Back to Journals » International Journal of Women's Health » Volume 12
Hormonal Receptors, Human Epidermal Growth Factor Receptor-2 and Triple Negative Immunohistochemical Typing in Women with Breast Cancer in Kampala, Uganda
Authors Mlole AT, Yahaya JJ, Othieno E , Kalungi S, Okwi AL
Received 30 June 2020
Accepted for publication 20 October 2020
Published 27 November 2020 Volume 2020:12 Pages 1109—1123
DOI https://doi.org/10.2147/IJWH.S270082
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Everett Magann
Angela T Mlole, 1 James J Yahaya, 2 Emmanuel Othieno, 3 Sam Kalungi, 3 Andrew L Okwi 1
1Department of Pathology, Makerere College of Health Sciences (MaKCHS), Makerere University, Kampala, Uganda; 2Department of Biomedical Science, College of Health Science (CHS), The University of Dodoma, Dodoma, Tanzania; 3Department of Pathology, Mulago National Hospital, Kampala, Uganda
Correspondence: James J Yahaya Department of Biomedical Science
College of Health Science (CHS), The University of Dodoma, P.O. Box 395, Dodoma, Tanzania
Email [email protected]
Background: The expression of estrogen and progesterone receptors (ER and PR) and human epidermal growth factor receptor-2 (HER2) has been reported to have an invaluable prognostic role. The aim of this study was to determine the expression of ER, PR and HER2 in women with breast cancer (BC) in Kampala, Uganda.
Methods: Expression of ER, PR and HER2 was determined immunohistochemically. Logistic regression was performed to determine the effect of the independent factors in predicting the risk of not expressing the breast markers. A two-tailed p< 0.05 was regarded to be statistically significant.
Results: ER, PR and HER2 were expressed in 53.4%, 46.6% and 18.5%, respectively. ER and PR co-expression was present in 42.7% and 37.9% patients had triple negative breast cancer (TNBC). Age was an independent predictor of expression of ER (AOR = 0.18, 95% CI = 0.062– 0.541, p = 0.002) and PR (AOR = 0.35, 95% CI = 0.129– 0.968, p = 0.043).
Conclusion: The majority of patients in this study had less than 50 years with high tumour grade. Interestingly, most of them had high expression of HER2 with TNBC which are molecular subtypes of BC with poor prognosis. Age was an independent predictor of expression of both ER and PR.
Keywords: hormonal receptors, HER2, triple negative, breast cancer, Uganda
Background
Breast cancer (BC) is a leading cause of female cancer-related mortality globally, particularly in those older than 50 years of age and only 5% to 7% of patients in whom the disease is diagnosed before the fourth decade.1 In a review, Fitzmaurice and her co-workers reported that, globally, BC is the cancer with the highest incidence and the leading cause of cancer-related deaths and disability-adjusted life-years (DALYs).2 In 2016, there were 1.7 million incident cases, 535,000 deaths, and 14.9 million DALYs of BC globally.2
In less developed areas, such as Africa and the Middle East where population-based screening practice is still a challenge and yet the population on average is comprised of 20% of the female patients who are diagnosed with BC before the age of 40.3,4 Nonetheless, the role of genetical predisposition or environmental factors in the pathogenesis of breast cancer for the premenopausal group is not clearly known as compared to those in the postmenopausal group.5
The expression of hormonal receptors (HRs) (estrogen (ER) and progesterone (PR)), human epidermal growth factor receptor-2 (HER2) protein and proliferation markers such as Ki67 in premenopausal women with BC differs from that in postmenopausal women.6–8 In the study that was done in West Africa it was found that, HRs negative and triple negative breast cancer (TNBC) were representing the majority of cases. Three studies done in Tanzania by Mbonde et al9 reported 33% and 18% of ER and PR expression, respectively, Rambau et al10 reported 32.7%, 42.3%, 23.1% and 38.4% for ER, PR, HER2 and TNBC, respectively and Mwakigonja et al11 also reported 43.4%, 26.4%, 28%, 15.2% and 45.6% for ER, PR, ER and PR co-expression, HER2 and TNBC, respectively of the patients who were expressing the markers and therefore, they were expected to benefit from hormonal therapy. In all the three studies, most of the patients were of young age and had advanced stage at the time of presentation. HRs and HER-2 protein expression together with other biological characteristics among women with BC are generally comparable to those of other indigenous Africans and a majority of patients have TNBC.
Similar observations were reported in Kenya in a study which involved women with BC in whom ER and PR expression was reported to be 24% and 10%, respectively with advanced stage.12 In Uganda studies have reported aggressive BC among women of young age and low expression of ER, PR and HER2. For example, Roy and Othieno reported that, women who are diagnosed with BC in Uganda are of younger age and they tend to have aggressive tumour grade with low expression of the ER, PR, HER2 and TNBC of 60%, 46%, 11% and 36%, respectively.13 In another study done in a tertiary hospital in Uganda by Galukande et al14 it reported 38%, 22% and 34% of the cases had ER, HER2 and TNBC, respectively.
This study aimed to determine the expression of hormonal receptors, HER2 and TNBC in women with BC in Uganda and the second objective was to determine the association of the expressed biomarkers with age, histological types and tumour grade.
Methods
Study Design and Setting
This was a cross-sectional analytical laboratory-based study which involved retrospective collection of the data. The study was conducted at the Department of Pathology, Makerere College of Health Sciences (MakCHS) in Kampala, Uganda. The department is situated at Mulago National Referral Hospital (MNRH). The department specifically serves the roles of teaching, research as well as offering diagnostic and autopsy services for the whole country.
Patients’ Specimens
The study utilized Formalin Fixed Paraffin Embedded (FFPE) tissue blocks of women who were diagnosed histologically with breast cancer from January 2010 to August 2017. The tissue blocks were retrieved from the laboratory archive and all the necessary clinical information of the patients were extracted from the laboratory request forms and supplementation of the clinical data was by means of the patients’ files which were obtained from the medical record of the hospital.
Sampling Procedure
Convenience sampling method was applied for sampling the cases which were included in the study. All the sampled cases that met the inclusion criteria were retrieved consecutively until the sample size of 103 specimens of the FFPE tissue blocks was attained. The inclusion criteria were: (1) female patients, (2) cases with available FFPE tissue blocks, (3) cases with available clinical information. The exclusion criteria were: (1) male patients, (2) missing FFPE tissue blocks, (3) cases with spoilt FFPE tissue blocks, (4) cases with missing clinical information.
