Back to Journals » Neuropsychiatric Disease and Treatment » Volume 12
HIV- and AIDS-associated neurocognitive functioning in Zambia – a perspective based on differences between the genders
Authors Kabuba N, Menon JA, Franklin Jr DR, Heaton RK, Hestad KA
Received 31 January 2016
Accepted for publication 19 April 2016
Published 11 August 2016 Volume 2016:12 Pages 2021—2028
DOI https://doi.org/10.2147/NDT.S105481
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Roger Pinder
Norma Kabuba,1,2 J Anitha Menon,1 Donald R Franklin Jr,3 Robert K Heaton,3 Knut A Hestad2,4,5
1Department of Psychology, The University of Zambia, Lusaka, Zambia; 2Department of Psychology, Norwegian University of Science and Technology, Trondheim, Norway; 3Department of Psychiatry, University of California, San Diego, CA, USA; 4Department of Research, Innlandet Hospital Trust, Hamar, Norway; 5Department of Public Health, Hedmark University of Applied Sciences, Elverum, Norway
Abstract: Human immunodeficiency virus (HIV) infection and acquired immune deficiency syndrome (AIDS) are frequently associated with neurocognitive impairment (NCI). However, few studies have examined the interrelationship between gender and NCI in the HIV and AIDS population. This cross-sectional study examined the neurocognitive (NC) functioning of HIV-infected male and female adults from urban Zambia. The participants included 266 HIV seropositive (HIV+) adults (males [n=107] and females [n=159]). Participants completed NC assessment by means of a comprehensive test battery using normative data from 324 HIV-seronegative (HIV-) controls. The norms corrected for effects of age, education, and gender in the general population, and the test battery measures domains of attention/working memory (learning and delayed recall), executive function, verbal fluency, processing speed, verbal and visual episodic memory, and fine motor skills. An overall comparison of the HIV+ male and female participants yielded no statistically significant differences. Analysis of covariance results controlling for disease characteristics showed that HIV+ female participants had worse delayed recall scores than males, F(1,117) =9.70, P=0.002, partial ƞ2=0.077. The females also evidenced a trend toward greater impairment on learning efficiency (P=0.015). The findings suggest that there are gender-related differences in NCI after controlling for disease characteristics. It was observed that although the HIV+ females enjoyed better health compared to their HIV+ male counterparts, they still had worse performance on the neuropsychological tests. This implies that HIV may have more NC consequences for Zambian females than males.
Keywords: HIV-1, neurocognitive functioning, gender, Zambia
Introduction
Statistics at the end of 2010 indicated that globally, 34 million people were living with HIV, with the worst hit region being sub-Saharan Africa.1 Reports also reflect disparities regarding rates of infection among men and women, and these too, show regional differences across the globe. For example, it is reported that in sub-Saharan Africa, nearly 60% of those infected with HIV are women, whereas in Latin America, Eastern Europe/Central Asia, and Asia, only 30%–35% of those affected are women.1,2
Sub-Saharan Africa, especially in its southern regions, has the world’s highest prevalence of HIV infection. Zambia is listed among the countries with the worst HIV and AIDS epidemics in this region.3 The majority of those infected with HIV in Zambia are females, which has led some researchers to observe that “the epidemic in Zambia has a female face”.4
The first AIDS diagnosis in Zambia was reported in 1984, and this was followed by a sharp rise in prevalence estimates.5 By 2005, it was estimated that the prevalence of HIV in Zambia was twice as high in urban areas as it was in rural areas.5,6 According to the Zambia Ministry of Health/National AIDS Council,7 sex disparities have been reported in the prevalence of HIV and AIDS, with a higher proportion of Zambian women (16.1%) suffering from HIV/AIDS compared to men (12.3%).
HIV-1 subtype C is of particular interest in the current study because it is predominant in Central, East, and Southern Africa, including Zambia, from which our sample is drawn. Furthermore, subtype C currently accounts for more than half of all the HIV infections worldwide, which is more than all the other subtypes combined.8 However, less research has been done on this subtype than subtype B, which dominates Europe and the US.
