Back to Journals » Clinical Ophthalmology » Volume 16
In Clinic Optometrist Insertion of Dextenza (Dexamethasone Ophthalmic Insert 0.4mg) Prior to Cataract Surgery: The PREPARE Study
Authors Ibach MJ , Zimprich L , Wallin DD, Olevson C, Puls-Boever K , Thompson V
Received 12 May 2022
Accepted for publication 4 August 2022
Published 13 August 2022 Volume 2022:16 Pages 2609—2615
DOI https://doi.org/10.2147/OPTH.S374405
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Video abstract presented by Mitchel J Ibach
Views: 201
Mitchel J Ibach,1 Larae Zimprich,1 Doug D Wallin,1 Collin Olevson,2 Keeley Puls-Boever,1 Vance Thompson1
1Ophthalmology, Vance Thompson Vision, Sioux Falls, SD, USA; 2Medical School, University of South Dakota School of Medicine, Vermillion, SD, USA
Correspondence: Mitchel J Ibach, Vance Thompson Vision, 3101 W. 57th St, Sioux Falls, SD, 57108, USA, Tel +1 605-361-3937, Fax +1 605-371-7035, Email [email protected]
Purpose: To evaluate the clinical outcomes with optometrist pre-surgical insertion of dexamethasone ophthalmic insert 0.4mg in the clinical office setting in patients undergoing same-day cataract surgery compared to standard of care steroid therapy.
Methods: In this prospective, contralateral eye trial, one eye received a dexamethasone ophthalmic insert 0.4mg and the other received topical prednisolone acetate 1% four times per day for one week, then three times per day for one week, then two times per day for one week, and then one time per day for one week. At one day, seven days, and four weeks postoperatively mean anterior chamber cell score and mean anterior chamber flare score was assessed by Slit Lamp Biomicroscopy and pain score was assessed by Visual Analog Scale from 0– 10. Incidence of increased intraocular pressure and cystoid macular edema were also assessed.
Results: Thirty patients (60 eyes) participated. At one day postoperative there was no significant difference in mean anterior chamber cell score (p= 0.70) or pain score (p= 0.92). There was no anterior chamber cell flare observed in the study or control group. Of the 30 patients, 29 expressed a preference for dexamethasone inserts compared to topical prednisolone acetate. One patient in the study group had elevated intraocular pressure that resolved and there was no cystoid macular edema measured.
Conclusion: In patients undergoing routine cataract surgery, there was an overwhelming preference for a dexamethasone insert compared to topical steroid drops. The dexamethasone insert produced similar ocular comfort and inflammation prevention compared to prednisolone acetate eyedrops. Dexamethasone inserts are a safe and effective treatment option for reducing pain and inflammation when inserted by an optometrist prior to routine cataract surgery.
Keywords: dexamethasone, dextenza, cataract
Introduction
Cataracts are a clouding of the crystalline lens within the eye and the most common cause of visual impairment with approximately 90% of blindness in developed countries being attributed to cataracts.1,2 While patients may be able to avoid surgery while symptoms are mild, surgery is the only option to restore vision.2 National and global cataract surgery volume is on the rise, and in 2022 US cataract surgeries performed will easily surpass 4 million surgeries.2,3 Cataract surgery is a relatively safe procedure that involves replacement of the clouded lens with a new artificial lens, and a majority of patients report better vision after.2 In most cases, serious complications do not occur. Traditional legendary postoperative care regimens consist of topical corticosteroids, non-steroidal anti-inflammatory, and antibiotic drug therapy, all in the form of eyedrops, to prevent inflammation and infection as well as decrease post-operative pain.4,5 Inflammation after ocular surgery can lead to photophobia, prolonged recovery, corneal edema, and or diminished visual benefit from the surgery.6
Although eyedrops are effective in reducing inflammation, there are challenges for patients.5 Patient non-adherence is often the result of an inability to properly administer medication or forgetting to administer medication.5 One study estimates 40% of patients forget to administer eyedrops and another found 92% of patients improperly administer eyedrops.7,8 Only 1–7% of the medication within the eye drop that is instilled is able to reach aqueous humor due to the natural eye barrier and clearance. Further, the preservatives often present in eyedrops may be toxic to the ocular surface and cause tear film disruption.5,9 Dexamethasone suspension 9% (DEXYCU®, Icon Bioscience Inc, Newark, CA) was approved in 2018 as one alternative to eye drops.10 This intraocular suspension removes need for corticosteroid drop compliance as it is a one-time placement in the posterior chamber at the time of surgery.10 Possible drawbacks include increased incidence of intraocular pressure spikes and blurred vision, and the medication is not easily removed.9–11
Dexamethasone ophthalmic insert 0.4mg (DEXTENZA®, Ocular Therapeutix, Bedford, MA) is a steroid-eluting intracanalicular plug approved on-label for the treatment of pain and post-operative inflammation in patients who have undergone ocular surgery.12 The dexamethasone insert is placed into the lower punctum and resides in the canaliculi. The intracanalicular plug will swell upon hydration by the patient’s tears and anchor into place.11 After insertion, the dissolvable dexamethasone insert delivers a tapered dose of 0.4mg dexamethasone for up to 30 days.11 By having one plug inserted, patients have a reduced ophthalmic drop regimen, which may minimize the risk of patient nonadherence as well as surface toxicity from eye drops.
