Back to Journals » Therapeutics and Clinical Risk Management » Volume 12
Human von Willebrand factor/factor VIII concentrates in the management of pediatric patients with von Willebrand disease/hemophilia A
Authors Castaman G, Linari S
Received 22 December 2015
Accepted for publication 2 May 2016
Published 30 June 2016 Volume 2016:12 Pages 1029—1037
DOI https://doi.org/10.2147/TCRM.S87543
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Giancarlo Castaman, Silvia Linari
Department of Oncology, Center for Bleeding Disorders, Careggi University Hospital, Florence, Italy
Abstract: Several plasma-derived intermediate and high-purity concentrates containing von Willebrand factor (VWF) and factor VIII (FVIII) are currently available. The main role of these products in the management of pediatric the population is represented by the replacement therapy in patients with severe or intermediate forms of von Willebrand disease, in whom other treatments are ineffective or contraindicated. Another important role of VWF/FVIII concentrates in children may be their use in immune tolerance induction (ITI) protocols. ITI is particularly recommended for hemophilia A children who have developed an inhibitor against FVIII, currently the most serious complication of substitutive treatment in hemophilia. Although recombinant concentrates may represent the preferred option in children with hemophilia A, VWF/FVIII concentrates may offer an advantage in rescuing patients who failed previous ITI.
Keywords: von Willebrand factor, factor VIII, plasma-derived concentrates, children, von Willebrand disease, hemophilia A
Introduction
Several plasma-derived intermediate and high-purity concentrates containing von Willebrand factor (VWF) and factor VIII (FVIII) are available. VWF is a large multimeric adhesive plasma glycoprotein, composed of a series of dimers of mature subunits, that has an essential role in both primary and secondary hemostasis.1 Biosynthesis of VWF is restricted to megakaryocytes and endothelial cells.2,3 Its primary function is to promote platelet adhesion to subendothelium exposed by vascular injury. VWF also cooperates with fibrinogen in platelet–platelet interactions, promoting thrombus growth and stabilization. A second critical role for VWF is to act as the carrier protein for coagulation FVIII in plasma, protecting it from early proteolytic degradation.4,5 This pleiotropic function of VWF can be evaluated using different laboratory assays because no single test covers the entire spectrum of VWF activities (Table 1). The deficiency or abnormality of VWF causes von Willebrand disease (VWD), the most frequent autosomal inherited bleeding disorder in humans. FVIII is crucial for coagulation, and its deficiency causes hemophilia A (HA), an X-linked bleeding disorder characterized by a life-long bleeding disorder whose severity is closely associated with the severity of FVIII deficiency in plasma.
  | Table 1 Laboratory assays for VWF activities16 |
The aim of the present review is to highlight the current role of human VWF/FVIII concentrates in the management of pediatric patients with VWD and HA.
Current human VWF/FVIII concentrates
Different human VWF/FVIII products are available for replacement therapy. These concentrates were initially introduced in clinical practice for the treatment of HA. All currently available VWF/FVIII concentrates are plasma derived; however, very recently, a recombinant VWF concentrate (vonicog alfa; BAX 111, licensed under the trade name Vonvendi; Baxalta US Inc., Westlake Village, CA, USA) has been approved by Food and Drug Administration (US FDA) in December 2015 for on-demand treatment and control of bleeding episodes in adults with VWD.6,7 Plasma-derived concentrate production depends on plasma donor availability, and despite viral screening and virucidal methods developed to minimize such concerns, the theoretical risk of blood-borne infection transmission cannot be excluded.8 Several procedures contribute to the viral safety of plasma-derived concentrates, including the quarantine of plasma undergoing industrial fractionation and obtained from regular well-surveyed donors and the introduction of nucleic acid amplification testing for five viruses (HIV 1–2, HBV (hepatitis B virus), HCV (hepatitis C virus), hepatitis A virus, and parvovirus B19). Furthermore, virucidal or removal techniques such as dry heating, pasteurization, vapor and solvent/detergent procedures, and ultrafiltration and nanofiltration steps contribute further to guarantee the safety of the final plasma-derived products. All coagulation factor concentrates are subjected to different methods of viral inactivation, attenuation, or elimination. Actually, plasma-derived concentrates maintain a high safety profile. However, vaccination against hepatitis B and A viruses should be offered to candidates for replacement treatment, if not already done through health programs.9
VWF/FVIII concentrates show a variable VWF and FVIII content and a heterogeneous multimer pattern (Table 2).10 However, the concentration of functional VWF may vary significantly, as supported by the wide difference in VWF:ristocetin cofactor (RCo)/VWF:antigen (Ag) ratio. Also, the ratio of VWF activity to FVIII:C content varies and this results in significantly different levels of the two proteins achieved post-infusion. Nowadays, most concentrates are labeled for their FVIII and VWF:RCo content, and appropriate and hemostatically safe replacement treatment can be planned.11,12 VWF concentrates differ with regard to production techniques, so that the retention or loss of high molecular weight (HMW) VWF may vary broadly.10 It has already been suggested that HMW VWF multimers represent the most adhesive functional forms of VWF, so that a HMW-containing VWF concentrate would theoretically provide more hemostatic efficacy.