HIV is known to affect the central nervous system (CNS), and it has been reported that 35%–50% of infected individuals eventually show neurocognitive (NC) alterations.9–12 Neuropathology and neuroimaging studies have documented a loss of neurons, especially in the frontal cortex and basal ganglia areas, with cerebral atrophy and demyelination of the white matter, particularly in patients with advanced infection and histories of severe immunosuppression.12,13 The associated cognitive changes have typically involved attention/working memory, speed of information processing, psychomotor speed, learning, delayed recall, and executive functioning.12 Neurocognitive impairment (NCI) in HIV is also frequently characterized by a decline in the ability to function in everyday activities, including the ability to perform in employment and other cognitively demanding tasks.14–16
There are a few studies that have examined how cognitive changes are manifested according to gender in relation to HIV and AIDS,12 and these have yielded somewhat conflicting results. Some studies have reported no differences between the genders in relation to the effects of HIV on neurocognition,17 whereas other studies have reported a higher prevalence of NCI among HIV-positive women.2 Previous studies carried out in Zambia18,19 have also revealed more HIV-related impairment in women relative to men. Seropositive females were reported to be significantly more impaired in neuropsychological tests compared to their male counterparts. Reports of both studies, however, are quick to point out that there is need for larger and more comprehensive studies to verify possible differences between the genders in HIV-related NC impairment. Also, there is a need for such studies to include NC normative corrections to control for performance differences related to gender, age, and education within the general (HIV uninfected) population.
Given the huge toll that HIV has taken on the populations of the world, and especially in its CNS manifestations, it is important to make strides in understanding possible differences between the genders in NC outcomes. This will enable health care professionals to provide gender specific management and treatment for people infected with HIV and AIDS.
The aim of the current cross-sectional study was to address whether there were differences between the genders in cognitive ability in a large sample of antiretroviral therapy (ART)-treated HIV-seropositive (HIV+) men and women in urban Zambia. We used a comprehensive NC test battery that has normative standards which control for demographic influences that exist in normal HIV-seronegative (HIV-) Zambian adults. Results were considered in relation to potentially relevant disease and treatment factors. We hypothesized that the seropositive females would be more cognitively impaired than the seropositive males.
Method
Participants
Our HIV+ sample was drawn from six urban clinics in the Zambian capital city Lusaka: Chilenje, Chipata, Kabwata, Kalingalinga, Matero Main, and Matero Referral clinics. The clinics were chosen because they routinely provide HIV counseling and testing services as well as treatment. All these clinics are under the management of the Lusaka District Health Management Team in Zambia. ART had been prescribed free of charge in these public health care centers in Zambia since 2004.20
Inclusion and exclusion criteria
Inclusion
- HIV status – All study participants were HIV+ and on ART. Information about HIV and treatment status was based on the participants’ medical files.
- Education level – The eligible participants were required to have a minimum of 5 years of formal education. English is the primary language of instruction in the Zambian school system, and the testing was performed in English.
- Age range – All the participants were required to be between 20 and 65 years of age (to conform to the age range of the HIV- controls who participated in the Zambian NC norming study).21
Exclusion
- History of neurological disorders – Individuals with a history of non-HIV-related neurological problems, such as epilepsy, closed head injury, and coma for any reason, were excluded from the study. This information was obtained using a neurobehavioral Medical Screen Form, which assesses past medical and neurological histories.22
- History of drug abuse – Individuals with a history of drug abuse were excluded from the study. This information was obtained using a structured Substance Use form.23,24
- Physical disabilities – Individuals with obvious physical disabilities were excluded from the study to minimize on the possibility of test performance requiring motor dexterity being impaired due to the handicap.
The target sample size was 324 participants, but only 266 HIV+ participants were included in the current study because of some key missing pieces of information (owing to cases of spoiled data on the computer versions of the Category and Wisconsin Card Sorting tests), thus 58 participants were excluded at the time of analysis. The proportion of males and females in our study was consistent with reports for the general HIV+ population in Zambia (ie, 40% males and 60% females).6 All the participants were on ART, and the age range of the participants was from 21 to 65 years (M=40.67, standard deviation [SD] =8.74). Education range, in number of years of formal education attained, was between 5 and 20 years (M=9.9, SD =2.24).
