Back to Journals » Hepatic Medicine: Evidence and Research » Volume 13
Identifying Patients at High Risk of Developing Non-Cirrhotic Portal Hypertension
Authors Gioia S, Riggio O, Nardelli S, d'Amati G, Ridola L
Received 4 August 2021
Accepted for publication 27 October 2021
Published 3 November 2021 Volume 2021:13 Pages 105—111
DOI https://doi.org/10.2147/HMER.S282674
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Gerry Lake-Bakaar
Stefania Gioia,1 Oliviero Riggio,1 Silvia Nardelli,1 Giulia d’Amati,2 Lorenzo Ridola1
1Department of Translational and Precision Medicine, Sapienza University of Rome, Rome, Italy; 2Department of Radiological, Oncological, and Pathological Sciences, Sapienza University of Rome, Rome, Italy
Correspondence: Stefania Gioia
Department of Translational and Precision Medicine, Sapienza University of Rome, Rome, Italy
Tel +39 06 49970463
Email [email protected]
Abstract: The term porto-sinusoidal vascular disease (PSVD) has been recently proposed to replace the term idiopathic non-cirrhotic portal hypertension (INCPH) to describe patients with or without signs of portal hypertension and typical histological lesions involving the portal venules or sinusoids in the absence of cirrhosis. According to the new definition, the presence of known causes of liver disease as well as of portal vein thrombosis does not rule out PSVD. Therefore, the patients in whom the diagnosis of PSVD is possible are much more than the patients strictly fulfilling the diagnostic criteria for INCPH. In this setting, the clinical challenge for the hepatologist is to identify patients at risk of developing PSVD and to indicate liver biopsy to confirm the diagnosis. We describe some possible scenarios in which PSVD should always be suspected, and we provide some tools useful to reach the diagnosis of PSVD.
Keywords: porto-sinusoidal vascular liver disease, idiopathic non-cirrhotic portal hypertension, portal vein thrombosis, portal hypertension
Introduction
For so far, various nomenclatures as “non-cirrhotic portal fibrosis”, “idiopathic portal hypertension,” “hepatoportal sclerosis” have been used to refer to patients with portal hypertension occurring in the absence of cirrhosis or other causes of portal hypertension, depending on the geographical area, on the apparent clinical or histological aspect of the disease.1–3 Due to this heterogeneity in the denomination and in part to the lack of awareness among clinicians, this condition remained largely under-recognized especially in the western world.
More recently, the term “idiopathic non-cirrhotic portal hypertension” (INCPH) was proposed4 by a consensus of experts who have the great merit of having introduced a common nomenclature and diagnostic criteria: essentially, the presence of an unexplained portal hypertension and the absence of cirrhosis in liver histology.
With the increase in the awareness and the observation of new cases, it became clear the term “idiopathic non-cirrhotic portal hypertension” was unsatisfactory. In fact, a number of INCPH were apparently associated to other diseases (such as immunodeficiency) or to the use of drugs, and thus, not so “idiopathic”.4 More importantly, histological signs observable in patients with INCPH could also be observed in patients without signs of portal hypertension, making portal hypertension not a mandatory feature of the disease.5,6 Finally, a diagnosis based on exclusion criteria4,7 such as the absence of cirrhosis but also the absence of all the potential causes of cirrhosis (HCV positivity, fatty liver, autoimmunity, etc.) may lead to an exclusion “by definition” of patients affected by a potential cause of chronic liver disease actually not evolved to a stage able to cause portal hypertension. For example, in a patient with varices and HCV positivity without significant fibrosis the signs of portal hypertension remain unexplained.