Haematoxylin and Eosin (H and E) Staining
The sections were first placed on a cooling part of the embedding station at a temperature of −10 °C for 30 minutes before being sectioned. Thereafter, they were sectioned at a thickness of 3 microns and placed on the slides and left in the oven at 50 °C for 30 minutes for dewaxing. The sections were, furthermore, dewaxed through three changes of xylene for 10 dips in each and then hydrated in grades of alcohol (100%, 95%, 90%, 75%, and 70%) followed by rinsing in running tape water.
This was followed by staining the tissue sections with Harris haematoxylin for 15 minutes. They were rinsed in running tap water for at least 5 minutes and then differentiated in 1% acid-alcohol (1% HCL in 70% alcohol) for 2 seconds. The tissue sections were washed in running tap water and left to bluing for 15 minutes then they were counter stained with eosin 1% for 5 minutes. They were washed in running tap water for 5 minutes. Then they were dehydrated in increased concentrations of alcohol (70%, 90%, 95%, 100%) for a few seconds followed by washing in running tap water for 5 minutes. Finally, the slides were cleared in two changes of xylene for 10 dips and mounted with coverslips using Distyrene Plasticizer Xylene (DPX).
Reporting of the H and E Tissue Sections
Reporting of the H and E stained tissue slides was done by two independent and experienced pathologists who were blinded of the clinical presentation of the patients. Scoring of the tumour grade was done by using a Bloom-Richard grading system as described in the study of Meyer et al in 2005.15
Immunohistochemistry (IHC) Staining for Hormonal Receptors and HER2 Protein Antibodies
The deparaffinized tissue sections of 3 microns thickness were placed on charged glass slides (FrostStat, DAKO-Denmark) and then heated at 750 watts in a microwave for 10 minutes using 10 mmol/L of tris buffered solution (TBS) of pH 7.0. The tissue sections were dipped in 3% of hydrogen peroxide solution for 10 minutes to block endogenous peroxidase activity in order to prevent background staining.
Then the tissue sections were rinsed in Phosphate Buffer Solution (PBS) followed by pre-treating with a secondary antibody amplifier Horseradish Peroxidase (HRP) and rinsing in buffered water. The tissue sections were incubated with monoclonal mouse anti ER, PR and HER2 antibody (DAKO Company, Denmark) for 30 minutes at room temperature. Diaminobenzidine tetrahydrochloride (DAKO LSAB2, Denmark) solution was added onto the tissue sections for 10 seconds for detection purpose. Then the tissue sections were counter stained with Harris hematoxylin for 30 seconds followed by making 10 dips of the slides in two changes of xylene, mounting the stained slides with DPX and lastly cover-slipping the slides.
Reporting of IHC Stained Tissue Slides
This was carried out by two independent and experienced pathologists different from the ones who reported the H and E tissue sections. The pathologists were blinded of both histological results and clinical information. The expression of ER and PR hormonal receptors was determined by using the guidelines provided in the American Society of Clinical Oncology/College of American Pathologists Guideline Recommendations for Immunohistochemical Testing of Estrogen and Progesterone Receptors in Breast Cancer as reported by Wolf et al.16 In this study, scoring of ER/PR positive cases was considered if the percentage of positivity was not less than 1%. The percentage for the positivity was obtained by dividing the positively stained tumour cells over the total number of tumour cells and the fraction obtained was multiplied by 100%. Intensity of nuclear staining ranged from 0–3 (0-negative, 1-weak, 2-moderate, 3-strong).
On the other hand, HER2 positivity was determined by HER2 test positive when IHC 3+ based on circumferential membrane staining that is complete and intense. HER2 test result as equivocal when IHC 2+ based on circumferential membrane staining that is incomplete and/or weak/moderate and within ˃10% of the invasive tumor cells or complete and circumferential membrane staining that is intense and within ≤10% of the invasive tumor cells. HER2 test result as negative when IHC 1+ as defined by incomplete membrane staining that is faint/barely perceptible and within ˃10% of the invasive tumor cells and IHC 0 as defined by no staining observed or membrane staining that is incomplete and is faint/barely perceptible and within ≤10% of the invasive tumor cells. All IHC 2+, IHC 1+ and 0 test results in this study were considered negative.
Statistical Analysis
Data collected were analyzed by using STATA version 13.0 (IBM Statistics, Chicago, USA). For checking errors and missing data, frequency tables and crosstabs were used. Continuous variables were presented in mean ± standard deviation (SD). Categorical variables were summarized in proportion. Chi-square statistical test was used to determine the association of expression of HRs (ER and PR) and HER2 with clinicopathological characteristics (age, tumour grade and histological types). Logistic regression analysis was used to determine the predictors of ER, PR and HER2 expression. Odds ratio (OR) at 95% confidence interval (CI) was used to measure the risk of not expressing the breast markers. A two tailed p < 0.05 was considered significant.
Ethical Consideration
We obtained ethical approval from the institution review board of the School of Biomedical Science of Makerere College of Sciences (MakCHS).
Results
Clinicopathological Characteristics of the Patients
A total of 103 patients were included in the present study. The mean ± SD age of the patients was 49 ± 15 years (range: 24–93 years). Thirty patients (29.1%) were in the age group 41–50 years, while 35.0% (36/103) were below 41 years. Regarding the histological types of BC, majority of the patients 68.9% (71/103) had invasive carcinoma of no special type (NST) followed by invasive lobular carcinoma which comprised 22.3% (23/103). More than half 53.4% (55/103) of the patients had intermediate grade (grade 2) and high grade (grade 3) was present in 31.1% (32/103) of the patients (Table 1). Of those with high grade cancer, 16.5% (17/103) were younger than 41 years and only 4.9% (5/103) of those older than 50 years of age had high grade BC. Also there were relatively more patients older than 50 years of age with grade 1 7.8% (8/103) compared to 1.9% (2/103) of patients who were aged less than 41 years, and most of patients with intermediate grade (grade 2) 23.3% (24/103) (Figure 1).
