Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 12
Improving Esthetics of Removable Partial Dentures Using Palatal Retentive Arms
Authors Yeung C , Yu OY , Lam WYH , Leung KCM , Wong AWY , Chu CH
Received 2 July 2020
Accepted for publication 18 August 2020
Published 29 September 2020 Volume 2020:12 Pages 391—397
DOI https://doi.org/10.2147/CCIDE.S266145
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Christopher E. Okunseri
Conson Yeung, Ollie Yiru Yu, Walter Yu Hang Lam, Katherine Chiu Man Leung, Amy Wai Yee Wong, Chun Hung Chu
Faculty of Dentistry, The University of Hong Kong, Hong Kong
Correspondence: Chun Hung Chu Prince Philip Dental Hospital, 3B26, 34 Hospital Road, Sai Ying Pun, Hong Kong
Tel +852 2859 0287
Email [email protected]
Abstract: A well-designed removable partial denture can replace the loss of hard and soft tissues, restore masticatory function and maintain arch integrity. It is relatively simple, non-invasive and economical compared to other treatment options. Removable partial denture is therefore a common option among various treatment replacing missing teeth. A removable partial denture replacing anterior missing teeth can improve esthetics and hence the patient’s quality of life. However, metal components of a removable partial denture may be visible and affects patient satisfaction. Esthetics of a removable partial denture can often be improved with some modifications to traditional designs. This article reported the use of a cobalt-chromium-based removable partial denture to replace a missing maxillary lateral incisor and molars. Palatal retentive arms were employed as the retentive components on the premolars to avoid the metal component being seen when speaking and smiling. The indications and design of the removable partial dentures with palatal retentive arms are also discussed.
Keywords: denture, removable partial denture, esthetics, palatal retentive arm
Introduction
Managing partially edentulous patients is always a great challenge to dentists. With advancements in technology, treatment modalities for tooth replacement have been expanded. Removable partial dentures, resin-bonded bridges and implant-supported prostheses are commonly prescribed treatment options for teeth replacement of partially edentulous patients. The removable partial denture has a wide scope of applications. It can replace multiple missing teeth in a single prosthesis and provide replacement to the loss of hard and soft tissues. For patients who anticipate further tooth loss, simple modifications can be made to the existing denture that has incorporated components to accommodate the future loss with good planning in advance. It is often regarded as a reversible treatment option and does not preclude the more complex future modalities.1 Hence, it is useful as a definitive prosthesis as well as a temporary prosthesis or a diagnostic tool prior to the next phase of treatment.
Implant-supported prosthesis has a wide scope of applications, from single tooth replacement to full arch rehabilitation. However, apart from economical concerns, there are other factors limiting its prescription. This includes, for example, the insufficient quantity of bone or poor bone quality that often occurs in the posterior region of the maxilla. The need for surgery and its association with the possible complications may impede patients from choosing this treatment option. Meta-analysis of implant placement nerve injury studies shows a range of incidence from 0% to 13% and 40% of sinus lift procedures end up with sinus membrane perforation.2 In addition, implant therapy may be contra-indicated in medically compromised patients such as those under chemotherapy . Having said that, we agree totally that implant treatment provides an additional treatment option to restore missing teeth with outcomes very often not achievable by other treatment options for patients who are willing to invest the money and time, and free from systemic and local contraindications.
Resin-bonded bridges are generally indicated for situations where occlusal loading on the pontics is limited.3 Also, it requires sufficient enamel for bonding.4 Preparing sound teeth as conventional bridge abutments is contraindicated in the current restorative philosophy of minimal invasive care.3 On the other hand, teeth that have extensive destruction or a doubtful prognosis due to their periodontal or endodontic conditions are not considered suitable candidates to serve as abutment teeth.4 Thus, the indication of conventional bridges can be rather limited.
In general dental practice, removable partial dentures remain one of the most prescribed treatment options for the partially edentulous patients. Many people prefer a removable partial denture for health, anatomic, psychological, or financial reasons.5 Frequently, much attention in the design of partial dentures is driven towards achieving desirable mechanical requirements, namely retention, support and stability. It appears that the esthetic aspect of the denture design has not received the amount of attention it deserves. Esthetics is an important factor affecting patient satisfaction,5 and it must be remembered that esthetics may be the primary reason for the patient to seek treatment. The placement of metal clasps on the buccal surface of premolars jeopardizes the appearance significantly. Attempts to avoid metal clasps have led to the development of precision attachment devices,6 tooth-colored resin clasps and flexible buccal flanges.7 However, precision attachment requires tooth reduction, tooth colored clasps make the denture more plaque retentive whereas flexible buccal flanges undermines the support of the denture in addition to being plaque retentive.