Recently, in order to overcome those difficulties and to reach a uniformity in the nomenclature, the term Porto-Sinusoidal Vascular Disease (PSVD) has been proposed by the European Association for the Vascular Liver Disease (VALDIG)8 to describe a new entity identifiable according to “positive” diagnostic criteria and not only by “exclusion” criteria. In fact, the new diagnostic criteria define the diagnosis of PSVD in presence of one of the three following features:
i) at least one specific sign of portal hypertension (gastroesophageal or ectopic varices, porto-systemic collaterals, bleeding due to portal hypertension) and the absence of cirrhosis at an adequate liver biopsy (a biopsy is considered adequate when it is ≥20 mm long, with ≥10 portal tracts, and not too fragmented);
ii) at least one specific histological sign of PSVD (obliterative portal venopathy, nodular regenerative hyperplasia, incomplete septal fibrosis or cirrhosis) and absence of cirrhosis at an adequate liver biopsy (this criterion allowed the inclusion of patients without signs of portal hypertension);
iii) at least one non-specific sign of portal hypertension (ascites, low platelets, splenomegaly) at an adequate liver biopsy and in addition to at least one non-specific histological sign of PSVD (portal tract abnormalities: multiplication, dilation of arteries, periportal vascular channels, and aberrant vessels; architectural disturbance: irregular distribution of the portal tracts and central veins; non-zonal sinusoidal dilation; mild perisinusoidal fibrosis) and to the absence of cirrhosis.
As a consequence, the patients in whom the diagnosis of PSVD is possible, according to the new criteria, are much more than the patients strictly fulfilling the diagnostic criteria for INCPH. In Table 1 is reported the comparison between the exclusion criteria for the diagnosis of INCPH and PSVD. A recent paper showed that with the new diagnostic criteria, the histological lesions and their distribution were similar in the group of patients fulfilling the diagnostic criteria for PSVD and in the subgroup of patients strictly fulfilling the definition of INCPH, indicating that both groups are affected by the same disease.9
 |
Table 1 Comparison Between Exclusion Criteria of INCPH Proposed by Schouten et al4 and of PSVD Proposed by VALDIG8 |
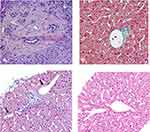
It should be noted that PSVD still must be distinguished from other diseases causing portal hypertension, such as schistosomiasis, Budd Chiari Syndrome, portal vein cavernoma, sarcoidosis, and so on.8 The specific and unspecific histological signs of PSVD can also help on this point. In Figure 1, some of the typical histological lesions of PSVD are shown.
From the above consideration, it is clear that liver biopsy is an essential tool for the diagnosis of PSVD. In fact, a biopsy-based diagnosis is mandatory in patients with clear (specific) signs of portal hypertension in order to exclude the presence of cirrhosis and in the patients without portal hypertension or with nonspecific signs of portal hypertension (for example, a splenomegaly, which may have a number of other possible causes) in order to demonstrate the histological signs of PSVD. Even if essential, liver biopsy may also have some limitations related to the nature of the disease itself. The fact that in PSVD the lesions are not always all present in the same patient and that they are focally distributed in the liver may reduce the possibility of reaching diagnosis. This makes necessary the execution of an adequate liver biopsy with a specimen the longer possible and containing the highest possible number of portal tracts to increase the possibility of including and then identifying one of the typical lesions.
When to Suspect PSVD?
As a consequence, the clinical challenge for the hepatologist is to suspect PSVD and to indicate liver biopsy to confirm the diagnosis.
Below we describe five possible scenarios in which PSVD should always be suspected.