 |
Table 1 Clinicopathologic Characteristics of the Patients (n = 103) |
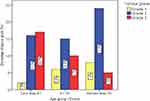 |
Figure 1 Histological grade of cancers among the different age groups of the patients. |
Expression of ER, PR and Co-Expression of ER and PR
ER was the most expressed HR and more than half of the patients 53.4% (55/103) had positive ER (Figure 2A) followed by PR that was positive in 46.6% (48/103) of the patients (Figure 2B). Co-expression of ER and PR was found in 42.7% (44/103) of all the patients. The level of expression of the HRs was lower in young patients than in old patients. The difference in expression of ER and ER and PR co-expression according to age groups of the patients was statistically significant; (95% CI = 0.081–0.594, p = 0.007), (95% CI = 0.070–0.525, p = 0.003) and (95% CI = 0.047–0.394, p = 0.000) respectively. The expression of ER, PR and ER and PR co-expression in this study according to tumour grades and histological types of BC among the cases was not statistically significantly different (Table 2).
 |
Table 2 Expression of ER, PR, and Co-Expression of ER and PR According to Age, Histological Type and Tumour Grade |
Expression of HER2 Protein and Triple Negative Breast Cancer (TNBC) in the Study
Expression of HER2 (Figure 2C) in this study was present in 18.5% (19/103) whereas triple negative breast cancer (TNBC) was present in 37.9% (39/103) of all the patients. HER2 expression and TNBC cases were predominantly found in premenopausal patients (≤50 years of age) as compared to the postmenopausal patients (>50 years of age). The difference in expression for HER2 among cases according to age groups was significantly different (95% CI = 1.011–2.109, p = 0.04). However, there was no significant difference for the expression of HER2 as per tumour grades (p = 0.287, 95% CI = 0.319–2.338) and histological types (p = 0.114, 95% CI = 0.332–2.838). Additionally, there was no significant difference for being triple negative among the cases based on tumour grades (0.626, 95% CI = 0.631–4.649), age (p = 0.090, 95% CI = 0.789–6.331) and histological types (p = 0.624, 95% CI = 0.520–2.970) (Table 3).
 |
Table 3 Expression of HER2 and TNBC According to Age, Histological Type and Tumour Grade |
Prediction of Clinicopathologic Characteristics for the Expression of Hormonal Receptors and HER2 Protein
Univariately, postmenopausal (>50 years of age) women were 3.7 times more likely to express ER compared to premenopausal (≤50 years of age) women (72.92% versus 42.42%) and the difference for expressing ER between the two groups was statistically significantly different (95% CI = 1.53–8.79, p = 0.004). When all other factors were adjusted, age remained an independent predictor of expression of ER and post-menopausal women were 72% more likely to express ER than premenopausal women and the difference was statistically significantly different (95% CI: 0.062–0.541, p = 0.002) (Table 4).
 |
Table 4 Univariate and Multivariate Analyses of the Association Between ER Expression and Age, Tumour Grade and Histological Types of Breast Cancer in the Patients |
In our study it was found that, patients with grade 2 were 7% less likely to have ER expression compared to those who had grade 1. Also patients with tumour grade 3 were 22% less likely to express ER compared to patients with grade 1. However, in both compared groups, the difference was not statistically significant (Table 4). Patients with invasive lobular carcinoma (ILC) were 42% more likely not to express ER than those with infiltrating ductal carcinoma of no specified type (IDC-NST). Patients with other types of BC were 54% more likely not to express ER than those with IDC-NST. The risk of not expressing the ER for ILC and other types of breast cancer as compared to IDC-NST in our series was not significantly different.
Association of Patients’ Clinicopathologic Characteristics with PR Expression
Under univariate analysis, post-menopausal women were 3.9 times more likely to express PR hormonal receptor than pre-menopausal women (67.6% versus 34.8%) and the difference was statistically significantly different (95% CI = 1.66–9.15, p = 0.002). Even in multivariate analysis, age remained a predicting factor for not expressing PR hormonal receptors in this study. Postmenopausal women were 65% more likely not to express the PR hormonal receptor and the difference was statistically significant (95% CI = 0.129–0.968) (Table 5).
 |
Table 5 Univariate and Multivariate Analyses for the Association Between PR Expression and Age, Tumour Grade and Histological Types of Breast Cancer in the Patients |
There was a difference in the risk of not expressing PR between cases with grade 2 and those with grade 1 (COR = 1.04, 95% CI = 0.344–3.316, p = 0.949) whereas those with tumour grade 3 were 40% less likely to express PR compared to cases with grade 1. However, in both compared groups the difference was not statistically significant. Cases with ILC were 3% more likely not to express ER than those with infiltrating ductal carcinoma of no specified type (IDC-NST). Other types of breast cancer were 1.63 more likely not to express ER than those with IDC-NST, however, there was no statistical difference (Table 5).
Association of Patients’ Clinicopathologic Characteristics with Co-Expression of ER and PR Hormonal Receptors
Post-menopausal women were 3.86 times more likely to co-express ER and PR hormonal receptors than pre-menopausal women in this study (88.9% versus 30.3%) and the difference between the two compared groups was significantly different (95% CI = 1.659–8.968, p = 0.001). Under multivariate analysis, age became not an independent predictor of co-expression of ER and PR although post-menopausal women had 14% more chance of having a co-expression of ER and PR than pre-menopausal women but there was no statistical difference (95% CI = 0.142–1.051, p = 0.063).
