Back to Journals » International Journal of General Medicine » Volume 9
Incidence of clinical symptoms during long-duration orbital spaceflight
Authors Crucian B, Babiak-Vazquez A, Johnston S, Pierson DL, Ott CM, Sams C
Received 3 June 2016
Accepted for publication 10 September 2016
Published 3 November 2016 Volume 2016:9 Pages 383—391
DOI https://doi.org/10.2147/IJGM.S114188
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Brian Crucian,1 Adriana Babiak-Vazquez,2 Smith Johnston,1 Duane L Pierson,1 C Mark Ott,1 Clarence Sams1
1Biomedical Research and Environmental Sciences Division, NASA-Johnson Space Center, 2Epidemiology/Lifetime Surveillance of Astronaut Health, KBR-Wyle, Houston, TX, USA
Background: The environment of spaceflight may elevate an astronaut’s clinical risk for specific diseases. The purpose of this study was to derive, as accurately as currently possible, an assessment of in-flight clinical “incidence” data, based on observed clinical symptoms in astronauts on board the International Space Station (ISS).
Methods: Electronic medical records were examined from 46 long-duration ISS crew members, each serving approximately a 6-month mission on board the ISS, constituting 20.57 total flight years. Incidence for immunological-related adverse health events or relevant clinical symptoms was tabulated in a non-identifiable fashion. Event categories included infectious diseases, allergies, and rashes/hypersensitivities. A subsequent re-evaluation of more notable events, either of prolonged duration or unresponsive to treatment, was performed.
Results: For the disease/symptom categories used in this evaluation, the ISS incidence rate was 3.40 events per flight year. Skin rashes were the most reported event (1.12/flight year) followed by upper respiratory symptoms (0.97/flight year) and various other (non-respiratory) infectious processes. During flight, 46% of crew members reported an event deemed “notable”. Among the notable events, 40% were classified as rashes/hypersensitivities. Characterization of on-orbit rashes manifested as redness with irritation, and could present on a variety of body locations.
Conclusion: Based on reported symptoms, astronauts experience adverse medical events of varying severity during long-duration spaceflights. The data suggests caution, from both a vehicle design and biomedical countermeasures perspective, as space agencies plan for prolonged deep space exploration missions.
Keywords: spaceflight, immunity, clinical incidence, astronauts, gravity, clinical risk, disease
Background
A vast evidence base demonstrates that dysregulation of the human immune system occurs immediately following spaceflight.1,2 Specific post-flight findings include: altered cytokine production patterns;3–7 diminished natural killer (NK) cell function;8 altered peripheral leukocyte distribution;9,10 diminished monocyte function;11 diminished granulocyte function;10,12 dysregulated T-cell intracellular signaling;13–15 altered neuroendocrine responses;16,17 and inhibited leukocyte proliferation following activation.18,19 Latent herpesviruses have been found to be reactivated in crew members during or following spaceflight.20–22 Humoral immunity may also be affected by spaceflight, as animal studies have indicated that the somatic hypermutation process responsible for diversification of antibody binding sites was reduced during spaceflight.23 Recent data collected on board the Space Shuttle and International Space Station (ISS) confirms that human immune dysregulation is indeed an in-flight phenomenon, and not merely a post-flight stress response to landing and readaptation following deconditioning.24,25
Immune dysfunction seems to coincide with, and is likely the mechanistic cause for, the documented reactivation of various latent herpesviruses during short-duration flight.20,21,26 Additional studies currently ongoing on board the ISS will ascertain if other uninvestigated aspects of immune dysregulation persist for the duration of a 6-month orbital spaceflight. Likely causes include physiological and psychological stressors, microgravity, and radiation. The effect of physiological stress on immunity is well established.27 Stress hormone levels have been found to be elevated following flight, heavily dependent on mission duration.17,28 Furthermore, “other” endogenous stress response systems, such as the endocannabinoid system in humans, have also been found to be dysregulated during spaceflight.29 Persistent in-flight immune dysregulation could result in specific clinical risks to crew members participating in exploration class deep space missions.30
Clinical events potentially related to immune system dysregulation may include a variety of bacterial or viral infections (skin, upper respiratory, urinary tract, etc.), clinical viral reactivation, documented hypersensitivities, or increased incidence of allergies. During prolonged missions (Mars, asteroids, etc.), more prolonged-development diseases such as autoimmunity or malignancies may become possible. During exploration missions, the risk for malignancies may be directly related to immune dysregulation (diminished NK cell function) synergizing with radiation exposure. Basic understanding of the incidence of clinical symptoms during orbital spaceflight is important for anticipation of potential clinical risks during exploration class deep space missions. This is especially true, considering the persistent immune dysregulation during spaceflight.
