Back to Journals » Patient Preference and Adherence » Volume 11
Impact of serum-derived bovine immunoglobulin/protein isolate therapy on irritable bowel syndrome and inflammatory bowel disease: a survey of patient perspective
Authors Shaw AL, Tomanelli A, Bradshaw TP, Petschow BW , Burnett BP
Received 16 February 2017
Accepted for publication 22 April 2017
Published 31 May 2017 Volume 2017:11 Pages 1001—1007
DOI https://doi.org/10.2147/PPA.S134792
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Audrey L Shaw,1 Adam Tomanelli,2 Timothy P Bradshaw,1 Bryon W Petschow,1 Bruce P Burnett3
1Clinical Research, Entera Health, Inc., Cary, NC, 2Market Research, Praxis Research Partners, Fairfield, CT, 3Medical Affairs, Entera Health, Inc., Cary, NC, USA
Background: Patients with irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD) commonly experience diarrhea, abdominal pain, bloating, and urgency. These symptoms significantly compromise the patient’s quality of life (QoL) by limiting participation in normal daily activities and adversely affect work productivity and performance.
Purpose: The aim of this study was to understand from the patient’s perspective how oral serum-derived bovine immunoglobulin/protein isolate (SBI) impacts bowel habits, management of condition, and basic QoL.
Methods: A 1-page questionnaire was distributed randomly to >14,000 patients who were prescribed SBI (EnteraGam®) for relevant intended uses. The survey was designed to collect data related to the influence of IBS or IBD on daily life activities and the impact of SBI usage on daily stool frequency, management of their condition, and QoL. Patient-reported responses were analyzed using a paired t-test to compare mean change in daily stool output and descriptive statistics for continuous variables.
Results: A total of 1,377 patients returned the surveys. Results from 595 surveys were analyzed with a focus on patients with IBS or IBD who had provided numeric responses regarding daily stool frequency. Respondents with IBS who reported having a normal stool frequency (≤4 stools per day) increased from 35% prior to using SBI to 91% while using SBI. A similar change toward normal stool frequency was reported by IBD respondents. Mean daily stool numbers decreased for respondents in the combined IBS and IBD groups (P=0.0001) from 6.5±4.3 before SBI to 2.6±1.9 following SBI use. The majority of respondents agreed strongly or very strongly that SBI helped them manage their condition (66.9%) and helped them return to the activities they enjoyed (59.1%).
Conclusion: Results from this patient survey suggest that SBI use can lead to clinically relevant decreases in daily stool frequency in patients with IBS or IBD along with improvements in the overall management of their condition and aspects of QoL.
Keywords: IBD, IBS, patient satisfaction, stool frequency, quality of life
Introduction
Irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) are both chronic and sometimes debilitating conditions of the gastrointestinal (GI) tract. IBS is a functional disorder of the GI system and currently affects ~35 million people, or 10%–11% of the population, in the US alone.1–3 Approximately 20%–22% of patients with IBS have symptoms characterized as diarrhea-predominant IBS (IBS-D) (frequent and loose stools, often with urgency).4 It has been reported that IBS symptoms interfere with productivity and performance on an average of 9 days per month and cause patients to completely miss school or work on an average of 2 days per month. Patients with IBS are often afraid to attend social events or even travel short distances out of concern for experiencing a sudden attack of diarrhea.3 While the exact etiology of IBS is not known, a number of possible etiologies have been proposed, including alterations in intestinal motility, food sensitivities, intestinal inflammation, altered barrier function, and dysbiosis of the intestinal microbiome.5
IBD is a condition that results from an inappropriate inflammatory response to intestinal microbes in a genetically susceptible host, creating characteristic GI and extraintestinal symptoms.1,6,7 This disease affects ~1.4 million people in the US, equivalent to ~0.5% of the population.1,5 While not completely understood, IBD is associated with onset at a young age and significantly influences social aspects of life, including the ability to work, undertake physical activity, and enjoy recreational activities.1 In a survey conducted in the European Union involving 5,576 patients with IBD, ~75% reported that symptoms affect their ability to enjoy leisure activities, while 68.9% felt symptoms affected their ability to perform at work.8
