, the nano sponge disintegrates releasing the drug in response to the acidic pH and further enhanced by high GSH concentration.114 Chiang et al used micelle encapsulating camptothecin that remains intact at normal redox (H2O2) and under normal GSH levels. At high redox or high GSH levels or both in the tumor milieu, micelles disintegrate releasing the anti-cancer drug.115
Extrinsic-Activation
Again, activation factors (like a hammer) from outside the tumor cell (wooden house), where this(ese) external effect(s) is/are applied to kill cancerous cells (house) (Figure 1c). Extrinsic-activation includes ultrasound, magnetic, as well as light-activation and X-ray activation.10
Ultrasound Extrinsic-Activation
Ultrasound is a favorable imaging tool for diagnosis and also a safe and efficient therapeutic tool.116
Sonoporation
As the cell membrane acts as a barrier to prevent chemotherapeutic drug entry, microbubbles are used to solve this. The bubbles travel through the body fluids and once they reach tumor cells, ultrasound is applied, then the microbubbles cause fluid streaming resulting in cell membrane poration that facilitates cytotoxic drug(s) entry leaving the microbubbles intact. This mechanism is known as “stable cavitation”117 as illustrated in Figure 6A. The cell membrane is like a boat and the microbubbles are balls underneath the boat. On applying ultrasound on these balls, they oscillate and hit the boat causing pore formation and therefore, drug entry. Alternatively, “inertial cavitation” in which bubbles collapse at the tumor site releasing ROS to aid in cell death. Furthermore, forming microjets and shockwaves that lead to pore formation, enhancing further uptake.118
Gas-Filled Microbubbles
A micron-sized bubble filled with perfluoro carbon gas and surrounded by a biocompatible polymer or protein was used, where the NPs can be delivered more efficiently by chemical attachment or encapsulation on or within the microbubble. NPs will be released at the tumor tissue and achieve specific targeting after applying ultrasound. NPs uptake was increased between 5–57 and 60–600 fold when administering the NPs using microbubble attachment119,120 together with an effective NPs penetration.121 This method was proposed to be used with potent anti-cancer drugs such as paclitaxel that is released directly after applying ultrasound and shell rupture.122 In cancer immunotherapy mRNA-lipoplexes bound to microbubbles were used to transfect dendritic cells. mRNA encoding tumor antigens trigger a tumor immune response. Results showed mRNA-lipoplexes to have efficient dendritic cell transfection using ultrasound activation where about 50% of the dendritic cells were successfully transfected. Cellular internalization and localization was detected by flow cytometry using fluorescently labeled lipoplexes.123 However, the major drawback is reduction of circulation time in addition to rapid microbubble destruction after applying ultrasound irradiation. In order to overcome these problems, nanobubbles composed of NPs enclosing gas is stabilized within a single cavity of nano-cups or nano-cones designed to increase the cavitation time 4-folds, till they reach the tumor site, where ultrasound is applied and subsequently the particles are detached from the nano-cups or nano-cones and continue to grow then collapse and are distributed in the surrounding tumor tissue. For example, using gold nanoparticles to deliver IgG mice antibodies in vivo.124 Moreover, activated imaging was enhanced using a “phase change contrast agent” which consists of perfluorocarbon gas particles coated with lipid shell containing fluorescent dye, forming nanosized lipid droplets. These droplets are vaporized into gaseous microbubble after ultrasound activation showing excellent imaging capabilities as well as providing a better therapeutic effect. Using folate as a ligand to target FR for treating MDA-MB-231 and MCF7 breast cancer cell lines, enhanced uptake 45-fold for MDA-MB-231 cells and 7-fold for MCF-7 cells in addition to improving microscope imaging and tracking the phase change.125
Piezoelectric Nanomaterials
The cell membrane is stabilized by a group of influx and efflux ions, once a disturbance happens in these ions, an altered cell growth and altered cell division occurs.126 Recently, “piezoelectric nanomaterials” have been used to change the fluctuation of cell membrane influx or efflux ions. These particles convert mechanical energy from the applied ultrasound into electrical energy which changes potassium and calcium levels and hence, s potential difference occurs to disrupt cell division causing cancer cell death.127,128 This is sketched in Figure 6B where the disturbance in ions is represented as traffic lights disturbance that may lead to car accidents (cell death).
Barium titanate is a piezoelectric NP conjugated to anti-HER2 antibody as a ligand for targeted therapy. After activation of this system with ultrasound, the barium titanate changes mechanical energy to electrical energy affecting potassium level and calcium homeostasis leading to cell arrest and suppression of breast cancer proliferation.129
Magnetic-Field Extrinsic-Activation
Magnetite (Fe3O4) and maghemite (-Fe2O3) are the most frequently used magnetic NPs as they are powerful tools in cancer treatment;130 as well as used as a contrast agents in MRI.131 In cancer therapy magnetic NPs can be heated up by an alternating magnetic field to exert a cytotoxic effect by inducing hyperthermia as well as providing a localized drug delivery,132 as summarized in Figure 7.
Magnetically-Induced Hyperthermia
The non-ionizing magnetic NPs are able to convert alternating magnetic energy into heat energy due to Brownian and Néel relaxation processes, the efficiency of the generated heat depends on many factors, such as the NP size, concentration, solution viscosity, magnetic field strength, and frequency.133
Ferro/ferric magnetic iron oxide nanoparticles (IONPs) or super paramagnetism IONPs (SPIONs)134,135 are particles having excellent biocompatibility.136 Moreover, they can act alone as a cancer therapy behaving as a single spin system achieving “super paramagnetism” using alternating magnetic fields with an increased local temperature up to 42 °C causing rapid tumor cell apoptosis with little effect on normal cells137,138 and inhibit the tumor proliferation and induces apoptosis.139 This is like “cancerous cells melt” (an ice cream subjected to heat) in Figure 7A. Furthermore, magnetic NPs produce mechanical stress and membrane deformation with the release of a large amount of Fe2+ ions, causing oxidative stress via the “Fenton reaction” to induce cancer cell death.140 A large pore-sized and biodegradable dendritic silica NP was used, encapsulating glucose oxidase and Fe3O4 NPs, simply glucose oxidase acts as an enzyme catalyst that depletes most of the tumor glucose and results in H2O2 production. Fe3O4 NPs catalyze H2O2 by Fenton-like reactions to form a toxic hydroxyl radical, causing apoptosis and cell death.141
Magnetically-Induced Localized Drug Release
SPIONs have the ability to enhance a tumor-directed effect due to their nano-size range giving either active or passive targeting as mentioned before. Various anti-cancer drugs, including paclitaxel, methotrexate, mitoxantrone, and DOX, have been conjugated with magnetic NPs to increase their target specificity.142,143
Tumor-Targeting with Nano Immunoliposome Platform Technology
Coating SPIONs with polymers as amino-PVA increases the interaction of those NPs with cancer cells and diminishes its interaction with normal cells.144 However, this coating may affect the super paramagnetic property of SPIONs, so, encapsulating the drug-loaded SPIONs within a cationic liposome has a great benefit as reported by Yang et al. In addition to facilitating active targeting towards cancer cells by functionalizing the formula with the TfR-antibody to improve the cytotoxic action.145
Generally, nano systems composed of chemotherapeutic drugs trapped into IONPs and carried by liposomes or micelles whose shell is made of a thermos-sensitive polymer such as poly-N (isopropylacrylamide) or poly (vinylcaprolactame) can be activated by one of these two methods either being exposed to an alternating magnetic field resulting in heating of IONPs, changing the polymer structure with the final release of the trapped chemotherapy making them an excellent choice for controlled release drug delivery agents or exposed to a permanent magnetic field causing IONPs to drag and squeeze the liposomes at a point resulting in its rupture and drug release.146–149 This is presented in Figure 7B in which IONPs (chick) force the liposomes (egg) to release what is inside (IONPs-containing anti-cancer drug).