Immune dysregulation during orbital flight, documented by research data as described above, may be perceived to only result in subclinical changes. Crews are generally not thought, with some well-publicized exceptions, to suffer significant illness during flight. This is primarily due to the confidential nature of astronaut medical data. Whereas research findings may in a non-identifiable fashion be published, adverse medical events are known only to the crew member and his/her flight surgeon. But at what rate do astronauts actually experience illness on-orbit? Although it should be possible to examine National Aeronautics and Space Administration (NASA) medical records and report incidence in an anonymous fashion, literature evidence detailing in-flight clinical incidence is lacking. Also, there are already existing countermeasures designed to limit crew illness during flight. These include a pre-flight quarantine period, defined as the “Health Stabilization Program” (HSP). This program was implemented after an in-flight infectious disease event occurred during an Apollo moon mission. Other in-place mitigation strategies include microbial monitoring of food, water, vehicles, and cargo.
Reports of adverse clinical events on board the ISS may appear in a variety of records or information sources. The primary source would normally be the crew electronic medical record (EMR), in which the flight surgeon may document on-orbit illness of his/her particular crew member. However, notations of on-orbit illness may also be recorded in secondary sources of information, within both medical operations and biomedical research. The goal of our activity was to tabulate incidence of adverse clinical events during ISS missions via reported symptoms by surveying the EMR and the secondary information sources. In most cases, a confirmatory diagnosis is simply not possible, given the paucity of medical laboratory equipment on board the ISS. A limitation of this activity is that it is not a standard epidemiological survey, but rather represents a simple tabulation of all available recorded occurrence of symptoms during flight. For some crew members, not all the various information sources were populated with information. As it is logical to assume that at least some events may not be recorded, based on the purview of the crew member and/or flight surgeon, the information reported here therefore may represent a baseline minimum compilation of known in-flight clinical incidence.
The aim of this activity was to retrospectively analyze existing astronaut medical records, to derive the most accurate assessment of in-flight clinical incidence technically possible within existing operational constraints. However, to perform the survey, it was necessary to replace the actual confirmed incidence with reported symptomatology, as in-flight crews rarely have the ability to confirm diagnoses, and treatment is usually based on presentation of symptoms.
Methods
Subjects
Per current NASA policy, an attributability review of the information provided via this article was conducted by the Epidemiology Division/Lifetime Surveillance of Astronaut Health at the Johnson Space Center, and approval to publish was granted. Further, per NASA policy, research based on extant de-identified data is exempt from institutional review board (IRB) review. However, the current Chair of the NASA IRB has reviewed and approved release of the data contained within this manuscript. The NASA IRB did not require written informed consent be obtained from the participants, as this was a retrospective surveillance activity, and all data was de-identified.
For this study, we examined medical records from 46 long-duration US astronaut missions on board the ISS. Of the 46 US crew members completing ISS missions as of the date of this manuscript, all were included in this study. No symptoms or immunological events were reported by 8 crew members. During the analysis period, 5 astronauts actually repeated long-duration space missions on board the ISS, for which each long-duration mission was counted as a separate “flight/mission”. Therefore, the records from 46 long-duration ISS crew members were examined, which actually consisted of 41 flown US astronauts. Among the 46 US astronauts, there were 34 male and 12 female astronauts, with an average age of 47.51 years at time of flight. The average mission duration was 162.95 days; the sum total for the 46 crew members (representing 38 missions) was 7058 flight days or 20.57 flight years.
Primary review of EMRs
For this report, an effort was made to review and categorize in-flight incidence, and tabulate those findings in a non-attributable fashion. The primary data review, consisting of ISS EMRs, was performed using the evaluation categories as described below. The ISS data set consists of 46 flown space station crew members (repeat flyers were counted as separate crew member missions), resulting in a total of 20.57 crew flight years. Data regarding the incidence of clinical symptoms was obtained by reviewing the records of crew private medical conferences. Reported symptoms were evaluated for correlation to the listed adverse event categories. Finally, the mission date of each event was included in the crew records. A breakdown of all reported events was derived by mission month for the 6-month orbital spaceflights.