Procedure
The recruitment process was carried out with the assistance of nurses at each clinic who identified participants meeting the inclusion criteria. Once informed consent was obtained, the participants were referred to one of ten Neuropsychology Master of Science students from University of Zambia, who had received extensive training in interviewing, as well as administration and scoring of the NC tests. The testing process for each participant took approximately 2 hours 30 minutes.
The first part of the testing process involved obtaining the participants’ demographic characteristics, medical, and psychiatric information based on self-report. Medical details were confirmed by the patients’ medical record provided by the medical personnel. Administration of NC tests of the test battery was carried out in the same order for all participants, and they were compensated the Zambian Kwacha equivalent of US$8 for transport and refreshment allowance at the end of the testing process.
Measures
Cognitive functioning
Cognitive functioning was measured using an NC test battery that measures cognition across the seven ability domains that have been identified as frequently affected in HIV-associated neurocognitive disorders:25 Executive Functioning (Stroop Color–Word Interference trial, Category Test errors, Wisconsin Card Sorting Test – 64 Total errors, and Color Trails 2); Working Memory/Attention (Paced Auditory Serial Addition Test – 50 (PASAT) and Wechsler Memory Scale-III Spatial Span Test); Speed of Information Processing (Wechsler Adult Intelligence Scale-III [WAIS-III], Digit Symbol, WAIS-III Symbol Search, Trails A, Color Trails 1, Stroop Color Naming and Stroop Word Naming), Verbal fluency (Letter fluency, Animal fluency, and Action fluency); Learning (Hopkins Verbal Learning Test – Revised [HVLT-R] learning and Brief Visuospatial Learning Test – Revised [BVMT-R] learning); Delayed recall (HVLT-R delay and BVMT delay); and complex Motor Function (Grooved Pegboard [dominant and nondominant hands]). The test battery is appropriate for the current study because it measures the domains typically affected by HIV.26 It is an international well-recognized NC assessment tool that has been translated into multiple languages around the world.10,14,18,24,27 The battery has been adapted and normed for the Zambian population.21
Test items such as those on the HVLT-R were adapted to make them more culturally appropriate for Zambia. For instance, all the precious stones in the learning trial of the test were changed to metals that are common in Zambia (copper, iron, lead, and zinc). In the recognition trial, steel and bronze were added.21,23
Disease characteristics
Participants were categorized according to whether their HIV viral loads were detectable or undetectable. Viral load was detected at 50 copies/mL. This information was obtained from the patients’ medical files and is considered here because previous studies have reported HIV viral load detectability as an induction of effective therapy.28,29
Information on duration of ART was obtained from the patients’ medical files.
CD4 count included nadir CD4 ranging from 1 cells/mm3 to 727 cells/mm3, and current CD4 taken at the time of testing for this study ranging from 0 cells/mm3 to 2,287 cells/mm3.
AIDS status constituted participants with AIDS and those without AIDS; this information was obtained from the participants’ medical files. AIDS is diagnosed in Zambia when an HIV-infected individual has a CD4 count below 200 cells/mm3 of blood, weakening the immune system and putting the individual at risk of illnesses and infections that are AIDS defined according to the World Health Organization (WHO) stages (WHO Stages 3 and 4 condition).30,31
Nutritional information such as body mass index (BMI) has been linked to NC functioning.26 In the current study, BMI categories were based on the WHO classification: BMI values of <18.50 are regarded as low, 18.50–24.99 is regarded as normal, ≥25 is overweight, and ≥30 is obese.32
Tuberculosis (TB) is a common comorbid factor in HIV in sub-Saharan Africa and is reported to have an effect on NC functioning.33 In the current study, TB status was obtained from the patients’ medical files.
Ethical consideration
The study was approved by the University of Zambia Biomedical Research Ethics Committee. The research was also formally approved by the Lusaka District Health Management Team, which oversees the clinics in Lusaka and the Ministry of Health.
Written informed consent was obtained from all research participants. Participants had the ability to take breaks or withdraw from the study at any time with no penalty incurred. All the data that was recorded was anonymous. The participants were assigned an arbitrary code for analysis purposes.