Smart Stimulus System/Innovative Nanodevice
Magnetite particles used as a pore blocking instrument in an innovative nanodevice to selectively release vitamin B12 and DNA from polymeric biodegradable multi-reservoir device according to the desired concentration and duration in a pulsed or burst manner depending on the magnetic field direction. In Figure 7C the magnetite particles (a window) that open or close to allow sunlight entry (drug) according to wind direction (alternating magnetic field direction).150
Magnito-fection is a process of cellular transfection of genetic material like RNAi or DNA using a magnetic field for higher transfection efficiency and rapid sedimentation of the gene-therapeutic agent onto the target area.151,152 Hu et al used a cationic lipopeptides and anionic magnetic NPs (MNPs) system. By applying the magnetic field, it aids in transfection of miR-125b, that not only regulates the tumor-associated macrophage polarization (upregulate genes responsible for M1 phase and down regulate genes responsible for M2 phase) and tumor cell inhibition, by targeting ETS proto-oncogene 1 and cyclin-J. Results showed tumor weight reduction of 60% and tumor metastasis suppression of 50%.153 Similarly, magnetic NPs were used for efficient transfection of microRNA-374a in glioma stem cells.154 A combination of cationic lipid N,N-di-n-hexadecyl-N,N-dihydroxyethyl ammonium chloride formulated with co-lipid cholesterol together with magnetic NPs was used to enhance DNA uptake by human glioblastoma-astrocytoma, epithelial-like cell line, hepatocellular carcinoma, cervical cancer, and breast cancer cells, where enhanced transfection was observed after applying the magnetic field.155
Extrinsic Light-Activation / Photodynamic Therapy (PDT)
PDT has been used in cancer treatment for many years, using a non-toxic, light sensitive photosensitizer dye, applied by systemic or topical administration. Once the photosensitizer is excited by using the appropriate wavelength in the presence of molecular oxygen, ROS is generated leading to a cytotoxic effect on cancer cells. Despite the great success made by PDT in cancer treatment, its usage became limited due to light's weak-penetration effect.156 In addition to lack of specificity of phototherapeutic agents that decrease efficacy and bioavailability with serious side effects. Using photosensitizer together with a NC or photon-up-conversion NPs holds the potential to act as a NC for photosensitizers with the adv. of localized action and higher efficiency as well as higher penetration depth than that of the conventional PDT157–159 as simplified in Figure 8. The above mechanism is like a billiard game where the billiard stick (light energy) hits the ball (nanocarrier) to transfer energy to the following ball (photosensitizers) that acquire a high energy to reach the pocket and achieve the ultimate goal (kill cancer cells).
Alternative excitation sources include near infrared light or X-ray are presented in the next section.160
Table 3 addresses photodynamic extrinsic-light-activation of anti-cancer drugs in NPs advantages and disadvantages, applications, and factors affecting action of different types of extrinsic-light-activation either near infrared (NIR),161,162 visible light163,164 or X-ray.165
 |
Table 3 Photodynamic Extrinsic-Light-Activation of Anti-Cancer Drugs in NPs Formula164 |
Combinatorial Intrinsic-Extrinsic-Activation
The addition of targeting moieties or the integration of other capabilities, such as focused radiation or ultrasound, can help improve targeting. Encapsulating calcium carbonate (CaCO3) which is a pH-sensitive metallic (intrinsic activation) NP within a PLGA coating, simultaneously used in conjugation with ultrasound (extrinsic activation) to enhance release and action.173 Moreover, the surface would be functionalized using rabies virus glycoprotein to enhance targeting to neuroblastoma cells.174 Encapsulating DOX in a drug delivery vehicle composed of TiO2 particles doped with Gd as a sonosensitizer and pH-sensitive NC for DOX. Once the NPs accumulated in the tumor tissue, amines in the coating are protonated which results in an influx of ions and subsequently lowers the osmotic potential. Consequently, the coating bursts (intrinsic activation) and releases the polymer-DOX nano-complex into the cancer cells. Then irradiation by ultrasound source (extrinsic activation) is carried out at the tumor site with ROS production to induce cell death at the tumor site.175
A nano formulation was designed consisting of DOX-loaded on reduced albumin-based NPs. Once the formulation reaches the tumor site, releasing DOX was achieved in response to the acidic-tumor microenvironment (intrinsic activation). Using ultrasound improves the targeted drug delivery by disrupting the endothelial linings by microbubble-assisted cavitation (extrinsic activation) that opens the road in front of the chemotherapeutic drug.176
Smart Nano-Reactor
Smart nano-reactor was designed to enhance the therapeutic outcome of PDT using a hollow silica NP encapsulating system, in its inner cavities catalase which is water-soluble H2O2-decomposing enzyme. Doping chlorine e6 (Ce6) as a photosensitizer into the silica lattice structure, was functionalized with (3-carboxypropyl)triphenyl phosphonium bromide which is a mitochondrial targeting moiety, further modified by acidic pH-responsive charge-convertible polymer (intrinsic activation). After reaching the tumor site, the pH-responsive polymer was degraded, releasing the catalase enzyme to produce O2 from H2O2 to overcome tumor hypoxia and further enhance in vivo PDT efficacy. Therefore, by applying light (extrinsic activation) the photosensitizer has the ability to use O2 in the tumor tissue and release ROS that kills cancer cells. Moreover, to overcome metastasis, scientists added an immune check-point inhibitor as programmed death-ligand 1 (PD-L1) antibody to promote cytotoxic T-lymphocytes infiltration into distant tumors.177 A pH-sensitive nano system was fabricated composed of dendrimer premixed with PAA through ionic interaction carrying DOX as a chemotherapeutic drug and indocyanine green which is a photothermal agent. This system was functionalized by PEG and herceptin to allow active targeting to HER2 in tumor cells. Furthermore, NIR irradiation (extrinsic activation) produces a considerable heat that induces apoptosis and promotes cell death.178 Ihsanullah et al proposed a nano system in which NPs made of amphiphilic polymers were synthesized incorporating two drugs (photosensitizer chlorine e6 (Ce6) and hypoxia activatable prodrug tirapazamine) and this NC is attached to a peptide. By applying external laser irradiation (extrinsic activation), the proximal cells from the vessel having sufficient oxygen content undergo PDT in which photosensitizer releases a singlet oxygen promoting cell death.179 Zhao et al used magnetic NPs Fe3O4 to synthesize a pH-responsive nano system, this was done by using acid-labile imine bonds to conjugate RGD (targeting moiety) and DOX to the magnetic NPs. Upon reaching the tumor acidic pH (intrinsic activation), the drug is released. Moreover, by the application of external magnetic field (extrinsic activation), the anti-cancer activity of the magnetic NPs is more enhanced than free DOX due to localized action and enhanced drug uptake by cancerous cells.180
State-of-The Art Nano-Robots for Cancer Therapy
Nano-robots are gadgets, between 0.1 and 10 micrometers in size.181 A nano-robot is a clever robot which can patrol the bloodstream, identify a specific target being diagnostic and deliver little lethal NP cargoes to destroy cancer cells,182 as used for brain tumors. Nano-robots seem like a fire alarm system that detects fire (diagnosis) and rapidly releases water (drug) to put the fire out (therapy). A full option nanobot was designed to contain all the desired facilities to achieve targeted, fast, and localized action at the tumor site. One nanobot is a multi-walled carbon nanotube (CNT) used as a carrier for DOX targeting, enhanced by first, addition of an anti-epithelial cell adhesion molecule monoclonal antibody (anti-EpCAM mAb) targeting ligand and second, by chemical co-ordination with Fe3O4 NPs for autonomous propulsion ability as well as superparamagnetic property providing localized action.183
Evaluating Intrinsic and Extrinsic-Activation Techniques
It is noteworthy to mention that every activation method, either intrinsic or extrinsic, has its advantage and/or disadvantage. Both of them definitely aim to achieve the highest concentration of chemotherapeutic drug at the target site together with decreasing off-target effects.
Concerning intrinsic activation, pH-dependent activation makes use of the difference in pH among cancer and healthy cells that can improve selective activation. Moreover, combination with other functionalities such as directed radiotherapy or ultrasound can improve activation and action. In a similar manner, although enzymes are found in both cancer and normal cells, but the difference in their expression level gives us an opportunity to use it as a way for targeted release and localized action. This is achieved by using a substrate being linked to the chemotherapeutic drug, where drug release is achieved only after attaching the substrate to the over-expressed enzyme at the tumor site mainly. Similarly, in concentration-dependent activation most of these molecules are found in both normal and cancerous cells, however, the difference in concentration of either membrane proteins or soluble molecules with the aid of functionalized ligands, the system is directed to the target site and selective activation is achieved. On the other hand, during extrinsic activation, ultrasound low penetration through bone and air, results in problems in activation in lungs or ribcage. More importantly, due to the risk of inertial cavitation causing petechial hemorrhage, some ultrasound frequencies cannot be used to treat cerebral tumors.184 Increased poration causes therapeutic molecules to accumulate in unwanted tissues/organs, especially when conducted adjacent to the vascular tissue, which limits sonoporation.185
Activation with NIR light has offered a stimulus that is inexpensive, safe, and has few side effects to healthy tissues. However, skin penetration depths are below 4 mm186 limiting the technique's utility. X-ray activation technique can be used as it penetrates deeply, reaching deep tumors,169 can be applied easily using hospital equipment and gives minimal side effects, but only has a weak ability of X-ray for photosensitizer activation.171 A more effective technique can be applied which is magnetic field activation due to its high penetration depth, non-ionizing property, and localized action to ensure normal cell's safety.187
Table 4 summarizes the advantages vs disadvantages of anti-cancer drug NPs various intrinsic and extrinsic-activation methods.
 |
Table 4 Advantages Vs Disadvantages of Anti-Cancer Drugs NPs Various Intrinsic and Extrinsic-Activation Methods |
Summary and Conclusion
One of the drawbacks of chemotherapy is the lack of specificity and MDR. Nano-bio-medicine fabricated a NC to carry anti-cancer drug(s) directly to the tumor site, where activation either intrinsic or extrinsic or a combination is selected, in order to release the NP-entrapped drug to perform its cytotoxic action precisely and selectively.
