Back to Journals » Clinical Interventions in Aging » Volume 17
Hip Fracture Surgery in Severe Aortic Stenosis: A Study of Factors Affecting Mortality
Authors Rostagno C , Cartei A , Rubbieri G, Ceccofiglio A, Civinini R, Curcio M, Polidori G, Boccaccini A
Received 30 January 2022
Accepted for publication 16 July 2022
Published 4 August 2022 Volume 2022:17 Pages 1163—1171
DOI https://doi.org/10.2147/CIA.S360538
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Nandu Goswami
Carlo Rostagno,1 Alessandro Cartei,2 Gaia Rubbieri,2 Alice Ceccofiglio,2 Roberto Civinini,3 Massimo Curcio,2 Gianluca Polidori,2 Alberto Boccaccini4
1Department of Experimental and Clinical Medicine, University of Florence, Florence, Italy; 2Department of Internal and Post-Surgery Unit, AOU Careggi, Florence, Italy; 3Department of Orthopaedics, University of Florence, Florence, Italy; 4Department of Anaesthesia, AOU Careggi, Florence, Italy
Correspondence: Carlo Rostagno, Department of Experimental and Clinical Medicine, University of Florence, Largo Brambilla 3, Florence, 50134, Italy, Tel +390557948545, Email [email protected]
Background: In elderly patients with hip fracture, the prevalence of severe aortic stenosis (valve area < 1 cm2) is close to 5%. Few studies have evaluated the prognostic role of aortic stenosis in hip fracture surgery and none has considered the effects of the postoperative setting (intensive care unit vs general ward) on clinical outcome.
Purpose: The aim of the present study was to evaluate the factors affecting mortality in patients with severe aortic stenosis undergoing surgery for hip fracture. We also evaluated whether postoperative monitoring in the intensive care unit may affect the prognosis in comparison to return to the general ward after surgery.
Patients and Methods: All 2274 patients referred for hip fracture to our tertiary teaching hospital between January 1 2015 and December 31 2019 were screened for the presence of severe aortic stenosis, defined by an aortic valve area < 1.0 cm2.
Results: The study included 66 patients (27 males, 39 females) with a mean±SD age of 85± 7 years. The average time between trauma and surgery was 2.6± 3 days. The mean aortic valve area was 0.74± 0.15 cm2. Seven patients died during hospitalization (10.4%). Diabetes, having two or more comorbidities, a low degree of autonomy, heart failure, history of coronary artery disease, atrial fibrillation, postoperative delirium and pulmonary hypertension were associated with poorer outcome. In logistic multivariate analysis, the number of diseases and values of pulmonary artery pressure were the only independent factors related to mortality. In hospital mortality (12 and 9%, respectively) and complication rates were not statistically different between patients referred to the intensive care unit for postoperative monitoring and patients returned to the general ward after surgery.
Conclusion: In patients undergoing hip fracture surgery, severe aortic stenosis is associated with high hospital mortality, and two or more comorbidities and pulmonary hypertension are associated with a worse prognosis. The postoperative setting (intensive care unit or general ward) does not affect outcome.
Keywords: aortic stenosis, prognosis, hip fracture, elderly
Introduction
Aortic stenosis is found in no less than 5% of patients with hip fracture1,2 and is associated with an high in-hospital and long-term mortality.3–5 None of the previous investigations included only patients with severe aortic valve disease (aortic valve area <1.0 cm2),2–5,7 and therefore information on this high-risk subset of patients is limited. The National Confidential Enquiries into Perioperative Deaths (NCEPOD) recommended the use of invasive monitoring and intensive care observation after surgery for patients with aortic stenosis undergoing non-cardiac surgery,6 particularly for procedures related to a high bleeding risk. At present, however, no randomized studies have been published regarding the postoperative setting, and most information is anecdotal.8 The aim of the present study was to evaluate the factors affecting mortality in patients with severe aortic stenosis undergoing surgery for hip fracture. We also evaluated whether postoperative monitoring in the intensive care unit (ICU) may affect the prognosis in comparison to return to the general ward after surgery.
Materials and Methods
Study Setting
The study is part of a project of the Italian Health Ministry and Regione Toscana (RF-2010-2316600) and was approved by Ethical Committee of Regione Toscana. All patients and/or their legal guardians gave written informed consent to treatment and collection of clinical data for research purposes at admission. The research was performed in accordance with the Declaration of Helsinki.