In the pivotal Food and Drug Administration (FDA) clinical trial for dexamethasone ophthalmic inserts, insertion was performed in the operating room (OR) immediately following cataract surgery with the surgeon’s standard protocol.11 This led to dexamethasone insert’s label for the treatment of pain and post-operative inflammation after ocular surgery. As adoption of dexamethasone inserts have increased, protocols for insertion have expanded to include some physicians placing the intracanalicular plug outside of the operating room. This includes both placement at the slit lamp with the patient in an upright position and placement with the patient supine in the exam chair. This study reviews the outcomes of 30 patients who underwent cataract surgery in which one eye received topical steroids and one eye received a dexamethasone insert in clinic. We believe this contralateral eye study is the first to compare clinic insertion of dexamethasone inserts versus topical corticosteroids with a focus on patient preference.
Methods
This study was a single site, prospective, open label, contralateral eye trial. The protocol and materials provided to patients were reviewed and approved by an appropriate IRB (Aspire IRB) on 09/24/2020. All subjects provided written informed consent to participate, and the study was conducted in accordance with ethical principles originating from the Declaration of Helsinki. The study was entered into clinicaltrials.gov (NCT05023304). The study enrolled subject 1 on August 25th 2021, and the final exit visit was completed on January 13th 2022.
Participants were age 18 or older, undergoing routine, uncomplicated bilateral cataract surgery. Subjects were excluded if they were pregnant, had active infectious ocular or extraocular disease, were being actively treated with local or systemic immunosuppression, had known hypersensitivity to dexamethasone, had severe disease that warranted critical attention and was deemed unsafe for the study, had proliferative diabetic retinopathy or uncontrolled diabetes mellitus as deemed by an HbA1C greater than 10, had history of ocular inflammation or macular edema, had pre-existing epiretinal membrane, had allergy or inability to receive intracameral antibiotic, on systemic non-steroidal anti-inflammatory drugs (NSAIDs) greater than 1200 mg/day, or had an existing corticosteroid implant.
Potential subjects underwent a comprehensive examination that included medical and ocular history and an ophthalmic examination 1–30 days prior to surgery to establish eligibility. Eligible subjects underwent routine bilateral cataract surgery. Both eyes received intracameral dexamethasone, moxifloxacin, and ketorolac (DMK) at the time of surgery. All subjects were prescribed topical moxifloxacin 0.5% four times a day for one week and topical bromfenac 0.07% one-time per day for one month. The control eye received topical prednisolone acetate 1% four times per day for one week, three times per day for one week, two times per day for one week, and one time per day for one week. The experimental eye received a dexamethasone ophthalmic insert 0.4 mg, placed in office by an optometrist, prior to the cataract surgery.
The study had a primary outcome and multiple secondary endpoints. The primary outcome was to determine the effect of a dexamethasone intracanalicular insert through week 4. This was evaluated using mean anterior chamber cell/flare score as measured by slit lamp Biomicroscopy evaluation using a grading scale of 0 to 4 + (SUN Working Group Grading Scheme) at post-operative day 1, day 7, and week 4. A second measure in the primary outcome was mean pain score as measured by Visual Analog Score numerical grading scale 0–10 at post-op day 1, day 7, and week 4. The primary endpoint correlates with the pivotal FDA approval trial for dexamethasone inserts. The secondary endpoints included: mean anterior chamber flare score measured at the slit lamp using the aforementioned scoring system at post-op day 1, day 7, and week 4, patient preference for post-operative steroid assessed using a modified Comparison of Ophthalmic Medications and Tolerability (COMToL) questionnaire, optometrist ease of insertion of the intracanalicular plug in the office setting measured by a survey. The secondary safety measures were incidence of increased intraocular pressure (IOP)>10mmHG measured by Goldmann applanation tonometry (GAT) at post op day 1, day 7, and week 4 in addition to incidence of cystoid macular edema (CME) measured by optical coherence tomography (OCT) at post-operative week 4.