Therefore, activatable therapies have the capacity to deliver toxic medications, precisely, where they are only needed at the tumor site, with decreased off-target events and side effects as well as achieving less mortality among cancer patients.
Strength
“No-harm, no-toxicity-to-the normal” is the insignia of nano-bio-medicine, therefore, targeted-drug delivery is a dynamic innovative field, trying to provide the best chemotherapeutic effect with minimal off-target effect(s) while ensuring overcoming cancer cell escape. These ideas were presented in the current review in simple, innovative, illustrative cartoon-simulation figures.
Recommendation
Either intrinsic-activation or extrinsic-activation of NPs cargos, free or not, or a combination of them, were all exploited experimentally, and need to go more into the clinical phase. MDR, remains one more obstacle that hinders the proper action of NPs carrying anti-cancer drugs (an issue that is addressed, currently, by our research group in an ongoing review).
Abbreviations
ADC, antibody drug conjugates; ANANAS, avidin-nucleic-acid nano-assemblies; CaCo3, calcium carbonate; CNTs, carbon nanotubes; CAP, capecitabine; CD-44, cluster of differentiation 44; Ce6, chlorin E6 photosensitizer; CTHP-CAP LPs, chitosan tumor homing peptide capecitabine liposome; DDMON, degradable dendritic mesoporous organosilica nanoparticle; DDS, drug delivery system; DOX, doxorubicin; ECM, extracellular matrix; EGFR, epidermal growth factor receptor; EPR, enhanced permeability and retention effect; ER, estrogen receptor; E2, estradiol; FR, folate receptor; GIT, gastrointestinal tract; GOx, glucose oxidase enzyme; GSH, glutathione; HAaSe, hyaluronidase; HER2, human epidermal growth factor receptor 2; HSNs, human serum albumin nanoparticles; IONPs, iron oxide nanoparticles; LDH, lactate dehydrogenase; LHRH, luteinizing hormone releasing hormone; MDR, multidrug resistance; MMPs, matrix metalloproteinases; MRI, magnetic resonance imaging; miR-145 MNPF, Mir-145-based magnetic nanoparticle formulation; MSNPs, mesoporous silica nanoparticles; MTX, methotrexate; miRNA, micro-RNA; NAD(P)H, nicotinamide dinucleotide phosphate; NADH, nicotinamide dinucleotide; NQO1, NAD(P)H quinone oxidoreductase-1; NCs, nanocarriers; ncRNA, non-coding RNA; NF-Κb, nuclear factor kappa B cell; NIR, near infrared; NPs, nanoparticles; NT, nanotechnology; PAA, poly acrylic acid; PD-L1, programmed death-ligand 1; PTX, paclitaxel; PDT, photodynamic therapy; PEG, polyethylene glycol; PpIX, protoporphyrin IX; PLA, poly lactic-acid; PLGA, poly lactic-co-glycolyic acid; PLL, poly-L-lysine hydrobromide; PSMA, prostate specific membrane antigen; PTK-7, protein tyrosine kinase-7; PVP, poly-vinyl pyrrolidone; RNA I, RNA interference; ROS, reactive oxygen species; SiRNA, small interfering RNA; SPIONs, super paramagnetic iron oxide nanoparticles; TfRs, transferrin receptors; TF, transferrin; THP, tumor homing peptide; TiOx, titanium peroxide; TiO2, titanium dioxide; UCN, up conversion nanoparticles.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. doi:10.3322/caac.21551
2. Gavas S, Quazi S, Karpiński TM. Nanoparticles for cancer therapy: current progress and challenges. Nanoscale Res Lett. 2021;16(1):173. doi:10.1186/s11671-021-03628-6
3. Zitvogel L, Apetoh L, Ghiringhelli F, et al. Immunological aspects of cancer chemotherapy. Nat Rev Immunol. 2008;8(1):59–73. doi:10.1038/nri2216
4. Ehrlich P. Experimental Researches on Specific Therapy: Chemotherapeutic Studies on Trypanosomes: THIRD HARBEN LECTURE, in the Collected Papers of Paul Ehrlich. Elsevier; 1960:130–134.
5. Aslam MS, Naveed S, Ahmed A, et al. Side Effects of Chemotherapy in Cancer Patients and Evaluation of Patients Opinion about Starvation Based Differential Chemotherapy. J Cancer Ther. 2014;5:817–822. doi:10.4236/jct.2014.58089
6. Dadwal A, Baldi A, Kumar Narang R. Nanoparticles as carriers for drug delivery in cancer. Artif Cells, Nanomed Biotechnol. 2018;46(sup2):295–305. doi:10.1080/21691401.2018.1457039
7. Subhan MA, et al. Recent Advances in Tumor Targeting via EPR Effect for Cancer Treatment. J Pers Med. 2021;11(6):56.
8. Large DE, Soucy JR, Hebert J, et al. Advances in receptor-mediated, tumor-targeted drug delivery. Adv Therapeutics. 2019;2(1):1800091. doi:10.1002/adtp.201800091
9. White BD, Duan C, Townley HE. Nanoparticle Activation Methods in Cancer Treatment. Biomolecules. 2019;9(5):98.
10. Racca L, Cauda V. Remotely Activated Nanoparticles for Anticancer Therapy. Nano Micro Lett. 2020;13(1):11. doi:10.1007/s40820-020-00537-8
11. Abdolmaleki A, Asadi A, Gurushankar K, et al. Importance of Nano Medicine and New Drug Therapies for Cancer. Adv Pharm Bull. 2021;11(3):450–457. doi:10.34172/apb.2021.052
