Back to Journals » Clinical Ophthalmology » Volume 14
Impact of Vitreal Tamponade on Functional Outcomes in Vitrectomy with ILM Peeling in Primary Macula-Involving Retinal Detachment: A Retrospective Analysis
Authors Deiss M, Kaya C, Pfister IB , Garweg JG
Received 16 October 2020
Accepted for publication 8 December 2020
Published 24 December 2020 Volume 2020:14 Pages 4493—4500
DOI https://doi.org/10.2147/OPTH.S287107
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mario Deiss,1,* Cagdas Kaya,2,3,* Isabel B Pfister,2,3 Justus G Garweg1– 4
1University of Bern, Bern, Switzerland; 2Swiss Eye Institute, Rotkreuz, Switzerland; 3Berner Augenklinik am Lindenhofspital, Bern, Switzerland; 4Department of Ophthalmology, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland
*These authors contributed equally to this work
Correspondence: Justus G Garweg
Berner Augenklinik am Lindenhofspital, Bremgartenstrasse 119, Bern CH – 3012, Switzerland
Email [email protected]
Background: To compare visual outcomes of vitrectomy with internal limiting membrane (ILM) peeling and failed SF6 gas tamponade requiring silicone oil (SO) in a second procedure with primary SO tamponade in fovea-involving retinal detachment (FiRD).
Methods: Retrospective analysis of 82 eyes with retinal detachment and mild, but without advanced proliferative retinopathy (PVR ≥C2) requiring vitrectomy for FiRD. Group 1 comprised 23 eyes that underwent SF6 tamponade resulting in re-detachment requiring revision surgery with secondary SO tamponade. Based on the intraoperative findings, group 2 patients had primarily received SO as vitreal tamponade (n=59). Patients receiving a scleral buckle surgery or with advanced PVR as well as patients with underlying vascular diseases and uveitis were excluded.
Results: Preoperative visual acuity (Early Treatment Diabetic Retinopathy Study letters) was 13.5 ± 19.1 in group 1 and 14.0 ± 18.3 in group 2 (p=0.44). Twelve months after first surgery for FiRD, visual acuity was 49.8 ± 19.8 in group 1 and 51.7 ± 18.7 letters in group 2 (p= 0.63). Re-detachment after SO removal requiring revision surgery developed in 17.4 (n=4) and 15.3% (n=9) cases.
Conclusion: Our findings suggest that if retinal traction is completely relieved at the end of surgery, vitrectomy with ILM peeling and SF6 may, if successful, improve the functional outcomes in instances with visual potential, ie, a foveal detachment of short duration despite the presence of a mild to moderate PVR, but with the inherent increased risk of re-detachment requiring further intervention and the use of a SO tamponade. Hence, secondary SO installation during re-vitrectomy after failed primary reattachment surgery results in similar functional outcomes as primary oil filling.
Keywords: internal limiting membrane, ILM peeling, macula-off, retinal detachment, silicone oil tamponade, vitrectomy
Introduction
Macular involvement in retinal detachment (RD) has been associated with poor visual outcome. Despite anatomic success, predictors of a lower functional outcome include the duration of macular detachment, preoperative presence of proliferative vitreoretinopathy (PVR), extension of RD, and the age of the patient.1–5 Surgical techniques for RD repair comprise scleral buckling and pars plana vitrectomy (PPV) alone or in combination. However, in cases of macular involvement, based on a low-certainty evidence, vitrectomy may achieve better functional outcomes,6–10 thus rendering the technique the treatment of choice for RD repair. The refinement of this technique in the last two decades has resulted in improved success.11–13
Especially in cases with extended RD complicated by macular involvement, PVR, vitreous hemorrhage, and multiple and inferior retinal breaks, the choice of vitreous tamponade in PPV has remained open to surgical experience.14 In cases complicated by macular involvement, functional outcome is frequently limited even after successful anatomical reattachment.15 In such cases, silicone oil (SO) is preferred because of its higher primary success rate.16–18 However, SO tamponade is associated with major disadvantages. These include SO removal, which usually occurs within months after successful reattachment, as well as the development of secondary glaucoma, keratopathy, epiretinal membranes (ERM), retinal nerve fiber layer loss, potential toxic effects, and unexplainable visual loss.19–23 Furthermore, SO tamponade does not necessarily have a better primary anatomical success rate and visual outcomes than gas.24–28
In a recent retrospective study, we reported unprecedented visual gains over 6 months after successful primary reattachment surgery with peeling of the inner limiting membrane (ILM) and SF6 gas tamponade,29 whereas the visual potential upon use of SO tamponade is usually limited to 1.0 or more on a LogMAR scale.29 Since the introduction of vital dyes, ILM peeling has become a routine part of vitrectomy and mainly helps to prevent epiretinal membrane formation and recurrences.30 Correspondingly, the primary objective of this study was to assess the functional outcomes of eyes with re-detachment after SF6 tamponade requiring revision surgery with SO tamponade. The functional outcomes were compared to eyes operated during the same period, but achieving anatomic success after the primary use of SO tamponade.