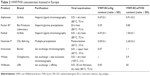  | Table 2 VWF/FVIII concentrates licensed in Europe |
The current indications for VWF/FVIII concentrates in children are replacement therapy in VWD and immune tolerance induction (ITI) therapy in HA with inhibitors.
Human VWF/FVIII concentrates in the management of pediatric patients with VWD
VWD is the most frequent inherited bleeding disorder, reaching a prevalence of ~1 % in pediatric populations.13 However, clinically relevant cases referred to specialized centers have a tenfold lower prevalence.14 The disorder is caused by the quantitative and/or qualitative abnormalities of VWF and is mainly transmitted in an autosomal dominant manner. VWD is a very heterogeneous disease and is classified into three main types according to quantitative (type 1 and 3) or qualitative (type 2A, 2B, 2M, and 2N) VWF abnormalities (Table 3).15,16 Type 1 is the most common form of VWD; it is characterized by an equivalent mild to moderately severe reduction in plasma of both VWF:Ag and VWF:RCo. VWF is functionally normal, as also demonstrated by the presence of all plasma VWF multimers, albeit at a reduced concentration, and plasma levels of FVIII are usually reduced in proportion to VWF. Type 2A is inherited mainly as a dominant trait and is the most frequent qualitative defect of VWF. The laboratory hallmark is a low VWF:RCo/VWF:Ag ratio (<0.6), associated with lack of large and often also of intermediate size VWF multimers, and ristocetin-induced platelet aggregation is severely reduced. Heightened ristocetin-induced platelet aggregation, occurring at ristocetin concentration lower than in normal controls, with mild to moderate thrombocytopenia, mildly reduced to normal FVIII and VWF:Ag, reduced VWF:RCo, and absence of the HMW multimers in plasma are peculiar features of typical type 2B cases, similarly inherited in a dominant manner with high penetrance. In this type, platelet function abnormality may be also present.15 In type 2M VWD, VWF multimer distribution is normal, but platelet-dependent VWF activities (VWF:RCo and von Willebrand factor collagen binding activity [VWF:CB]) are disproportionally reduced compared to VWF:Ag. Type 2N is recessively inherited, and patients show normal levels of VWF:Ag and VWF:RCo and a normal multimer pattern. Low plasma levels of FVIII:C (typically 5–40 U/dL) result from the increased clearance of this moiety as a consequence of mutations occurring in the VWF region, which reduce binding of FVIII. Type 3 VWD is rare and recessively inherited. It is characterized by severe bleeding tendency, very low VWF levels (usually <3 U/dL), and FVIII:C reduction similar to what is observed in moderate HA (typically 1–5 U/dL).
  | Table 3 Classification of von Willebrand disease |
The diagnosis of VWD is based on the triad including the presence of a bleeding history, preferably collected through standardized questionnaires, evidence of bleeding tendency in other family members, and reduced VWF:RCo levels in plasma (<40 U/dL). Further characterization of VWD type requires the measurement of VWF:Ag and FVIII:C and the analysis of multimer pattern.16,17 VWF levels below 30 U/dL are associated with a more significant clinical severity18 and with the likelihood of finding causative mutations in VWF gene, mapped at chromosome 12p13.2.19 Therefore, the severity of bleeding tendency is usually proportional to the degree of the primary deficiency of VWF and to that of secondary deficiency of FVIII. Mucocutaneous bleeding (easy bruising, epistaxis especially in children, menorrhagia) is frequently reported, often impairing the quality of life and requiring iron treatment for chronic anemia. Since FVIII is usually only mildly reduced, hemarthrosis and deep muscle hematoma, typical of severe clotting deficiency, are rare apart from type 3 VWD, in which bleeding episodes resemble those of moderate hemophilia. Gastrointestinal bleeding in older patients may be particularly frequent and difficult to manage, especially in patients with type 2 lacking HMW multimers in plasma.20 Bleeding after dental extraction is the most frequent postoperative bleeding manifestation, whereas bleeding after surgery may occur in more severely affected type 1 and 3 VWD patients. Since FVIII/VWF levels are usually normalized at the end of pregnancy in mild type 1 cases, replacement therapy postpartum to prevent immediate or delayed bleeding is required in females with type 2A, 2B, and 3 VWD.
