Back to Journals » Journal of Asthma and Allergy » Volume 15
Idiopathic Hypereosinophilia: A Multicenter Retrospective Analysis
Authors Rhyou HI , Lee SE, Kim MY, Park CS , Jo EJ, Choi GS, Nam YH
Received 7 September 2022
Accepted for publication 25 November 2022
Published 10 December 2022 Volume 2022:15 Pages 1763—1771
DOI https://doi.org/10.2147/JAA.S388341
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Luis Garcia-Marcos
Hyo In Rhyou,1 Seung Eun Lee,2 Mi-Yeong Kim,3 Chan Sun Park,4 Eun-Jung Jo,5 Gil Soon Choi,6 Young Hee Nam7
1Department of Internal Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Republic of Korea; 2Department of Internal Medicine, Pusan National University Yangsan Hospital, Yangsan, Republic of Korea; 3Department of Internal Medicine, Busan Paik Hospital, Inje University College of Medicine, Busan, Republic of Korea; 4Department of Internal Medicine, Inje University Haeundae Paik Hospital, Busan, Republic of Korea; 5Department of Internal Medicine, Pusan National University College of Medicine, Busan, Republic of Korea; 6Department of Internal Medicine, Kosin University College of Medicine, Busan, Republic of Korea; 7Department of Internal Medicine, Dong-A University College of Medicine, Busan, Republic of Korea
Correspondence: Young Hee Nam, Department of Internal Medicine, College of Medicine, Dong-A University, 26 Daesingongwon-ro, Seo-Gu, Busan, Republic of Korea, Tel +8251-240-5860, Fax +82-51-242-5864, Email [email protected]
Purpose: Physicians can sometimes encounter idiopathic hypereosinophilia (HE), but little is known about it. In this multicenter study, we analyzed the clinical characteristics, treatment, and outcomes of patients with idiopathic HE.
Patients and Methods: Patients diagnosed with idiopathic HE (idiopathic hypereosinophilic syndrome: iHES or hypereosinophilia with undetermined significance: HEus) at six tertiary hospitals between January 2010 and June 2021 were included in this retrospective observational study. Demographics, clinical and laboratory data, and treatment responses were obtained from the electronic medical records of the study subjects.
Results: A total of 73 patients with idiopathic HE (45 with iHES and 28 with HEus) were included in the present study. Overall, 12 (26.7%) and 5 (17.9%) were women, and mean age of patients at diagnosis was 51.84 ± 17.29 years and 60.21 ± 18.01 years in iHES and HEus groups, respectively. Forty-three (95.6%) patients of iHES and 15 (53.6%) patients of HEus received corticosteroids as 1st-line treatment. Treatment response to corticosteroids in patients with iHES was generally good: complete response (n=25, 58.1%), partial response (n=12, 27.9%), no response (n=6, 14.0%). Treatment response to corticosteroids in HEus was complete response (n=7, 46.7%), partial response (n=6, 40.0%), and no response (n=2, 13.3%). There were 13 patients (46.4%) with HEus who were not treated.
Conclusion: Corticosteroid treatment is generally effective and well tolerated by patients with iHES. Some patients with HEus are treated with corticosteroids in clinical practice. Extensive research is needed to establish a standardized management guidelines for iHES and determine whether treatment for HEus is required.
Keywords: idiopathic hypereosinophilia, idiopathic hypereosinophilic syndrome, hypereosinophilia of undetermined significance
Introduction
Hypereosinophilia (HE) is defined as a persistent elevation of peripheral blood eosinophil count to greater than 1.5 × 109/L. A variety of conditions can cause HE, but prolonged elevation can cause organ damage. A broad and complex diagnostic workup is required for HE to optimize treatment plans.1,2 Idiopathic HE is defined as persistent HE, which is excludes as a cause of reactive change or neoplasm. Idiopathic HE can be classified as either idiopathic hypereosinophilic syndrome (iHES) or hypereosinophilia with undetermined significance (HEus) depending on the presence of eosinophilic organ involvement.3 Clinical manifestations of iHES vary depending on the extent of organ damage, and the mainstay of treatment is corticosteroids.4,5 However, there are no standardized treatment guidelines and the clinical outcomes of iHES are not yet known. In addition, little is known about the treatment and prognosis of HEus. Therefore, the evaluation and management of idiopathic HE are performed differently, depending on expert opinions and institution-specific directives. This multicenter retrospective study aimed to analyze the clinical characteristics, treatment, and outcomes of patients with idiopathic HE.