Methods
Study Design
Medical reports of 452 consecutive patients who underwent vitreoretinal surgery for primary RD between January 2008 and December 2017 at the Berner Augenklinik am Lindenhofspital, Bern, Switzerland were analysed retrospectively. All patients were informed about the nature of their disease, treatment options, as well as the potential risks associated with the surgical procedure. Written informed consent was provided by the study participants including the use of coded data for investigational and quality control purposes.
Patients who met the following criteria were eligible for inclusion: Primary extensive retinal detachment involving the foveal centre of the macula (FiRD) requiring vitreoretinal surgery with ILM peeling. If at the end of surgery in the absence of larger breaks in the lower 4 clock-hours of the retinal no residual traction was evident, the decision to use SF6 or SO (2000 centistokes) was based on the intraoperative surgical decision, and the majority of eyes received a 15% SF6 tamponade. Patients were requested to position on the opposite side of breaks to optimize the support of the breaks. In the case of a macula-off situation, patients were generally requested to additionally perform face down positioning for 3 hours per day during the first days with the idea to prevent foveal dislocation and to support resorption of residual submacular fluid. SO tamponade as a primary surgical strategy was chosen in patients who were not able to follow the positioning requests, had underlying diseases limiting their support for a revision surgery or the presence of a mild-to-moderate PVR (up to PVR stage C1 according to the updated Retina Society grading system).31 The same criteria were applied in eyes requiring a re-vitrectomy for re-detachment within 6 months after primary vitrectomy with SF6 gas tamponade and a PVR up to stage C1.
Eyes with the following findings were excluded: not completely resolved traction and large inferior breaks at the end of vitrectomy; RD within 6 months after any intraocular surgery; history of previous RD surgery or ocular trauma; axial myopia more than −6 diopters or an axial length >26 mm; any macular pathology prohibiting visual recovery (ie, age-related macular degeneration, macular hole); PVR grade C2 or higher as well as tractional component at the time of surgery, because this would trigger SO implantation (Retina Society classification);31 end-stage glaucoma; hereditary optic neuropathy; amblyopia; and inflammatory or vascular ocular diseases potentially affecting the postoperative clinical course (ie, uveitis, diabetic retinopathy, or condition after retinovascular occlusion).
Clinical Assessments
A full clinical examination including best-corrected visual acuity (BCVA), intraocular pressure, axial length, biomicroscopy of the anterior and posterior segment, as well as retinal imaging using an ultra-widefield scanning laser ophthalmoscopy (Optos® 200Tx, Dunfermline, United Kingdom) and spectral-domain OCT (SD-OCT; Heidelberg Spectralis-OCT; Heidelberg Engineering, Heidelberg, Germany) were performed prior to surgery, and postoperatively after 1, 6, and 12 months. Baseline was set at the date of vitrectomy with SO tamponade (group 1, date of re-vitrectomy; group 2, date of first surgical procedure). The height of foveal retinal detachment was measured from the ILM to the inner surface of the retinal pigment epithelium.