Data management
The raw data that was obtained on the neuropsychological test battery was converted into demographically corrected T-scores based on data previously collected from 324 healthy Zambians. The 324 healthy sample comprised 157 (48.5%) males and 167 (51.5%) females, with an average age of 38.5 (SD =12.80) years and an average education level of 11.0 (SD =2.58) years. The norming process was similar to that used for the US normative data.21,23 The raw scores were corrected for the effects of age, education, sex, and urban/rural background by first converting them to normally distributed scaled scores with a mean of 10 and SD of 3; the scaled scores were then converted to demographically corrected T-scores with a mean of 50 and SD of 10. Detailed procedures and results of the norming study have been reported elsewhere.21
Global Deficit Scores were used as an alternative method to determine the NCI levels of the participants.34 Global Deficit Score is a mean of impairment ratings that uses demographically corrected T-scores on a five-point scale from normal to severely impaired. A deficit score of 0 means normal performance (T-score ≥40), whereas a deficit score of 1 means mild impairment (T-score =35–39), 2 means mild-to-moderate impairment (T-score =30–34), 3 means moderate impairment (T-score =25–29), 4 means moderate-to-severe impairment (T-score =20–24), and 5 means severe impairment (T-score <20). Participants were classified as impaired in an ability domain if they had an average deficit score ≥0.5 on that particular cognitive domain. This average is called the Domain Deficit Score (DDS). Participants were further classified as having global impairment if they had a total average deficit score ≥0.5 across all domains.34–36
The use of the “deficit score” approach reflects our focus on abilities that may have been affected by CNS injury or disease. It has been used in many previous studies of HIV-associated neurocognitive disorders and, similar to clinical ratings of NC results (which does not allow for good/normal performances on some tests or domains obscure problematic results on others), purposely gives less weight to high test scores in the normal range.34
Data analysis
All the data in this study was analyzed using the Statistical Package for Social Sciences version 20 (IBM Corporation, Armonk, NY, USA). The statistical package was used to obtain the distribution of the participant’s demographics and disease characteristics. It was also used to compute independent t-tests comparing males versus females within the HIV+ sample and to generate Chi-square analyses for the HIV+ male and female disease characteristics. Analyses of covariance were computed to compare male and female NC functioning while controlling for disease characteristics.
Results
Demographics
The HIV+ male participants were older (M=42.37, SD =9.37) than the HIV+ female participants (M=39.5, SD =8.11; P=0.009) and had more years of education (M=10.47, SD =2.33) than the HIV+ female participants (M=9.67, SD =2.12; P=0.004). However, the effects of “normal” age, education, and sex on the NC test performances were controlled for by using demographically corrected standard scores (T-scores) generated with a previously collected 324 HIV- normative sample.21
Disease characteristics based on sex
To determine disease characteristics based on gender, independent t-tests were computed for the continuous variables, such as current CD4 count, nadir CD4 count, and duration on ART. Chi-square tests were carried out for the dichotomous disease characteristics such as viral load detected/undetected, AIDS status, BMI, and TB status.
Current CD4 counts were statistically different between the males (mean =396.78, SD =235.52) and females (mean =539.02, SD =230.71) P≤0.001. Nadir CD4 counts were not statistically different between the males (mean =180.87, SD =136.92) and females (mean =215.93, SD =156.07), P=0.108.
Duration on ART was not statistically different between the males (mean =52.96, SD =32.75) and females (mean =55.95, SD =31.42), P=0.506.
Table 1 outlines the disease and immune characteristics of the HIV+ participants stratified by gender.
Chi-square tests for independence with Yates continuity correction (Table 1) and independent t-test analyses revealed statistically significant differences with regard to gender and disease characteristics for viral load, AIDS status, TB status, BMI, and current CD4. Males were more likely to have AIDS, detectable viral loads, had more current immunosuppression (lower CD4 cell counts), and were more likely to have TB coinfection, whereas females were more likely to be overweight. Thus, the males were sicker and had a worse immunological status, both at the inception of ART and also at the time of testing for the current study when compared to the female participants. We further sought to determine how these aforementioned disease characteristics may have impacted on NC functioning in our seropositive male and female samples.
Overall NC functioning
Using T-scores, we examined whether there were any genderrelated cognitive differences in our seropositive participants on overall NC functioning. Results obtained for the seven cognitive domains and the global mean score are presented in Table 2.