Adverse event categorization
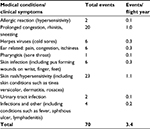
The NASA integrated medical model (IMM) is an operational NASA tool that helps to align science, technology, and operational activities. The IMM is intended for use in optimizing crew health and safety and to ensure mission success by quantifying the probability and consequences of medical risks.31 The IMM has identified 83 medical conditions that have occurred, or have the potential to occur, in-flight. From this list, we identified 13 IMM conditions that could be associated with dysregulated immunity during spaceflight. For purposes of this review, otitis media and otitis externa were combined into a single analysis category of ear-related symptoms: pain, congestion, and itchiness. Additionally, the condition of upper respiratory infections was removed and the related symptoms, prolonged congestion, rhinitis, and sneezing were added instead. The IMM category identified as “skin rashes” was interpreted to also apply to hypersensitivities. Two other conditions not contained within the IMM, malignancy and autoimmunity, were also evaluated during this activity. Finally, one additional category identified as “Infections, other” was created to account for those infectious disease conditions that occurred during spaceflight but were not associated with any specific IMM condition (Table 1). Some overlap between categories is possible depending on the specific clinical symptoms. Skin rash and hypersensitivities were categorized, yet in some cases where rash was accompanied by symptoms of infection, it was classified under skin infection instead. For all such instances, the epidemiologist and immunologist evaluators worked to select the most appropriate category based on the event clinical symptoms reported. Observable symptom events thought NOT to be related to immune dysregulation, such as brief episodes of loose stools, or injury-related events, were not included in this evaluation.
Causality and potential consequence is not always reported. An attempt was made to particularly tabulate events that have the potential to relate to immune dysregulation. There could be multiple events for individual crew members. Events were not double scored into multiple categories. Where possible, if an event was reported as a recurrence of a previously noted event, we did not count twice. In addition to the 70 events reported and included in this tabulation, an additional 28 events were excluded, as they were deemed to not be associated with dysregulated immunity. Such events included intestinal complaints due to food or nutrition, abrasions, eye irritations and/or tearing. Events such as congestion, nausea, diarrhea, or constipation, which were reported and resolved within the first 30 days of flight, were excluded and classified as space adaptation symptoms.
Secondary tabulation of incidence data from additional sources
Since additional sources of information exist regarding medical events on board the ISS, and due to operational constraints no single source would be complete for an individual crew member, we reviewed all available additional sources of clinical incidence information. These secondary sources included: medical requirements reports, private medical conference notes (non-EMR), research clinical surveys, post-flight experiment debriefings, and space medicine operations team notes. Essentially, anywhere a notation was possible of an in-flight medical anomaly, clinical symptoms, or treatment, the records were reviewed and events tabulated. It is important to note that this deviates from a standard epidemiological investigation, since by definition, the recording techniques may differ among the 46 ISS astronauts, and confirmatory laboratory diagnoses were not possible. Therefore, this information represents a “tabulation of reported clinical symptoms”. We further classified these events as non-notable or notable. For this review, the definition of a “notable” event consisted of an event of: 1) prolonged duration of >1 week, with some lasting through mission end; 2) repeated and/or intensified incidence; or 3) non-responsive to, or unresolved following, medication treatment during flight.
Clinical characterization of rashes onboard ISS
To generally characterize the rashes occurring on board the ISS from a clinical perspective, a more detailed evaluation of crew medical records documenting in-flight rash occurrence was performed by a NASA flight surgeon. This additional analysis was performed on all crew members who had rash events. This represented a 16-astronaut subset of the overall 46 participating crew members. For each subject, all available information (which could vary between subjects) was used for the evaluation. Rash appearance and location were recorded. In some cases, photographs of the rashes were available.
Results
Tabulation of symptom events on ISS
Specific incidence data for reported symptoms from 46 long-duration missions onboard ISS is summarized in Table 1. Spanning all event categories, 70 reports of symptoms potentially related to immune dysregulation were tabulated during flight, including both notable and non-notable events. The accumulated incidence rate for these events was found to be 3.40 events per flight year, or averaging approximately 1.7 events per 6-month ISS expedition crew member. By far, the majority of the adverse events observed on board the ISS were skin rashes (23 events), followed by upper respiratory symptoms, including congestion, rhinitis and/or sneezing (20 events). Tabulating the various types of infectious disease observed during spaceflight (including pharyngitis, skin infection, etc.) indicates at least 13 infectious disease events occurred during the reporting period. Additional categories included in the review, but for which no on-orbit reports were observed, included: malignancies, autoimmunity, sepsis, and anaphylaxis. Note that these immunologically related IMM categories do consist of confirmed-diagnosis disease states; however, for completeness, we report that no incidence of relevant symptoms for these diseases was observed for the evaluated crew members.