In this article, we present a case in which cobalt-chromium-based removable partial denture was prescribed to replace maxillary missing teeth. Through some modifications to the traditional design and with attention to details, esthetics of the removable partial denture can be achieved without compromising the mechanical requirements of the denture. In addition, no additional cost and treatment time is required.
Case Report
A 56-year-old male patient requested replacement of his missing maxillary left lateral incisor (Figure 1). The missing tooth had been replaced by a resin-bonded bridge but was dislodged some time ago. He was unhappy about his appearance (Figure 2). He also complained about difficulty in chewing, especially on the right side. The medical history was clear.
 |
Figure 1 Smile profile. |
 |
Figure 2 Frontal view. |
On examination, no occluding pair was present on the right posterior region (Figure 3) and three occluding pairs (maxillary canine to mandibular canine, maxillary first premolar to mandibular first premolar and maxillary second molar to mandibular first molar) were present on the left side (Figure 4). Multiple teeth were missing in the maxillary (Figure 5) and mandibular arches (Figure 6). Radiographic examination showed generalized mild horizontal bone loss. Although all the missing teeth were extracted due to caries, he was then following a non-cariogenic diet. His oral hygiene was satisfactory and there was no active caries that required operative treatment. The objectives of the dental care plan were to maintain his oral hygiene and to replace his missing teeth to restore esthetics and function.
 |
Figure 3 Buccal right view (flipped mirror image). |
 |
Figure 4 Buccal left view (flipped mirror image). |
 |
Figure 5 Upper occlusal view (flipped mirror image). |
 |
Figure 6 Lower occlusal view (flipped mirror image). |
The care plan included oral hygiene reinforcement and scaling to prepare him for dental care. Sodium fluoride varnish was applied to his stained and arrested caries lesions. During discussion with the patient, full treatment options were presented and he opted for removable partial denture as all missing teeth could be replaced by a single prosthesis. However, he expressed concerns about the possible visibility of the metal clasps. It was decided to provide a maxillary cobalt-chromium-based removable partial denture with modified retentive components.
Cast cobalt-chromium ring clasps each engaging 0.25 mm undercut were employed on the mesio-buccal aspect of the maxillary molars. Palatal retentive components were employed on the premolars to avoid the metal being displayed during speaking and smiling. Tips of the circumferential clasp engaged the mesio-palatal undercut (0.25 mm) of the premolar abutments. Instead of the conventional reciprocal arm design that extended to the mesio-buccal aspect of the abutment tooth, a small buccal plate that extended mesially was employed to provide just more than 180° encirclement of the tooth (Figure 7). Figure 8 shows the removable partial denture fitted in the mouth. Through the use of a labial flange, the maxillary left lateral incisor was set in the correct bucco-palatal angulation. The patient was satisfied with the esthetics (Figure 9). Figure 10 shows the removable partial denture replacing the lateral incisor and associated soft tissue. No metal could be seen when the patient spoke or smiled.
 |
Figure 7 Denture framework and the fulcrum line AB. |
 |
Figure 8 Upper occlusal view with denture in situ (flipped mirror image). |
 |
Figure 9 Open profile with denture. |
 |
Figure 10 Frontal view with denture. |
Discussion
Replacement with Removable Partial Denture
The patient sought treatment because of esthetics concerns after the cantilever resin-bonded bridge was dislodged. Although a 2-unit cantilever resin-bonded bridge is a non-invasive treatment option with a 5-year success rate close to 90%,8 the patient was worried about its longevity and refused to re-cement the dislodged bridge or remake a new bridge. A considerable amount of bone loss, especially labially, had occurred at the edentulous ridge of the left lateral incisor region. An additional grafting procedure would be required so that the implant-supported prosthesis could be constructed in the proper bucco-palatal position and orientation. A sufficient amount of hard and soft tissue was also essential for an aesthetic location of the gingival margin. Implant-supported prosthesis was not considered suitable because the patient preferred a non-invasive treatment without surgery.