Patient with Gastro-Esophageal Varices, Portal Hypertensive Bleeding, Porto-Systemic Collaterals
At least for epidemiological reasons, the first diagnostic hypothesis in front of this kind of patient should be liver cirrhosis. Reasons to suspect diseases other than cirrhosis could be based on the absence of well-established aetiological factors for chronic liver disease (ie, HCV or HBV positivity, steatohepatitis, alcohol intake, etc) and/or on the discrepancy between the evident signs of portal hypertension and a mild hepatocellular damage. With the new criteria, the identification of an aetiological factor potentially causing cirrhosis does not exclude the possibility of a diagnosis of PSVD. Thus, the suspicion of a portal hypertension not due to a cirrhosis but eventually to a PSVD is now mainly based on the second criterion: the discrepancy between portal hypertension and the mild liver damage. However, in practice, the distinction between a compensated cirrhosis (Child-Pugh class A) and PSVD may be difficult. For example, as previously shown,10 by comparing liver function and particularly the hepatic protein synthetic capacity in patients with “cryptogenic compensated cirrhosis” and in those affected by histologically proven idiopathic non-cirrhotic portal hypertension, although the mean level of albumin was lower in patients with cirrhosis, only 25% of them had albumin below the normal value (3.5 mg/dl) and the remaining cirrhotic patients were indistinguishable from the patients without cirrhosis from this point of view. On the other hand, even if less frequent, signs of hepatic decompensation may also be present in patients with PSVD. Ascites is described in up to 30% of patients11 and hepatic encephalopathy, even if infrequent, is a possible complication of the disease;12 a mild grade of hepatocellular dysfunction is reported too.13–15
To facilitate the distinction between PSVD and cirrhosis, imaging techniques may be helpful. By comparing the abdominal CT-scans or MRI of cirrhotic and PSVD patients, Kang16 showed that liver surface nodularity was more typical of patients with cirrhosis than in the PSVD group (89.2%) as well as the caudate lobe hypertrophy and atrophy of segment IV. However, all these radiological characteristics can also be seen in the patients with PSVD, making the distinction difficult in a given individual patient.
Hepatic vein catheterisation may also play a potential diagnostic role being the hepatic venous pressure gradient (HVPG)17 significantly lower in PSVD patients than in cirrhotic patients. However, a large overlap between cirrhosis and PSVD exists. Moreover, HVPG determination is not available in all centers, and more importantly, the reliability of such determination in a disease in which the portal hypertension is typically pre-sinusoidal is arguable. Probably, a low HVPG supports the diagnosis of PSVD.
The best diagnostic tool is probably liver stiffness, based on the fact that liver fibrosis is much more pronounced in cirrhotic patients than in non-cirrhotic portal hypertension. Elkrief et al18 identified thresholds for liver stiffness measurement (LSM) by transient elastography useful for routine clinical practice. In patients with signs of portal hypertension, LSM by transient elastography (Fibroscan) below 10 kPa strongly suggests PSVD; therefore, a biopsy should be performed to fully establish this diagnosis. Conversely, when LSM is above 20 kPa, the probability of PSVD is very low.
Moreover, due to the evident discrepancy between portal hypertension and liver fibrosis in PSVD, spleen stiffness may be useful to rule out cirrhosis. Furuichi et al investigated the diagnostic role of liver and spleen stiffness in patients with non-cirrhotic and cirrhotic portal hypertension and chronic non-cirrhotic hepatitis, showing that the median values of spleen stiffness and of the spleen/liver stiffness ratio were higher in patients with PSVD than in cirrhotics.19 Whereas the spleen/liver stiffness ratio decreased with the progression of the pathology from chronic non-cirrhotic hepatitis to cirrhosis, it increased instead in the PSVD group suggesting that it is a disease in which the spleen becomes markedly stiffer than the liver. However, more studies are needed to explore the diagnostic role of spleen stiffness and its clinical applications.
Patients with Splenomegaly and Thrombocytopenia
A second clinical scenario in which PSVD should be suspected is in patients with splenomegaly, defined as spleen size ≥13 cm in the largest axis, and platelet count <150,000 per μL. Usually, these patients are initially evaluated by a haematologist and submitted to a complete haematological diagnostic work-out, including an osteomedullary biopsy. In case of negativity of the above-mentioned investigations, they are then typically referred to as hepatologists. At this point, a liver biopsy showing positive and specific signs of PSVD is mandatory to confirm the diagnosis in these patients with nonspecific signs of portal hypertension.