The aim of therapy in VWD is to correct the dual defect of hemostasis, ie, the abnormal platelet adhesion–aggregation caused by low or dysfunctional VWF and the abnormal intrinsic coagulation owing to low FVIII levels. Two main therapeutic options are available: desmopressin (DDAVP [1-deamino-8-D-arginine-vasopressin]), which releases endogenous VWF from endothelial cells, and exogenous VWF contained in VWF/FVIII concentrates. DDAVP is an analog of the antidiuretic hormone vasopressin, V2 agonist.21 The drug is free of risk of viral transmission and inexpensive. DDAVP raises circulating FVIII and VWF levels by three- to fivefold over the patient’s baseline level by stimulating the release of FVIII/VWF from the storage sites in the vascular endothelial cells. DDAVP is the first-choice treatment for patients with type 1 VWD and baseline VWF and FVIII levels higher than 10 U/dL, provided a normal content of VWF in storage compartments.22 Variable responses are observed in type 2A and 2M, but typically VWF:RCo is hardly corrected in these types. In type 2B, thrombocytopenia may occur or aggravate because an abnormal VWF with enhanced affinity for platelet GPIb is released leading to an increased risk of bleeding and thus the compound is generally contraindicated.23 Patients with type 3 VWD do not respond to DDAVP because of the lack of VWF in storage compartments. DDAVP can be administered intravenously, subcutaneously, or intranasally. DDAVP can be given prior to surgical procedures or for the treatment of acute spontaneous or traumatic bleeding events. DDAVP can be administered every 12–24 hours, but when repeated doses are administered at closely-spaced intervals tachyphylaxis often ensues because of the depletion of VWF/FVIII from the stores. Flushing and mild increase of blood pressure are relatively frequent minor side effects, while retention of free water may induce hyponatremia, especially in infants less than 2 years of age, thus precipitating the onset of seizures. Therefore, close monitoring of these subjects with fluid restriction and serum sodium levels is advised. The occasional episodes of arterial thrombosis during treatment have never been reported in pediatric patients, and DDAVP is best avoided in adults with overt cardiovascular diseases.
When DDAVP is ineffective or contraindicated, replacement therapy with VWF/FVIII concentrates is the treatment of choice to restore VWF and FVIII levels. All these concentrates maintain similar hemostatic efficacy and show similar pharmacokinetics.24–29 However, the VWF/FVIII concentrate Haemate® P (CSL Behring, King of Prussia, PA, USA) has been widely used in patients with VWD for its particularly high VWF content (VWF:RCo/FVIII ratio 2.5).30 After infusion, the half-life of FVIII:C is approximately twice that of VWF:Ag (20–24 vs 10–14 hours) because of the endogenous increase of FVIII, which is stabilized by providing exogenous VWF.31 Replacement of VWF to achieve hemostatically adequate plasma levels for prevention or treatment of acute bleeding is the mainstay of treatment when DDAVP cannot be used. Spontaneous or posttraumatic bleeding should be treated promptly and surgery should be planned to prevent bleeding complications. There are a large number of expert and national guidelines or recommendations for VWD treatment, and although there are similarities in some recommendations, notable differences may exist in practice and the suggestions mentioned in Table 4 may be used to guide treatment.16 According to the severity of bleeding episode, a single or daily doses for 2–3 days of 20–50 IU/kg of VWF:RCo are indicated to treat spontaneous or posttraumatic bleeding episodes or prior to invasive procedures in patients with severe VWF deficiency (VWF:RCo levels at baseline below 10 U/dL). For major surgery, the aim is to maintain FVIII plasma level at ~80–100 U/dL for at least 2 days and through level above 50 U/dL for additional 5–7 days. A loading dose of 50 IU/kg of VWF:RCo is usually administered 30–60 minutes before surgery, and similar doses should be given for the next 2 days. After infusion there is an accumulation of FVIII, which is exogenously infused but also normally produced in VWD patients and stabilized by the infused VWF. This may result in a very high plasma FVIII:C concentration when repeated infusions are given, especially to cover major surgery.32 There is some concern that sustained high levels of post-infusion FVIII:C may be associated with episodes of deep vein thrombosis in adult VWD patients,33,34 but no such cases have been reported in pediatric patients. To guarantee appropriate and safe doses, FVIII:C plasma level should be measured daily to avoid levels greater than 150 U/dL, which is roughly recognized as a the threshold for an increased risk of venous thromboembolism.35 Treatment may also be monitored with VWF:RCo assays. Alternatively, a product containing high dose of VWF and very little FVIII (Wilfactin®; LFB, Les Ulis, France) can be used. However, with this product, post-infusion FVIII:C levels increase slowly with the peak being reached after 6–8 hours. Thus, coadministration of a priming dose of FVIII may be required if prompt hemostasis is needed in patients with baseline FVIII:C levels ≤30 U/dL.36 Plasma-derived concentrates containing VWF are contraindicated in some type 3 VWD patients with homozygous gene deletions or nonsense mutations who develop precipitating alloantibodies causing life-threatening anaphylactic reactions.37 Recombinant activated factor VII or recombinant FVIII concentrates free of VWF administered by continuous intravenous infusion have been successfully used in these patients.38,39
  | Table 4 Suggestions for replacement therapy in VWD16 |
A human recombinant VWF, vonicog alfa, synthesized by a genetically engineered CHO cell line, has been developed to avoid the risks associated with the use of plasma-derived VWF.6 Vonicog alfa (BAX 111) has been approved by FDA in December 2015 for on-demand treatment and control of bleeding episodes in adults with VWD.6,7 Further clinical trials are ongoing to assess its safety and efficacy in the pediatric population and for prophylaxis.