Patients and Methods
Study Design and Subjects
We retrospectively analyzed patients diagnosed with iHES and HEus at six tertiary hospitals between January 2010 and June 2021. The study participants were recruited in two steps. First, patients diagnosed with iHES or HEus using the 8th version of the Korean Standard Classification of Diseases (KCD) codes were included. Second, it was confirmed through a chart review whether they met the diagnostic criteria. iHES is defined as a sustained peripheral eosinophil count of ≥1.5 × 109/L on two occasions in an interval of ≥1 month and end-organ damage without other causes of eosinophilia by the International Cooperative Working Group on Eosinophilic Disorders in 2012.6 HEus is defined as a sustained peripheral eosinophil count of ≥1.5 × 109/L and no end-organ damage, with no other cause of eosinophilia.6 Ninety patients who had been diagnosed with iHES or HEus were included in the present study. We excluded patients who were followed up within 6 months. Finally, 73 patients with iHES or HEus were included in the analysis: 45 and 28 patients had iHES and HEus, respectively.
Demographics, clinical and laboratory data, and treatment responses were obtained from the electronic medical records of the study subjects. Atopy was defined as a positive test for specific immunoglobulin (Ig)E (≥ 0.35 kU/L) to at least one allergen or a positive result on the allergen skin prick test with wheals of a mean diameter ≥ 3 mm for any allergen. Clinical manifestations related to tissue eosinophil infiltration are described at the initial presentation.
A complete blood count with differential count and serological studies including total IgE, vitamin B12, tryptase, eosinophil cationic protein (ECP), and parasite-specific IgG were confirmed. If active parasite infection had been not excluded in patients with elevated levels of parasite IgG, they took the anti-helminthic drugs. Patients with sustained hypereosinophilia after anti-parasite treatment were excluded “secondary hypereosinophilia” due to parasite infection.
Studies for the evaluation of organ damage were reviewed: chest computed tomography (CT), abdominal and pelvic CT (APCT), bone marrow (BM) examination, cytogenetic study, esophagogastroduodenoscopy (EGDS), colonoscopy (CFS), echocardiography, and pulmonary function test (PFT). Cytogenetic studies were conducted in the BM and/or peripheral blood, and included screening for rearrangements of PDGFRA, PDGFRB, FGFR1, BCR-ABL, and/or PCM1-JAK2.
The treatment response of patients with iHES was classified as complete response (CR), partial response (PR), or no response. CR was defined as a decrease in eosinophil count to within the normal range (0–0.5 × 109 /L) and improvement of symptoms and/or organ damage. PR was defined as a decrease in eosinophil count, but not to within the normal range, and an improvement in symptoms and/or organ damage. No response was defined as sustained HE and no improvement in symptoms or organ damage. In the treatment response of patients with HEus, CR was defined as a decrease in eosinophil count to within the normal range (0–0.5 × 109 /L), PR was a decrease in eosinophil count, but not to the normal range, and no response was a sustained HE. This study was approved by the Dong-A University Hospital Institutional Review Board (DAUHIRB-21-027), and informed consent was not necessary for this retrospective observational study according to the ethical guidelines of Dong-A university hospital. All personal data were protected and de-identified. Confidentiality and compliance with the Declaration of Helsinki was maintained.
Statistics Analysis
Statistical analyses were performed using IBM SPSS version 22 for Windows (IBM SPSS Inc., Chicago, Ill, USA). Categorical variables are described as frequencies and proportions, and continuous variables are presented as mean ± standard deviation and absolute numbers. To assess statistical significance, the Student’s t-test or Mann–Whitney U-test was used for continuous variables, and Fisher’s exact test was used for categorical variables. Multiple logistic regression analysis was used to identify the predictive factors for treatment response in patients with iHES. Statistical significance was set at P < 0.05.