12. Fallingborg J. Intraluminal pH of the human gastrointestinal tract. Dan Med Bull. 1999;46(3):183–196.
13. Alqahtani MS, Kazi M, Alsenaidy MA, et al. Advances in Oral Drug Delivery. Front Pharmacol. 2021;12. doi:10.3389/fphar.2021.618411
14. Stuurman FE, Nuijen B, Beijnen JH, et al. Oral anticancer drugs: mechanisms of low bioavailability and strategies for improvement. Clin Pharmacokinet. 2013;52(6):399–414. doi:10.1007/s40262-013-0040-2
15. Bradley G, Juranka PF, Ling V. Mechanism of multidrug resistance. Biochimica et Biophysica Acta. 1988;948(1):87–128. doi:10.1016/0304-419X(88)90006-6
16. Mathur P, Rawal S, Patel B, et al. Oral delivery of anticancer agents using nanoparticulate drug delivery system. Curr Drug Metab. 2019;20(14):1132–1140. doi:10.2174/1389200220666191007154017
17. El-Sherbiny IM, Abdel-Mogib M, Dawidar A-AM, et al. Biodegradable pH-responsive alginate-poly (lactic-co-glycolic acid) nano/micro hydrogel matrices for oral delivery of silymarin. Carbohydr Polym. 2011;83(3):1345–1354. doi:10.1016/j.carbpol.2010.09.055
18. Tian B, Liu S, Wu S, et al. pH-responsive poly (acrylic acid)-gated mesoporous silica and its application in oral colon targeted drug delivery for doxorubicin. Colloids Surf B Biointerfaces. 2017;154:287–296. doi:10.1016/j.colsurfb.2017.03.024
19. Cui J, Yu B, Zhao Y, et al. Enhancement of oral absorption of curcumin by self-microemulsifying drug delivery systems. Int J Pharm. 2009;371(1–2):148–155. doi:10.1016/j.ijpharm.2008.12.009
20. Jiang B. Aerobic glycolysis and high level of lactate in cancer metabolism and microenvironment. Genes Dis. 2017;4(1):25–27. doi:10.1016/j.gendis.2017.02.003
21. Jang M, Kim SS, Lee J. Cancer cell metabolism: implications for therapeutic targets. Exp Mol Med. 2013;45(10):e45–e45. doi:10.1038/emm.2013.85
22. Deberardinis RJ. Is cancer a disease of abnormal cellular metabolism? New angles on an old idea. Genetics Med. 2008;10(11):767–777. doi:10.1097/GIM.0b013e31818b0d9b
23. Qian Y, Wang Y, Jia F, et al. Tumor-microenvironment controlled nanomicelles with AIE property for boosting cancer therapy and apoptosis monitoring. Biomaterials. 2019;188:96–106. doi:10.1016/j.biomaterials.2018.10.003
24. Ko J, Park K, Kim Y-S, et al. Tumoral acidic extracellular pH targeting of pH-responsive MPEG-poly(beta-amino ester) block copolymer micelles for cancer therapy. J Control Release. 2007;123(2):109–115. doi:10.1016/j.jconrel.2007.07.012
25. Lee ES, Na K, Bae YH. Super pH-sensitive multifunctional polymeric micelle. Nano Lett. 2005;5(2):325–329. doi:10.1021/nl0479987
26. Griset AP, Walpole J, Liu R, et al. Expansile Nanoparticles: synthesis, Characterization, and in Vivo Efficacy of an Acid-Responsive Polymeric Drug Delivery System. J Am Chem Soc. 2009;131(7):2469–2471. doi:10.1021/ja807416t
27. Glunde K, Guggino SE, Solaiyappan M, et al. Extracellular Acidification Alters Lysosomal Trafficking in Human Breast Cancer Cells. Neoplasia. 2003;5(6):533–545. doi:10.1016/S1476-5586(03)80037-4
28. Fennelly C, Amaravadi RK. Lysosomal Biology in Cancer. Methods Mol Biol. 2017;1594:293–308.
29. Chen R, Jäättelä M, Liu B. Lysosome as a Central Hub for Rewiring PH Homeostasis in Tumors. Cancers. 2020;12(9):2437. doi:10.3390/cancers12092437
30. Chen X, Mangala LS, Rodriguez-Aguayo C, et al. RNA interference-based therapy and its delivery systems. Cancer Metastasis Rev. 2018;37(1):107–124. doi:10.1007/s10555-017-9717-6
31. Hwang AA, Lu J, Tamanoi F, et al. Functional nanovalves on protein-coated nanoparticles for in vitro and in vivo controlled drug delivery. Small. 2015;11(3):319–328. doi:10.1002/smll.201400765
32. Muniswamy VJ, Raval N, Gondaliya P, et al. ‘Dendrimer-Cationized-Albumin’ encrusted polymeric nanoparticle improves BBB penetration and anticancer activity of doxorubicin. Int J Pharm. 2019;555:77–99. doi:10.1016/j.ijpharm.2018.11.035
33. Min KH, Kim J-H, Bae SM, et al. Tumoral acidic pH-responsive MPEG-poly(beta-amino ester) polymeric micelles for cancer targeting therapy. J Control Release. 2010;144(2):259–266. doi:10.1016/j.jconrel.2010.02.024
34. Chu S, Shi X, Tian Y, et al. pH-Responsive Polymer Nanomaterials for Tumor Therapy. Front Oncol. 2022;12. doi:10.3389/fonc.2022.855019
35. Dai Z, Song X-Z, Cao J, et al. Dual-stimuli-responsive TiO x /DOX nanodrug system for lung cancer synergistic therapy. RSC Adv. 2018;8(39):21975–21984. doi:10.1039/C8RA02899K
36. Dong Z, Feng L, Zhu W, et al. CaCO(3) nanoparticles as an ultra-sensitive tumor-pH-responsive nanoplatform enabling real-time drug release monitoring and cancer combination therapy. Biomaterials. 2016;110:60–70. doi:10.1016/j.biomaterials.2016.09.025
37. Yue Z-G, Wei W, You Z-X, et al. Iron Oxide Nanotubes for Magnetically Guided Delivery and pH-Activated Release of Insoluble Anticancer Drugs. Adv Funct Mater. 2011;21(18):3446–3453. doi:10.1002/adfm.201100510
38. Lee MR, Baek K-H, Jin HJ, et al. Targeted enzyme‐responsive drug carriers: studies on the delivery of a combination of drugs. Angewandte Chemie. 2004;116(13):1707–1710. doi:10.1002/ange.200353204
39. Baig MH, Adil M, Khan R, et al. Enzyme targeting strategies for prevention and treatment of cancer: implications for cancer therapy. Semin Cancer Biol. 2017;56:566.
40. Villar-Alvarez E, Cambón A, Pardo A, et al. Gold Nanorod-Based Nanohybrids for Combinatorial Therapeutics. ACS omega. 2018;3(10):12633–12647. doi:10.1021/acsomega.8b01591
41. Yildiz T, Gu R, Zauscher S, et al. Doxorubicin-loaded protease-activated near-infrared fluorescent polymeric nanoparticles for imaging and therapy of cancer. Int J Nanomedicine. 2018;13:6961–6986. doi:10.2147/IJN.S174068
42. Li X, Kim J, Yoon J, et al. Cancer-Associated, Stimuli-Driven, Turn on Theranostics for Multimodality Imaging and Therapy. Adv Mater. 2017;29(23)8963.
43. Nairon K, Samykutty A, McNally MW, et al. Enzymatically-responsive tumor-targeted mesoporous silica nanoparticle for identification of pancreatic cancer. Cancer Res. 2018;78(13_Supplement):4664. doi:10.1158/1538-7445.AM2018-4664
44. Penate Medina O, Haikola M, Tahtinen M, et al. Liposomal Tumor Targeting in Drug Delivery Utilizing MMP-2- and MMP-9-Binding Ligands. J Drug Deliv. 2011;2011:160515. doi:10.1155/2011/160515
45. Kawano T, Murata M, Piao J, et al. Systemic Delivery of Protein Nanocages Bearing CTT Peptides for Enhanced Imaging of MMP-2 Expression in Metastatic Tumor Models. Int J Mol Sci. 2015;16:148–158. doi:10.3390/ijms16010148
46. Ansari C, Tikhomirov GA, Hong SH, et al. Cancer Therapy: development of Novel Tumor-Targeted Theranostic Nanoparticles Activated by Membrane-Type Matrix Metalloproteinases for Combined Cancer Magnetic Resonance Imaging and Therapy (Small 3/2014). Small. 2014;10(3):417. doi:10.1002/smll.201470016
47. Zhang M, Xu C, Wen L, et al. A hyaluronidase-responsive nanoparticle-based drug delivery system for targeting colon cancer cells. Cancer Res. 2016;76(24):7208–7218. doi:10.1158/0008-5472.CAN-16-1681
48. Choi KY, Silvestre OF, Huang X, et al. Versatile RNA Interference Nanoplatform for Systemic Delivery of RNAs. ACS Nano. 2014;8(5):4559–4570. doi:10.1021/nn500085k
49. Davies G, Henrissat B. Structures and mechanisms of glycosyl hydrolases. Structure. 1995;3(9):853–859. doi:10.1016/S0969-2126(01)00220-9