At variance with what is commonly observed in hemophilia, long-term prophylaxis is rarely used in VWD because of the greater phenotypic heterogeneity. The bleeding pattern is usually milder than in severe hemophilia and irreversible sequelae are not as common. However, some patients with type 3 VWD and FVIII:C levels <10 U/dL may suffer from frequent hemarthrosis, with development of target joints and chronic arthropathy, or recurrent spontaneous gastrointestinal bleeding, often without evidence of grossly anatomical lesions. Pediatric patients can also experience epistaxis frequently and severe enough to cause anemia. Secondary long-term prophylaxis may be useful in these patients, and indeed sporadic clinical experience with secondary long-term prophylaxis in VWD has been successful in case series, although using heterogeneous schedules of administration.40–42 Unfortunately, as for hemophilia patients, the impact on already established joint damage is limited and thus prophylaxis for joint bleeding in children with VWD should be started as soon as possible to attenuate the risk of late joint complications. However, prospective trials are needed to better evaluate the cost-effectiveness of this approach and the impact on patient’s quality of life in comparison with on-demand therapy.
Human VWF/FVIII concentrates in the management of pediatric patients with HA
HA is an X-linked recessive bleeding disorder caused by mutations in the gene encoding coagulation FVIII. Patients with FVIII plasma levels <1 U/dL are classified as severe hemophiliacs,43 and they usually suffer from recurrent musculoskeletal bleeding, particularly joint bleeding, as the hallmark of disease. Primary prophylaxis is the regular continuous treatment initiated in the absence of documented osteochondral joint disease and started before the second clinically evident large joint bleeding and the age of 3 years44 and currently represents the primary goal of FVIII replacement therapy.45 Primary prophylaxis is the regimen of choice for the treatment of children with severe hemophilia, with the aim of achieving FVIII levels always >1–2 U/dL with infusion of 25–40 IU/kg concentrates three times per week on non-consecutive days or every other day. According to different national guidelines and the Italian Association of Haemophilia Centres (AICE, Associazione Italiana Centri Emofilia) recommendations,46 recombinant FVIII concentrates represent the product of choice in children. The development of IgG alloantibodies (inhibitors) directed against FVIII, neutralizing its activity by a rapid clearance of infused FVIII and resulting in a marked reduction or absence of efficacy, is nowadays the most serious complication of treatment with clotting factor concentrates in HA. Inhibitors make replacement therapy ineffective. As a consequence the patients cannot continue prophylaxis, with an increased risk of mortality, morbidity, and disability. The incidence of inhibitor is around 30 % of severe cases and usually the risk is the greatest during the first 10–15 days of exposure. Since replacement treatment starts early in severe hemophilia, the vast majority of inhibitors occur in pediatric patients, quickly reaching this threshold. The inhibitor risk is significantly reduced in patients with severe HA exposed to FVIII for more than 50–150 days. At variance with these figures, the incidence is ~10% only in patients with mild or moderate HA and the risk increases with increasing exposure days so that these patients are mostly adults.47 The pathogenesis of inhibitors is multifactorial and not fully understood, although several risk factors have been identified. Both genetic factors (ie, F8 mutations, family history of inhibitors, ethnicity, polymorphisms of immune response genes, human leukocyte antigen, and FVIII haplotypes) and environmental factors (ie, age at first FVIII exposure, intensive FVIII treatment, surgery, and prophylaxis) have been implicated.48,49 A lower incidence of inhibitors has been recently reported in patients treated with plasma-derived FVIII products compared to those treated with recombinant FVIII, suggesting that the source of FVIII and/or the content of VWF may influence inhibitor development in previously untreated patients.50–53 Treatment of patients with inhibitors may be difficult, and management of bleeding must be undertaken by a specialized well-experienced center. Accurate measurement of inhibitor titer is mandatory since the choice of treatment product is based on titer of inhibitors, and patients with a low-responding inhibitor (<5 Bethesda Units [BU]) may still be treated with specific factor replacement at much higher doses to neutralize the antibody and to provide the required hemostatic FVIII level. On the other hand, patients with high-responding