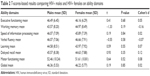  | Table 2 T-scores-based results comparing HIV+ males and HIV+ females on ability domains |
Results in Table 2 indicated that there were no statistically significant differences between the HIV+ males and females on the overall and domain T-scores in neuropsychological test performance. Similar results were also obtained when the HIV+ males and females were compared using DDS (data not shown).
Disease characteristics and NC functioning of the HIV+ males and females
One-way analyses of covariance to compare the performance of males and females on NC functioning were carried out while controlling for differences in disease characteristics. The grouping variable was gender. The intention was to look at differences between males and females while controlling for covariates, these being disease characteristics associated with HIV infection. Dependent variables were NC mean T-scores and DDS across the seven domains. Covariates were disease characteristics: categorical variables (detectable/undetectable viral load, AIDS, and TB status) and continuous variables (nadir CD4, current CD4, duration on ART, and BMI).
Statistically significant results were observed on the following domains.
Mean T-scores
Learning mean T-score: There was a statistically significant effect of gender F(1,117) =7.42, P=0.007, partial η2=0.06, with an adjusted mean T-score for males of 46.62 (standard error [SE] =0.96) and females of 43.02 (SE =0.84). There were no statistically significant effects for the covariates, detectable/undetectable viral load, AIDS and TB status, nadir CD4, current CD4, duration on ART, and BMI.
Delayed recall mean T-score: There was a statistically significant effect of gender, F(1,117) =8.78, P=0.004, partial η2=0.070, with an adjusted mean T-score for males of 47.99 (SE =1.05) relative to 43.68 (SE =0.92) in the female group. A statistically significant effect was also obtained for the covariate TB, F(1,117) =3.99, P=0.048, partial η2=0.033, indicating more TB in the male group. There were no statistically significant effects of the other covariates, detectable/undetectable viral load, AIDS status, nadir CD4, current CD4, duration on ART, and BMI on recall mean T-score.
Motor mean T-score: There was no statistically significant effect of gender, F(1,117) =0.394, P=0.531, partial η2=0.003. Statistically significant effects were found for the covariates current CD4 count, F(1,117) =9.27, P=0.003, partial η2=0.073, and nadir CD4 count, F(1,117) =6.27, P=0.011, partial η2=0.054, with an adjusted mean T-score for males of 53.65 (SE =1.45) and females of 52.39 (SE =1.26). The other covariates, detectable/undetectable viral load, AIDS status, TB status duration on ART, and BMI, did not have a statistically significant effect on the motor mean T-score.
Speed of information processing T-score: There was no statistically significant effect of gender, F(1,117) =2.24, P=0.123, partial η2=0.020. A statistically significant effect was found for the covariate current CD4 count, F(1,117) =4.93, P=0.028, partial η2=0.040, with an adjusted mean T-score for males of 48.09 (SE =1.02) and females of 45.89 (SE =0.894). There were no statistically significant effects of the other covariates: undetectable/detectable viral load, AIDS status, TB status, nadir CD4, duration on ART, and BMI on speed of information processing T-score.
Global mean T-score: There was no statistically significant effect of gender F(1,117) =2.93, P=0.089, partial η2=0.024. A statistically significant effect was found for current CD4 count, F(1,117) =5.91, P=0.012, partial η2=0.048, with an adjusted mean T-score for males: 48.14 (SE =0.76) and females: 46.35 (SE =0.66). There were no statistically significant effects of the other covariates such as undetectable/detectable viral load, AIDS status, TB status, nadir CD4, duration on ART, and BMI on the global mean T-score.
Domain deficit scores
Learn mean DDS: There was no statistically significant effect of gender F(1,117) =2.79, P=0.097, partial η2=0.023. A statistically significant effect was found for the covariate duration on ART, F(1,117) =6.09, P=0.015, partial η=0.049, with an adjusted mean T-score for males: 0.333 (SE =0.095) and females: 0.552 (SE =0.083). The other covariates, detectable/undetectable viral load, AIDS status, TB status, nadir CD4, current CD4, and BMI, did not have statistically significant effects on learn mean DDS.