50. Dzamukova MR, Naumenko EA, Lvov YM, et al. Enzyme-activated intracellular drug delivery with tubule clay nanoformulation. Sci Rep. 2015;5(1):10560. doi:10.1038/srep10560
51. Huang F, You M, Chen T, et al. Self-assembled hybrid nanoparticles for targeted co-delivery of two drugs into cancer cells. Chem Commun (Camb). 2014;50(23):3103–3105. doi:10.1039/c3cc49003c
52. Shin WS, Han J, Verwilst P, et al. Cancer Targeted Enzymatic Theranostic Prodrug: precise Diagnosis and Chemotherapy. Bioconjug Chem. 2016;27(5):1419–1426. doi:10.1021/acs.bioconjchem.6b00184
53. Dinkova-Kostova AT, Talalay P. NAD(P)H:quinone acceptor oxidoreductase 1 (NQO1), a multifunctional antioxidant enzyme and exceptionally versatile cytoprotector. Arch Biochem Biophys. 2010;501(1):116–123. doi:10.1016/j.abb.2010.03.019
54. Shi H, Gao T, Shi L, et al. Molecular imaging of telomerase and the enzyme activity-triggered drug release by using a conformation-switchable nanoprobe in cancerous cells. Sci Rep. 2018;8(1):16341. doi:10.1038/s41598-018-34670-7
55. Bavelaar BM, Song L, Jackson MR, et al. Oligonucleotide-Functionalized Gold Nanoparticles for Synchronous Telomerase Inhibition, Radiosensitization, and Delivery of Theranostic Radionuclides. Mol Pharm. 2021;18(10):3820–3831. doi:10.1021/acs.molpharmaceut.1c00442
56. Han H, Valdepérez D, Jin Q, et al. Dual enzymatic reaction-assisted gemcitabine delivery systems for programmed pancreatic cancer therapy. ACS Nano. 2017;11(2):1281–1291. doi:10.1021/acsnano.6b05541
57. Radhakrishnan K, Tripathy J, Gnanadhas DP, et al. Dual enzyme responsive and targeted nanocapsules for intracellular delivery of anticancer agents. RSC Adv. 2014;4(86):45961–45968. doi:10.1039/C4RA07815B
58. Yang Y, Lu Y, Abbaraju PL, et al. Stepwise Degradable Nanocarriers Enabled Cascade Delivery for Synergistic Cancer Therapy. Adv Funct Mater. 2018;28(28):1800706. doi:10.1002/adfm.201800706
59. Chiu YR, Ho WJ, Chao JS, et al. Enzyme-encapsulated silica nanoparticle for cancer chemotherapy. J Nanopart Res. 2012;14(4):1–10. doi:10.1007/s11051-012-0829-1
60. Zhang Q, Wang N, Ma M, et al. Transferrin Receptor-Mediated Sequential Intercellular Nanoparticles Relay for Tumor Deep Penetration and Sonodynamic Therapy. Adv Therapeutics. 2019;2(6):1800152. doi:10.1002/adtp.201800152
61. Nag M, Gajbhiye V, Kesharwani P, et al. Transferrin functionalized chitosan-PEG nanoparticles for targeted delivery of paclitaxel to cancer cells. Colloids Surf B Biointerfaces. 2016;148:363–370. doi:10.1016/j.colsurfb.2016.08.059
62. Roncato F, Rruga F, Porcù E, et al. Improvement and extension of anti-EGFR targeting in breast cancer therapy by integration with the Avidin-Nucleic-Acid-Nano-Assemblies. Nat Commun. 2018;9(1):4070. doi:10.1038/s41467-018-06602-6
63. Zhou Z, Jafari M, Sriram V, et al. Delayed sequential co-delivery of gefitinib and doxorubicin for targeted combination chemotherapy. Mol Pharm. 2017;14(12):4551–4559. doi:10.1021/acs.molpharmaceut.7b00669
64. Xu W, Siddiqui IA, Nihal M, et al. Aptamer-conjugated and doxorubicin-loaded unimolecular micelles for targeted therapy of prostate cancer. Biomaterials. 2013;34(21):5244–5253. doi:10.1016/j.biomaterials.2013.03.006
65. Mangadlao JD, Wang X, McCleese C, et al. Prostate-specific membrane antigen targeted gold nanoparticles for theranostics of prostate cancer. ACS Nano. 2018;12(4):3714–3725. doi:10.1021/acsnano.8b00940
66. Singh G, Kumar M, Soni U, et al. Cancer Cell Targeting Using Folic Acid/Anti-HER2 Antibody Conjugated Fluorescent CdSe/CdS/ZnS-Mercaptopropionic Acid and CdTe-Mercaptosuccinic Acid Quantum Dots. J Nanosci Nanotechnol. 2016;16(1):130–143. doi:10.1166/jnn.2016.10825
67. Yoo HS, Park TG. Folate receptor targeted biodegradable polymeric doxorubicin micelles. J Control Release. 2004;96(2):273–283. doi:10.1016/j.jconrel.2004.02.003
68. Banu H, Sethi DK, Edgar A, et al. Doxorubicin loaded polymeric gold nanoparticles targeted to human folate receptor upon laser photothermal therapy potentiates chemotherapy in breast cancer cell lines. J Photochem Photobiol B. 2015;149:116–128. doi:10.1016/j.jphotobiol.2015.05.008
69. Singh MK, Pindiprolu SK, Sanapalli BK, et al. HER2 targeted biological macromolecule modified liposomes for improved efficacy of capecitabine in breast cancer. Int J Biol Macromol. 2020;150:631–636. doi:10.1016/j.ijbiomac.2020.02.131
70. Ghassami E, Varshosaz J, Jahanian-Najafabadi A, et al. Pharmacokinetics and in vitro/in vivo antitumor efficacy of aptamer-targeted Ecoflex(®) nanoparticles for docetaxel delivery in ovarian cancer. Int J Nanomedicine. 2018;13:493–504.
71. Mamnoon B, Feng L, Froberg J, et al. Hypoxia-responsive, polymeric nanocarriers for targeted drug delivery to estrogen receptor-positive breast cancer cell spheroids. Mol Pharm. 2020;17(11):4312–4322. doi:10.1021/acs.molpharmaceut.0c00754
72. Li J, Li M, Tian L, et al. Facile strategy by hyaluronic acid functional carbon dot-doxorubicin nanoparticles for CD44 targeted drug delivery and enhanced breast cancer therapy. Int J Pharm. 2020;578:119122. doi:10.1016/j.ijpharm.2020.119122
73. Shi H, Sun W, Liu C, et al. Tumor-targeting, enzyme-activated nanoparticles for simultaneous cancer diagnosis and photodynamic therapy. J Materials ChemB. 2016;4(1):113–120. doi:10.1039/C5TB02041G
74. Yadav AS, Radharani NNV, Gorain M, et al. RGD functionalized chitosan nanoparticle mediated targeted delivery of raloxifene selectively suppresses angiogenesis and tumor growth in breast cancer. Nanoscale. 2020;12(19):10664–10684. doi:10.1039/C9NR10673A
75. Kobatake E, Ikeda Y, Mie M. Construction of protein nanoparticles for targeted delivery of drugs to cancer cells. Materials Adv. 2022;3(15):6262–6269. doi:10.1039/D2MA00419D
76. Taheri A, Dinarvand R, Nouri FS, et al. Use of biotin targeted methotrexate-human serum albumin conjugated nanoparticles to enhance methotrexate antitumor efficacy. Int J Nanomedicine. 2011;6:1863–1874.
77. Li M, Tang Z, Zhang Y, et al. LHRH-peptide conjugated dextran nanoparticles for targeted delivery of cisplatin to breast cancer. J Mater Chem B. 2014;2(22):3490–3499. doi:10.1039/c4tb00077c
78. Yao Y, Zhou Y, Liu L, et al. Nanoparticle-based drug delivery in cancer therapy and its role in overcoming drug resistance. Front Mol Biosci. 2020;7. doi:10.3389/fmolb.2020.00193
79. Seymour LW, Ferry DR, Anderson D, et al. Hepatic drug targeting: Phase I evaluation of polymer-bound doxorubicin. J Clin Oncol. 2002;20(6):1668–1676. doi:10.1200/JCO.2002.20.6.1668
80. Yang Y, Wan J, Niu Y, et al. Structure-dependent and glutathione-responsive biodegradable dendritic mesoporous organosilica nanoparticles for safe protein delivery. Chem Materials. 2016;28(24):9008–9016. doi:10.1021/acs.chemmater.6b03896
81. Iyer R, Nguyen T, Padanilam D, et al. Glutathione-responsive biodegradable polyurethane nanoparticles for lung cancer treatment. J Control Release. 2020;321:363–371. doi:10.1016/j.jconrel.2020.02.021
82. Cui T, Li X, Shu Y, et al. Utilizing glutathione-triggered nanoparticles to enhance chemotherapy of lung cancer by reprogramming the tumor microenvironment. Int J Pharm. 2018;552(1):16–26. doi:10.1016/j.ijpharm.2018.09.050
83. Jung M, Mertens C, Tomat E, et al. Iron as a central player and promising target in cancer progression. Int J Mol Sci. 2019;20(2):656.