inhibitors (>5 BU) accompanied by brisk anamnesis must be treated with non-containing bypassing agents such as recombinant activated factor VII or activated prothrombin complex concentrates.54,55 The eradication of inhibitors by ITI protocols should be the primary aim in patients with a high-responding inhibitor, especially children, to restore the efficacy of FVIII replacement treatment.56 The main candidates for ITI are children with recent-onset high-responding inhibitors, possibly when titers <10 BU/mL are measured. ITI therapy using daily administration of high FVIII doses (usually 100–200 U/kg/day in children), sometimes in combination with immunomodulatory or immunosuppressive drugs, is the only strategy that has been shown to achieve long-lasting antigen-specific tolerance.57,58 The overall success rate for ITI in severe HA is ~60%–70%, but the ideal treatment regimen remains still debated and a variety of approaches have been adopted after the original protocol (Bonn protocol) suggesting the usefulness of very high daily doses of FVIII.59 Several key issues in ITI remain unresolved, and the current practice is largely influenced by individual clinician preferences at each hemophilia center as well as by published guidelines.60–62 The possibility that the type of FVIII product used for ITI could influence the likelihood of successful tolerization is the subject of intense debate.63 In particular, it has been postulated that VWF/FVIII concentrates may improve the ITI success rate in some patients with inhibitors, especially those with the following poor prognostic characteristics: a historical peak inhibitor level >200 BU/mL, an inhibitor level >10 BU/mL at the start of ITI, age >5 years, or gap of >24 months between inhibitor detection and start of ITI.63–67
In vitro experimental data and animal studies suggest that VWF decreases potential FVIII immunogenicity by epitope masking and protection from endocytosis by dendritic cells.68,69 Thus, increasing plasma concentration of VWF could decrease the amount of FVIII (antigen) presented to T lymphocytes, thereby reducing T-cell activation. The immunoprotective effect of VWF on FVIII may consequently have a positive impact on ITI. Published studies on efficacy and safety of primary and rescue ITI using human VWF/FVIII concentrates are largely retrospective70–73 and show a very favorable outcome for the cohort of patients undergoing first ITI and those with rescue ITI. The RITS-FITNHES Study,64 the REScue Immune Tolerance Study (RESIST),74,75 and the multicenter PRospectIve Observational Study of Plasma-derived FVIII/VWF in Immune Tolerance Induction (PRISM) Registry76 prospectively evaluated the use of VWF/FVIII concentrates in ITI, in addition to the International Immune Tolerance Study.57 However, in children undergoing ITI for the first time, in keeping with expert recommendations, the same product associated with inhibitor development should be preferred.46,60,61,77 Alternatively, another recombinant product with similar characteristics could be proposed, using human VWF/FVIII concentrates, in children with a previous ITI failure.
Conclusion
The VWF/FVIII concentrates play a key role in the management of pediatric patients. They are the treatment of choice for patients with type 3 and type 2B VWD and severe/intermediate patients in whom desmopressin does not work or is contraindicated. Replacement therapy is also required for VWD patients responsive to desmopressin undergoing major surgery and procedures with high bleeding risk, or for those in whom even minor bleeding should be avoided (eg, neurosurgery). Although recombinant concentrates may represent the treatment of choice in children with HA, the VWF/FVIII concentrates may offer an advantage in the success of previously failed ITI with recombinant FVIII.
Disclosure
The authors report no conflicts of interest in this work.
References
Yee A, Kretz CA. Von Willebrand factor: form for function. Seminar Thromb Hemost. 2014;40:17–27. | ||
Wagner DD, Marder VJ. Biosynthesis of von Willebrand protein by human endothelial cells. Identification of a large precursor polypeptide chain. J Biol Chem. 1983;258:2065–2067. | ||
Sporn LA, Chavin SI, Marder VJ, Wagner DD. Biosynthesis of von Willebrand protein by human megakaryocytes. J Clin Invest. 1985;76:1102–1106. | ||
Castaman G, Federici AB, Rodeghiero F, Mannucci PM. Von Willebrand’s disease in the year 2003: towards the complete identification of gene defects for correct diagnosis and treatment. Haematologica. 2003;88:94–108. | ||
Federici AB. The factor VIII/von Willebrand factor complex: basic and clinical issues. Haematologica. 2003;88:EREP02. | ||
Mannucci PM, Kempton C, Millar C, et al. Pharmacokinetics and safety of a novel recombinant human von Willebrand factor manufactured with a plasma-free method: a prospective clinical trial. Blood. 2013;122(5):648–657. | ||