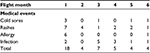
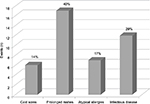
Characterization of notable medical events
A more detailed evaluation of the 70 reported medical events further classified 42 events as “notable”. Notable events included such characteristics as prolonged duration, repeated or recurring and/or, being unresponsive to treatment. These 42 notable events were observed in 46% of the crew members, whereas the remaining 54% either experienced no notable events or only events that were not classified as “notable” (Figure 1). The most likely diagnosis breakdown of these 42 noteworthy events, based on the reported symptoms, is presented in Figure 2. Almost one-half were found to be prolonged rashes, followed by infectious disease, atypical allergies, and cold sores. An evaluation of the 42 notable events in the context of mission kinetics (month) is presented in Table 2. The highest concentration of notable adverse medical events occurred during the first month of flight (18 events); however, beyond the first month, there was a generally even spread of events between months 2 and 6 of flight. An evaluation of the distribution of the 42 notable medical events among the 46 crew members is presented in Figure 3. Eleven crew members experienced a single notable in-flight medical event, whereas 10 individual crew members experienced 2 or more events. One unique crew member experienced 9 in-flight notable medical events.
  | Figure 1 Distribution of notable and non-notable in-flight reported medical events in 38 6-month ISS missions in 46 US ISS crew. Abbreviation: ISS, International Space Station. |
  | Figure 2 Breakdown of 42 reported notable medical events reported in 21 of 46 International Space Station crew members. Notes: Relative percentages among the reported events are indicated. |
  | Figure 3 Breakdown of 42 reported notable medical events reported in 46 crew members by individual crew member incidence. |
Clinical rash characterization
During spaceflight, rashes were observed to occur in the following locations: scalp, face, neck, chest, back, trunk, abdomen, arms, and hands. A representative photograph from a persistent rash incident on board the ISS is presented in Figure 4. The appearance of the rashes generally consisted of bumps/nodules and/or small brown scaly patches, with or without petechiae, redness/hyperemia, and itching.
  | Figure 4 Photograph of a persistent rash incident on a US astronaut during long-duration spaceflight on board the International Space Station. |
Discussion
The concept of astronauts becoming ill during spaceflight is not new. Early (Mercury, Gemini, Apollo) astronauts reported illness, including a noteworthy urinary tract infection on Apollo 13, which eventually resulted in the NASA HSP.32 The HSP places astronauts in a 7-day period of restricted access before a spaceflight, in an attempt to mitigate crew infectious disease on-orbit. The HSP is not a pure isolation, as astronauts still have contact with family and staff. Rather, the HSP limits contact to individuals who have been medically screened and trained to minimize crew exposure to infectious disease. This program has been successful in reducing the rate of on-orbit communicable infectious disease;32 however, illness during spaceflight remains a possibility for astronauts. Breaks in the HSP quarantine are possible, and astronauts may become infected before flight and carry a pathogen to orbit. Certain pathogens, such as latent herpesviruses, cannot be screened out by a quarantine period. Although studies are ongoing to characterize immune dysregulation during flight, increased microbial virulence during space flight may also contribute to elevated risk for infectious disease. Recent data has demonstrated that some microbes actually increase their virulence during spaceflight.33 Mermel recently summarized the infectious disease risk in the context of immunity, microbial virulence changes, and environmental conditions such as air handling, recycling, and hygiene.34 In conjunction with research data regarding human physiology during flight, it is important to know in-flight incidence rates for the ISS program. The incidence data may provide the most important tool for assessing astronaut risk during exploration class missions. Unfortunately, detailed incidence rates for the Space Shuttle and ISS programs have historically been lacking, due to astronaut medical privacy concerns.
Although an extremely large number of US astronauts were able to fly short-duration space missions onboard the Shuttle, incidence (or clinical symptoms) data from the Space Shuttle era is likely to be artificially elevated due to the presence of early space-adaptation symptoms during a 2-week orbital spaceflight. This is almost certainly true for stuffiness and congestion, which may certainly resemble allergic symptoms. Short-duration spaceflight is extremely busy and stressful, as most waking time is accounted for to meet mission objectives. Shuttle missions, with their short duration and very stressful timelines, are therefore likely to not be representative of the expected incidence for exploration class spaceflight. It is for this reason that incidence data from ISS missions must be evaluated. ISS missions consist of long-duration exposure to the microgravity and radiation environment of low Earth orbit spaceflight. ISS crew members work on a somewhat more reasonable schedule compared to Shuttle flights and generally adapt to the space environment by approximately 2–4 weeks on-orbit. Furthermore, crews are isolated from daily contact, so opportunity for communicable infectious disease is dramatically reduced. ISS incidence data therefore likely represents a more accurate reflection of in-flight clinical incidence, as human physiology would equilibrate during long-duration spaceflight.