84. Candelaria PV, Leoh LS, Penichet ML, et al. Antibodies Targeting the Transferrin Receptor 1 (TfR1) as Direct Anti-cancer Agents. Front Immunol. 2021;12. doi:10.3389/fimmu.2021.607692
85. Clark AJ, Davis ME. Increased brain uptake of targeted nanoparticles by adding an acid-cleavable linkage between transferrin and the nanoparticle core. Proc Natl Acad Sci U S A. 2015;112(40):12486–12491. doi:10.1073/pnas.1517048112
86. Ulbrich K, Hekmatara T, Herbert E, et al. Transferrin- and transferrin-receptor-antibody-modified nanoparticles enable drug delivery across the blood-brain barrier (BBB). Eur J Pharm Biopharm. 2009;71(2):251–256. doi:10.1016/j.ejpb.2008.08.021
87. Wosikowski K, Schuurhuis D, Kops GJ, et al. Altered gene expression in drug-resistant human breast cancer cells. Clin Cancer Res. 1997;3(12 Pt 1):2405–2414.
88. Akimoto T, Hunter NR, Buchmiller L, et al. Inverse relationship between epidermal growth factor receptor expression and radiocurability of murine carcinomas. Clin Cancer Res. 1999;5(10):2884–2890.
89. Galizia G, Lieto E, Ferraraccio F, et al. Prognostic significance of epidermal growth factor receptor expression in colon cancer patients undergoing curative surgery. Ann Surg Oncol. 2006;13(6):823–835. doi:10.1245/ASO.2006.05.052
90. Fu Z, Li S, Han S, et al. Antibody drug conjugate: the “biological missile” for targeted cancer therapy. Signal Transduction Targeted Therapy. 2022;7(1):93. doi:10.1038/s41392-022-00947-7
91. Nejadmoghaddam M-R, Minai-Tehrani A, Ghahremanzadeh R, et al. Antibody-drug conjugates: possibilities and challenges. Avicenna J Med Biotechnol. 2019;11(1):3–23.
92. Mhawech-Fauceglia P, Zhang S, Terracciano L, et al. Prostate-specific membrane antigen (PSMA) protein expression in normal and neoplastic tissues and its sensitivity and specificity in prostate adenocarcinoma: an immunohistochemical study using multiple tumour tissue microarray technique. Histopathology. 2007;50(4):472–483. doi:10.1111/j.1365-2559.2007.02635.x
93. Rauscher I, Maurer T, Fendler WP, et al. (68)Ga-PSMA ligand PET/CT in patients with prostate cancer: how we review and report. Cancer Imaging. 2016;16(1):14. doi:10.1186/s40644-016-0072-6
94. Liu H, Rajasekaran AK, Moy P, et al. Constitutive and antibody-induced internalization of prostate-specific membrane antigen. Cancer Res. 1998;58(18):4055–4060.
95. Muralidharan R, Babu A, Amreddy N, et al. Folate receptor-targeted nanoparticle delivery of HuR-RNAi suppresses lung cancer cell proliferation and migration. J Nanobiotechnology. 2016;14(1):47. doi:10.1186/s12951-016-0201-1
96. Tokunaga E, Kimura Y, Oki E, et al. Akt is frequently activated in HER2/neu-positive breast cancers and associated with poor prognosis among hormone-treated patients. Int J Cancer. 2006;118(2):284–289. doi:10.1002/ijc.21358
97. Iqbal N, Iqbal N. Human Epidermal Growth Factor Receptor 2 (HER2) in Cancers: overexpression and Therapeutic Implications. Mol Biol Int. 2014;2014:852748. doi:10.1155/2014/852748
98. Borrow AP, Handa RJ. Estrogen Receptors Modulation of Anxiety-Like Behavior. Vitam Horm. 2017;103:27–52.
99. Cui J, Shen Y, Li R. Estrogen synthesis and signaling pathways during aging: from periphery to brain. Trends Mol Med. 2013;19(3):197–209. doi:10.1016/j.molmed.2012.12.007
100. Huang B, Omoto Y, Iwase H, et al. Differential expression of estrogen receptor α, β1, and β2 in lobular and ductal breast cancer. Proc Natl Acad Sci U S A. 2014;111(5):1933–1938. doi:10.1073/pnas.1323719111
101. Eyster KM. The estrogen receptors: an overview from different perspectives. Methods Mol Biol. 2016;1366:1–10.
102. Sneath RJ, Mangham DC. The normal structure and function of CD44 and its role in neoplasia. Mol Pathol. 1998;51(4):191–200. doi:10.1136/mp.51.4.191
103. Jordan AR, Racine RR, Hennig MJP, et al. The Role of CD44 in Disease Pathophysiology and Targeted Treatment. Front Immunol. 2015;6. doi:10.3389/fimmu.2015.00182
104. Orian-Rousseau V. CD44, a therapeutic target for metastasising tumours. Eur J Cancer. 2010;46(7):1271–1277. doi:10.1016/j.ejca.2010.02.024
105. Wang Z, Shi Q, Wang Z, et al. Clinicopathologic correlation of cancer stem cell markers CD44, CD24, VEGF and HIF-1α in ductal carcinoma in situ and invasive ductal carcinoma of breast: an immunohistochemistry-based pilot study. Pathol Res Pract. 2011;207(8):505–513. doi:10.1016/j.prp.2011.06.009
106. Pavalko FM, Otey CA. Role of adhesion molecule cytoplasmic domains in mediating interactions with the cytoskeleton. Proc Soc Exp Biol Med. 1994;205(4):282–293. doi:10.3181/00379727-205-43709
107. Haass NK, Smalley KSM, Li L, et al. Adhesion, migration and communication in melanocytes and melanoma. Pigment Cell Res. 2005;18(3):150–159. doi:10.1111/j.1600-0749.2005.00235.x
108. Chen K, Chen X. Integrin targeted delivery of chemotherapeutics. Theranostics. 2011;1:189–200. doi:10.7150/thno/v01p0189
109. Brooks PC, Strömblad S, Sanders LC, et al. Localization of matrix metalloproteinase MMP-2 to the surface of invasive cells by interaction with integrin alpha v beta 3. Cell. 1996;85(5):683–693. doi:10.1016/S0092-8674(00)81235-0
110. Ghanghoria R, Kesharwani P, Tekade RK, et al. Targeting luteinizing hormone-releasing hormone: a potential therapeutics to treat gynecological and other cancers. J Control Release. 2018;269:277–301. doi:10.1016/j.jconrel.2016.11.002
111. Zhu S, Wang Q, Jiang J, et al. A conjugate of methotrexate and an analog of luteinizing hormone releasing hormone shows increased efficacy against prostate cancer. Sci Rep. 2016;6(1):33894. doi:10.1038/srep33894
112. Minko T. Drug targeting to the colon with lectins and neoglycoconjugates. Adv Drug Deliv Rev. 2004;56(4):491–509. doi:10.1016/j.addr.2003.10.017
113. Mura S, Nicolas J, Couvreur P. Stimuli-responsive nanocarriers for drug delivery. Nat Mater. 2013;12(11):991–1003.
114. Argenziano M, Lombardi C, Ferrara B, et al. Glutathione/pH-responsive nanosponges enhance strigolactone delivery to prostate cancer cells. Oncotarget. 2018;9(88):35813–35829. doi:10.18632/oncotarget.26287
115. Chiang YT, Yen YW, Lo CL. Reactive oxygen species and glutathione dual redox-responsive micelles for selective cytotoxicity of cancer. Biomaterials. 2015;61:150–161. doi:10.1016/j.biomaterials.2015.05.007
116. Entzian K, Aigner A. Drug Delivery by Ultrasound-Responsive Nanocarriers for Cancer Treatment. Pharmaceutics. 2021;13(8):1135. doi:10.3390/pharmaceutics13081135
117. Qin J, Wang TY, Willmann JK. Sonoporation: applications for cancer therapy. Adv Exp Med Biol. 2016;880:263–291.
118. Jangjou A, Meisami AH, Jamali K, et al. The promising shadow of microbubble over medical sciences: from fighting wide scope of prevalence disease to cancer eradication. J Biomed Sci. 2021;28(1):49. doi:10.1186/s12929-021-00744-4
119. Mullin LB, Phillips LC, Dayton PA. Nanoparticle delivery enhancement with acoustically activated microbubbles. IEEE Trans Ultrason Ferroelectr Freq Control. 2013;60(1):65–77. doi:10.1109/TUFFC.2013.2538
120. De Temmerman M-L, Dewitte H, Vandenbroucke RE, et al. mRNA-Lipoplex loaded microbubble contrast agents for ultrasound-assisted transfection of dendritic cells. Biomaterials. 2011;32(34):9128–9135. doi:10.1016/j.biomaterials.2011.08.024
121. Burke CW, Hsiang Y-HJ, Alexander E, et al. Covalently Linking Poly(lactic-co-glycolic acid) Nanoparticles to Microbubbles Before Intravenous Injection Improves their Ultrasound-Targeted Delivery to Skeletal Muscle. Small. 2011;7(9):1227–1235. doi:10.1002/smll.201001934
122. Cochran MC, Eisenbrey J, Ouma RO, et al. Doxorubicin and paclitaxel loaded microbubbles for ultrasound triggered drug delivery. Int J Pharm. 2011;414(1–2):161–170. doi:10.1016/j.ijpharm.2011.05.030
123. De Temmerman ML, Dewitte H, Vandenbroucke RE, et al. mRNA-Lipoplex loaded microbubble contrast agents for ultrasound-assisted transfection of dendritic cells. Biomaterials. 2011;32(34):9128–9135.