Gill JC, Castaman G, Windyga J, et al. Hemostatic efficacy, safety, and pharmacokinetics of a recombinant von Willebrand factor in severe von Willebrand disease. Blood. 2015;126(17):2038–2046. | ||
Di Minno G, Canaro M, Ironside JW, et al. Pathogen safety of long-term treatments for bleeding disorders: still relevant to current practice. Haematologica. 2013;98(10):1495–1498. | ||
Steele M, Cochrane A, Wakefield C, et al. Hepatitis A and B immunization for individuals with inherited bleeding disorders. Haemophilia. 2009;15(2):437–447. | ||
Batlle J, Lopez-Fernandez MF, Fraga EL, et al. Von Willebrand factor/factor VIII concentrates in the treatment of von Willebrand disease. Blood Coagul Fibrinolysis. 2009;20:89–100. | ||
Favaloro EJ, Kershaw G, McLachlan AJ, Lloyd J. Time to think outside the box? Proposal for a new approach to future pharmacokinetic studies of von Willebrand factor concentrates in people with von Willebrand disease. Semin Thromb Hemost. 2007;33:745–758. | ||
Favaloro EJ, Franchini M, Lippi G. Biological therapies for von Willebrand disease. Expert Opin Biol Ther. 2012;12(5):551–564. | ||
Rodeghiero F, Castaman G, Dini E. Epidemiological investigation of prevalence of von Willebrand’s disease. Blood. 1987;69(2):454–459. | ||
Castaman G, Eikenboom JCJ, Bertina RM, Rodeghiero F. Inconsistency of association between type 1 von Willebrand disease phenotype and genotype in families identified in an epidemiological investigation. Thromb Haemost. 1999;82(3):1065–1070. | ||
Casari C, Berrou E, Lebret M, et al. von Willebrand factor mutation promotes thrombocytopathy by inhibiting integrin αIIbβ3. J Clin Invest. 2013;123(12):5071–5081. | ||
Castaman G, Goodeve A, Eikenboom J. Principles of care for diagnosis and treatment of von Willebrand disease. Haematologica. 2013; 98(5):667–674. | ||
Sadler JE, Budde U, Eikenboom JC, et al. Update on the pathophysiology and classification of von Willebrand disease: a report of the Subcommittee on von Willebrand Factor. J Thromb Haemost. 2006; 4(10):2013–2014. | ||
Tosetto A, Rodeghiero F, Castaman G, et al. A quantitative analysis of bleeding symptoms in type 1 von Willebrand disease: results from a multicenter European study (MCMDM-1 VWD). J Thromb Haemost. 2006;4(4):766–773. | ||
Goodeve A, Eikenboom J, Castaman G, et al. Phenotype and genotype of a cohort of families historically diagnosed with type 1 von Willebrand disease in the European study, Molecular and Clinical Markers for the Diagnosis and Management of Type 1 von Willebrand Disease (MCMDM-1 VWD). Blood. 2007;109(1):112–121. | ||
Castaman G, Federici AB, Tosetto A, et al. Different bleeding risk in type 2A and 2M von Willebrand disease: a two-year prospective study in 107 patients. J Thromb Haemost. 2012;10(4):632–638. | ||
Rodeghiero F, Castaman G, Tosetto A. How I treat von Willebrand disease. Blood. 2009;114(6):1158–1165. | ||
Castaman G, Lethagen S, Federici AB, et al. Response to desmopressin is influenced by the genotype and the phenotype in type 1 von Willebrand disease (VWD): results from the European study MCMDM-1 VWD. Blood. 2008;111:3531–3539. | ||
Federici AB, Mannucci PM, Castaman G, et al. Clinical and molecular predictors of thrombocytopenia and risk of bleeding in patients with von Willebrand disease type 2B: a cohort study of 67 patients. Blood. 2009;113(5):526–534. | ||
Mannucci PM, Franchini M. The use of plasma-derived concentrates. In: Federici AB, Lee CA, Berntorp EE, Lillicrap D, Montgomery RR. Von Willebrand disease. Oxford, UK: Wiley-Blackwell; 2011:200–206. | ||
Mannucci PM, Chediak J, Hanna W, Byrnes J, Marlies L, Ewenstein BM; Alphanate Study Group. Treatment of von Willebrand disease with high-purity factor VIII/von Willebrand factor concentrate: a prospective, multicenter study. Blood. 2002;99:450–456. | ||
Bello IF, Yuste VJ, Molina MQ, Navarro FH. Fanhdi, efficacy and safety in von Willebrand’s disease: prospective International study results. Haemophilia. 2007;13(Suppl5):25–32. | ||
Gill JC, Ewenstein BM, Thomson AR, Mueller-Velten G, Schwartz BA; Humate-P Study Group. Successful treatment of urgent bleeding in von Willebrand disease with factor VIII/von Willebrand factor concentrate (Humate-P): use of the ristocetin cofactor assay (VWF:RCo) to measure potency and to guide therapy. Haemophilia. 2003;9:688–695. | ||
Thomson AR, Gill JC, Ewenstein BM, Mueller-Velten G, Schwartz BA; Humate-P Study Group. Successful treatment for patients with von Willebrand disease undergoing urgent surgery using factor VIII/von Willebrand factor concentrate (Humate-P). Haemophilia. 2004;10:42–51. | ||
Lethagen S, Kyrle PA, Castaman G, Haertel S, Mannucci PM; Haemate P Surgical Study Group. Von Willebrand factor/factor VIII concentrate (Haemate P) dosing based on pharmacokinetics: a prospective multicenter trial in elective surgery. J Thromb Haemost. 2007;5:1420–1430. | ||