Delayed recall mean DDS: There was a statistically significant effect for gender, F(1,117) =9.70, P=0.002, partial η2=0.077, with an adjusted mean T-score for males of 0.236 (SE =0.094) and for females of 0.641 (SE =0.082). There were no statistically significant effects for the covariates such as detectable/undetectable viral load, AIDS and TB status, nadir CD4, current CD4, duration on ART, and BMI on recall mean DDS.
Discussion
NC functioning of HIV+ males compared to HIV+ females
Unadjusted comparisons of the HIV+ males and females on both the T-scores and DDS did not yield any significant differences between the two groups. The results obtained in this regard are in agreement with some previous studies that have shown no overall differences between HIV+ males and females,17,37,38 but were at odds with those that were previously reported in Zambia, suggesting significant gender differences in NC functioning owing to HIV infection. Possible reasons for this disparity could be that previous studies had smaller sample sizes, did not utilize Zambian norms, and/or did not employ a comprehensive test battery.19,18 Furthermore, the prior studies did not correct for possible differences in disease characteristics.
Disease characteristics and gender in relation to NC functioning
Our analyses revealed that males were significantly sicker than the females. That is to say, the males had a more impaired immune system both at the time of the current study and when they were initially introduced to ART, were more likely to have AIDS and to have detectable virus on ART, and more likely to have coinfection with TB. This revelation could possibly be as a result of women actually seeking treatment at an earlier time than men, either due to opportunistic infections or because they are more aware of signs of sickness than the men. This possibility is consistent with results of a study that showed that males are less likely to seek medical treatment in the earlier clinical stages of HIV than females.39 This trend has been linked to cultural and social issues to do with masculinity and power that demand physical and emotional strength from the male population, thus making them less likely to seek treatment early as a way of avoiding feelings of vulnerability and loss of power.40
Nevertheless, when we explored the cognitive functioning of HIV+ males and HIV+ females while controlling for disease characteristics, the females were more impaired compared to their male counterparts in the cognitive domains of learning and recall using the T-scores corrected for disease characteristics and the DDS. The females further performed worse than the males on motor, speed of information processing, and global mean T-scores.
It is worth mentioning that in spite of the males having more severe illness than their female counterparts, they still managed to perform relatively better on NC tests. Reasons for poorer relative NC outcomes in females might be attributed to either genetic or social factors or a combination of these factors. Some scholars41 postulate that seropositive females could be at greater risk of developing neuropsychological impairments compared to seropositive males. There is thus a great need to better understand what factors could be accounting for the gender differences we found in both disease severity and its associated NC outcomes.
Conclusion and recommendation
The findings obtained from this study raise an important need to investigate further the extent to which the HIV+ female population could be more negatively affected by HIV infection on cognitive functioning relative to HIV+ males.
Acknowledgments
The authors thank the NORAD’s program for Master studies (NOMA project) that funded the data collection process. The authors also thank the first and second cohort Masters students in clinical neuropsychology for their contribution in collecting the data of the healthy sample and the seropositive sample, respectively.
Disclosure
The authors report no conflicts of interest in this work.