124. Kwan JJ, Myers R, Coviello CM, et al. Ultrasound-propelled nanocups for drug delivery. Small. 2015;11(39):5305–5314. doi:10.1002/smll.201501322
125. Marshalek JP, Sheeran PS, Ingram P, et al. Intracellular delivery and ultrasonic activation of folate receptor-targeted phase-change contrast agents in breast cancer cells in vitro. J Control Release. 2016;243:69–77. doi:10.1016/j.jconrel.2016.09.010
126. Yamashita M. Ion channel activities in neural stem cells of the neuroepithelium. Stem Cells Int. 2012;2012:247670. doi:10.1155/2012/247670
127. Cucullo L, Dini G, Hallene KL, et al. Very low intensity alternating current decreases cell proliferation. Glia. 2005;51(1):65–72. doi:10.1002/glia.20188
128. Wang X, Song J, Liu J, et al. Direct-current nanogenerator driven by ultrasonic waves. Science. 2007;316(5821):102–105. doi:10.1126/science.1139366
129. Marino A, Battaglini M, De Pasquale D, et al. Ultrasound-activated piezoelectric nanoparticles inhibit proliferation of breast cancer cells. Sci Rep. 2018;8(1):6257. doi:10.1038/s41598-018-24697-1
130. Sharma K, Chauhan C. Role of Magnetic Nanoparticle (Mnps) in Cancer Treatment: A Review. Materials Today: Proceedings; 2021.
131. Avasthi A, Caro C, Pozo-Torres E, et al. Magnetic Nanoparticles as MRI Contrast Agents. Top Curr Chem. 2020;378(3):40. doi:10.1007/s41061-020-00302-w
132. Price PM, Mahmoud WE, Al-Ghamdi AA, et al. Magnetic drug delivery: where the field is going. Front Chem. 2018;6. doi:10.3389/fchem.2018.00619
133. Shah RR, Davis TP, Glover AL, et al. Impact of magnetic field parameters and iron oxide nanoparticle properties on heat generation for use in magnetic hyperthermia. J Magn Magn Mater. 2015;387:96–106. doi:10.1016/j.jmmm.2015.03.085
134. Johannsen M, Gneveckow U, Eckelt L, et al. Clinical hyperthermia of prostate cancer using magnetic nanoparticles: presentation of a new interstitial technique. Int J Hyperthermia. 2005;21(7):637–647. doi:10.1080/02656730500158360
135. Ungureanu BS, Teodorescu CM, Săftoiu A. Magnetic nanoparticles for hepatocellular carcinoma diagnosis and therapy. J Gastrointestin Liver Dis. 2016;25(3):375–383. doi:10.15403/jgld.2014.1121.253.nan
136. Sohail A, Ahmad Z, Bég OA, et al. A review on hyperthermia via nanoparticle-mediated therapy. Bull Cancer. 2017;104(5):452–461. doi:10.1016/j.bulcan.2017.02.003
137. Bañobre-López M, Teijeiro A, Rivas J. Magnetic nanoparticle-based hyperthermia for cancer treatment. Rep Practical Oncol Radiother. 2013;18(6):397–400. doi:10.1016/j.rpor.2013.09.011
138. Liu JF, Jang B, Issadore D, et al. Use of magnetic fields and nanoparticles to trigger drug release and improve tumor targeting. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2019;11(6):e1571–e1571. doi:10.1002/wnan.1571
139. Yan S, Zhang D, Gu N, et al. Therapeutic Effect of Fe2O3 Nanoparticles Combined with Magnetic Fluid Hyperthermia on Cultured Liver Cancer Cells and Xenograft Liver Cancers. J Nanosci Nanotechnol. 2005;5(8):1185–1192. doi:10.1166/jnn.2005.219
140. Ashikbayeva Z, Tosi D, Balmassov D, et al. Application of nanoparticles and nanomaterials in thermal ablation therapy of cancer. Nanomaterials. 2019;9(9):1195. doi:10.3390/nano9091195
141. Huo M, Wang L, Chen Y, et al. Tumor-selective catalytic nanomedicine by nanocatalyst delivery. Nat Commun. 2017;8(1):357. doi:10.1038/s41467-017-00424-8
142. Kohler N, Sun C, Fichtenholtz A, et al. Methotrexate-immobilized poly(ethylene glycol) magnetic nanoparticles for MR imaging and drug delivery. Small. 2006;2(6):785–792. doi:10.1002/smll.200600009
143. Alexiou C, Arnold W, Klein RJ, et al. Locoregional cancer treatment with magnetic drug targeting. Cancer Res. 2000;60(23):6641–6648.
144. Petri-Fink A, Chastellain M, Juillerat-Jeanneret L, et al. Development of functionalized superparamagnetic iron oxide nanoparticles for interaction with human cancer cells. Biomaterials. 2005;26(15):2685–2694. doi:10.1016/j.biomaterials.2004.07.023
145. Yang C, Rait A, Pirollo KF, et al. Nanoimmunoliposome delivery of superparamagnetic iron oxide markedly enhances targeting and uptake in human cancer cells in vitro and in vivo. Nanomedicine. 2008;4(4):318–329. doi:10.1016/j.nano.2008.05.004
146. Katagiri K, Imai Y, Koumoto K, et al. Magnetoresponsive On-Demand Release of Hybrid Liposomes Formed from Fe3O4 Nanoparticles and Thermosensitive Block Copolymers. Small. 2011;7(12):1683–1689. doi:10.1002/smll.201002180
147. Hu S-H, Chen S-Y, Gao X. Multifunctional nanocapsules for simultaneous encapsulation of hydrophilic and hydrophobic compounds and on-demand release. ACS Nano. 2012;6(3):2558–2565. doi:10.1021/nn205023w
148. Pradhan P, Giri J, Rieken F, et al. Targeted temperature sensitive magnetic liposomes for thermo-chemotherapy. J Controlled Release. 2010;142(1):108–121. doi:10.1016/j.jconrel.2009.10.002
149. Plassat V, Wilhelm C, Marsaud V, et al. Anti-Estrogen-Loaded Superparamagnetic Liposomes for Intracellular Magnetic Targeting and Treatment of Breast Cancer Tumors. Adv Funct Mater. 2011;21(1):83–92. doi:10.1002/adfm.201001450
150. Cai K, Luo Z, Hu Y, et al. Magnetically triggered reversible controlled drug delivery from microfabricated polymeric multireservoir devices. Adv Mater. 2009;21(40):4045–4049. doi:10.1002/adma.200900593
151. Park JW, Bae KH, Kim C, et al. Clustered Magnetite Nanocrystals Cross-Linked with PEI for Efficient siRNA Delivery. Biomacromolecules. 2011;12(2):457–465. doi:10.1021/bm101244j
152. Uthaman S, Muthiah M, Park IK, et al. In Narain R, Editor. 9 - Fabrication and Development of Magnetic Particles for Gene Therapy, in Polymers and Nanomaterials for Gene Therapy. Woodhead Publishing; 2016:215–230.
153. Hu A, Chen X, Bi Q, et al. A parallel and cascade control system: magnetofection of miR125b for synergistic tumor-association macrophage polarization regulation and tumor cell suppression in breast cancer treatment. Nanoscale. 2020;12(44):22615–22627. doi:10.1039/D0NR06060G
154. Pan Z, Shi Z, Wei H, et al. Magnetofection Based on Superparamagnetic Iron Oxide Nanoparticles Weakens Glioma Stem Cell Proliferation and Invasion by Mediating High Expression of MicroRNA-374a. J Cancer. 2016;7(11):1487–1496. doi:10.7150/jca.15515
155. Govindarajan S, Kitaura K, Takafuji M, et al. Gene delivery into human cancer cells by cationic lipid-mediated magnetofection. Int J Pharm. 2013;446(1):87–99. doi:10.1016/j.ijpharm.2013.01.055
156. Agostinis P, Berg K, Cengel KA, et al. Photodynamic therapy of cancer: an update. CA Cancer J Clin. 2011;61(4):250–281. doi:10.3322/caac.20114
157. Allison RR, Sibata CH. Oncologic photodynamic therapy photosensitizers: a clinical review. Photodiagnosis Photodyn Ther. 2010;7(2):61–75. doi:10.1016/j.pdpdt.2010.02.001
158. Ibrahim S. The Electromagnetic Spectrum. Phys Rev. 2007;97:689.
159. Wang M, Abbineni G, Clevenger A, et al. Upconversion nanoparticles: synthesis, surface modification and biological applications. Nanomedicine: nanotechnology. Biol Med. 2011;7(6):710–729.