Berntorp E, Archey W, Auerswald G, et al. A systematic overview of the first pasteurized VWF/FVIII medicinal product Haemate-P/Humate-P: history and clinical performance. Eur J Haematol Suppl. 2008;70:3–35. | ||
Mannucci PM. Treatment of von Willebrand’s disease. N Engl J Med. 2004;351(7):683–694. | ||
Franchini M. Surgical prophylaxis in von Willebrand’s disease: a difficult balance to manage. Blood Transfus. 2008;6(Suppl 2):33–38. | ||
Makris M, Colvin B, Gupta V, Shields ML, Smith MP. Venous thrombosis following the use of intermediate purity FVIII concentrate to treat patients with von Willebrand’s disease. Thromb Haemost. 2002;88:387–388. | ||
Mannucci PM. Venous thromboembolism in von Willebrand disease. Thromb Haemost. 2002;88:378–379. | ||
Kyrle PA, Minar E, Hirschl M, et al. High plasma levels of factor VIII and the risk of recurrent venous thromboembolism. N Engl J Med. 2000; 343:457–462. | ||
Borel-Derlon A, Federici AB, Roussel-Robert V, et al. Pharmacokinetic studies on Wilfactin, a von Willebrand factor concentrate with a low FVIII content treated with three virus-inactivation/removal methods. J Thromb Haemost. 2005;3(10):2219–2227. | ||
Mannucci PM, Tamaro G, Narchi G, et al. Life-threatening reaction to factor VIII concentrate in a patient with severe von Willebrand disease and alloantibodies to von Willebrand factor. Eur J Haematol. 1987;39:467–470. | ||
Ciavarella N, Schiavoni M, Valenzano E, Mangini F, Inchingolo F. Use of recombinant factor VIIa (Novoseven) in the treatment of two patients with type III von Willebrand’s disease and an inhibitor against von Willebrand factor. Haemostasis. 1996;26:10–14. | ||
Franchini M, Gandini G, Giuffrida A, Gironcoli M, Federici AB. Treatment for patients type 3 von Willebrand disease and alloantibodies: a case report. Haemophilia. 2008;14:645–646. | ||
Berntorp E, Petrini P. Long-term prophylaxis in von Willebrand disease. Blood Coagul Fibrinolysis. 2005;16(Suppl 1):S2–S26. | ||
Federici AB. Highly purified VWF/FVIII concentrates in the treatment and prophylaxis of von Willebrand disease. The PRO.WILL study. Haemophilia. 2007;13(Suppl 5):15–24. | ||
Abshire TC, Federici AB, Alvarez MT, et al. Prophylaxis in severe forms of von Willebrand’s disease: results from the von Willebrand disease prophylaxis network (VWD PN). Haemophilia. 2013;19(1):76–81. | ||
Bolton-Maggs PH, Pasi KJ. Haemophilias A and B. Lancet. 2003; 361:1801–1809. | ||
Srivastava A, Brewer AK, Mauser-Bunschoten EP, et al; Treatment Guidelines Working Group on Behalf of the World Federation of Hemophilia. Guidelines for the management of hemophilia. Haemophilia. 2013;19:e1–e47. | ||
Manco-Johnson MJ, Abshire TC, Shapiro AD, et al. Prophylaxis versus episodic treatment to prevent joint disease in boys with severe haemophilia. N Engl J Med. 2007;357:535–544. | ||
Rocino A, Coppola A, Franchini M, et al. Principles of treatment and update of recommendations for the management of haemophilia and congenital bleeding disorders in Italy. Blood Transfus. 2014;12:575–598. | ||
Astermark J, Altisent C, Batorova A, et al; European Haemophilia Therapy Standardisation Board. Non-genetic risk factors and the development of inhibitors in haemophilia: a comprehensive review and consensus report. Haemophilia. 2010;16:747–766. | ||
Astermark J. Inhibitor development: patient-determined risk factors. Haemophilia. 2009;16:66–70. | ||
Santagostino E, Mancuso ME, Rocino A, et al. Environmental risk factors for inhibitor development in children with haemophilia A: a case-control study. Br J Haematol. 2005;130:422–227. | ||
Escuriola Ettingshausen C, Kreuz W. Recombinant vs. plasma-derived products, especially those with intact VWF, regarding inhibitor development. Haemophilia. 2006;12(suppl 6):102–106. | ||
Gouw SC, van der Bom JG, Auerswald G, Escuriola Ettingshausen C, Tedgard U, van der Berg HM. Recombinant versus plasma-derived factor VIII products and the development of inhibitors in previously untreated patients with severe haemophilia A: the CANAL cohort study. Blood. 2007;109:4693–4697. | ||
Mancuso ME, Mannucci PM, Rocino A, Garagiola I, Tagliaferri A, Santagostino E. Source and purity of FVIII products as risk factors for inhibitor development in patients with hemophilia A. J Thromb Haemost. 2012;10(5):781–790. | ||
Peyvandi F, Mannucci PM, Garagiola I, et al. Source of factor VIII replacement (plasmatic or recombinant) and incidence of inhibitory alloantibodies in previously untreated patients with severe hemophilia a: the Multicenter Randomized Sippet Study. Oral presentation at 57th ASH Annual Meeting and Exposition. Orlando, FL, USA; 2015. | ||