Serum-derived bovine immunoglobulin/protein isolate (SBI) is the primary ingredient in a novel Food and Drug Administration (FDA)-regulated medical food (EnteraGam®) intended for the dietary management of chronic loose and frequent stools.9 The active ingredient (ie, SBI) is a protein-enriched formulation that consists of ~60% immunoglobulins by weight, primarily in the form of immunoglobulin G (IgG). This immunoglobulin component in SBI has been shown to bind, in vitro, to a variety of breakdown components from microbes associated with GI disease. Following oral administration of SBI, such binding activity is expected to reduce the antigenic load of the lamina propria, which should, in turn, lead to an overall dampening of immune activation and, therefore, improvement in gut barrier function and overall GI health.10 The purpose of this survey was to gain a better understanding of the physician-directed use of SBI and its impact on the lives of patients, with particular attention to diarrhea as one of the major symptoms experienced by this patient population.
Methods
Between October 2015 and August 2016, patients who had been prescribed SBI (EnteraGam®) were mailed a 1-page survey, along with the product, by the specialty pharmacy responsible for filling the prescription. The survey was designed to collect protected and non-identifiable health information from the patient including medical information regarding their condition, the approximate length of time on SBI, and how their bowel habits and daily activities have changed because of therapy. Informed consent was obtained from all survey respondents who were included in the analysis. This market survey research using de-identified information is exempt from IRB review according to the US Department of Health & Human Services Office for Human Research Protection under 45 CFR 46.101 subpart A.
Responses to the following survey questions were analyzed:
- What is your diagnosis? IBS, IBD, or “other”
- When were you first diagnosed? Within the last year, 1–3 years ago, or more than 3 years ago.
- How many different drugs have you been on since you were diagnosed?
- When were you prescribed EnteraGam®? First prescription, within the past 6 months, or more than 6 months ago.
- What was the number of stools before SBI?
- What was the number of stools while on SBI?
In addition, a 6-point Likert scale (from Agree Very Strongly to Disagree Very Strongly) was used to score the following patient statements:
- My condition prevented me from doing things I enjoy.
- My condition prevented me from doing my job.
- EnteraGam® has helped manage my condition.
- EnteraGam® has allowed me to get back to doing activities I enjoy.
- I want to continue taking EnteraGam®.
The analysis of patient responses to questions about baseline characteristics, number of medications used to treat their condition since diagnosis, and timing of prescription for SBI was based on all qualifying respondents (n=1,065), defined as those who had a primary diagnosis of chronic diarrhea associated with conditions such as IBS, IBD, and HIV infection. Analysis of responses to questions on stool frequency was limited to respondents who 1) had been diagnosed specifically with IBS or IBD and 2) provided numeric responses to the stool frequency questions; respondents who provided no answer or descriptive data (eg, many, loose, etc.) were eliminated from analysis. Numeric answers to questions regarding stool frequency were used to calculate estimates and rank the percent change in stool frequency (<25%, 25%–50%, 50%–75%, >75%). A normal stool frequency for this patient population was defined as ≤4 stools per day based on previously published reports.11,12 The impact of SBI on stool frequency was also evaluated for the following subgroups: primary diagnosis (IBS or IBD), gender (male, female), age (<50 years, 50–64 years, 65–75 years, >75 years), and whether it was a new prescription for SBI or a refill prescription (ie, during the previous 6 months or ≥6 months).
Descriptive statistics were used to analyze responses to questions on continuous variables. Statistical testing included the following: Z-test (proportions between subgroups), t-test (mean between subgroups), and paired t-test (pre–post shifts within the same subgroup). P-values ≤0.05 were considered statistically significant.