Surgical Procedure
All surgical cases were performed by the same surgeon using 23-gauge PPV combined with trypan blue (MembranBlue®, Dorc International, Zuidland, the Netherlands) assisted peeling of ILM, retinotomy, endodrainage, endolaser- and cyro-retinopexy, as well as SF6 tamponade if postoperative positioning was supported by the patient and deemed sufficient to support the retina. Based on surgical decision at the end of re-attachment surgery, SO was primarily installed in presence of significant traction (group 2) or during revision surgery after re-detachment within 6 months of primary reattachment surgery (group 1). Patients in a phakic state upon RD diagnosis underwent lens replacement during retinal reattachment surgery. SO tamponade was generally left for six, but minimally 3 months in order to follow the wound healing process and a possible development of PVR, and to allow this biological process to stabilize if present, which usually takes six months. In order to minimize the burden of disease, SO removal was not enforced in eyes without functional potential well tolerating this tamponade.32
We hypothesized that re-detachment after unsuccessful primary reattachment surgery might be associated with a less favourable functional outcome. Accordingly, the primary outcome parameter was change in BCVA from before SO instillation to 12 months postoperatively.
Ethics
The study was approved by the Institutional Review Board of the Kantonale Ethikkommission Bern (Swiss Ethics Committees on research involving humans under the registration number KEK 386/2015). The study conformed to the tenets set forth in the Declaration of Helsinki and was performed in accordance with the Health Insurance Portability and Accountability Act of 1996.
Statistical Analysis
As the data were not normally distributed, a series of nonparametric tests were used and data presented with mean and standard deviation (SD) as well as median and interquartile range (IQR). The Wilcoxon signed-rank test was applied for each group separately to determine significance in changes in Early Treatment Diabetic Retinopathy Study (ETDRS) scores within the group over time. The Mann-Whitney U-test was used to compare differences between the two groups in ETDRS scores at all time points. The Pearson chi-square test was used to compare the number of patients with recurrence of new PVR and new ERM formation 12 months postoperatively. All statistical analyses were performed using the SPSS software package V.23 (SPSS, Inc., Chicago, Illinois, USA) and R (version 3.2.4; R: A language and environment for statistical computing, R Foundation for Statistical Computing, Vienna, Austria, 2016). A value of p < 0.05 was considered statistically significant.
Results
Selection and Participants
A total of 82 of 386 eyes were eligible for inclusion, whereas 370 patients were excluded. Of these, 119 patients had RD not involving the fovea, 49 patients had a secondary RD (vitreous surgery in the past or history of trauma to the affected eye), 19 patients showed concomitant eye disease [age-related macular degeneration (n = 5), history of uveitis (n = 1), end-stage glaucoma (n = 1), diabetic retinopathy (n = 2), hereditary optic neuropathy (n = 2), retinal vascular occlusive disease (n = 2), amblyopia (n = 3), RD with a coexisting macular hole (n = 3)], as well as 33 patients with high myopia. In addition, four eyes remained phakic in younger participants, eight patients were lost to follow-up, five patients did not consent to the use of their coded data, and 67 patients had been operated successfully for a primary FiRD using ILM peeling and SF6 as an endotamponade. As mentioned above, the results in these eyes were reported elsewhere.29
Of the 82 eyes that underwent surgery for FiRD, 23 had initially been treated with an SF6 endotamponade but developed retinal re-detachment (re-FiRD; 14 macula-off, nine macula-on) within a 6-month follow-up period. These patients subsequently underwent re-vitrectomy with a secondary SO tamponade (group 1), whereas 59 eyes primarily received a SO endotamponade (group 2).