Statistical analysis of the primary outcome was conducted in a direct comparison and secondarily analyzed with a Wilcoxon signed-rank test. Post-operative pain was a matched comparison measured by a commonly used pain patient survey in Visual Analog Score. Pain scores were sub-analyzed with the Wilcoxon signed-rank test. The COMToL questionnaire used for patient preference has been validated for consistency, reliability, and reproducibility in assessing preference for medication administration. Finally, physician ease of use was surveyed for every dexamethasone insert administration on a scaled score from 0 (very easy) to 10 (very hard) in increments of 1.
Results
A total of 30 patients (60 eyes) participated in this trial. The trial included 13 male subjects and 17 female subjects. The median age in the trial was 67 years old, with no significant difference in age (p=0.389) between the two groups. All patients completed scheduled postoperative visits up to month 3. All primary and secondary assessments occurred pre-operatively as well as at 1, 7, 30, and 90 days postoperatively.
The first of two primary outcomes of anterior chamber cell score as measured by slit lamp biomicroscopy showed no evidence for a statistically significant difference between the control eyes and the experimental eyes at any time interval. On post-op day 1, scaled 0–4 on the Sun Score, the mean cell score was 1.06 in the study group and 1.15 in the control group (p=0.70). Using the same scale, on post-op day 7 the mean cell score was 0.25 in the study group and 0.22 in the control group (p=0.56; Figure 1). On post-op day 30, 28 of 30 eyes had a completely quiet anterior chamber in the control group, and all 30 eyes had a completely quiet anterior chamber in the study group. The second measure in the primary outcomes was pain score as measured by Visual Analog Score (0–10). This metric showed no evidence for a statistically significant difference in pain between the control eyes and the experimental eyes at any time interval. On post-op day 1, both groups had 23/30 patients rate pain as a 0, and the overall p-value between the treatment and control group was p=0.92 (Figure 2).
 |
Figure 2 Pain score measured by Visual Analog Score Scale (0–10). No statistical significance was found. |
The first of two secondary outcomes of anterior chamber flare score as measured by slit lamp biomicroscopy was unable to be statistically analyzed as there was no flare observed during the study. The secondary outcome of patient preference was overwhelmingly in favor of the dexamethasone insert group with 29 of 30 patients preferring dexamethasone inserts with one patient selecting no preference (Figure 3). Subjects were surveyed about eye drop burden at 7 days and 30 days postoperatively. One subject did not complete the survey. The results were consistent between time points. At 7 days postoperatively, 26/29 subjects responded eye drops are low burden and 3/29 subjects responded eye drops are a moderate burden. At 30 days postoperatively 27/29 subjects responded eye drops are low burden and 2/29 subjects responded eye drops are a moderate burden. The physician ease of use survey showed a mean result of 3.9 with a range of scores from 0–10.
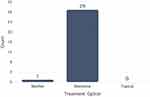 |
Figure 3 Subjective patient preference comparing the Dextenza cohort versus the control arm. Subjects expressed an overwhelming preference for treatment with Dextenza. |
The first of two safety endpoints was incidence of increased IOP >10mmgHg above baseline as measured by GAT at post-op day 1, day 7, and week 4. In the study group, one patient did have a defined IOP spike at post-op Day 1 that resolved by the day 7 appointment. Due to the timing, this IOP increase can be most likely attributed to retained viscoelastic material. There were no IOP spikes found in the control group. For the safety measure of incidence of CME, neither group had a CME diagnosis by OCT at post-op week 4.