Generating an appropriate terrestrial comparison group for this dataset is particularly challenging. The relevant space agencies fly extremely healthy and fit individuals, screen their health frequently, put them through a pre-flight quarantine, and then deploy them in an extreme and physiologically disruptive (and entirely unique) environment. We suggest that the goal of the spaceflight medical program is that the incidence numbers should therefore be “zero”. However, as rashes were the most reported event on board the ISS and are of clinical concern to flight surgeons, we will briefly discuss rash presentation and terrestrial incidence for this particular symptom. The prevalence of persistent rashes in the US population is about 0.044 cases/year,35 and our observed incidence of rashes on board the ISS was elevated in comparison at 1.12 events per flight year. The incidence for rashes on board the ISS is therefore 25-fold higher than terrestrial incidence. The body locations for rash occurrence on board the ISS seemed to vary; however, the appearance was generally consistent, manifesting as bumps, nodules, small scaly patches, and itchy redness. Presumed diagnoses for such rashes could include eczema, contact dermatitis, psoriasis, allergic cholinergic urticaria, and/or simple acne. Ilscus et al speculated that contributing factors to on-orbit rashes could include constraints of hygiene, infection, atypical herpesvirus infection, photo dermatitis, or cutaneous decompression sickness.36 Hygienic contributing factors may include soaps and no-rinse shampoo use with suboptimal ability to completely rinse the body areas after cleansing. Irritation from operational equipment, such as extravehicular (EVA – spacewalk) suits, electrocardiography electrodes, or oxygen masks could be other contributing factors, however the timing and locations of the rash events suggest that they were not related to EVA activity. In addition, the environment onboard ISS may be conducive to rashes, consisting of low humidity, prolonged contact with moisture from sweat or wet clothing, and constrained airflow. It is also possible, given that the majority of the notable in-flight events occurred in the first month of spaceflight, that early space adaptation influences these incidence numbers (Figure 3). However, we speculate that the persistent dysregulation of the immune system, including some data indicating a Th2 shift, may be a significant contributing factor to the incidence of on-orbit rashes.
Recent research data confirms persistent immunological dysregulation during spaceflight.24,37 Rashes and hypersensitivities would suggest immune dysregulation of a hypersensitive nature. There is other anecdotal commentary from recent ISS astronauts during post-flight experiment debriefing sessions that supports the possibility for some aspects of Th2 immunity to be sensitized. These include statements from multiple astronauts regarding upper respiratory symptoms (stuffiness, etc.) which persisted for 6 months and were treated with, and reported responsive to, antihistamines (data not shown). Ilscus et al further suggested that possible mitigations for on-orbit rashes might include allergy/patch testing of crew members and various crew-use and/or food products, and avoidance of any defined irritants.36 Suggested laboratory assays to further investigate rashes in astronauts could include immunoglobulin E, complement (C3a, 4a, 5a), cytokines (interleukin 5 and 13), mast/baso/eosinophils levels, prostaglandins (D2), stress hormones, and leukotrienes.
Medication usage is not routinely tracked onboard ISS; however, a recent NASA pharmacology survey of astronaut archival health records indicated that antihistamines were the most prescribed medication during flight for chronic conditions that persisted >7 days.38 For acute (<7-day duration) issues, antihistamines were second only to sleep medications. Suggested treatments for persistent allergic/hypersensitivity symptoms in astronauts may include oral antihistamines, topical steroids, antibiotics (if an infectious agents is suspected), or oral steroids. The NASA Human Research Program is currently characterizing the nature of immune system dysregulation in astronauts. This research may result in a monitoring strategy, which may be used to validate potential immune countermeasures. Addressing immune dysregulation itself may significantly mitigate the rash issue onboard ISS.