Demographic parameters including age, gender, baseline visual acuity, lens status and RD height were comparable between both groups (Table 1). This was also observed for baseline characteristics, namely the duration of symptoms and vision loss before surgery, duration from diagnosis to surgery, and presence of PVR or ERM, as well as RD extension (Table 2). Preoperative visual acuity and postoperative functional (Figure 1) and anatomic recovery (Figure 2, Table 3, Table 4) were similar between both groups. Secondary ERM development was not observed clinically and in OCT. Both groups presented comparable rates of new PVR and re-detachment during the postoperative follow-up period (Table 4). The mean time until SO removal was 6.5 ± 1.8 months in the total sample and was similar in groups 1 and 2 (group 1, 6.6 ± 2.1 months vs group 2, 6.4 ± 1.7 months; p = 0.97, Mann–Whitney U-test test). Furthermore, visual outcome was stable in both group 1 (before SO removal: median 50.1, interquartile range (IQR) 35 to 58.9 mean and SD 47.4 ± 17.3 vs after SO removal: median 54.9, IQR 39.0 to 65.1 mean and SD 51.6 ± 17.0; p = 0.09, Wilcoxon signed rank test) and group 2 (before SO removal: median 54.9, IQR 44.1 to 65.1, mean and SD 53.0 ± 15.0 vs after SO removal: median 59.6, IQR 45.2 to 65.1, mean and SD 55.4 ± 15.5; p = 0.09, Wilcoxon signed rank test). SO still remained in 12 cases (group 1 = 6 patients, group 2 = 6 patients) at 12 months following SO instillation.
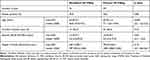 |
Table 1 Baseline Characteristics |
 |
Table 2 Preoperative Characteristics |
 |
Table 3 Change in BCVA |
 |
Table 4 Postoperative Complications |
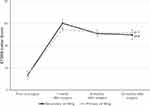 |
Figure 1 Best-corrected visual acuity (BCVA in EDTRS letters). Error bars represent the standard error of the mean (SEM). |
 |
Figure 2 Central retinal thickness (CRT in μm). Error bars represent the standard error of the mean (SEM). |
Re-detachment after SO removal requiring revision surgery developed in 17.4% (n=4) of patients with secondary oil filling and in 15.3% (n=9) of patients with primary oil filling (p=0.73). Of the four patients from group 1, two had a re-detachment with macula on and 2 with macula off. In group 2, six of the nine patients had a re-detachment with macula on and three with macula off (Table 4).
Discussion
According to our retrospective analysis, the outcome of secondary SO instillation after failed primary reattachment surgery seems not to lead to a poorer functional outcome compared to primary oil filling. Recently, we reported a mean visual gain of >25 letters after vitrectomy with ILM peeling and successful SF6 gas filling but excluded cases with re-detachment.29 A high anatomic success rate, but not a comparable visual gain was observed after primary SO tamponade in the present study. The functional results in the here reported primarily unsuccessful cases after ILM peeling and SF6 tamponade indicate that the chance of significant visual improvement might outweigh the benefits of a primary SO tamponade.
One quarter of our eyes with relatively extensive, ie, macula-involving RD that received primary SF6 gas filling (23 out of 90 eyes), developed re-detachment (group 1 patients). The retinal reattachment rate in eyes receiving primary SF6 gas filling was thus 74.4%, which is well in line with a recent meta-analysis reporting a primary success rate between 72% and 79%9 and a recently published study33 with a reattachment rate of 72.6% after primary surgery. Although the study cohorts were relatively small, both groups were well comparable regarding baseline characteristics as well as visual and anatomic outcomes and showed similarities to previously published studies.34–37 We think that although a retrospective analysis was performed, representation of this problem was achieved. The comparable demographic and preoperative characteristics of both groups add to the strength of the present study, which applied strict inclusion and exclusion criteria to exclude a maximum number of outcome confounders.
SO is the standard treatment used in the presence of PVR.38,39 Based on the exclusion of eyes with advanced PVR, eyes that primarily received SO (group 2) showed a similar disease severity, namely preoperative PVR. This is also supported by a similar postoperative course between the two groups regarding new PVR formation over the 12-month follow-up period. The intraoperative surgical decision to use SO may indicate that the surgical risk for re-detachment was estimated as increased, thus arguing for the primary use of SO.27,28
The lack of postoperative ERM formation can be explained by the systematic use of ILM peeling in all patients.40 However, based on our retrospective analysis, an advantage for visual outcomes after peeling was not observed using SO compared to the successful use of SF6 gas tamponade29 but was similar to non-ILM peeled eyes.41 The rates of new PVR formation (17% vs 13%, p=0.73) and of re-detachment after SO removal were comparable in both groups and within the expected range (17% vs 15%, p=0.73), suggesting that secondary SO placement after failed primary vitrectomy with gas tamponade does not expose the eye to an additional PVR risk.