Results
Demographic and Clinical Characteristics
Idiopathic Hypereosinophilic Syndrome
A total of 45 patients with iHES were included in this cohort. The demographic and clinical characteristics of patients are shown in Table 1. There were 12 female patients (26.7%), and mean age of study subjects at diagnosis was 51.84 ± 17.29 years. The time interval between symptom onset and diagnosis was 10.54 ± 28.67 months. Comorbidities of patients with iHES were as follows: malignancies (n=2; lung cancer and diffuse large B-cell lymphoma, respectively) and no autoimmune disease. The patient with lung cancer had been diagnosed idiopathic hypereosinophilia, and he had lung cancer 3 years later. The other patient with diffuse large B-cell lymphoma had achieved complete remission after chemotherapy when he was diagnosed with hypereosinophilia. Nineteen patients (42.2%) had atopy. Among them, all the patients with allergic disease had mild symptoms, or they were well controlled state. Thirty-two (71.1%) had clinical manifestations at initial presentation, while 12 patients showed no symptoms or signs aside from high eosinophil count. The most common manifestations were pulmonary (60%) and gastrointestinal (60%), and followed by cutaneous (48.9%), hematologic (44.4%), constitutional (22.2%), cardiac (13.3%), neurologic (13.3%), and rheumatologic (2.2%) symptoms (Table 2).
 |
Table 1 Demographic and Clinical Characteristics in Patients with Idiopathic HE |
 |
Table 2 Clinical Manifestations of Study Subjects at Initial Presentation |
Undetermined Significance Hypereosinophilia
A total of 28 patients with HEus were included in this study. There were 5 (17.9%) female patients, and the mean age at diagnosis was 60.21 ± 18.01 years (Table 1). Presence of comorbidities in the patients with HEus was as follows: malignancy (n=2, 7.1%) and autoimmune disease (n=1, 3.6%). Both two patients with malignancy had thyroid cancer. One had no evidence of disease after surgery when he was diagnosed with hypereosinophilia. The other one had thyroid cancer after 2 years later after the diagnosis of hypereosinophilia. Atopy was recorded in 9 patients (32.1%), and there was no patient with uncontrolled or partly controlled allergic disease. Five patients (17.9%) had clinical cutaneous manifestations, even if it was confirmed that they were not related to eosinophilic organ damage. Symptoms reported were: cutaneous (n=5, 17.9%), pulmonary (n=4, 14.3%), gastrointestinal (n=4, 14.3%), hematologic (n=4, 14.3%), rheumatologic (n=1, 3.6%), and neurologic (n=1, 3.6%) (Table 2).
Laboratory Data and Evaluation of Organ Damage
Idiopathic Hypereosinophilic Syndrome
The mean counts of initial white blood cells and eosinophils were 16.62 ± 8.91×109 /L and 7.53 ± 7.39×109 /L, respectively (Table 1). They increased to 19.89 ± 10.92×109 /L and 11.29 ± 8.68×109 /L during the study period. The mean serum levels of total IgE (1680.18 ± 2605.16 IU/mL), vitamin B12 (1054.08 ± 954.61 pg/mL), and ECP (142.64 ± 65.68 µg/L) were elevated. Fourteen out of 38 patients (36.8%) had high serum levels of parasite-specific IgG (data not shown).
Organ involvement was assessed using a variety of methods (Figure 1). The most commonly conducted studies were chest CT (n=40, 88.9%), followed by APCT (n=37, 82.2%), BM (n=31, 68.9%), cytogenetic study (n=31, 68.9%), echocardiography (n=20, 66.7%), PFT (n=27, 60%), EGDS (n=17, 37.8%), and CFS (n=10, 22.2%). The positive or abnormal test results were recorded as follows: APCT (n=28, 75.7%), chest CT (n=28, 70%), EGDS (n=11, 64.7%), PFT (n=9, 33.3%), BM (n=10, 32.3%), CFS (n=3, 30%), echocardiography (n=6, 20%), cytogenetic analysis (n=0).
Hypereosinophilia with Undetermined Significance
The mean initial whole blood counts and eosinophil counts were 11.48 ± 4.87×109 /L and 4.12 ± 3.88×109 /L, respectively (Table 1). They increased to 12.35 ± 6.20×109 /L and 7.02 ± 10.43×109 /L during the study period.