The maxillary left central incisor and canine were sound and had no caries experience. Preparing these two teeth for the conventional bridge would require removing a lot of sound tooth substance. As gingival recession was evident, more tooth substance would have to be removed to place the retainer margin equi-gingivally, which could injure the pulp. The pontic needs to be over-built to replace the amount of soft tissue loss. In addition, the pontic would have to be more proclined than it should be for the incisal edge to be located at the right level. Soft tissue grafting to augment the edentulous ridge was not proposed because no conclusion could be made regarding its long-term success.9 A removable partial denture with a buccal flange allowed proper orientation of the prosthetic tooth. It also enabled the gingival margin of the prosthetic tooth to be placed at the correct level. Occluding pairs at the posterior region, especially on the right side, were provided, which addressed the patient’s complaint of difficulty in chewing. An esthetic removable partial denture was therefore the choice of treatment for this patient. At the time, it did not appear that a lower removable partial denture would further improve chewing function or esthetics.
Use of Palatal Clasps
One of the major challenges of designing the removable partial denture in this case was how to prevent the anterior saddle area to rotate away from the denture bearing area about a fulcrum line joining the distal rests on the upper right second molar and the upper left first molar (line AB in Figure 7). This could be resisted by the ring-clasps engaging the undercuts on the mesio-buccal aspect of these molars. However, these retentive arms would not be effective in preventing such a movement because they were close to the fulcrum line. Although placing retentive arms on the central incisor and canine was mechanically favorable, the denture would be esthetically unacceptable. The esthetics could be improved by placing the retentive arms at the buccal surface of the maxillary premolars. Further improvement in esthetics could be obtained by shifting the retentive arms to the palatal side. To illustrate the design of the palatal retentive arm, a close-up view of the buccal reciprocal plate from a different patient is shown on cast (Figure 11) and in the patient’s mouth (Figure 12). The esthetics was good without any visible clasp on the premolar, and the plate was hardly visible. It is therefore desirable if the retentive components are placed on the palatal surface instead of the buccal surface. One possible drawback of this design is that the denture has to be retrieved by disengaging the clasp tips from the undercut at the palatal side. Nonetheless, the patient showed no difficulty in removing the denture.
 |
Figure 11 Palatal clasp design. |
 |
Figure 12 Denture in situ (same denture as in Figure 11). |
Clasp Design
The cast should be surveyed as usual. To design a palatal clasp for esthetics, the mesial abutment tooth should allow placement of a distal guiding plane and a disto-buccal reciprocal plate, as well as having a proper undercut at the mesio-palatal aspect. Tooth preparation may be required to achieve this. By engaging the mesio-palatal undercuts and having the reciprocal plate extending more than 180° of the tooth, an extremely good aesthetic result could be achieved without jeopardizing retention or stability of the denture.
The flexibility of the clasp reduces as the length of the arm decreases. Short clasps would make denture insertion and removal difficult and even damaging. The length of the retentive arm on premolars can be limited because of their small size. This is not a problem if a suitable undercut can be located in the gingival one-third of the tooth. The circumferential clasp emerges distally near the occlusal surface of the tooth and engages a mesial undercut more gingivally. This helps to make the clasp arm longer, thereby increasing its flexibility. Note that cobalt-chromium was used for the clasp arms in this case because suitable undercut areas were sufficiently gingivally located to allow the clasp arms to be of the desirable length.
However, for premolars with pronounced cervical constriction, if cast cobalt-chromium is used, we cannot make the clasp arm longer by having the clasp tip more gingivally placed because of its high modulus of elasticity. This problem can be solved by choosing a material with a lower modulus of elasticity such as wrought gold wires. The modulus of elasticity of wrought gold wire10 is only about half that of cast cobalt-chromium.11 Wrought gold wire can engage a 0.50 mm undercut, which allows for the clasp tip to be more gingivally placed. This, in turn, would increase the clasp length for better flexibility. The wrought wire can either be soldered to the framework or cast to the framework by embedding the wire in the wax pattern of the framework (Figure 13). Figure 14 shows the same denture framework in the mouth.
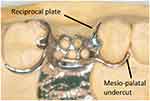 |
Figure 13 Framework with wrought gold wire. |
 |
Figure 14 Framework try-in to check retention. |
Wrought metal refers to a metal that has been plastically deformed to alter its shape and certain mechanical properties, such as strength, hardness, and ductility.10 If the piece is reheated, annealing may occur and thereby changing some of these mechanical properties. It may therefore appear that if a wrought clasp is short, the heating effect of soldering may change the flexibility of the clasp. However, this is not the true. Firstly, although the mesio-distal width of the premolar tooth which was employed as the abutment tooth for the wrought clasp was shorter than the mesio-distal width of an average molar, as mentioned above, by engaging an undercut area which was more gingivally placed, the length of the clasp became considerably longer than the mesio-distal width of the premolar. Most importantly, the modulus of elasticity remains unchanged during cold working in the first place.12 Hence, reversal of the effect of cold working, if any, would have no effect on the flexibility of the wrought clasp.