However, it should be noted that the prevalence of myeloproliferative neoplasm is considerable in patients affected by PSVD.20 In two European series, a myeloproliferative disease was identified, respectively, in 8% and 17% of patients with INCPH.11,21 The problem is therefore that a patient with splenomegaly and hypersplenism in whom a haematological disorder is identified as the possible cause of these alterations is probably not always referred to a hepatologist with the consequent risk of missing the diagnosis of PSVD.
Patients with Chronic and Unexplained Alteration of Liver Enzymes
It has been reported that the histological lesions usually observed in patients affected by PSVD with portal hypertension may be present in the liver biopsies of patients without portal hypertension.5,6 Guido et al,5 by reviewing 482 liver biopsies from patients with chronic ALT/AST elevation without cirrhosis and portal hypertension, described histological alterations similar to those observed in patients with idiopathic non-cirrhotic portal hypertension in 94 patients (19%). Interestingly, in this series, some patients were affected by diseases known to be associated with INCPH, such as autoimmune disorders and prothrombotic disorders. These observations were confirmed by a more recent study by Wöran9 showing that among PSVD patients 9% had specific histological signs of PSVD but no clinical signs of portal hypertension.
This kind of population is very interesting and is still a matter of investigation. Future studies are necessary to define the natural history, the possible development of signs of portal hypertension (esophageal varices, ascites, etc.) and its incidence, the development of liver nodules or hepatic decompensation. As previously described, some patients developed signs of portal hypertension during follow-up.5 In the study by Woran, the clinical course of patients with specific clinical signs of portal hypertension (n=49) was compared with those of patients with only unspecific clinical signs or no clinical signs (n=34) and it was observed that while patients with specific signs of portal hypertension had a cumulative incidence of hepatic decompensation at 3 years of 11.2%, no patient with only unspecific or no clinical signs experienced hepatic decompensation at 3 years (log-rank p=0.002).9
Finally, these observations suggest first that PSVD should be suspected and actively searched for among the patients with chronic liver test abnormalities of unknown aetiology even in the absence of signs of portal hypertension. If PSVD without portal hypertension may represent an “early” pre-symptomatic stage of PSVD, with portal hypertension is still to be clarified. Certainly, attempts to standardize the nomenclature can favour and facilitate collaborative studies that explore this condition.
Patients with Extrahepatic Diseases Known to Be Associated to PSVD
A positive implication of the change in the denomination of the disease from idiopathic non-cirrhotic portal hypertension to porto-sinusoidal vascular liver disease is the abolition of the adjective “idiopathic”. In fact, it has been reported that more than half of PSVD patients have an associated disease.4,10,22 PSVD is frequently associated with several systemic conditions and with the chronic exposure to various drugs and toxins (Table 2) that may play a direct role in the pathophysiology of the liver alterations. In this setting, the role of the hepatologist is to make the other specialists following the patients affected by these diseases or exposed to these drugs aware of the coexistence with PSVD or of the possibility to develop it during follow-up. Thus, they should actively search at least for the specific and non-specific signs of portal hypertension and unexplained alterations of liver tests. When one of these alterations is present, the patient should be referred to a hepatologist.
 |
Table 2 Conditions Associated with Porto-Sinusoidal Vascular Disease |
Patients with Portal Vein Thrombosis
With new insights into the natural history of PSVD and its physiopathology, it is known that PSVD is frequently complicated by extra-hepatic portal vein thrombosis.11,22 This event occurs in 30–40% of patients, with an incidence much higher than in patients with cirrhosis.8,22 A high incidence of thrombosis is sustained, but there is a strong association between PSVD, prothrombotic conditions and the slowing down of the blood flow in the portal vein axis secondary to portal hypertension. Thus, it could be assumed that a patient with non-cirrhotic portal vein thrombosis (PVT) may be actually affected by a pre-existing PSVD. Since the criteria for the patency of the portal vein have been eliminated in the last definition of PSVD, the presence of a pre-existing, undiagnosed PSVD should be suspected in any patient with PVT.