In conclusion, given the remarkably better functional outcome of successful primary SF6 tamponade compared to primary SO tamponade, our results advocate a primary attempt with SF6 in combination with vitrectomy and ILM peeling in FiDR if the retina is completely attached, the traction fully and the patient cooperative and able to follow positioning advice.
Eyes requiring a second vitrectomy with SO after failed primary reattachment surgery in this retrospective analysis showed similar functional and anatomic outcomes as those primarily receiving SO tamponade.
Data Sharing Statement
The dataset generated and analysed during the current study is available at:
http://augenklinik-bern.ch/research/Vitreal_tamponade_Data_July_2020.xlsx.
Disclosure
JGG advises several pharmaceutical companies (Alcon, Allergan, Bayer, Novartis) and participates in a number of international, multicentre clinical studies that are sponsored by Novartis, Bayer in the fields of AMD and diabetic retinopathy. These activities had no bearing on the study that gave rise to the submitted article, for which JGG received neither direct nor indirect financial support; nor has he conflicts of interest with any of the presented data or this work. The other authors have no potential conflicts of interest for this work.
References
1. Ross WH, Kozy DW. Visual recovery in macula-off rhegmatogenous retinal detachments. Ophthalmology. 1998;105(11):2149–2153. doi:10.1016/S0161-6420(98)91142-3
2. Pastor JC, Fernandez I, de la Rodriguez RE, et al. Surgical outcomes for primary rhegmatogenous retinal detachments in phakic and pseudophakic patients: the Retina 1 Project-report 2. Br J Ophthalmol. 2008;92(3):378–382. doi:10.1136/bjo.2007.129437
3. Poulsen C, Green D, Grauslund J, Peto T. Long-term outcome of patients operated with pars plana vitrectomy for primary rhegmatogenous retinal detachment. Ophthalmic Res. 2020;63(1):25–33. doi:10.1159/000499130
4. Mitry D, Awan MA, Borooah S, et al. Surgical outcome and risk stratification for primary retinal detachment repair: results from the Scottish Retinal Detachment study. Br J Ophthalmol. 2012;96(5):730–734. doi:10.1136/bjophthalmol-2011-300581
5. Mitry D, Awan MA, Borooah S, et al. Long-term visual acuity and the duration of macular detachment: findings from a prospective population-based study. Br J Ophthalmol. 2013;97(2):149–152. doi:10.1136/bjophthalmol-2012-302330
6. Huang C, Fu T, Zhang T, Wu X, Ji Q, Tan R. Scleral buckling versus vitrectomy for macula-off rhegmatogenous retinal detachment as accessed with spectral-domain optical coherence tomography: a retrospective observational case series. BMC Ophthalmol. 2013;13(1):12. doi:10.1186/1471-2415-13-12
7. Schmidt JC, Rodrigues EB, Hoerle S, Meyer CH, Kroll P. Primary vitrectomy in complicated rhegmatogenous retinal detachment—a survey of 205 eyes. Ophthalmologica. 2003;217(6):387–392. doi:10.1159/000073067
8. Wolfensberger TJ, Gonvers M. Optical coherence tomography in the evaluation of incomplete visual acuity recovery after macula-off retinal detachments. Graefes Arch Clin Exp Ophthalmol. 2002;240(2):85–89. doi:10.1007/s00417-001-0410-6
9. Znaor L, Medic A, Binder S, Vucinovic A, Lovric JM, Puljak L. Pars plana vitrectomy versus scleral buckling for repairing simple rhegmatogenous retinal detachments. Cochrane Database Syst Rev. 2019;3(3):CD009562.