If the palatal aspect of the tooth is rotated mesially to such an extent that a clasp of sufficient length cannot be employed, this approach would not be suitable.
Alternatives in Esthetics Denture Design
A whole array of precision attachment devices exists that can avoid the use of clasps on teeth, though these devices would require crowning of the tooth.6 If the tooth does not otherwise require a crown, crowning it would increase the financial cost, weaken the tooth and jeopardize pulpal health. Note that while surveyed crowns allow more precise control over the contour of the abutment teeth in regions planned for rest seats, retentive arms and reciprocal arms,13 they do not in themselves eliminate the need for retentive arms. Some clinicians use tooth-colored resin clasps to improve esthetics of removable partial dentures. However, these clasps are generally bulky and promote plaque retention.7 In addition, materials such as polyoxymethylene and polyetheretherketone (PEEK) are not suitable for clasp fabrication because they can break during removal with large undercuts.14 Moreover, they are difficult to adjust and polish, and are easy to break. Flexible removable partial dentures with no rest are not recommended because they are mucosal borne and can increase risk of periodontal disease.7
Conclusion
This case report described the indication and design of palatal retentive arms in removable partial dentures. This modified retentive arm provides good esthetics in addition to support, stability and retention. It provides a non-invasive and economical treatment option to restore oral health in partially edentulous patients. The patient was very satisfied with the outcome.
Ethics and Consent
Written informed consent for joining the study was obtained prior to the commencement of the treatment. Consent for publication: Written informed consent was also obtained for publication of the details of the patient. No institutional approval was required to publish the case details.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Rich B, Goldstein GR. New paradigms in prosthodontic treatment planning: a literature review. J Prosthet Dent. 2002;88(2):208–214. doi:10.1067/mpr.2002.127886
2. Resnik RR. Classification of dental implant complications. In: Mich’s Avoiding Complications in Oral Implantology. Resnik RR, Misch CE, editors. St. Louis, Missouri: Elsevier; 2018:1–12.
3. Shah R, Laverty DP. The use of all-ceramic resin-bonded bridges in the anterior aesthetic zone. Dent Update. 2017;44(3):230–238. doi:10.12968/denu.2017.44.3.230
4. Shillingburg HT, Sather DA, Wilson EL, et al. Fundamentals of Fixed Prosthodontics.
5. Chu CH, Chow TW. Esthetic design of removable partial dentures. Gen Dent. 2003;51(4):322–324.
6. Kaiser F. Attachments in the Laboratory. Hanover Park, IL: Quintessence Pub; 2013.
7. Fueki K, Ohkubo C, Yatabe M, et al. Clinical application of removable partial dentures using thermoplastic resin Part I: definition and indication of non-metal clasp dentures. J Prosthodont Res. 2014;58(1):3–10. doi:10.1016/j.jpor.2013.12.002
8. Lam WYH, Botelho MG, McGrath CPJ. Longevity of implant crowns and 2-unit cantilevered resin-bonded bridges. Clin Oral Implants Res. 2013;24(12):1369–1374. doi:10.1111/clr.12034
9. Marzadori M, Stefanini M, Mazzotti C, Ganz S, Sharma P, Zucchelli G. Soft‐tissue augmentation procedures in edentulous esthetic areas. Periodontol 2000. 2018;77(1):111–122. doi:10.1111/prd.12210
10. Anusavice KJ, Shen C, Rawls HR. Wrought metals. In: Phillips’ Science of Dental Materials-E-Book. Anusavice KJ, Phillips RW, editors.
11. Anusavice KJ, Shen C, Phillips RW. Dental casting alloys and metal joining. In: Phillips’ Science of Dental Materials–E-Book. Anusavice KJ, Phillips RW, editors.
12. Anusavice KJ, Shen C, Rawls HR. Mechanical properties of dental materials. In: Phillips’ Science of Dental Materials-E-Book. Anusavice KJ, Phillips RW, editors.
13. Carr AB, Brown DT. Considerations for the use of dental implants with removable partial dentures. In: McCracken’s Removable Partial Prosthodontics. Brown DT, Carr AB, McCracken WL, editors.
14. Tribst JPM, Dal Piva A, Borges ALS, et al. Effect of different materials and undercut on the removal force and stress distribution in circumferential clasps during direct retainer action in removable partial dentures. Dent Mater. 2020;36(2):179–186. doi:10.1016/j.dental.2019.11.022
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