Results
Survey respondents
A total of 14,262 surveys were distributed to patients, and a total of 1,377 (9.7%) returned answers to the survey questions. Of these, 1,065 were from respondents who indicated a diagnosis consistent with SBI prescribing directions (chronic diarrhea associated with IBS, IBD, etc.). Since SBI is prescribed mainly for IBS-D, it was assumed that most respondents who claimed IBS as their diagnosis had IBS-D. Some respondents provided incomplete or otherwise unusable responses to some of the survey questions (eg, descriptive rather than numeric answers to questions about stool frequency). Therefore, the results presented here are based on responses obtained from 595 patients who indicated a primary diagnosis of IBS (n=344) or IBD (n=251) and provided numeric answers to the questions about number of stools before and during SBI therapy.
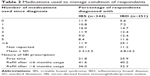
As shown in Table 1, the percentage of respondents was evenly distributed across age categories (<50 years, 50–64 years, 65–75 years, and >75 years). As a group, patients with a diagnosis of IBD were somewhat younger than those with IBS with the shift in mean age driven by the disparity in numbers in the “older than 75” age category. Significantly more surveys were received from females versus males (~3:1). Over half the patients responding indicated a primary diagnosis of IBS (57.8%), and nearly 50% of respondents had been diagnosed for their condition at least 3 years prior to completing the survey, regardless of whether they claimed IBS or IBD as their primary diagnosis (Table 2).
Medications prior to SBI
Prior to initiating SBI therapy, the mean number of medications used by respondents to help manage symptoms related to their condition was 3.3±3.5 for IBS patients and 4.8±4.2 for IBD patients (Table 2). Importantly, ~20% of IBS respondents and 36.7% of IBD respondents reported having tried 5 or more medications to help manage their symptoms prior to taking SBI. Similar numbers of IBS and IBD patients also reported having responded to the survey during the time they were receiving oral SBI as their first prescription or as a refill prescription, regardless of whether they had been taking SBI for <6 months or >6 months (Table 2).
Change in stool frequency among respondents
Patients diagnosed with either IBS or IBD reported a more normal stool pattern, defined as ≤4 stools per day,11,12 while using SBI when compared to stool patterns before use of SBI (Figure 1). While only 35% of IBS patients reported having 4 or less stools per day prior to starting SBI therapy, >90% of IBS patients reported a more normal stool frequency while using SBI. Respondents diagnosed with IBS reported a significant reduction in daily stool numbers (P=0.0001) from 5.7±3.7 before SBI to 2.3±1.8 following SBI use. Mean daily stool numbers also decreased for IBD patients (P=0.0001), ranging from 7.4±4.9 stools per day before SBI to 3.0±2.0 following SBI use. It is worth noting that nearly 1 in 3 IBS patients (32.8%) reported 7 or more stools per day before using SBI, compared to ~2% while on SBI therapy. Similarly, nearly 83% of patients diagnosed with IBD reported a normal stool pattern while taking SBI, compared to only 25% prior to using SBI. Almost half of IBD patients (48.6%) reported experiencing >7 stools per day before using SBI compared to only 6.4% patients during SBI therapy.
Change in stool frequency by age and gender
The survey also assessed whether age or gender had any impact on the reduction in stool frequency observed in IBS and IBD respondents. The overall decrease in daily stools associated with SBI use in the combined IBS and IBD group was comparable in males (89.0%; n=138) and females (87.0%; n=448) (data not shown). When comparing male and female patients in the combined IBS and IBD group, a higher percentage of female patients reported a 25%–50% decrease in stool frequency and a lower percentage reported a >75% decrease, although these differences did not reach statistical significance (data not shown).