The most commonly conducted exams were chest CT (n=16, 57.1%), followed by APCT (n=15, 53.6%), echocardiography (n=13, 46.4%), cytogenetic studies (n=12, 42.9%), EGDS (n=12, 42.9%), BM (n=11, 39.3%), PFT (n=9, 32.1%), and CFS (n=7, 25.0%). The positivity of abnormal results in these exams were in 25.0% (4/16), 20.0% (3/15), 30.8% (4/13), 8.3% (1/12), 25.0% (3/12), 9.1% (1/11), 33.3% (3/9), 14.3% (1/7), respectively, although none of them confirmed eosinophilic organ involvement (Figure 1).
Treatment Response and Outcomes
Idiopathic Hypereosinophilic Syndrome
A total of 43 (95.6%) patients were treated for iHES with systemic corticosteroids as the 1st-line treatment. The mean dose of corticosteroids was 16.24 ± 28.49 mg/day of prednisolone (median, 10.00 mg/day of prednisolone), and the maximum dose was 104.25 ± 205.33 mg/day of prednisolone (median, 60.00 mg/day of prednisolone). The overall duration of corticosteroid treatment was 109.32 ± 143.97 weeks (median, 41.00 weeks). Thirty-seven patients (86.0%) showed CR (58.1%) or PR (27.9%), and six patients (14.0%) had no response to corticosteroid treatment (Figure 2). Four patients reported complications from corticosteroids; however, none of the patients discontinued the administration of corticosteroids due to adverse reactions.
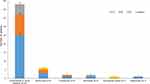 |
Figure 2 Treatment response of patients with iHES. Abbreviations: iHES, idiopathic hypereosinophilic syndrome; CR, complete response; PR, partial response. |
Nine patients received 2nd-line treatment in the form of hydroxyurea (n=5), cyclosporine (n=2), biologics (n=2), or mycophenolate mofetil (n=1). Two patients were treated with hydroxyurea and methotrexate as 3rd-line treatment, respectively. The treatment response to hydroxyurea was generally good: CR (n=3), PR (n=2), and unknown (n=1) (Figure 2).
Two patients treated with cyclosporine also showed good treatment response: CR (n=1) and PR (n=1). Two patients treated with reslizumab showed CR and no response. The treatment response to methotrexate was CR, while the response to mycophenolate mofetil was unknown. None of the patients had complications from 2nd- or 3rd-line treatment, except for one patient who experienced decreased renal function due to cyclosporine. Two patients with iHES did not receive any treatment and their outcomes were not confirmed.
Overall treatment duration of patients with iHES was 109.32 ± 143.97 weeks (median, 41.00 weeks), and follow up duration was 53.26 ± 67.33 months (median, 42.00 months).
Hypereosinophilia with Undetermined Significance
A total of 15 (53.6%) patients were treated for HEus with systemic corticosteroids as the 1st-line treatment. The mean dose of corticosteroids was 9.80 ± 4.37 mg/day of prednisolone (median, 9.76 mg/day of prednisolone), and the maximal dose was 37.20 ± 24.46 mg/day of prednisolone (median, 30.00 mg/day of prednisolone). The overall duration of corticosteroid treatment was 85.46 ± 127.90 weeks (median, 16.00 weeks). Thirteen patients (86.7%) showed CR (n=7, 46.7%), PR (n=6, 40.0%), and 2 patients (13.3%) had no response to corticosteroid treatment (Figure 3). Two patients received 2nd-line treatment with hydroxyurea and methotrexate. Neither had a response to the 2nd-line treatment. There were 13 patients (46.4%) with HEus who were not treated. Blood eosinophil counts were restored to the normal range in two, decreased but were higher than the normal range in two, and remained persistently high in two patients. The clinical outcome was unknown in seven patients. Overall duration of treatment of patients with HEus was 44.42 ± 101.42 weeks (median, 2.00 weeks), and follow up duration was 28.90 ± 33.19 months (median, 11.50 months).