160. Wang C, Cheng L, Liu Z. Upconversion nanoparticles for photodynamic therapy and other cancer therapeutics. Theranostics. 2013;3(5):317–330. doi:10.7150/thno.5284
161. Osuchowski M, Osuchowski F, Latos W, et al. The Use of Upconversion Nanoparticles in Prostate Cancer Photodynamic Therapy. Life. 2021;11(4):360. doi:10.3390/life11040360
162. Lucky SS, Muhammad Idris N, Li Z, et al. Titania Coated Upconversion Nanoparticles for Near-Infrared Light Triggered Photodynamic Therapy. ACS Nano. 2015;9(1):191–205. doi:10.1021/nn503450t
163. Meng Q, Meng J, Ran W, et al. Light-Activated Core–Shell Nanoparticles for Spatiotemporally Specific Treatment of Metastatic Triple-Negative Breast Cancer. ACS Nano. 2018;12(3):2789–2802. doi:10.1021/acsnano.7b09210
164. Yue C, Yang Y, Zhang C, et al. ROS-responsive mitochondria-targeting blended nanoparticles: chemo- and photodynamic synergistic therapy for lung cancer with on-demand drug release upon irradiation with a single light source. Theranostics. 2016;6(13):2352–2366. doi:10.7150/thno.15433
165. Chen H, Wang GD, Chuang Y-J, et al. Nanoscintillator-Mediated X-ray Inducible Photodynamic Therapy for In Vivo Cancer Treatment. Nano Lett. 2015;15(4):2249–2256. doi:10.1021/nl504044p
166. Güleryüz B, Ünal U, Gülsoy M. Near infrared light activated upconversion nanoparticles (UCNP) based photodynamic therapy of prostate cancers: an in vitro study. Photodiagnosis Photodyn Ther. 2021;36:102616. doi:10.1016/j.pdpdt.2021.102616
167. Juarranz Á, Jaén P, Sanz-Rodríguez F, et al. Photodynamic therapy of cancer. Basic principles and applications. Clin Transl Oncol. 2008;10(3):148–154. doi:10.1007/s12094-008-0172-2
168. Gunaydin G, Gedik ME, Ayan S. Photodynamic Therapy—Current Limitations and Novel Approaches. Front Chem. 2021;9:656.
169. Liu T, Yang K, Liu Z. Recent advances in functional nanomaterials for X-ray triggered cancer therapy. Progress Nat Sci. 2020;30(5):567–576. doi:10.1016/j.pnsc.2020.09.009
170. Vankayala R, Kuo C-L, Nuthalapati K, et al. Nucleus-Targeting Gold Nanoclusters for Simultaneous In Vivo Fluorescence Imaging, Gene Delivery, and NIR-Light Activated Photodynamic Therapy. Adv Funct Mater. 2015;25(37):5934–5945. doi:10.1002/adfm.201502650
171. Hu T, Wang Z, Shen W, et al. Recent advances in innovative strategies for enhanced cancer photodynamic therapy. Theranostics. 2021;11(7):3278–3300. doi:10.7150/thno.54227
172. Qiu M, Wang D, Liang W, et al. Novel concept of the smart NIR-light–controlled drug release of black phosphorus nanostructure for cancer therapy. Proce Nat Acad Sci. 2018;115(3):501–506. doi:10.1073/pnas.1714421115
173. Yuan P, Song D. MRI tracing non-invasive TiO2-based nanoparticles activated by ultrasound for multi-mechanism therapy of prostatic cancer. Nanotechnology. 2018;29(12):125101. doi:10.1088/1361-6528/aaa92a
174. Lee J, Min H-S, You DG, et al. Theranostic gas-generating nanoparticles for targeted ultrasound imaging and treatment of neuroblastoma. J Controlled Release. 2016;223:197–206. doi:10.1016/j.jconrel.2015.12.051
175. Yuan P, Song D. MRI tracing non-invasive TiO2-based nanoparticles activated by ultrasound for multi-mechanism therapy of prostatic cancer. Nanotechnology. 2018;29(12):125101.
176. Kim D, Lee SS, Yoo WY, et al. Combination Therapy with Doxorubicin-Loaded Reduced Albumin Nanoparticles and Focused Ultrasound in Mouse Breast Cancer Xenografts. Pharmaceuticals. 2020;13(9):235. doi:10.3390/ph13090235
177. Yang G, Xu L, Xu J, et al. Smart Nanoreactors for pH-Responsive Tumor Homing, Mitochondria-Targeting, and Enhanced Photodynamic-Immunotherapy of Cancer. Nano Lett. 2018;18(4):2475–2484. doi:10.1021/acs.nanolett.8b00040
178. Weng -C-C, Yang T-A, Li Y-K. Design and fabrication of cell-targeted, dual drug-loaded nanoparticles with pH-controlled drug release and near-infrared light-induced photothermal effects. Mater Des. 2021;197:109230. doi:10.1016/j.matdes.2020.109230
179. Ihsanullah KM, Kumar BN, Zhao Y, et al. Stepwise-activatable hypoxia triggered nanocarrier-based photodynamic therapy for effective synergistic bioreductive chemotherapy. Biomaterials. 2020;245:119982. doi:10.1016/j.biomaterials.2020.119982
180. Zhao Z, Huang D, Yin Z, et al. Magnetite nanoparticles as smart carriers to manipulate the cytotoxicity of anticancer drugs: magnetic control and pH-responsive release. J Mater Chem. 2012;22(31):15717–15725. doi:10.1039/c2jm31692g
181. Venkatesan M, Jolad B. Nanorobots in Cancer Treatment. Interact. 2011;258–264.
182. Kishore C, Bhadra P. Targeting brain cancer cells by nanorobot, a promising nanovehicle: new challenges and future perspectives. CNS Neurol Disord Drug Targets. 2021;20(6):531–539. doi:10.2174/1871527320666210526154801
183. Andhari SS, Wavhale RD, Dhobale KD, et al. Self-propelling targeted magneto-nanobots for deep tumor penetration and ph-responsive intracellular drug delivery. Sci Rep. 2020;10(1):4703. doi:10.1038/s41598-020-61586-y
184. Burke CW, Alexander E, Timbie K, et al. Ultrasound-activated agents comprised of 5FU-bearing nanoparticles bonded to microbubbles inhibit solid tumor growth and improve survival. Mol Therapy. 2014;22(2):321–328. doi:10.1038/mt.2013.259
185. Mullin LB, Phillips LC, Dayton PA. Nanoparticle delivery enhancement with acoustically activated microbubbles. IEEE Trans Ultrason Ferroelectr Freq Control. 2012;60(1):65–77.
186. Stolik S, Delgado JA, Pérez A, et al. Measurement of the penetration depths of red and near infrared light in human “ex vivo” tissues. J Photochem Photobiol B. 2000;57(2–3):90–93. doi:10.1016/S1011-1344(00)00082-8
187. Wu M, Huang S. Magnetic nanoparticles in cancer diagnosis, drug delivery and treatment. Mol Clin Oncol. 2017;7(5):738–746. doi:10.3892/mco.2017.1399
188. Burke CW, Alexander E, Timbie K, et al. Ultrasound-activated Agents Comprised of 5FU-bearing Nanoparticles Bonded to Microbubbles Inhibit Solid Tumor Growth and Improve Survival. Mol Therapy. 2014;22(2):321–328.
189. Dietrich CF, Mathis G, Cui X-W, et al. Ultrasound of the Pleurae and Lungs. Ultrasound Med Biol. 2015;41(2):351–365. doi:10.1016/j.ultrasmedbio.2014.10.002
190. Stolik S, Delgado JA, Pérez A, et al. Measurement of the penetration depths of red and near infrared light in human “ex vivo” tissues. J Photochem Photobiol B. 2000;57(2):90–93.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.