In general, the overall decrease in stool frequency reported by respondents while taking SBI appeared to occur across various age subgroups (data not shown). Among those patients who experienced a decrease in stool frequency with SBI, the majority reported a 50% or greater decrease in daily stool output (<50 years: 69.4%; 50–64 years: 71.2%; 65–75 years: 75.7%; >75 years: 79.0%). Nearly 22% of respondents reported no impact of SBI on stool frequency (12.2% of respondents <50 years of age; 2.9% of respondents 50–64 years of age; 3.6% of respondents 65–75 years of age; 2.9% of respondents >75 years of age). Some patients reported an increase in stool frequency while taking SBI (<50 years of age, 8.8%; 51–64 years of age, 9.4%; 65–74 years of age, 4.2%; >75 years of age, 5.7%).
Stool frequency reduction according to time on SBI
Over 65% of respondents who claimed to be taking SBI for the first time (first prescription) reported a 50% or greater decrease in daily stool output, while 5.7% reported an increase in stool frequency, and 6.4% reported no impact (data not shown). Respondents who claimed to be taking SBI as a refill prescription reported a similar impact of SBI on stool frequency; a 50% or greater decrease in daily stool output was reported by 77.1% of respondents taking SBI for <6 months and 73.6% of respondents on SBI for ≥6 months. The percentage of respondents who reported no impact or an increase in stool frequency while taking SBI among patients taking SBI for <6 months was 5.3% and 5.3%, respectively. In contrast, 10.2% of respondents who had been taking SBI for >6 months reported an increase in stool frequency, while 5.9% reported no impact.
Patient perceptions regarding impact of condition and SBI on quality of life (QoL)
A summary of all IBS and IBD respondents’ (n=595) attitudes and perceptions regarding the impact of their disease condition on daily life activities is shown in Figure 2. Prior to using SBI, most patients felt strongly or very strongly (top 2 bars) that their condition prevented them from participating in the things they enjoyed (62.3%) and from doing their job (42.1%). A total of 525 (88.2%) respondents indicated “my condition prevented me from doing things I enjoy”, and 345 (58.0%) of them said that their condition prevented them from doing their job (Table 3). After receiving SBI treatment, 492 (93.7%) patients who had expressed “my condition prevented me from doing things I enjoy” (n=525) also reported that SBI “has allowed me to get back to doing activities I enjoy” and 509 (97.0%) reported that SBI “has helped me manage my condition”. Among those who indicated that their condition prevented them from doing their job (n=345), 337 (97.7%) reported that SBI “has allowed me to get back to doing activities I enjoy” and 326 (94.5%) reported that SBI “has helped me manage my condition”. Most patients agreed strongly or very strongly that SBI helped them manage their condition (66.9%) and return to doing the activities they enjoyed (59.1%) (Figure 3). Over 73% of patients (top 2 bars) reported that they desired to continue taking SBI. These positive perceptions of SBI use were consistent among all respondents, regardless of whether the patient was on their first SBI prescription or a refill prescription (data not shown).
Discussion
Treatment optimization and symptom control are of the utmost importance for the management of IBS and IBD. The objective of this survey was to better understand from the patient’s perspective how loose and watery stools, one of the hallmark symptoms reported for both IBS and IBD, impact the daily life activities of such patients and how SBI use impacts stool frequency and related aspects of patient’s QoL.
An important survey of IBS patients conducted by the American Gastroenterological Association (AGA) reported that a majority of IBS sufferers experience intestinal symptoms at least 4–6 days per week, and nearly 1 in 4 patients report an inability to accurately predict if they will experience symptoms on any given day.3 As a result, nearly one-third of IBS patients commonly avoid situations where a bathroom is not located nearby.3 Social and emotional impacts are also observed in patients with IBS.1,3 Improvements in symptoms among patients with IBS were small at 3 months after first-time gastroenterologic consultation and were not sustained at a 12-month follow-up.2,13 IBD is a chronic inflammatory condition of the intestinal tract that comprises 2 distinct disease states: ulcerative colitis (UC) and Crohn’s disease (CD). Patients with IBD commonly experience symptoms of bloody loose stools, abdominal pain, urgency, and fatigue.14,15 In addition to the physical component of the illness, patients with IBD have high rates of psychosocial problems such as embarrassment, depression, anger, and social isolation.1 Symptoms resulted in weekly impacts of QoL in 9.6% of patients with IBD.8 However, 76.0% of respondents reported that they were satisfied with the results obtained from their current medication, despite a similar proportion (75.6%) reporting that symptoms affect their ability to enjoy leisure activities. This suggests that many patients expect to adapt their lifestyles to allow for IBD. Furthermore, it suggests that patients may have low expectations of treatment for their condition.