The clinical significance of these numbers is open to interpretation. Among the incidents reported here, certainly some category-specific clinical issues appear to be elevated compared to the general terrestrial population, and almost certainly appear elevated based on expectations for extremely healthy individuals in a putatively isolated environment. The hypersensitivity findings are seemingly discordant with various research data that indicates other aspects of adaptive immunity are depressed during spaceflight.2,24 It is established that several variables influence adaptive/cellular immune parameters in a negative fashion (microgravity, stress, radiation, etc.), although this phenomenon had been believed to be largely subclinical (diminished function, altered cytokine profiles, latent viral reactivation, etc.). For exploration missions, chronic immune dysregulation, coupled with increased radiation exposure and no return option, has the potential to progress into clinical diseases. It is therefore interesting that what may be considered “precursor” clinical conditions, such as tabulated here, are already being observed on-orbit. In fact, these incidence rates fit perfectly the model of spaceflight-associated immune alterations reported in the literature, which include diminished T-cell function (relates to infectious disease) and a Th2 cytokine shift (relates to hypersensitivities).1 A linkage was recently reported between alterations in cytokine profiles in astronauts and the reactivation of latent herpesviruses,37 which supports the postulate that specific types of immune bias shifts will increase risks for specific types of disease. Although subclinical reactivation of these viruses has been previously reported during spaceflight, the incidence data confirms that 6 instances of oral herpesvirus reactivation have already occurred on board the ISS. Herpesvirus reactivation resulting in fever blisters has also been reported by astronauts to occur during spaceflights. It is also interesting that the highest concentration of reported events occurred early within the 6-month mission durations. While the slope of immune alterations during spaceflight is still largely unknown, the literature to date generally finds that alterations persist for the duration of a 6-month orbital spaceflight.25 We anticipate upcoming investigations on board the ISS will shed further light on the complexities of immune adaptation during flight, and planned 1-year mission durations will improve our understanding regarding the kinetics of these alterations.
The authors acknowledge that this is a subjective report; however, great rigor was exercised to achieve a repeatable readout on ISS incidence (based on reported symptoms), given the criteria that were used. Where possible, if an event was reported as a recurrence of a previously noted event, we did not count twice. If there was no indication from the flight surgeon notes or any other source documents that the event was a recurrence, we did not infer recurrence and as such, for the purposes of this tabulation, we counted it as a new event. This criteria could lead to a higher frequency score. An evaluation of the same records using different criteria would likely generate different results. To ensure as accurate and unbiased reporting as possible, the immunologists had no exposure to the record evaluation process. Records evaluation was strictly performed by the Epidemiology staff, after the evaluation criteria were devised in consultation with the Immunology Discipline Team at the Johnson Space Center.
On the ISS, factors associated with spaceflight, including confinement, nutritional limits, and disrupted circadian rhythms, are likely to be similar to those anticipated for exploration class missions. Although a quick-return option exists for orbital flight, in-flight clinical care capability is likely similar to that experienced on exploration class missions. Therefore, we anticipate the incidence of adverse clinical events during an ISS mission to represent the best available evidence from which to extrapolate incidence rates for exploration class missions. The incidence for missions beyond Earth orbital spaceflight is likely to be higher than the rate observed during ISS missions. Unfortunately, many aspects of human immunology remain relatively uninvestigated during spaceflight. Further studies on board the ISS will complete our understanding of immune status during spaceflight. We suggest that a thorough investigation of Th2 immunity on board the ISS must be coupled with precise capture of crew clinical information and medication usage. Operational influences (crew equipment, hygiene, sleep, and work schedules), as well as deployment of unique allergens into the ISS environment (such as a permanent murine habitat), must be thoroughly evaluated to not exacerbate an already-existing clinical issue.
Finally, we note that assessments of astronauts during flight may provide unique insight into “similar” conditions that present as immunological dysregulation on Earth. For example, it is well understood that stress adversely affects immunity, which may increase susceptibility to disease.27 Aged individuals are known to present with increased infectious disease or latent viral reactivation, which may be related to immune senescence with decreased T-cell function.39 Also, terrestrial “space analog” conditions exist; locations where remote deployment, prolonged isolation, and extreme environment recreate some of the stress effects of spaceflight.40 Examples include undersea deployment or Antarctica winter-over missions. It has been established that crew members participating in such terrestrial missions also shed latent herpesviruses.41 Similarly, better controlled laboratory simulations of spaceflight confinement, such as a recent Russian 500-day Mars simulation, have also been found to re-create immune dysregulation, which shares some aspects of flight-associated dysregulation.42 We suggest monitoring strategies and countermeasures developed to assess and prevent incidence in astronauts may facilitate the reduction of illness on Earth.