 |
Figure 3 Treatment response of patients with HEus. Abbreviations: HEus, hypereosinophilia with undetermined significance; CR, complete response; PR, partial response. |
Predictive Factors for Good Treatment Response in Idiopathic Hypereosinophilic Syndrome
The predictive factors for CR to treatment in patients with iHES were identified using multiple logistic regression analysis (Table 3). Number of involved organs (odds ratio [ORs] 1.861, 95% confidence interval [CI] 1.016–3.409, P=0.044) and initial platelet count (0.993, 0.987–0.999, P=0.034) were significantly associated with CR to treatment in iHES by univariate logistic regression. Multivariate logistic regression revealed that only the number of involved organs (4.395, 1.033–18.699, P=0.045) was significantly associated with CR to treatment in iHES.
 |
Table 3 Predictive Factors of Complete Response to Treatment in Patients with iHES |
Discussion
IHES is a rare disorder with several clinical manifestations.4,7,8 However, the epidemiology, clinical characteristics, and outcomes of iHES are unknown, and the evaluation and management of iHES can vary among different institutions and/or physicians.9 In the current study, a total of 73 patients from six tertiary hospitals were included. We focused on idiopathic HE, unlike previous studies, that were performed on heterogeneous populations of HE. HES is known to predominantly affect males,10,11 as was also found in this study. iHES tends to occur in adults aged between 20 and 50,10,11 and our study population reflects this, with the mean age of patients at diagnosis with iHES being 51 years. In addition, little is known about the clinical manifestations and outcomes of HEus.12 A recent retrospective study of 40 patients with HEus suggested that it was more common in women,12 but our study reported a significant predominance of HEus in men. The age at diagnosis of HEus was reported to be middle-age in both this and the previous studies. Further studies are required to determine the clinical characteristics of patients with HEus.
Patients with clinical manifestations at initial presentation were common in the iHES group. Pulmonary and gastrointestinal symptoms were the most common, followed by cutaneous, hematologic, constitutional, cardiac, neurologic, and rheumatological manifestations. The most large-scale retrospective study of 188 patients with HES demonstrated that cutaneous and pulmonary presentations were the most common; however, variant subtypes of HES were included in the study.13 A recent retrospective study of iHES that included 33 study subjects reported that splenomegaly and cardiac manifestations were the most common.14 The authors stated that a particular clinical subspecialty, referral bias, and area of expertise could affect discrepancies between studies. Additionally, nearly one-third of patients with iHES in the current study did not experience any symptoms. Patients with HEus are defined by unexplained persistent asymptomatic HE,6 but five patients with HEus complained of symptoms at initial examination, although it was confirmed that there was no eosinophilic organ involvement, and they were not related to blood eosinophilia. Therefore, the clinical manifestations of patients with eosinophilia can present in a variety of ways, regardless of eosinophilic organ involvement. In the HEus group, there was no significant difference in the blood eosinophil counts regardless of the presence of clinical manifestations. No patient in the HEus group was not identified newly developed organ involvement during the study period. However, little is known about the prognosis of patients with HEus with clinical manifestations. Whether they will develop iHES in the future needs to be closely and continuously monitored.
Most patients underwent chest and abdominopelvic CT scans, but many patients did not undergo echocardiography, PFT, BM, or cytogenetic studies. In addition, serum vitamin B12 and ECP levels were not assessed in most patients. Evaluation of patients with HE has not been fully conducted in clinical practice. It is difficult in real clinical practice to conduct multiple tests on patients with suspected HES, but the workup for patients with suspected idiopathic HE should be more extensive.
Corticosteroids are the mainstay of iHES management,5,15 and all patients who received treatment were administered corticosteroids as a 1st-line treatment in the present study. However, standards for the duration and dosage of corticosteroid therapy have not yet been established for iHES, and recommendations usually vary depending on clinical manifestations, comorbidities, and expert experience. The median maximal and maintenance doses of prednisolone reported in a multicenter retrospective study of 188 patients with hypereosinophilic syndrome (HES) were 40 mg/day and 10 mg/day, respectively.13 A study of 33 patients with iHES demonstrated that the median starting dose of prednisolone is 30 mg/day.14 The dosing of corticosteroids used in the present study was similar to that used in previous studies. However, the duration of corticosteroid treatment has been reported vary widely in both the present and in previous studies.12,14 Treatment response to corticosteroids is generally good.13,14 In the present study, the treatment response to corticosteroids was good and well-tolerated. However, there were differences in study subjects and the time period for evaluating treatment response among previous studies. No other hematologic abnormalities were identified in patients who did not respond clinically to steroid treatment during the study period. However, it is necessary to continue tracking them in the future.