10. Baba T, Kawasaki R, Yamakiri K, et al. Japan-Retinal Detachment Registry Group. Visual outcomes after surgery for primary rhegmatogenous retinal detachment in era of microincision vitrectomy: Japan-Retinal Detachment Registry Report IV. Br J Ophthalmol. 2020;
11. Jackson TL, Donachie PH, Sallam A, Sparrow JM, Johnston RL. United Kingdom National Ophthalmology Database study of vitreoretinal surgery: report 3, retinal detachment. Ophthalmology. 2014;121(3):643–648. doi:10.1016/j.ophtha.2013.07.015
12. Haugstad M, Moosmayer S, Bragadόttir R. Primary rhegmatogenous retinal detachment – surgical methods and anatomical outcome. Acta Ophthalmol. 2017;95(3):247–251. doi:10.1111/aos.13295
13. Heimann H, Bartz-Schmidt KU, Bornfeld N, Weiss C, Hilgers R-D, Foerster MH. Scleral buckling versus Primary Vitrectomy in Rhegmatogenous Retinal Detachment Study Group. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment: a prospective randomized multicenter clinical study. Ophthalmology. 2007;114(12):2142–2154. doi:10.1016/j.ophtha.2007.09.013
14. Heussen N, Feltgen N, Walter P, Hoerauf H, Hilgers RD, Heimann H, SPR Study Group. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment study (SPR Study): predictive factors for functional outcome. Study report no. 6. Graefes Arch Clin Exp Ophthalmol. 2011;249(8):1129–1136. doi:10.1007/s00417-011-1619-7
15. Garweg JG, Tappeiner C, Halberstadt M. Pathophysiology of proliferative vitreoretinopathy in retinal detachment. Surv Ophthalmol. 2013;58(4):321–329. doi:10.1016/j.survophthal.2012.12.004
16. Karel I, Michalickova M, Soucek P. Long-term results of pars plana vitrectomy and silicone oil for giant tears. Eur J Ophthalmol. 1996;6(3):315–321. doi:10.1177/112067219600600316
17. Ghosh YK, Banerjee S, Savant V, et al. Surgical treatment and outcome of patients with giant retinal tears. Eye. 2004;18(10):996–1000. doi:10.1038/sj.eye.6701390
18. Unlu N, Kocaoğlan H, Acar MA, Sargin M, Aslan BS, Duman S. The management of giant retinal tears with silicone oil. Eur J Ophthalmol. 2003;13(2):192–195. doi:10.1177/112067210301300211
19. Newsom RS, Johnston R, Sullivan PM, Aylward GB, Holder GE, Gregor ZJ. Sudden visual loss after removal of silicone oil. Retina. 2004;24(6):871–877. doi:10.1097/00006982-200412000-00005
20. Cazabon S, Groenewald C, Pearce IA, Wong D. Visual loss following removal of intraocular silicone oil. Br J Ophthalmol. 2005;89(7):799–802. doi:10.1136/bjo.2004.053561
21. Herbert EN, Laidlaw DA, Williamson TH, Habib M, Steel D. Loss of vision once silicone oil has been removed. Retina. 2005;25(6):
22. Moya R, Chandra A, Banerjee PJ, Tsouris D, Ahmad N, Charteris DG. The incidence of unexplained visual loss following removal of silicone oil. Eye. 2015;29(11):1477–1482. doi:10.1038/eye.2015.135
23. Poulsen CD, Peto T, Grauslund J, Green A. Epidemiologic characteristics of retinal detachment surgery at a specialized unit in Denmark. Acta Ophthalmol. 2016;94(6):548–555.