Among the patients who responded to our survey, ~65% of IBS patients and nearly 75% of IBD patients reported an abnormal stool frequency, defined as 4 or more stools per day, because of their condition. Only 11% of patients in the combined IBS and IBD group of patients reported ≤2 stools per day prior to using SBI. These numbers are consistent with other reports on the incidence of loose and frequent stools in IBS and IBD patients.3,8 Importantly, nearly 90% of the 595 respondents with either IBS or IBD reported a more normalized stool frequency while using SBI. Over 72% of respondents in the combined IBS and IBD group of respondents reported a 50% or greater reduction in stool frequency, with mean stool frequency decreasing from 6.5±4.3 stools/day prior to SBI use to 2.6±1.9 stools/day while using SBI. While some differences were observed between patient subgroups (eg, gender, age, length of SBI use), 80% or more of the patients in each subgroup had decreased stools while using SBI. Importantly, the reduction in stool frequency is maintained over the long term, as patients who reported using SBI for ≥6 months reported comparable reductions in stool frequency to patients being treated for the first time and patients who had used SBI for <6 months.
Patients with IBS or IBD have also reported dissatisfaction with current treatment options. Less than 25% of patients with IBS judged themselves to be “very satisfied” overall with treatment they have received for their condition.3 A survey of 5,576 patients with IBD in the European Union reported that nearly 75% of respondents (n=4,213) felt that symptoms affected their ability to enjoy leisure activities and 68.9% felt symptoms affected their ability to perform at work. Approximately 75% were either very (40.0%) or somewhat (36.0%) satisfied with the results obtained from their current treatment medication.8 Our results found that most patients with IBS or IBD felt their condition prevented them doing the things they enjoyed (62.3%) and their job (42.1%). Furthermore, after using SBI most patients with IBS or IBD agreed strongly or very strongly that they could better manage their condition (66.9%) and get back to doing the activities they enjoyed (59.1%), with most patients (73.5%) reporting that they wish to continue taking SBI (EnteraGam®). It is worth noting that these results are consistent with those documented in the AGA survey of 3,254 patients with IBS-D,3 where 30% of diagnosed IBS-D patients reported to be “very satisfied” with EnteraGam® therapy for managing their symptoms. In summary, the long-term reduction in stool frequency observed with SBI therapy may also enable long-term improvements in QoL measures. These positive perceptions of SBI use were consistent and comparable to the results from all respondents, regardless of whether the patient was on their first SBI prescription, had used SBI for <6 months, or had used SBI for ≥6 months.
Certain limitations in this survey should be recognized when evaluating the results. First, the survey questions did not ask patients to distinguish between a diagnosis of IBS-D versus constipation-predominant IBS (IBS-C). However, EnteraGam® is primarily prescribed for IBS-D, so the authors feel that the vast majority of IBS respondents had symptoms characteristic of IBS-D. Second, nearly 75% of IBS respondents were taking SBI as a refill prescription, which may have resulted in more favorable ratings for impact on QoL compared to patients taking SBI for the first time. Third, nearly one-third of respondents had been taking SBI for >6 months, which may have impacted the accuracy of their recall about daily stool frequency prior to taking SBI.