Young G, Shafer FE, Rojas P, Seremetis S. Single 270 micro kg(−1)-dose rFVIIa vs. Standard 90 micro kg(−1)-dose rFVIIa and aPCC for home treatment of joint bleeds in haemophilia patients with inhibitors: a randomized comparison. Haemophilia. 2008;14:287–294. | ||
Astermark J, Donfield SM, DiMichele DM, et al; FENOC Study Group. A randomized comparison of bypassing agents in haemophilia complicated by an inhibitor: the FEIBA NovoSeven Comparative (FENOC) Study. Blood. 2007;109:546–551. | ||
Oldenburg J, Austin SK, Kessler CM. ITI choice for the optimal management of inhibitor patients – from a clinical and pharmacoeconomic perspective. Haemophilia. 2014;20(Suppl 6):17–26. | ||
Hay CR, Di Michele DM; International Immune Tolerance Study. The principal results of the International Immune Tolerance Study: a randomized dose comparison. Blood. 2012;119:1335–1344. | ||
Kempton CL, White GC II. How we treat a hemophilia A patient with a factor VIII inhibitor. Blood. 2009;113:11–17. | ||
Brackmann HH, Gormsen J. Massive factor-VIII infusion in haemophiliac with FVIII inhibitor, high responder. Lancet. 1977;2:933. | ||
Collins PW, Chalmers E, Hart DP, et al; UK Haemophilia Centre Doctors Organization. Diagnosis and treatment of FVIII and IX inhibitors in congenital haemophilia: 4th edition. Br J Haematol. 2013;160:153–170. | ||
Di Michele DM, Hoots WK, Pipe SW, Rivard GE, Santagostino E. International workshop on immune tolerance induction: consensus recommendations. Haemophilia. 2007;13(Suppl 1):1–22. | ||
Benson G, Auerswald G, Elezovic I, et al. Immune tolerance induction in patients with severe hemophilia with inhibitors: expert panel views and recommendations for clinical practice. Eur J Haematol. 2012;88: 371–379. | ||
Franchini M, Lippi G. Von Willebrand factor-containing factor VIII concentrates and inhibitors in haemophilia A: a critical literature review. Thromb Haemost. 2010;104:931–940. | ||
Ettingshausen CE, Kreuz W. Role of von Willebrand factor in immune tolerance induction. Blood Coagul Fibrinolysis. 2005;16(Suppl 1):S27–S31. | ||
Gringeri A, Musso R, Mazzucconi MG, et al. Immune tolerance induction with a high purity von Willebrand factor/VIII complex concentrate in haemophilia A patients with inhibitors at high risk of a poor response. Haemophilia. 2007;13:373–379. | ||
Kreuz W. The role of VWF for the success of immune tolerance induction. Thromb Res. 2008;122 (Suppl 2):S7–S12. | ||
Greninger DA, Saint-Remy JM, Jacquemin M, Benhida A, Di Michele DM. The use of factor VIII/ von Willebrand factor concentrate for immune tolerance induction in haemophilia A patients with high-titre inhibitors: association of clinical outcome with inhibitor epitope profile. Haemophilia. 2008;14:295–302. | ||
Dasgupta S, Repesse Y, Bayry J, et al. VWF protects FVIII from endocytosis by dendritic cells and subsequent presentation to immune effectors. Blood. 2007;109:610–612. | ||
Qadura M, Waters B, Burnett E, et al. Recombinant and plasma-derived factor VIII products induce distinct splenic cytokine microenvironments in haemophilia A mice. Blood. 2009;114:871–880. | ||
Kurth M, Puetz J, Kouides P, et al. The use of a single von Willebrand factor-containing, plasma-derived FVIII product in hemophilia A immune tolerance induction: the US experience. J Thromb Haemost. 2011;9:2229–2234. | ||
Oldenburg J, Jimenez-Yuste V, Peiro-Jordan R, Aledort LM, Santagostino E. Primary and rescue immune tolerance induction in children and adults: a multicentre international study with a VWF-containing plasma-derived FVIII concentrate. Haemophilia. 2014;20:83–91. | ||
Rothschild C, D’Orion R, Borel-Derlon A, Gruel Y, Navarro R, Negrier C. Use of Haemate® P as immune tolerance induction in patients with severe haemophilia A who failed previous induction attempts: a multicentre observational study. Haemophilia. 2013;19:281–286. | ||
Bidlingmaier C, Kurnik K, Escuriola-Ettingshausen C, et al. Immune tolerance induction with a factor VIII concentrate containing von Willebrand factor (Haemoctin SDH®) in 14 patients with severe haemophilia A. Haemophilia. 2011;17:e837–e840. | ||
Gringeri A. VWF/FVIII concentrates in high-risk immune tolerance: the RESIST study. Haemophilia. 2007;13(Suppl 5):73–77. | ||
RESIST 2015. Rescue Immune Tolerance Study website. Available from: http://www.itistudy-resist.com/index.htm. Accessed May 18, 2016. | ||
Kruse-Jarres R, Gilsenam A, Spears J, Kaye JA. Prospective, observational study of plasma-derived factor VIII/von Willebrand factor in immune tolerance induction: the PRISM registry. Haemophilia. 2015; 21(2):e122–e124. | ||
Astermark J, Morado M, Rocino A, et al; European Haemophilia Treatment Standardisation Board. Current European practice in immune tolerance induction therapy in patients with haemophilia and inhibitors. Haemophilia. 2006;12:363–371. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