Acknowledgments
The authors wish to thank Ms Jessica Garcia, NASA-JSC Epidemiology Group, for assistance in the review of the raw data sources and compilation of category-specific incidence data. We also thank Dr Hawley Kunz with KBR-Wyle at the NASA-JSC Environmental Sciences Branch for assistance with preparation of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Gueguinou N, Huin-Schohn C, Bascove M, Bueb JL, Tschirhart E, Legrand-Frossi C, Frippiat JP. Could spaceflight-associated immune system weakening preclude the expansion of human presence beyond Earth’s orbit? J Leukoc Biol. 2009;86(5):1027–1038. | ||
Borchers AT, Keen CL, Gershwin ME. Microgravity and immune responsiveness: implications for space travel. Nutrition. 2002;18(10):889–898. | ||
Chapes SK, Morrison DR, Guikema JA, Lewis ML, Spooner BS. Production and action of cytokines in space. Adv Space Res. 1994;14(8):5–9. | ||
Crucian BE, Stowe RP, Pierson DL, Sams CF. Immune system dysregulation following short- vs long-duration spaceflight. Aviat Space Environ Med. 2008;79(9):835–843. | ||
Morukov VB, Rykova MP, Antropova EN, Berendeeva TA, Ponomarev SA, Larina IM. [Indicators of innate and adaptive immunity of cosmonauts after long-term space flight to international space station]. Fiziol Cheloveka. 2010;36(3):19–30. | ||
Sonnenfeld G. Effect of space flight on cytokine production. Acta Astronaut. 1994;33:143–147. | ||
Sonnenfeld G, Miller ES. The role of cytokines in immune changes induced by spaceflight. J Leukoc Biol. 1993;54(3):253–258. | ||
Rykova MP, Antropova EN, Larina IM, Morukov BV. Humoral and cellular immunity in cosmonauts after the ISS missions. Acta Astronautica. 2008;63(7–10):697–705. | ||
Crucian BE, Cubbage ML, Sams CF. Altered cytokine production by specific human peripheral blood cell subsets immediately following space flight. J Interferon Cytokine Res. 2000;20(6):547–556. | ||
Stowe RP, Sams CF, Mehta SK, Kaur I, Jones ML, Feeback DL, Pierson DL. Leukocyte subsets and neutrophil function after short-term spaceflight. J Leukoc Biol. 1999;65(2):179–186. | ||
Kaur I, Simons ER, Castro VA, Ott CM, Pierson DL. Changes in monocyte functions of astronauts. Brain Behav Immun. 2005;19(6):547–554. | ||
Kaur I, Simons ER, Castro VA, Mark Ott C, Pierson DL. Changes in neutrophil functions in astronauts. Brain Behav Immun. 2004;18(5):443–450. | ||
Boonyaratanakornkit JB, Cogoli A, Li CF, et al. Key gravity-sensitive signaling pathways drive T cell activation. FASEB J. 2005;19(14):2020–2022. | ||
Cogoli A. The effect of space flight on human cellular immunity. Environ Med. 1993;37(2):107–116. | ||
Schwarzenberg M, Pippia P, Meloni MA, Cossu G, Cogoli-Greuter M, Cogoli A. Signal transduction in T lymphocytes – a comparison of the data from space, the free fall machine and the random positioning machine. Adv Space Res. 1999;24(6):793–800. | ||
Stowe RP, Sams CF, Pierson DL. Effects of mission duration on neuroimmune responses in astronauts. Aviat Space Environ Med. 2003;74(12):1281–1284. | ||
Stowe RP, Sams CF, Pierson DL. Adrenocortical and immune responses following short- and long-duration spaceflight. Aviat Space Environ Med. 2011;82(6):627–634. | ||
Grove DS, Pishak SA, Mastro AM. The effect of a 10-day space flight on the function, phenotype, and adhesion molecule expression of splenocytes and lymph node lymphocytes. Exp Cell Res. 1995;219(1):102–109. | ||
Nash PV, Konstantinova IV, Fuchs BB, Rakhmilevich AL, Lesnyak AT, Mastro AM. Effect of spaceflight on lymphocyte proliferation and interleukin-2 production. J Appl Physiol (1985). 1992;73(2 Suppl):186S–190S. | ||
Mehta SK, Stowe RP, Feiveson AH, Tyring SK, Pierson DL. Reactivation and shedding of cytomegalovirus in astronauts during spaceflight. J Infect Dis. 2000;182(6):1761–1764. | ||