References
What are HIV and AIDS? AVERT, 2012. Available from: www.avert.org/aids-hiv.htm. Accessed March 5, 2012. | ||
Maki MP, Marttin-Thormeyer E. HIV, cognition and women. Neuropsychol Rev. 2009;19:204–214. | ||
HIV and AIDS in Zambia. AVERT, 2012. Available from: www.avert.org/aids-zambia.htm. Accessed March 5, 2012. | ||
Global Press Institute, 2012. Available from: www.globalpressinstitute.org/global-news/africa. Accessed March 5, 2012. | ||
Zambia Ministry of Health/National AIDS Council. Zambia Country Report: Monitoring the Declaration of Commitment on HIV and AIDS and the Universal Access. Biennial report submitted to the United Nations General Assembly Special Session on HIV and AIDS Reporting period: January, 2010–December 2011. UNGASS, 2012. Available from: http://www.unaids.org/sites/default/files/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/ce_ZM_Narrative_Report.pdf. Accessed March 19, 2014. | ||
Central Statistics Office (CSO), Ministry of Health (MOH), Tropical Diseases Research Centre (TDRC), University of Zambia, Macro International Inc. Zambia Demographic and Health Survey 2007. Calverton, MD: CSO and Macro International Inc.; 2009. | ||
Zambia Ministry of Health/National AIDS Council. Zambia Country Report: Monitoring the Declaration of Commitment on HIV and AIDS and the Universal Access. Biennial report submitted to the United Nations General Assembly Special Session on HIV and AIDS. Available from: http://www.unaids.org/sites/default/files/country/documents/ZMB_narrative_report_2014.pdf. Accessed February 11, 2015. | ||
Jackson H. AIDS Africa – Continent in Crisis. Harare, Zimbabwe: SAfAIDS. | ||
Heaton R, Grant I, Butters N, et al. The HNRC 500-Neuropsychology of HIV infection at different disease stages. J Int Neuropsychol Soc.1995;1(3):231–251. | ||
Heaton RK, Clifford DB, Franklin DR Jr, et al; CHARTER Group. HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: CHARTER Study. Neurology. 2010;75:2087–2096. | ||
Reger MA, Martin DJ, Sherwood LC, Strauss G. The relationship between viral load and neuropsychological functioning in HIV-1 infection. Arch Clin Neuropsychol. 2005;20(2):137–143. | ||
Faílde-Garrido JM, Alvarez M, Simón-López MA. Neuropsychological impairment and gender differences in HIV-1 infection. Psychiatry Clin Neurosci. 2008;62;494–502. | ||
Hestad K, McArthur JH, Dal Pan GJ, et al. Regional atrophy in HIV-1 infection: association with specific neuropsychological test performance. Acta Neurol Scand. 1993;88:112–118. | ||
Heaton R, Marcotte TD, Mindt MR, et al. The impact of HIV-associated neuropsychological impairment on everyday functioning. J Int Neuropsychol Soc. 2004;10:317–331. | ||
Albert SM, Flater SR, Clouse R, et al. Medication management skill in HIV-1 evidence for adapting medication management strategies in people with cognitive impairment II. Evidence for a pervasive lay model of medication efficacy. AIDS Behav. 2003;7(3):329–338. | ||
Marcotte TD, Heaton RK, Wolfson T, et al; HNRC group. The impact of HIV related neuropsychological dysfunctions on driving behavior. J Neuropsychol Soc. 1999;7:579–592. | ||
Robertson KR, Kapoor C, Robertson WT, Fiscus S, Ford S, Hall CD. No gender differences in the progression of nervous system disease in HIV infection. J Acquir Immune Defic Syndr. 2004;36(36):817–822. | ||
Hestad AK, Menon JA, Ngoma M, et al. Sex differences in the neuropsycholgical performance as an effect of human immunodeficiency virus infection: a pilot study in Zambia, Africa. J Nerv Ment Dis. 2012;200(4): 336–342. | ||
Holguin A, Banda M, Willen EJ, et al. HIV-1 effects on neuropsychological performance in a resource-limited country, Zambia. AIDS Behav. 2011;15:1895–1901. doi:10.10071510461-011-9988-9. | ||
Stringer JS, Zulu I, Levy J, et al. Rapid scale-up of antiretroviral therapy at primary care sites in Zambia: feasibility and early outcomes. JAMA. 2006;296:782–793. doi:10.1001/jama.296.7.782. | ||
Hestad KA, Menon JA, Serpell R, et al. Do neuropsychological test norms from African Americans in the United States generalize to a Zambian population? Psychol Assess. 2016;28(1):18–38. doi:10.1037/pas0000147. | ||