Discussion
This single site, prospective, open label, contralateral eye trial showed an overwhelming preference for dexamethasone ophthalmic inserts over topical prednisolone acetate for postoperative healing and pain after routine cataract surgery. Although there was no significant difference between pain and inflammation between the control and experimental eyes, 29/30 patients expressed a preference for the dexamethasone insert. Increased preference for a dexamethasone insert is consistent with other clinical trials for alternative ophthalmological procedures.13–15 In a survey of patients who received dexamethasone inserts, reported convenience was the primary reason they viewed the insert as ideal for themselves and their peers.15
In three Phase III randomized clinical studies, dexamethasone ophthalmic inserts were shown to be safe and effective for control of inflammation and pain following routine cataract surgery.11,16 In the previously mentioned Phase III clinical trials, dexamethasone ophthalmic inserts were inserted in the operating room immediately following insertion of the intraocular lens (IOL). The main difference in our study is the clinic insertion of the insert by an optometric provider. Corticosteroids are effective anti-inflammatory drugs that act at multiple points in the inflammatory cascade which lead to a reduction in prostaglandins and leukotrienes.4,6 Traditionally, corticosteroids have been administered for weeks after ocular surgery in the form of eyedrops with instillation techniques and tapering instructions that may be difficult for patients to adhere to.4,5 92.6% of patients were found to have improper instillation technique and 39.2% of patients were found to be nonadherent to eyedrop regimens.7,8 Dexamethasone ophthalmic inserts reduces the reliance on correct eyedrop instillation and adherence.
In addition to the sustained dexamethasone release, another hypothesized benefit of a punctal plug is the benefits for the tear film.13 Preservatives found in eyedrops and ocular surgery can cause disruption to tear film which leads to vision and ocular symptoms.5,17,18 Dexamethasone intracanalicular inserts do not contain preservatives and this eliminates one source of ocular surface toxicity.5,19 Further by occluding the natural tear drainage pathway in the inferior canaliculus tears are unable to drain, maintaining a consistent tear film on the eye for longer.20
A prior contralateral eye study in patients undergoing photorefractive keratectomy (PRK) in which one eye was treated with topical prednisolone acetate and the second eye received a dexamethasone intracanalicular insert was unable to show a statistically significant difference in time to epithelialization.13 SPEED survey scores were not clinically or statistically different.13 Though, measurement of tear film disruption, tear osmolarity, or inflammatory markers were not determined study endpoints. A future study is needed to support this hypothesis.
Dexamethasone intracanalicular inserts are currently FDA approved to be inserted upon the completion of ophthalmic surgery.16,19 This study shows that the inserts are also effective when inserted in clinic prior to ocular surgery. The ability for an optometrist to perform insertion in a clinical setting, rather than operating room, could lead to increased practitioner adoption and patient access. This will also allow ophthalmologists to focus efforts and streamline efficiency in the operating room.
This study’s strengths include the randomized contralateral eye design which allows subjects to experience both treatments and the combination of objective and subjective measurements. The small sample size of 30 eyes in each cohort is a limitation. This sample size makes it less likely to establish statistical significance and larger studies must be done to confirm findings.
Conclusion
In patients undergoing routine cataract surgery, there was an overwhelming preference for a dexamethasone insert compared to topical steroid drops. The dexamethasone insert produced similar ocular comfort and inflammation prevention compared to prednisolone acetate eyedrops. Dexamethasone inserts are a safe and effective treatment option for reducing pain and inflammation when inserted by an optometrist prior to routine cataract surgery.
Abbreviations
FDA, Food and Drug Administration; OR, Operating room; NSAIDs, Non-steroidal anti-inflammatory drugs; DMK, Dexamethasone, moxifloxacin, and ketorolac; COMToL, Comparison of ophthalmic medications and tolerability; IOP, Intraocular pressure; GAT, Goldmann applanation tonometry; CME, Cystoid macular edema; OCT, Optical coherence tomography; PRK, Photorefractive keratectomy.
Data Sharing Statement
No individual data will be shared as a result of this clinical trial. All patients have been de-identified for enrollement, data acquisition, data analysis, and discussion. Since no individual data will be shared, the data will not be accessible on an individual basis.
Ethics Approval and Informed Consent
The protocol and materials provided to patients were reviewed and approved by an appropriate IRB (Aspire IRB) on 09/24/2020. All subjects provided written informed consent to participate, and the study was conducted in accordance with ethical principles originating from the Declaration of Helsinki. The study was entered into clinicaltrials.gov (NCT05023304). The study enrolled subject 1 on August 25th 2021, and the final exit visit was completed on January 13th 2022.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work. Consent for publication was obtained.
Funding
Supported by Ocular Therapeutix.
Disclosure
Mitch J Ibach, OD, Vance Thompson, MD, and Ms Keeley Puls-Boever have received honoraria for consulting services from Ocular Therapeutix. The authors report no other conflicts of interest in this work.
References
1. Thompson J, Lakhani N. Cataracts. Prim Care. 2015;42:409–423. doi:10.1016/j.pop.2015.05.012
2. National Eye Institute. Cataracts. National Eye Institute; 2022. Available from: https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/cataracts.