Grade 2 and 3 cases were 1.91 and 1.59 times more likely to have a co-expression of ER and PR, respectively but there was no statistical significant difference when both were compared to cases with tumour grade 1 (95% CI = 0.563–6.477, p = 0.300) and (95% CI = 0.645.3.921, p = 0.313). Cases with ILC were 8% less likely not to co-express ER and PR than those with IDC-NST and other types of breast cancer were 4% less likely not to express ER than those with IDC-NST, however, there was no statistical difference (Table 6).
 |
Table 6 Univariate and Multivariate Analyses for the Association of Co-Expression of ER and PR and Age, Tumour Grade and Histological Types of Breast Cancer in the Patients |
Association of Patients’ Clinicopathologic Characteristics with HER2 Expression
There was no statistically significant association between patients’ age and HER2 expression even for univariate analysis (95% CI = 0.27–2.29, p = 0.663) but post-menopausal women (>50 years of age) had 21% less chance of expressing HER2 protein compared to pre-menopausal women (≤50 years of age) (31.6% versus 68.4%) (Table 7). HER2 expression, which is an indication of poor prognosis, was increasing with increase in the tumour grades. Cases with tumour grade 2 and 3 were 3.33 and 5 times more likely to have positive HER2, respectively, but the difference for both grades with those having tumour grade 1 was not significantly different (95% CI = 0.39–28.25, p = 0.27) and (95% CI = 0.57–44.08, p = 0.147). The histological types of BC among the cases could not predict the risk of not expressing PR in univariate analysis.
 |
Table 7 Univariate and Multivariate Analyses for the Association Between HER2 Expression and Age, Tumour Grade and Histological Types of Breast Cancer in the Patients |
Association of Patients’ Clinicopathologic Characteristics with Triple Negative Expression
The risk of post-menopausal women (>50 years of age) to be TN was 61% less than pre-menopausal women (≤50 years) (23.1% versus 76.9%) and the difference was statistically significantly different (95% CI = 0.16–0.94, p = 0.037) for univariate analysis. Also age continued to be an independent predicting factor under multivariate analysis of being TN between pre-and post-menopausal cases. Women with breast cancer not greater than 50 years of age were 4.4 times more likely to be TN than those greater than 50 years of age and the association was significantly different (95% CI = 1.451–13.223, p = 0.009) (Table 8).
 |
Table 8 Univariate and Multivariate Analyses for the Association Between TNBC and Age, Tumour Grade and Histological Types of Breast Cancer in the Patients |
Tumour grade was increasing with increase in the proportion of triple negative cases. Cases with tumour grade 2 and 3 were 21% and 33% more likely to be TN than grade 1, respectively, however, the difference was not statistically significantly different (95% CI = 0.26–2.45, p = 0.69) and (95% CI = 0.20–2.30, p = 0.53), respectively. Cases with ILC were 60% less likely to be TN whereas those with other histological types were 20% less likely to be TN. However, the difference in the chances of being TN for the two compared histological types was not statistically significant (95% CI = 0.21–3.51, p = 0.31) and (95% CI = 0.34–1.92, p = 0.62) (Table 8).
Discussion
HRs and HER2 characterization of patients with BC has been widely documented in the literature with an entire focus on their ability to predict and determine prognosis of BC when they are examined in conjunction with the conventional clinicopathological prognostic factors. Although a number of studies agree on the positive correlation of such biomarkers with age, tumour grade among many other conventional prognostic factors, still there is quite a significant number of studies in the literature reporting contradicting results.
We determined the prevalence of expression of ER, PR, ER and PR co-expression and HER2 and in whom the three breast markers were all not expressed (TNBC). The key findings for this study are that, HRs expression was higher in postmenopausal than in premenopausal women. HER2 protein expression was higher in premenopausal patients compared to postmenopausal ones. Likewise, there were more patients not greater than 50 years of age with TNBC than patients who were greater than 50 years of age. Interestingly, this study found that, age was an independent predictor for the positive association of ER, PR and TNBC.
The majority of African and Black-American women with BC are of young age (younger than 50 years of age) compared to Caucasians and patients in other developed countries in which patients with BC tend to be older than 50 years of age. The majority of the patients in our study 64.1% (66/103) were ≤50 years (49 ± 15 years) (Table 1). This finding is in agreement with other studies which were conducted in Tanzania (48.3 and 49.0 years), Uganda (45.0 years), Ghana (51.0 years) and Egypt (51.3 years).10,11,14,17,18 The mean age of patients with BC reported in most developing countries is lower than that reported in developed countries. For example, Adjei et al17 reported a mean age of 60.2 years in Norwegian women with BC.
Additionally, the vast majority of patients with BC in developing countries, particularly who are living in the southern sub-Saharan region, are 50 years or younger.14 In our study 64.1% of the patients were 50 years or younger, similar and even slightly lower than the proportion in the two studies which were previously done in Uganda, which reported that 68.8% and in another study 73% of the patients were 50 years or younger.13
Furthermore, younger patients aged 50 years or younger in our series had high tumour grade compared to those aged greater than 50 years of age (26.2% versus 4.9%) (Figure 1). This is similar to the reports in most of the African countries which reported that aggressive BC is more prevalent among young patients.14,19 For example, in Uganda, Kenya and Tanzania it was reported that, most patients with BC were aged 50 years or younger and most of them, 67.4%, 41.1% and 76.9%, had tumour grade 3, respectively.10,12,14 However, these findings differ from results of studies conducted in developed countries in which most of the patients with BC have low tumour grade and low tumour stage at initial diagnosis. In two studies, one from Ireland and another in Norway, they reported that 15.2% and 47% of the patients had grade 3, respectively.20,21 Also in another study which was done by Adjei et al which included patients with BC from Norway and Ghana, it was found 57% of cases from Ghana had grade 3 and only 30% of the cases from Norway had grade 3.17
The difference in the histological grades from studies done in different settings is mainly due to the difference in the trend of BC screening practices for the different settings. It is clearly known that delaying in screening for BC contributes significantly to early detection of the disease. This leads to detection of the disease while at an advanced stage with a high grade especially in developing countries.22 Negative health seeking behaviour, lack of awareness and low or lack of knowledge on BC in developing countries, remain the major factors for the current high prevalence of high grade BC in the literature. The reason why the prevalence of BC in patients aged 50 years or younger in developing countries is high compared to western countries could be attributed to the natural history of the disease (tumour biology) which needs further investigation to understand.23
This may include genetical screening for the carrier status of both BRCA1and BRCA2 gene mutations and also a detailed analysis of the risk factors for BC while comparing the pre-and post-menopausal females at risk of developing BC. Regarding histological subtypes of BC in our study, IDC-NST was present in the vast majority of the patients (68.9%). This is similar to the reports from both developed and developing countries. In the previously done studies in Tanzania, Uganda, Nigeria and Norway IDC-NST was found in 88.6%, 89.6% and 78%, 95% and 81.4%, respectively.11,13,14,20,24 This is because BC commonly develops initially from the ducts and occasionally it may develop from lobules. Its pathogenesis may be coupled by formation of different morphogenesis such as formation of mucin, papillary mesenchymal components and metaplastic changes among many others.20
ILC in our study was the second in terms of prevalence which is also similar to many other previously done studies. Four percent, 6.3% and 2.9% of ILC were reported in Uganda, Norway and Tanzania.13,14,17 However, these proportions are very low when compared to the 22.3% of ILC found in the present study. This variation may be due to a difference in diagnostic methods used in the different studies, difference in experience in reporting the histological tissue sections and possible tumour biology of BC in the different countries. The prevalence of other histological types in our study was as low as in many previously done studies.