Hydroxyurea is a cytotoxic agent that reduces eosinophil counts and has been used to treat corticosteroid-resistant HES.5,15 Hydroxyurea was the most commonly used agent for 2nd-line treatment in the present study, and the median dose and treatment response were reported to be similar to those of previous studies.13,14 Hydroxyurea treatment seemed to be effective and well tolerated, although the number of study subjects was too small to draw further conclusions. Generally, hydroxyurea is not applied as a monotherapy, and it is used as a corticosteroid sparing and maintenance agent. Other secondary treatments, such as cyclosporine, biologics, and methotrexate, were administered in the present study, but there was little data to analyze the dosing, duration, and response to treatment. The efficacy and safety of these steroid-sparing agents for the treatment of iHES should be further investigated.
Predictive factors for worse outcomes of HES are male sex, degree of eosinophilia, cardiac disease, association with myeloproliferative syndrome, and lack of response to corticosteroids.9,16 However, those of iHES are not yet known. We analyzed the predictive factors of CR to corticosteroids in patients with iHES and found that only the number of involved organs was significantly associated with a good response to corticosteroid treatment. iHES patients with multiple organ involvement can be considered for intense corticosteroid treatment, which may lead to good outcomes for patients with iHES. Dose of corticosteroids (including mean daily dose and maximal daily dose) and steroid treatment duration were not significantly associated with outcomes of iHES by multivariate analysis, but patients with multiple organ infiltration (3 or more) showed a tendency to receive high dose of maximal corticosteroid. (data are not shown). In addition, there were no cases of treatment discontinuation due to the adverse effects of corticosteroids. When iHES is diagnosed, prompt and intensive corticosteroid treatment is required.
Generally, patients with HEus should be closely followed without treatment.3 No clear recommendations regarding the treatment of HEus are mentioned in the current guidelines.9,12 Patients with moderate to high blood eosinophilia and/or risk of end-organ damage were reportedly treated with corticosteroids in a previous study on 40 patients with HEus.12 There were 21 patients (52%) who were treated with corticosteroids, and all treated patients maintained CR during treatment period. However, in the present study, there was no significant difference in blood eosinophil count between patients who were treated and those who were not (all patients with moderate to high blood eosinophilia), and the prescription pattern of treatment for HEus varied among physicians. The treatment response to corticosteroids was good and well tolerated. However, the necessity for corticosteroid treatment must be confirmed, and physicians must carefully consider the initiation of corticosteroids because of their risks.
The present study has some limitations. First, this was a retrospective, observational study. All authors were involved in double-checking the diagnosis of patients with idiopathic HE using the KCD-8 and a detailed chart review. Therefore, only patients with confirmed diagnoses of idiopathic HE were included in the present study. Second, we had a small sample size; however, to the best of our knowledge, it is the largest sample of patients with iHES studied to date. A large-scale prospective study is recommended to confirm and validate our results. Third, the timing of the assessment of the treatment response was not uniform. Overall, we assessed the treatment response during the treatment period, and re-assessment was performed when the medication was changed or added. However, it was meaningful to observe the overall treatment response of patients with iHES in real-world clinical practice.
Conclusion
In summary, patients with iHES should be more thoroughly examined regardless of the presence of clinical manifestations. The treatment response to corticosteroids was generally good and well tolerated in patients with iHES, and prompt and intense corticosteroid treatment may ensure better outcomes for patients with iHES. However, standardized guidelines are required in the future. Treatment of patients with HEus is generally not recommended; however, some patients with HEus have been treated with corticosteroids in clinical practice. Further research is necessary to determine whether treatment is required.