3. Lindstrom RL. Future of Cataract Surgery Seems Promising. Ocular Surgery News; 2021.
4. Porela-Tiihonen S, Kokki H, Kokki M, Kokki M. Recovery after cataract surgery. Acta Ophthalmol. 2016;94(5):1–34. doi:10.1111/aos.13055
5. Matossian C. Noncompliance with prescribed eyedrop regimens among patients undergoing cataract surgery—prevalence, consequences, and solutions. US Ophthal Rev. 2020;13(1):18–22. doi:10.17925/USOR.2020.13.1.18
6. Dua HS, Attre R. Treatment of post-operative inflammation following cataract surgery – a review. Eur Ophthal Rev. 2012;6(2):98–103. doi:10.17925/EOR.2012.06.02.98
7. Vandebroeck S, Geest SD, Dobbels F, Fieuws S, Stalmans I, Zeyen T. Prevalence and correlates of self-reported nonadherence with eye drop treatment: the Belgian Compliance Study in Ophthalmology (BCSO). J Glaucoma. 2011;20(7):414–421. doi:10.1097/IJG.0b013e3181f7b10e
8. An JA, Kasner O, Samek DA, Levesque V. Evaluation of eyedrop administration by inexperienced patients after cataract surgery. J Cataract Refract Surg. 2014;40(11):1857–1861. doi:10.1016/j.jcrs.2014.02.037
9. Brooks C, Jabbehdari S, Gupta PK. Dexamethasone 0.4mg sustained-release intracanalicular insert in the management of ocular inflammation and pain following ophthalmic surgery: design, development and place in therapy. Clin Ophthamol. 2020;14:89–94. doi:10.2147/OPTH.S238756
10. Grzybowski A, Brockmann T, Kanclerz P, Pleyer U. Dexamethasone intraocular suspension: a long-acting therapeutic for treating inflammation associated with cataract surgery. J Ocular Pharmacol Therap. 2019;35:525–534. doi:10.1089/jop.2019.0072
11. Walters T, Bafna S, Vold S, et al. Efficacy and safety of sustained release dexamethasone for the treatment of ocular pain and inflammation after cataract surgery: results from two phase 3 studies. J Clin Exp Ophthalmol. 2016;7(4):1.
12. Donnenfeld E, Hovanesian JA. FDA Approves Dextenza for Treatment of Postoperative Ocular Pain. Ocular Surgery News; 2018.
13. Ibach MJ, Shafer BM, Wallin DD, et al. Safety of dextenza 0.4 mg for the treatment of postoperative inflammation and pain in patients after photorefractive keratectomy: the RESTORE trial. J Refract Surg. 2021;37(9):590–594. doi:10.3928/1081597X-20210610-05
14. Greenwood MD, Gorham RA, Boever KR. A randomized fellow-eye clinical trial to evaluate patient preference for dexamethasone intracanalicular insert or topical prednisolone acetate for control of postoperative symptoms following bilateral femtosecond laser in site keratomileusis (LASIK). Clin Ophthamol. 2020;14:2223–2228. doi:10.2147/OPTH.S265311
15. Gira JP, Sampson R, Silverstein SM, Walters TR, Metzinger JL, Talamo JH. Evaluating the patient experience after implantation of a 0.4mg sustained release dexamethasone intracanalicular insert (Dextenza): results of a qualitative survey. Patient Prefer Adherence. 2017;11:487–494. doi:10.2147/PPA.S126283
16. Tyson SL, Bafna S, Gira JP, et al. Multicenter randomized phase 3 study of a sustained-release intracanalicular dexamethasone insert for treatment of ocular inflammation and pain after cataract surgery. J Cataract Refract Surg. 2019;45(2):204–212. doi:10.1016/j.jcrs.2018.09.023
17. Koh S, Tung CI, Inoue Y, Jhanji V. Effects of tear film dynamics on quality of vision. Br J Ophthalmol. 2018;102:1615–1620. doi:10.1136/bjophthalmol-2018-312333
18. Naderi K, Gormley J, O’Brart D. Cataract surgery and dry eye disease: a review. Eur J Ophthalmol. 2020;30(5):840–855. doi:10.1177/1120672120929958
19. Ocular Therapeutix. Dextenza (dexamethasone ophthalmic insert). U.S. Food and Drug Administration website; 2019. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/208742s001lbl.pdf.
20. Ervin A-M, Law A, Pucker AD. Punctal occlusion for dry eye syndrome (Review). Cochrane Database Syst Rev. 2017;2017(6). doi:10.1002/14651858.CD006775.pub3
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