Expression of HRs varies greatly from one study to another in the same setting and sometimes between different races or geographical areas. The ER expression of 53.4% in the present study is quite higher than 32.7% and slightly lower than 60% which were reported by Galukande et al and Roy et al in Uganda.13,14 In Tanzania, the expression of ER in patients with BC was also reported to vary across different studies in different periods. For example, Mwakigonja et al, Mbonde et al and Rambau et al reported 43%, 33% and 32.7%, respectively.9–11 These findings indicate how the prevalence of ER expression vary across different studies within the same setting. In studies which were done among African women with BC residing in the USA and Britain, it was reported that the prevalence of expression of ER was 61% and 66%, respectively.20,25
Adjei et al reported 76% and 85% expression of ER in a study which was done to compare its expression among Ghanaian and Norwegian women with BC.17 The major reason for the existing difference in expression of ER is the issue of handling the biopsies during the pre-analytical phase. The time taken before fixing of biopsies, the time taken for tissue fixation and ratio of the fixative to the volume of the specimen, have been reported to contribute greatly to affecting the staining ability of the IHC antibodies including ER. Additionally, the difference in study designs, sample size used and genetic composition of the patients may also help to explain the difference in expression of this biomarker.
Of the HRs, ER is usually expressed frequently compared to PR. Most studies have reported the expression of PR to be ranging from 13.9% to 61.3% for both primary and metastatic BCs.26,27 This observation was also similar in the present study. The 46.6% prevalence of expression of PR in our study was similar to the 42.3% that was reported in the study of Rambau et al but higher than 10%, 31.8%, 5.8% and 26.4% expression of PR which were reported in Kenya, India, Uganda and Tanzania, respectively.10–12,14,28 Adjei reported a higher prevalence of expression of PR of 65% in Ghanaian women with BC. The same study also reported that the PR expression in Norwegian women was 82%.17
Hormonal therapy (HT) has been well experimented for early and advanced BC with treatment decisions currently based on the semiquantitative and IHC assessment of HRs expression on histological biopsies. Unproven use of HT in patients with BC has been reported to be of no benefit in improving the prognosis of the patients. Some studies have even reported a possible worsening of prognosis which is more likely to occur as a result of unproven use of HT.29 The prognostic role of ER and PR has been reported to vary. In a study which was done by Purdie et al in United Kingdom (UK), it was found that, PR was a potential predictor of overall survival, breast cancer-specific survival and disease-specific survival. The study reported that patients with negative PR were 3.24 times more likely to die than the ones in whom PR was positive and the difference was statistically significant (95% CI = 2.42–4.34, p<0.0001).29 Furthermore, the same study found that, the prognosis of the patients was poor even in cases who were ER positive provided that PR was negative.
BC cases in whom ER is negative but PR is positive are exceptionally rare and are said to comprise 0.3%. This suggests that the assessment of PR expression in ER-negative tumours in identifying those that might still benefit from ET may not be justified.30 The expression of ER, PR as well as ER and PR co-expression in this study were found to increase with increase in age of the patients. All biomarkers were more expressed in patients who were aged 50 years or above unlike those aged 50 years or younger. These data are all in keeping with a previous study which reported that PR-expressing tumours are more common in post-menopausal women with low-grade, ER-positive, breast cancers who, generally, have a good prognosis.31 Additionally, age was the potential predictor of ER and PR but not co-expression of two biomarkers. These findings may help to provide insightful information regarding preferential use of imperative use of these markers in postmenopausal women with BC unlike premenopausal cases.
Many studies have reported that younger age is an independent factor for poor prognosis in BC.8,32,33 This fact was not different in the current study, where among all the patient characteristics, it was only young age that showed a statistical significance with expression of ER, PR hormones and triple negative breast cancer. Post menopause patients (50 years and over) were 0.39 times less likely not to have triple negative breast cancers, but 3.7 and 3.9 times more likely to show expression of negative ER and PR receptor hormones respectively (Table 5). These findings support the notion that age at diagnosis should be taken into account when studying effects of breast cancer risk factors.34 This study finding is consistent with findings by Fletcher, which reported that age may play a role in increasing risk of developing TNBC. Premenopausal women have been found to develop TNBC more often than postmenopausal women.35 In another similar study conducted in China36 it was revealed that women aged 40 years and below were more likely to be PR positive compared to those aged greater than 40 years which is in agreement with the current study.
HER2-positive BC has a better prognosis than HER2-negative BC. Patients with BC who are pre-menopausal are more likely to be HER2-positive than post-menopausal ones. Also Purdie et al reported that, ER-positive BC cases are more likely to be HER2-positive than PR-negative BC cases.29 The expression of HER of 18.4% in the present study was similar to 18.5% which was reported in Brazil and lower than the 40.7%, 24%, 23.1% and 22% that were reported in India, Ghana, Tanzania and Uganda, respectively.14,17,28 Studies have shown that expression of HER2 in both African American and African patients with BC is higher compared to Caucasians.
For example, in the study done by Adjei et al which was comparing expression of breast markers between Ghanaian and Norwegian women with BC, it was found that, the expression of HER2 in Ghanaian was 24% whereas in Norwegian patients HER2 expression was found in 14%.17 Purdie et al also reported 13.9% of HER2 expression among patients with BC. The difference could be due to the difference in methodology. Studies that involve the use of fluorescent in situ hybridization (FISH) technique in deciding whether the equivocal cases (2+) are truly positive, have reported lower prevalence of HER expression than studies which do not involve the FISH method.