Abbreviations
HE, hypereosinophilia; iHES, idiopathic hypereosinophilic syndrome; HEus, hypereosinophilia with undetermined significance; KCD, Korean Standard Classification of Diseases; Ig, immunoglobulin; ECP, eosinophil cationic protein; CT, computed tomography; APCT, abdominal and pelvic computed tomography; BM, bone marrow; EGDS, esophagogastroduodenoscopy; CFS, colonoscopy; PFT, pulmonary function test; CR, complete response; PR, partial response; OR, odds ratio; CI, confidence interval; HES, hypereosinophilic syndrome.
Funding
This work was supported by the Dong-A University research fund.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wang SA. The diagnostic work-up of hypereosinophilia. Pathobiology. 2019;86(1):39–52. doi:10.1159/000489341
2. Roufosse F, Weller PF. Practical approach to the patient with hypereosinophilia. J Allergy Clin Immunol. 2010;126(1):39–44. doi:10.1016/j.jaci.2010.04.011
3. Kahn JE, Groh M, Lefévre G. (A critical appraisal of) classification of hypereosinophilic disorders. Front Med. 2017;4:216. doi:10.3389/fmed.2017.00216
4. Shdid RA, Azrieh B, Alebbi S, Mansour S, Naeem M. Idiopathic hypereosinophilic syndrome with multiple organ involvement. Case Rep Oncol. 2021;14(1):249–255. doi:10.1159/000511396
5. Klion AD. How I treat hypereosinophilic syndromes. Blood. 2015;126(9):1069–1077. doi:10.1182/blood-2014-11-551614
6. Valent P, Klion AD, Horny H-P, et al. Contemporary consensus proposal on criteria and classification of eosinophilic disorders and related syndromes. J Allergy Clin Immunol. 2012;130(3):607–612. doi:10.1016/j.jaci.2012.02.019
7. Mahajan VK, Singh R, Mehta KS, et al. Idiopathic hypereosinophilic syndrome: a rare cause of erythroderma. J Dermatol Case Rep. 2014;8(4):108–114. doi:10.3315/jdcr.2014.1185
8. Wu P, Chen Y, Zhang H, Li C. Idiopathic hypereosinophilic syndrome presenting with multiple organ damage. Medicine. 2019;98(10):e14532. doi:10.1097/MD.0000000000014532
9. Leru PM. Eosinophilic disorders: evaluation of current classification and diagnostic criteria, proposal of a practical diagnostic algorithm. Leru Clin Transl Allergy. 2019;9:36. doi:10.1186/s13601-019-0277-4
10. Roufosse FE, Goldman M, Cogan E. Hypereosinophilic syndromes. Orphanet J Rare Dis. 2007;2(1):37. doi:10.1186/1750-1172-2-37
11. Weller PF, Bubley GJ. The idiopathic hypereosinophilic syndrome. Blood. 1994;83(10):2759–2779. doi:10.1182/blood.V83.10.2759.2759
12. Helbig G, Hus M, Francuz T, Dziaczkowska-Suszek J, Soja A, Kyrcz-Krzemień S. Characteristics and clinical outcome of patients with hypereosinophilia of undetermined significance. Med Oncol. 2014;31(1):815. doi:10.1007/s12032-013-0815-1
13. Ogbogu PU, Bochner BS, Butterfield JH, et al. Hypereosinophilic syndromes: a multicenter, retrospective analysis of clinical characteristics and response to therapy. J Allergy Clin Immunol. 2009;124(6):1319–25.e3. doi:10.1016/j.jaci.2009.09.022
14. Helbig G, Wiśniewska-Piąty K, Francuz T, Dziaczkowska-Suszek J, Kyrcz-Krzemień S. Diversity of clinical manifestations and response to corticosteroids for idiopathic hypereosinophilic syndrome: retrospective study in 33 patients. Leuk Lymphoma. 2013;54(4):807–811. doi:10.3109/10428194.2012.731602
15. Butt NM, Lambert J, Ali S, et al. Guideline for the investigation and management of eosinophilia. Br J Haematol. 2017;176(4):553–572. doi:10.1111/bjh.14488
16. Shomali W, Gotlib J. World Health Organization-defined eosinophilic disorders: 2019 update on diagnosis, risk stratification, and management. Am J Hematol. 2019;94(10):1149–1167. doi:10.1002/ajh.25617
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