Heaton RK, Cysique LA, Jin H, et al; San Diego HIV Neurobehavioral Research Center Group. Neurobehavioral effects of human immunodeficiency virus infection among former plasma donors in rural China. J Neurovirol. 2008;14(6):536–549. doi:10.1080/13550280802378880. | ||
Heaton RK, Miller SW, Taylor MJ, Grant I. Revised comprehensive Norms for an Expanded Halstead Reitan Battery: Demographically Adjusted Neuropsychological Norms for African American and Caucasian Adults. Lutz, FL: Psychological Assessment Resources Inc.; 2004. | ||
Kabuba N, Menon JA, Hestad K. Moderate alcohol consumption and cognitive functioning in a Zambian population. Med J Zambia. 2011;38(2). | ||
Antinori A, Arendt G, Becker JT, et al. Updated research nosology for HIV-associated neurocognitive disorders. Neurology. 2007;69(18):1789–1799. doi:10.1212/01.WNL.0000287431.88658.8b. | ||
Joska JA, Westgarth-Taylor J, Myer L, et al. Characterization of HIV-associated neurocognitive disorders among individuals starting antiretroviral therapy in South Africa. AIDS Behav. 2011;15(6):1197–1203. doi:10.1007/s10461-010-9744-6. | ||
Kanmogne DA, Kaute CT, Cysique LA, et al. HIV-associated neurocognitive disorders in sub-Saharan Africa: a pilot study in Cameroon. BMC Neurol. 2010;10:60. doi:10.1186/1471-2377-10-60. | ||
Ellis RJ, Hsia K, Spector SA, et al. Cerebrospinal fluid human immunodeficiency virus type 1 RNA levels are elevated in neurocognitively impaired individuals with acquired immunodeficiency syndrome. HIV Neurobehavioral Research Center Group. Ann Neurol. 1997;42(5):679–688. | ||
McArthur JC, McClernon DR, Cronin MF, et al. Relationship between human immunodeficiency virus-associated dementia and viral load in cerebrospinal fluid and brain. Ann Neurol. 1997;42:689–698. | ||
Zambia Ministry of Health. Adult and Adolescent Antiretroviral Therapy Protocols. Zambia Ministry of Health; 2010. Available from: http://www.who.int/hiv/pub/guidelines/zambia_art.pdf. Accessed April 5, 2016. | ||
Childs EA, Lyles RH, Selnes OA, et al. Plasma viral load and CD4 lymphocytes predict HIV-associated dementia and sensory neuropathy. Neurology. 1999;52(3):607–613. doi:10.1212/WNL.52.3.607. | ||
WHO. Global Database on Body Mass Index. WHO; 2016. Available from: http://apps.who.int/bmi/index.jsp?introPage=intro_3.html. Accessed March 8, 2016. | ||
Robertson K, Liner J, Heaton, R. Neuropsychological assessment of HIV-infected populations in international settings. Neuropsychol Rev. 2009;19(2):232–249. doi:10.1007/s11065-009-9096-z. | ||
Blackstone K, Moore DJ, Franklin DR. Defining neurocognitive impairment in HIV: deficit scores versus clinical ratings. Clin Neuropsychol. 2012;26(6):894–908. doi:10.1080/13854046.2012.694479. | ||
Carey C, Woods SP, Gonzalez R, et al. Predictive validity of global deficit scores in detecting neuropsychological impairment in HIV infection. J Clin Exp Neuropsychol. 2004;26(3):307–319; PubMed: 15512922. | ||
Hinkin CH, Hardy DJ, Mason KI, et al. Medication adherence in HIV-infected adults: effect of patient age, cognitive status and substance abuse. AIDS. 2004;18(Suppl 1):S19–S25. | ||
Garrido JM, Fernandez ML, Foltz M, Castro YR, Fernandez MVC. Cognitive performance in men and women infected with HIV-1. Psychiatry J. 2013;2013: Article ID 382126. | ||
Stern RA, Arruda JE, Somerville JA, et al. Neurobehavioral functioning in asymptomatic HIV-1 infected women. J Int Neuropsychol Soc. 1998;4(2):172–178. | ||
Braitstein P, Boulle A, Nash D, et al. Gender and the use of antiretroviral treatment in resource-constrained settings: findings from a multicenter collaboration. J Womens Health (Larchmt). 2008;17(1):47–55. | ||
Gibbs A, Jobson G. Narratives of masculinity in the Daily Sun: implications for HIV risk and prevention. S Afr J Psychol. 2011;4(2). | ||
Satz P, Morgenstern H, Miller EN, et al. Low education as a possible risk factor for cognitive abnormalities in HIV-1: findings from the multicenter AIDS cohort study (MACS). J Acquir Immune Defic Syndr. 1993;6(5):503–511. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