Prediction of expression of HER2 by age, tumour grade and histological type in this study was not having any statistical association. However, the expression of HER2 in this study was higher in patients with ≤50 years than those older than 50 years of age (68.4% versus 31.6%). Also the expression of HER2 in this study was increasing with an increase in the tumour grades but without statistical association (Table 7). Although most studies have reported that patients with BC aged less than 50 years tend to have a higher expression of HER2 than those 50 years or over, however, some studies have shown contradicting results. For example, Arias et al reported that, there was 57.7% and 41.1% of postmenopausal and premenopausal patients with BC that were expressing HER2 and the difference in expression of the biomarker was not statistically significant (p = 0.065).37 Mwakigonja et al reported that the expression of HER2 in the patients with BC aged ≤55 years was 41% compared to 10% for those aged greater than 55 years and the difference was statistically significant (p = 0.079).11 In another study done by Kolečková et al it was also found that the expression of HER2 in patients with BC aged 20–39 years was higher than those greater than 50 years of age.38
HER2 expression in our study was increasing with an increase in the tumour grades. However, the increase in expression was not statistically significant (Table 7). This is in line with the finding in the study done by Rao et al39 in India who also reported that HER2 overexpression was higher among cases with grade 3 than those with either grade 2 or 1 but the difference in expression was statistically significant (p<0.05). Parise et al also reported that the risk of patients with BC that were expressing HER2 in the study was 3.9 compared to 2.7 of the ones who were not expressing HER2.40
TNBC carries the worst prognosis of all the molecular subtypes of BC (Luminal A, B, C, HER2 and TNBC). TNBC is an aggressive disease, recurring and metastasizing more often than other kinds of BCs.41 Patients with BC who fall in this category of being triple negative (TN), they do not respond to either hormonal therapy or targeted therapy such as trastuzumab which usually is of prognostic value for those patients with BC who can express HER2. The prevalence of TNBC in this study of 37.9% was almost similar to 36%, 34% and 38.4% which were previously reported in Uganda and Tanzania, respectively.10,13,14 Slightly higher prevalences of TNBC of 41%, 45.6% and 50% were reported previously in Uganda, Tanzania and India, respectively.11,39,42 The reasons for higher rates of TNBC are not well understood, however, partly they may include genetical predisposition and difference in methodology used in determining the expression of the breast markers. Adjei et al reported that the prevalence of TNBC in Ghanaian women with BC was 3 times more than Norwegian women with BC (22% versus 7%).17 This finding indicates the fact that, there are many patients who are TN from the African race unlike in the population of the whites.
Age was the potential predictor of TNBC in this study. Patients aged 50 years or younger, were 4.4 times more likely to have TNBC than those older than 50 years of age and the difference was statistically significant (p = 0.009). This observation is similar to the findings in the study by Wang et al which was done in China which found that, the prevalence of TNBC in patients aged ≤40 years was 13.8% compared to 7.1% found in patients older than 40 years but the difference in having TNBC between the two age groups was not statistically significant (p = 0.443).43 Salman et al also reported a larger number of Hispanic patients younger than 40 years compared to non-Hispanics who had TNBC in a study which was done in the USA (P = 0.002).44 In another study, which was done in United Kingdom (UK), it was found that, patients with TNBC had the worst prognosis than the rest of the molecular subtypes.40
Tumour grading in our study showed no statistical association with occurrence of TNBC in the cases. However, as the tumour grades were increasing, the number of cases with TNBC was also increasing. This observation is similar to the finding in the study of Rao et al which reported that, patients with high grade (grade 3) were found to have TNBC compared to the rest of the grades and the difference was statistically significant (p<0.05).39 On the other hand, histological types were not the predictor of TNBC in this study despite that there are more IDC-NST type cases that had TNBC (Table 8).
Breast cancer therapy (BCT) depends on the main three factors which include tumour stage, HRs and HER2 status, and patient’s preference. About 90% of the patients with BC do not have metastatic disease at initial diagnosis.45 BCT may either be local or systemic depending on the clinical stage of the patient. For local BC, surgical removal of the primary tumour with regional axillary lymph node dissection followed by radiotherapy is the mainstay modality of management.45 The purpose of postoperative radiotherapy is to prevent recurrence of the cancer. On the other hand, systemic therapy may be preoperative (neoadjuvant), postoperative (adjuvant), or both.
BCT is different among patients with BC depending on the expression of HRs (either ER or PR) and HER2. A majority of HRs-positive patients receive HT (eg, tamoxifen and aromatase inhibitors) and a minority of them receive HR in combination with chemotherapy.45 Patients who are HER2-positive receive HER2-targeted therapy (eg, trastuzumab) in combination with chemotherapy and patients with TNBC are treated with chemotherapy alone.45
The survival of patients with BC is greatly influenced by both clinical stage and also status of the biomarkers (HRs and HER2).45 For example, the median overall survival for patients with metastatic TNBC is one year whereas for patients with other molecular subtypes (HRs-and HER2-positive) the rate is 5 years.45 Furthermore, it has also been found that, the 5-year BC-specific survival for patients with clinical stage I is ≥99%, ≥94% and ≥85% for HRs-positive, HER2-positive, and TNBC patients, respectively.45
Lorusso and co-workers reported the use of liposomal anthracyclines in the management of metaplastic breast carcinoma (MBC) and other histological types of BC which are locally advanced.46 The addition of a liposomal component to the conventional anthracyclines came into practice after it was proved that the conventional one was found to have a potential cardiotoxicity effect. Therefore, addition of liposomes aims at encapsulating the drugs in order to prevent rapid dissolving of the drugs.
Both liposomal doxorubicin (LD) and pegylated liposomal doxorubicin (PLD) formulations of the liposomal anthracyclines have been found to prevent complications caused by conventional anthracyclines including myelosuppression, alopecia, nausea, vomiting, stomatitis and mostly cardiotoxicity.46 This is because conventional anthracyclines were found to be associated with fatal congestive heart failure as a result of cardiotoxicity.46 The therapeutic advantages resulting from the use of PLD are reduced time to BC progression, improving overall survival and promising response rate.46
Limitations
We were unable to control issues related to the pre-analytical phase including fixation time, cold ischemic time, tissue storage and thickness of the sections during grossing altogether may have affected the quality of the immuno-staining results. Because of the nature of the study being retrospective, we were not able to obtain other variables such as tumour stage, lymph node status and tumour size among many others which would have increased the power of the methodology. Additionally there were financial constraints, including lack of proliferation biomarkers such as Ki67 would have helped to perform molecular subtyping of the BC in our study.