The importance of not missing a diagnosis of a pre-existing PSVD, especially in patients with recent PVT, has important therapeutic implications. In a patient with a recent PVT without an identified provoking factor, anticoagulant treatment is often stopped once the PVT is resolved. However, in the patients with PVT secondary to PSVD the slowing down of portal flow is a persistent condition lasting after the resolution of the PVT and the withdrawal of anticoagulation could lead to the recurrence of thrombosis, and a long-term anticoagulant probably should be recommended.23,24
However, if a patient is observed after PVT occurs, it may be very hard to determine if there is a pre-existing PSVD. In these cases, imaging techniques may be helpful. HVPG and liver stiffness have been shown to be lower in patients with non-cirrhotic PVT than in patients with INCPH.17 Even if the diagnostic gold standard for PSVD is liver biopsy, in this case it may be doubtful if histology is actually the best tool to identify PSVD in patients with PVT. The histological distinction between intrahepatic portal vein obstruction like in PSVD and an extrahepatic portal vein obstruction as in PVT is not completely defined.
Conclusion
In conclusion, the diagnosis of PSVD based on liver biopsy and a common unique nomenclature provide diagnostic criteria essential for future collaborative studies in order to investigate and define the characteristics and the natural history of this new entity. PSVD should be actively searched for both in patients with liver disease and in patients with extrahepatic associated conditions. As a consequence, PSVD may be less infrequent than is currently reported.
Abbreviations
PSVD, porto sinusoidal vascular liver disease; PVT, portal vein thrombosis; NCPH, non-cirrhotic portal hypertension; INCPH, idiopathic non-cirrhotic portal hypertension; OPV, obliterative portal venopathy; LSM, liver stiffness measurement; CT, computed tomography; AST, aspartate aminotransferase; ALT, alanine aminotransferase.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No financial support.
Disclosure
The authors declare that no conflict of interest exists concerning this paper.
References
1. Valla DC, Cazals-Hatem D. Vascular liver diseases on the clinical side: definitions and diagnosis, new concepts. Virchows Arch. 2018;473(1):3–13. doi:10.1007/s00428-018-2331-3
2. Basu AK, Boyer J, Bhattacharya R, Basu Mallick KC, Sen Gupta LP. Non-cirrhotic portal fibrosis with portal hypertension: a new syndrome. I. Clinical and function studies and result of operations. II. Histopathological studies. Indian J Med Res. 1967;55(4):336–339.
3. Mikkelsen WP, Edmondson HA, Peters RL, Redeker AG, Reynolds TB. Extra- and intra-hepatic portal hypertension without cirrhosis (hepatoportal sclerosis). Ann Surg. 1965;162(4):602–620. doi:10.1097/00000658-196510000-00006
4. Schouten JNL, Garcia-Pagan JC, Valla DC, Janssen HLA. Idiopathic noncirrhotic portal hypertension. Hepatology. 2011;54:1071–1081. doi:10.1002/hep.24422
5. Guido M, Sarcognato S, Sonzogni A, et al. Obliterative portal venopathy without portal hypertension: an underestimated condition. Liver Int. 2016;36(3):454–460. doi:10.1111/liv.12936
6. Cazals-Hatem D, Hillaire S, Rudler M, et al. Obliterative portal venopathy: portal hypertension is not always present at diagnosis. J Hepatol. 2011;54(3):455–461. doi:10.1016/j.jhep.2010.07.038
7. European Association for The Study of the Liver. EASL clinical practice guidelines: vascular diseases of the liver. J Hepatol. 2016;64(1):179–202. doi:10.1016/j.jhep.2015.07.040