24. Inan S, Polat O, Ozcan S, Inan UU. Comparison of long-term automated retinal layer segmentation analysis of macula between silicone and gas tamponade after vitrectomy for rhegmatogenous retinal detachment. Ophthalmic Res. 2020. doi:10.1159/000506382
25. Scheerlinck LM, Schellekens PA, Liem AT, Steijns D, van Leeuwen R. Retinal sensitivity following intraocular silicone oil and gas tamponade for rhegmatogenous retinal detachment. Acta Ophthalmol. 2018;96(6):641–647. doi:10.1111/aos.13685
26. Purtskhvanidze K, Hillenkamp J, Tode J, et al. Thinning of inner retinal layers after vitrectomy with silicone oil versus gas endotamponade in eyes with macula-off retinal detachment. Ophthalmologica. 2017;238(3):124–132. doi:10.1159/000477743
27. Lee SH, Han JW, Byeon SH, et al. Retinal layer segmentation after silicone oil or gas tamponade for macula-on retinal detachment using optical coherence tomography. Retina. 2018;38(2):310–319. doi:10.1097/IAE.0000000000001533
28. Vaziri K, Schwartz SG, Kishor KS, Flynn HW
29. Garweg JG, Deiss M, Pfister IB, Gerhardt C. Impact of inner limiting membrane peeling on visual recovery after vitrectomy for primary rhegmatogenous retinal detachment involving the fovea. Retina. 2019;39(5):853–859. doi:10.1097/IAE.0000000000002046
30. Su J, Liu X, Zheng L, Hongpin C. Vitrectomy with internal limiting membrane peeling vs no peeling for Macular Hole-induced Retinal Detachment (MHRD): a meta-analysis. BMC Ophthalmol. 2015;15:62. doi:10.1186/s12886-015-0048-5
31. Hilton G, Machemer R, Michels R, Okun E, Schepens C, Schwartz A. The classification of retinal detachment with proliferative vitreoretinopathy. Ophthalmology. 1983;90(2):121–125. doi:10.1016/S0161-6420(83)34588-7
32. Halberstadt M, Domig D, Kodjikian L, Koerner F, Garweg JG. PVR recurrence and the timing of silicon oil removal. Klin Monbl Augenheilkd. 2006;223(5):361–366. doi:10.1055/s-2006-926594
33. Yu Y, Yue Y, Thong N, Zheng P, Liu W, An M. Anatomic outcomes and prognostic factors of vitrectomy in patients with primary rhegmatogenous retinal detachment associated with choroidal detachment. Curr Eye Res. 2019;44(3):329–333. doi:10.1080/02713683.2018.1540705
34. Falkner-Radler CI, Myung JS, Moussa S, et al. Trends in primary retinal detachment surgery: results of a Bicenter study. Retina. 2011;31(5):928–936. doi:10.1097/IAE.0b013e3181f2a2ad
35. Thompson JA, Snead MP, Billington BM, Barrie T, Thompson JR, Sparrow JM. National audit of the outcome of primary surgery for rhegmatogenous retinal detachments. II. Clinical outcomes. Eye. 2002;16(6):771–777. doi:10.1038/sj.eye.6700325
36. Heimann H, Zou X, Jandeck C, et al. Primary vitrectomy for rhegmatogenous retinal detachment: an analysis of 512 cases. Graefes Arch Clin Exp Ophthalmol. 2006;244(1):69–78. doi:10.1007/s00417-005-0026-3
37. Lumi X, Luznik Z, Petrovski G, Petrovski BE, Hawlina M. Anatomical success rate of pars plana vitrectomy for treatment of complex rhegmatogenous retinal detachment. BMC Ophthalmol. 2006;16(1):216. doi:10.1186/s12886-016-0390-2
38. Joussen AM, Rizzo S, Kirchhof B, et al. HSO -Study Group. Heavy silicone oil versus standard silicone oil in as vitreous tamponade in inferior PVR (HSO Study): interim analysis. Acta Ophthalmol. 2011;89(6):e483–9. doi:10.1111/j.1755-3768.2011.02139.x
39. Heimann H, Stappler T, Wong D. Heavy tamponade 1: a review of indications, use, and complications. Eye. 2008;22(10):1342–1359.
40. Garweg JG, Deiss M, Pfister IB, Gerhardt C. Reply. Retina. 2020;40(2):e8–e10.
41. Nam KY, Kim JY. Effect of internal limiting membrane peeling on the development of epiretinal membrane after pars plana vitrectomy for primary rhegmatogenous retinal detachment. Retina. 2015;35(5):880–885. doi:10.1097/IAE.0000000000000421
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