Pierson DL, Stowe RP, Phillips TM, Lugg DJ, Mehta SK. Epstein-Barr virus shedding by astronauts during space flight. Brain Behav Immun. 2005;19(3):235–242. | ||
Stowe RP, Pierson DL, Feeback DL, Barrett AD. Stress-induced reactivation of Epstein-Barr virus in astronauts. Neuroimmunomodulation. 2000;8(2):51–58. | ||
Bascove M, Gueguinou N, Schaerlinger B, Gauquelin-Koch G, Frippiat JP. Decrease in antibody somatic hypermutation frequency under extreme, extended spaceflight conditions. FASEB J. 2011;25(9):2947–2955. | ||
Crucian B, Stowe R, Mehta S, Uchakin P, Quiriarte H, Pierson D, Sams C. Immune system dysregulation occurs during short duration spaceflight on board the space shuttle. J Clin Immunol. 2013;33(2):456–465. | ||
Crucian BE, Stowe RP, Mehta SK, Quiriarte H, Pierson DL, Sams CF. Alterations in adaptive immunity persist during long-duration spaceflight. npj Microgravity. 2015;1:15013. | ||
Stowe RP, Mehta SK, Ferrando AA, Feeback DL, Pierson DL. Immune responses and latent herpesvirus reactivation in spaceflight. Aviat Space Environ Med. 2001;72(10):884–891. | ||
Webster Marketon JI, Glaser R. Stress hormones and immune function. Cell Immunol. 2008;252(1–2):16–26. | ||
Stowe RP, Yetman DL, Storm WF, Sams CF, Pierson DL. Neuroendocrine and immune responses to 16-day bed rest with realistic launch and landing G profiles. Aviat Space Environ Med. 2008;79(2):117–122. | ||
Strewe C, Feuerecker M, Nichiporuk I, et al. Effects of parabolic flight and spaceflight on the endocannabinoid system in humans. Rev Neurosci. 2012;23(5–6):673–680. | ||
Crucian B, Sams C. Immune system dysregulation during spaceflight: clinical risk for exploration-class missions. J Leukoc Biol. 2009;86(5):1017–1018. | ||
NASA. Math and Science at Work: The Integrated Medical Model; 2013. Available from: http://www.nasa.gov/audience/foreducators/mathandscience/research/Prob_IMM_detail.html. Accessed 2015. | ||
Wooley BC, McCollum GW. Flight crew health stabilization program. In: Jones WL, editor. SP-368 Biomedical Results of Apollo. Houston (TX): BioTechnology, Inc., NASA; 1975:141–149. | ||
Wilson JW, Ott CM, Honer zu Bentrup K, et al. Space flight alters bacterial gene expression and virulence and reveals a role for global regulator Hfq. Proc Natl Acad Sci U S A. 2007;104(41):16299–16304. | ||
Mermel LA. Infection prevention and control during prolonged human space travel. Clin Infect Dis. 2013;56(1):123–130. | ||
Cherry DK, Burt CW, Woodwell DA. National ambulatory medical care survey: 2001 summary. Adv Data. 2003;(337):1–44. | ||
Ilscus LS, Johnston SL, Moynihan S, Kerstman EL, Marshal GD. Rashes and exanthems on long duration space flights. Poster presented at: 80th Annual Scientific Meeting of the Aerospace Medical Association; 2009; California. | ||
Mehta SK, Crucian BE, Stowe RP, Simpson RJ, Ott CM, Sams CF, Pierson DL. Reactivation of latent viruses is associated with increased plasma cytokines in astronauts. Cytokine. 2013;61(1):205–209. | ||
Wotring VE. Space Pharmacology. 1st ed. New York: Springer-Verlag New York; 2012. | ||
Makinodan T, Hahn TJ, McDougall S, Yamaguchi DT, Fang M, Iida-Klein A. Cellular immunosenescence: an overview. Exp Gerontol. 1991;26(2–3):281–288. | ||
Crucian B, Simpson RJ, Mehta S, et al. Terrestrial stress analogs for spaceflight associated immune system dysregulation. Brain Behav Immun. 2014;39:23–32. | ||
Mehta SK, Pierson DL, Cooley H, Dubow R, Lugg D. Epstein-Barr virus reactivation associated with diminished cell-mediated immunity in Antarctic expeditioners. J Med Virol. 2000;61(2):235–240. | ||
Pagel JI, Chouker A. Effects of isolation and confinement on humans-implications for manned space explorations. J Appl Physiol (1985). 2016;120(12):1449–1457. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.