8. De Gottardi A, Rautou PE, Schouten J. Porto-sinusoidal vascular disease: proposal and description of a novel entity. Lancet Gastroenterol Hepatol. 2019;4(5):399–411. doi:10.1016/S2468-1253(19)30047-0
9. Wöran K, Semmler G, Jachs M, et al. Clinical course of porto-sinusoidal vascular disease is distinct from idiopathic noncirrhotic portal hypertension. Clin Gastroenterol Hepatol. 2020;
10. Riggio O, Gioia S, Pentassuglio I, Nicoletti V, Valente M, d’Amati G. Idiopathic noncirrhotic portal hypertension: current perspectives. Hepat Med. 2016;8:81–88. doi:10.2147/HMER.S85544
11. Gioia S, Nardelli S, Pasquale C, et al. Natural history of patients with non‐cirrhotic portal hypertension: comparison with patients with compensated cirrhosis. Dig Liver Dis. 2018;50(8):839–844. doi:10.1016/j.dld.2018.01.132
12. Nicoletti V, Gioia S, Riggio O, et al. Hepatic encephalopathy in patients with non-cirrhotic portal hypertension: description, prevalence and risk factors. Dig Liv Dis. 2016;48(9):1072–1077. doi:10.1016/j.dld.2016.06.014
13. Krasinskas AM, Eghtesad B, Kamath PS, Demetris AJ, Abraham SC. Liver transplantation for severe intrahepatic noncirrhotic portal hypertension. Liver Transpl. 2005;11:621. doi:10.1002/lt.20431
14. Dumortier J, Bizollon T, Scoazec JY, et al. Orthotopic liver transplantation for idiopathic portal hypertension: indications and outcome. Scand J Gastroenterol. 2001;36:417–422. doi:10.1080/003655201300051298
15. Schouten JN, Nevens F, Hansen B, et al. Idiopathic noncirrhotic portal hypertension is associated with poor survival: results of a long-term cohort study. Aliment Pharmacol Ther. 2012;35:1424–1433. doi:10.1111/j.1365-2036.2012.05112.x
16. Kang JH, Kim DH, Kim SY, et al. Porto-sinusoidal vascular disease with portal hypertension versus liver cirrhosis: differences in imaging features on CT and hepatobiliary contrast-enhanced MRI. Abdom Radiol (NY). 2021;46(5):1891–1903. doi:10.1007/s00261-020-02831-w
17. Seijo S, Reverter E, Miquel R, et al. Role of hepatic vein catheterisation and transient elastography in the diagnosis of idiopathic portal hypertension. Dig Liver Dis. 2012;44(10):855–860. doi:10.1016/j.dld.2012.05.005
18. Elkrief L, Lazareth M, Chevret S, et al.; ANRS CO12 CirVir Group. Liver stiffness by transient elastography to detect porto-sinusoidal vascular liver disease with portal hypertension. Hepatology. 2021;74(1):364–378. doi:10.1002/hep.31688
19. Furuichi Y, Moriyasu F, Taira J, et al. Noninvasive diagnostic method for idiopathic portal hypertension based on measurements of liver and spleen stiffness by ARFI elastography. J Gastroenterol. 2013;48(9):1061–1068. doi:10.1007/s00535-012-0703-z
20. Alvarez-Larrán A, Abraldes JG, Cervantes F, et al. Portal hypertension secondary to myelofibrosis: a study of three cases. Am J Gastroenterol. 2005;100(10):2355–2358. doi:10.1111/j.1572-0241.2005.50374.x
21. Hillaire S, Bonte E, Denninger MH, et al. Idiopathic non-cirrhotic intrahepatic portal hypertension in the West: a re-evaluation in 28 patients. Gut. 2002;51(2):275–280. doi:10.1136/gut.51.2.275
22. Siramolpiwat S, Seijo S, Miquel R, et al. Idiopathic portal hypertension: natural history and long-term outcome. Hepatology. 2014;59:2276–2285. doi:10.1002/hep.26904
23. Gioia S, Nardelli S, Ridola L, d’Amati G, Riggio O. Is porto sinusoidal vascular disease to be actively searched in patients with portal vein thrombosis? World J Hepatol. 2019;11(8):613–618. doi:10.4254/wjh.v11.i8.613
24. Hernández-Gea V, Baiges A, Turon F, Garcia-Pagán JC. Idiopathic portal hypertension. Hepatology. 2018;68(6):2413–2423. doi:10.1002/hep.30132
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.