Conclusion
The majority of patients with BC in our study were aged 50 years or younger and they had a high grade of the disease. Furthermore, these patients had TNBC and had a high prevalence of HER2 expression compared to the patients older than 50 years of age. This indicates that a significant number of women with BC in developing countries are younger and carry molecular subtypes of BC with a poor prognosis. Age was a strong predictor for expression of ER, PR and occurrence of TNBC among the cases included in our study.
Data Sharing Statement
The datasets used in this study are available from the corresponding author and they may be provided when requested.
Ethics Approval
All procedures performed in this study were in accordance with the ethical standards of the Ethics Committee of Makerere College of Health Sciences (MakCHS).
Consent to Participate
Written consent for us to use the FFPE tissue blocks was obtained from the patients and it has been kept for review by the editor-in-chief if needed. Patient consent was also informed consent, and this study was conducted in accordance with the Declaration of Helsinki.
Acknowledgments
We thank Mr. Peres for performing IHC staining and also Mr. Noel Namuhani for working with statistics.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed on the journal to which the article will be submitted; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This research did not receive funding from any source.
Disclosure
The authors declare that they have no competing interests.
References
1. Brinton LA, Sherman ME, Carreon JD, Anderson WF. Recent trends in breast cancer among younger women in the United States. J Natl Cancer Inst. 2008;100(22):1643–1648.
2. Fitzmaurice C, Akinyemju TF, Al Lami FH, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2016. A systematic analysis for the global burden of disease study. JAMA Oncol. 2018;4(11):1553–1568. doi:10.1001/jamaoncol.2018.2706
3. Akarolo-Anthony SN, Ogundiran TO, Adebamowo CA. Emerging breast cancer epidemic: evidence from Africa. Breast Cancer Res. 2010;12(4):S8. doi:10.1186/bcr2737
4. El Saghir NS, Khalil MK, Eid T, et al. Trends in epidemiology and management of breast cancer in developing Arab countries: a literature and registry analysis. Int J Surg. 2007;5(4):225–233. doi:10.1016/j.ijsu.2006.06.015
5. Chouchane L, Boussen H, Sastry KS. Breast cancer in Arab populations: molecular characteristics and disease management implications. Lancet Oncol. 2013;14(10):e417–e424. doi:10.1016/S1470-2045(13)70165-7
6. Cancello G, Maisonneuve P, Rotmensz N, et al. Prognosis and adjuvant treatment effects in selected breast cancer subtypes of very young women (< 35 years) with operable breast cancer. Ann Oncol. 2010;21(10):1974–1981.
7. Azim HA, Partridge AH. Biology of breast cancer in young women. Breast Cancer Res. 2014;16(4):427. doi:10.1186/s13058-014-0427-5
8. Gnerlich JL, Deshpande AD, Jeffe DB, Sweet A, White N, Margenthaler JA. Elevated breast cancer mortality in women younger than age 40 years compared with older women is attributed to poorer survival in early-stage disease. J Am Coll Surg. 2009;208(3):341–347. doi:10.1016/j.jamcollsurg.2008.12.001
9. Mbonde MP, Amir H, Schwartz-Albiez R, Akslen LA, Kitinya JN. Expression of estrogen and progesterone receptors in carcinomas of the female breast in Tanzania. Oncol Rep. 2000;7(2):277–360.
10. Rambau P, Masalu N, Jackson K, Chalya P, Serra P, Bravaccini S. Triple negative breast cancer in a poor resource setting in North-Western Tanzania: a preliminary study of 52 patients. BMC Res Notes. 2014;7(1):399. doi:10.1186/1756-0500-7-399
11. Mwakigonja AR, Lushina NE, Mwanga A. Characterization of hormonal receptors and human epidermal growth factor receptor-2 in tissues of women with breast cancer at Muhimbili National Hospital, Dar es salaam, Tanzania. Infect Agent Cancer. 2017;12(1):60. doi:10.1186/s13027-017-0170-5
12. Bird P, Hill A, Houssami N. Poor hormone receptor expression in East African breast cancer: evidence of a biologically different disease? Ann Surg Oncol. 2008;15(7):1983. doi:10.1245/s10434-008-9900-7
13. Roy I, Othieno E. Breast carcinoma in Uganda: microscopic study and receptor profile of 45 cases. Arch Pathol Lab Med. 2011;135(2):194–199.
14. Galukande M, Wabinga H, Mirembe F, Karamagi C, Asea A. Molecular breast cancer subtypes prevalence in an indigenous Sub Saharan African population. Pan Afr Med J. 2014;17:249–330. doi:10.11604/pamj.2014.17.249.3305
15. Meyer JS, Alvarez C, Milikowski C et al. Breast carcinoma malignancy grading by Bloom–Richardson system vs proliferation index: reproducibility of grade and advantages of proliferation index. Modern Pathology. 2015;18:1067–1078.
16. Wolff AC, Hammond MEH, Schwartz JN, et al. American society of clinical oncology/college of American pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. Arch Pathol Lab Med. 2007;131(1):18–43.
17. Adjei EK, Owusu‐Afriyie O, Awuah B, Stalsberg H. Hormone receptors and Her2 expression in breast cancer in Sub-Saharan Africa. A comparative study of biopsies from Ghana and Norway. Breast J. 2014;20(3):308–311. doi:10.1111/tbj.12261
18. Salhia B, Tapia C, Ishak EA, et al. Molecular subtype analysis determines the association of advanced breast cancer in Egypt with favorable biology. BMC Women’s Health. 2011;11(1):44. doi:10.1186/1472-6874-11-44
19. Awadelkarim K, Arizzi C, Elami E, et al. Pathological, clinical and prognostic characteristics of breast cancer in Central Sudan versus Northern Italy: implications for breast cancer in Africa. Histopathology. 2008;52(4):445–456. doi:10.1111/j.1365-2559.2008.02966.x
20. Albrektsen G, Heuch I, Thoresen SØ. Histological type and grade of breast cancer tumors by parity, age at birth, and time since birth: a register-based study in Norway. BMC Cancer. 2010;10(1):226. doi:10.1186/1471-2407-10-226
21. Kennedy S, O’Driscoll L, Purcell R, et al. Prognostic importance of survivin in breast cancer. Br J Cancer. 2003;88(7):1077–1083.