In conclusion, data from this survey demonstrate that SBI use resulted in long-term, clinically relevant decreases in stool frequency in patients with IBS or IBD, with associated improvements in management of their condition, as well as productivity and enjoyment of their activities.
Acknowledgments
The authors thank Linda Gordon and James Martin for their role in the design and development of this survey project. The authors also thank Brooke Jackson for collection and data entry of patient surveys and Janice Gleavy for her contributions in the writing of this manuscript. Financial sources: this study was funded by Entera Health Inc., 2000 Regency Parkway, Suite 255, Cary, NC 27518, USA.
Author contributions
ALS and BPB also participated in the development and execution of this survey. ALS, BWP, and BPB supervised and managed the collection and analysis of data; AT conducted statistical analysis of data; ALS, TPB, BWP, and BPB analyzed and interpreted the data. BWP, TPB, and ALS also participated in writing and critical review of the manuscript for publication. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
ALS, TPB, BWP, and BPB are former employees of Entera Health, Inc. AT reports no conflicts of interest in this work.
References
Blagden S, Kingstone T, Soundy A, Lee R, Singh S, Roberts L. A comparative study of quality of life in persons with irritable bowel syndrome and inflammatory bowel disease. Gastroenterol Nurs. 2015;38(4):268–278. | ||
Canavan C, West J, Card T. The epidemiology of irritable bowel syndrome. Clin Epidemiol. 2014;6:71–80. | ||
IBS in America. 2016. Available from: http://www.multivu.com/players/English/7634451-aga-ibs-in-america-survey/docs/survey-findings-pdf-635473172.pdf. Accessed December 19, 2016. | ||
Hungin AP, Chang L, Locke GR, Dennis EH, Barghout V. Irritable bowel syndrome in the United States: prevalence, symptom patterns and impact. Aliment Pharmacol Ther. 2005;21(11):1365–1375. | ||
Chey WD, Kurlander J, Eswaran S. Irritable bowel syndrome: a clinical review. JAMA. 2015;313(9):949–958. | ||
Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009;361(21):2066–2078. | ||
World Gastroenterology Organization [webpage on the Internet]. World Gastroenterology Organisation Global Guidelines. 2015. Available from: http://www.worldgastroenterology.org/guidelines/global-guidelines/inflammatory-bowel-disease-ibd/inflammatory-bowel-disease-ibd-english. Accessed December 20, 2016. | ||
Ghosh S, Mitchell R. Impact of inflammatory bowel disease on quality of life: results of the European Federation of Crohn’s and Ulcerative Colitis Associations (EFCCA) patient survey. J Crohns Colitis. 2007;1(1):10–20. | ||
EnteraGam [Product Information Sheet]. Cary, NC: Entera Health, Inc; 2015. Available from: http://enteragam.com/assets/lib/EnteraGam_Product_Information.pdf. Accessed December 19, 2016. | ||
Petschow BW, Blikslager AT, Weaver EM, et al. Bovine immunoglobulin protein isolates for the nutritional management of enteropathy. World J Gastroenterol. 2014;20(33):11713–11726. | ||
Heaton KW, Radvan J, Cripps H, Mountford RA, Braddon FE, Hughes AO. Defecation frequency and timing, and stool form in the general population: a prospective study. Gut. 1992;33(6):818–824. | ||
Everhart JE, Go VL, Johannes RS, Fitzsimmons SC, Roth HP, White LR. A longitudinal survey of self-reported bowel habits in the United States. Dig Dis Sci. 1989;34(8):1153–1162. | ||
Canavan C, West J, Card T. Change in quality of life for patients with irritable bowel syndrome following referral to a gastroenterologist: a cohort study. PLoS One. 2015;10(10):e0139389. | ||
Danese S, Fiocchi C. Ulcerative colitis. N Engl J Med. 2011;365(18):1713–1725. | ||
Crohn’s and Colitis Foundation. The Facts About Inflammatory Bowel Disease. New York: Crohn’s and Colitis Foundation; 2014. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.