22. Babu GR, Samari G, Cohen SP, et al. Breast cancer screening among females in Iran and recommendations for improved practice: a review. Asian Pac J Cancer Prev. 2011;12(7):1647–1655.
23. Fredholm H, Eaker S, Frisell J, Holmberg L, Fredriksson I, Lindman H. Breast cancer in young women: poor survival despite intensive treatment. PLoS One. 2009;4(11):e7695. doi:10.1371/journal.pone.0007695
24. Ntekim A, Nufu F, Campbell O. Breast cancer in young women in Ibadan, Nigeria. Afr Health Sci. 2009;9(4):242–246.
25. Chu KC, Anderson WF. Rates for breast cancer characteristics by estrogen and progesterone receptor status in the major racial/ethnic groups. Breast Cancer Res Treat. 2002;74(3):199–211. doi:10.1023/A:1016361932220
26. Ikpatt O, Ndoma-Egba R. Oestrogen and progesterone receptors in Nigerian breast cancer: relationship to tumour histopathology and survival of patients. Cent Afr J Med. 2003;49(11):122–126.
27. Stierer M, Rosen H, Weber R, Hanak H, Spona J, Tüchler H. Immunohistochemical and biochemical measurement of estrogen and progesterone receptors in primary breast cancer. Correlation of histopathology and prognostic factors. Ann Surg. 1993;218(1):13. doi:10.1097/00000658-199307000-00004
28 Bansal C, Sharma A, Pujani M, et al. Correlation of hormone receptor and human epidermal growth factor Receptor-2/neu expression in breast cancer with various clinicopathologic factors. Indian J Med Paediatr Oncol. 2017;38(4):483. doi:10.4103/ijmpo.ijmpo_98_16
29. Purdie C, Quinlan P, Jordan L, et al. Pro gesterone receptor expression is an independent prognostic variable in early breast cancer: a population-based study. Br J Cancer. 2014;110(3):565–572.
30. Nguyen VH, Lawrence HJ. Use of gabapentin in the prevention of taxane-induced arthralgias and myalgias. J Clin Oncol. 2004;22(4):1767–1769. doi:10.1200/JCO.2004.99.298
31. Liu Y, Gao H, Marstrand TT, et al. The genome landscape of ERα-and ERβ-binding DNA regions. Proc Natl Acad Sci U S A. 2008;105(7):2604–2609. doi:10.1073/pnas.0712085105
32. Lobbezoo DJ, van Kampen RJ, Voogd RJ, et al. Prognosis of metastatic breast cancer subtypes: the hormone receptor/HER2-positive subtype is associated with the most favorable outcome. Breast Cancer Res Treat. 2013;141(3):507–514. doi:10.1007/s10549-013-2711-y
33. Carey LA, Perou CM, Livasy CA, et al. Race, breast cancer subtypes, and survival in the carolina breast cancer study. JAMA. 2006;295(21):2492–2502. doi:10.1001/jama.295.21.2492
34. Tryggvadottir L, Tulinius H, Eyfjord JE, Sigurvinsson T. Breast cancer risk factors and age at diagnosis: an Icelandic cohort study. Int J Cancer. 2002;98(4):604–608. doi:10.1002/ijc.10217
35. Baum JE, Sung KJ, Tran H, Song W, Ginter PS. Mammary epithelial-myoepithelial carcinoma: report of a case with HRAS and PIK3CA mutations by next-generation sequencing. Int J Surg Pathol. 2019;27(4):441–445. doi:10.1177/1066896918821182
36. Wang J, Sang D, Xu B, et al. Value of breast cancer molecular subtypes and Ki67 expression for the prediction of efficacy and prognosis of neoadjuvant chemotherapy in a Chinese population. Medicine. 2016;95(18):234–241.
37. Kolečková M, Kolář Z, Ehrmann J, Kořínková G, Trojanec R. Age-associated prognostic and predictive biomarkers in patients with breast cancer. Oncol Lett. 2017;13(6):4201–4207. doi:10.3892/ol.2017.6000
38. Arias VEA, Gobbi H, Ioshii SO, et al. Assessment of HER-2 status in invasive breast cancer in Brazil. Revista Da Associação Médica Brasileira. 2017;63(7):566–574. doi:10.1590/1806-9282.63.07.566
39. Rao C, Shetty J, Prasad HK. Morphological profile and receptor status in breast carcinoma: an institutional study. J Cancer Res Ther. 2013;9(1):44. doi:10.4103/0973-1482.110358
40. Parise CA, Caggiano V. Breast cancer survival defined by the ER/PR/HER2 subtypes and a surrogate classification according to tumor grade and immunohistochemical biomarkers. J Cancer Epidemiol. 2014;5(3):421–431.
41. Dent R, Hanna WM, Trudeau M, Rawlinson E, Sun P, Narod SA. Pattern of metastatic spread in triple-negative breast cancer. Breast Cancer Res Treat. 2009;115(2):423–428. doi:10.1007/s10549-008-0086-2
42. Nalwoga H, Arnes J, Wabinga H, Akslen L. Expression of aldehyde dehydrogenase 1 (ALDH1) is associated with basal-like markers and features of aggressive tumours in African breast cancer. Br J Cancer. 2010;102(2):369–375. doi:10.1038/sj.bjc.6605488
43. Wang B, Wang X, Zou Y. Association between hormone receptors and HER-2/neu is age-related. Int J Clin Exp Pathol. 2015;8(7):8472.
44. Salman O, Alok Kumar D, Anthony LN, Andres A, Gayathri N. Prognostic impact of age at diagnosis in triple negative breast cancer: analysis of 204 patients from single institution registry. J Clin Oncol. 2018;36(15):154–156.
45. Waks AG, Winer EP. Breast cancer treatment: a review. JAMA - J Am Med Assoc. 2019;321:288–300. doi:10.1001/jama.2018.19323
46. Lorusso V, Manzione L, Silvestris N. Role of liposomal anthracyclines in breast cancer. Ann Oncol. 2007;18:70–73. doi:10.1093/annonc/mdm229
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