Population
Medical records of patients referred to our tertiary teaching hospital for hip fracture between January 1 2015 and December 31 2019 were collected. A multidisciplinary hip fracture unit, including internal medicine specialists/geriatricians, cardiologists, orthopaedic surgeons and anaesthesiologists, has existed in our hospital since 2011, allowing early careful preoperative evaluation including bedside echocardiography.9 Bedside echocardiography was performed in all patients with a systolic ejection murmur, history of heart failure, coronary artery disease (CAD) and atrial fibrillation. Patients with severe aortic stenosis (valve area <1 cm2, mean valve gradient >40 mmHg) were entered into the study. Exclusion factors were age <70 years, a myocardial infarction in the 30 days before trauma and the presence of active neoplasm. Three patients with severe aortic valve stenosis were excluded because they underwent preoperative aortic balloon valvuloplasty (n=2) or percutaneous aortic valve replacement (n=1) before surgery. Figure 1 presents the flowchart of patients enrolled in the study.
 |
Figure 1 Study flowchart. Abbreviations: AVA, aortic valve area; AVR, aortic valve replacement; AVBV, aortic balloon valvuloplasty; AMI, acute myocardial infarction; ICU, intensive care unit. |
Surgery was performed under general anaesthesia with continuous invasive blood pressure monitoring. Although preoperatively all patients were given an indication for postoperative observation in intensive care, owing to limited of availability of beds in the intensive care setting, by chance about 50% of patients returned to the hospital ward in the immediate postoperative period.
Data
Several variables were collected from the clinical records, including age, gender, functional status before trauma, history of atrial fibrillation, diabetes, congestive heart failure, CAD, dementia and chronic kidney failure. The overall number of comorbidities was calculated. Moreover, for each patient, the time from admission to surgery, the need for red blood cell transfusion and the number of red blood cell units transfused were evaluated. Finally, we recorded the occurrence of postoperative complications such as delirium, stroke, pneumonia, sepsis, wound infection, deep vein thrombosis (DVT), pulmonary embolism, congestive heart failure, respiratory failure, atrial fibrillation and anaemia, defined as haemoglobin <8 g/dL.
Outcomes
The main endpoint of the study was the assessment of overall in-hospital mortality and the identification of factors related to an unfavourable outcome. We also assessed whether postoperative management in an ICU may affect the prognosis in comparison to return to the general ward after surgery.
Statistical Analysis
Continuous variables were reported as mean and standard deviation. Non-continuous variables were reported as frequency of distribution. Statistical analysis of continuous data was performed using the Student’s t-test, while non-continuous data were analysed using the χ2 test or Fisher’s exact test. After the univariate analyses, a logistic multivariable regression analysis was performed to identify independent predictors for mortality. Because of multiple testing, only variables with a two-sided p<0.05 in the univariate analysis were accepted for the model. Statistical analysis was performed using SPSS 18.0 (Chicago, IL, USA) statistical software. A probability value of 0.05 was considered statistically significant.
Results
Clinical Characteristics of Patients
In the period under investigation, 2274 patients with fragility fracture involving the hip were referred to our tertiary teaching hospital. According to the inclusion criteria, 66 patients (27 males, 39 females), with mean age 85±7 years, were entered into the study. In 32 patients we found a neck femur fracture, in 30 a per-trochanteric fracture, and finally four had a subtrochanteric fracture. The average time between trauma and surgery was 2.6±2.3 days. In 42 (63%), surgery was performed within 48 hours of trauma. Clinical and echocardiographic characteristics of patients are reported in Table 1.
 |
Table 1 Comparison of Clinical and Echocardiographic Characteristics of Patients Discharged Alive and Who Died in Hospital |
The average aortic valve area was 0.74±0.15 cm2, while the peak pressure gradient was 84±26 mmHg. Moderate to severe mitral regurgitation was present in 10 patients, 12 had left ventricular dysfunction and 26 had moderate to severe pulmonary hypertension.
Postoperative Findings
Thirty-two patients showed a postoperative increase-fall in troponin I values, suggesting myocardial injury; however, only eight showed electrocardiographic ischaemic changes or abnormalities of left ventricular wall motion. Seven patients died during hospitalization (10.4%). Table 2 compares the clinical and echocardiographic characteristics of patients who died and patients who were discharged alive. We did not find any significant difference in time to surgery between patients who died and those who were discharged alive. A lower degree of autonomy before trauma, history of diabetes, atrial fibrillation, CAD and heart failure were related to a poorer outcome.
 |
Table 2 Postoperative Complications in Patients Discharged Alive and Patients Who Died in Hospital |
Patients who died in hospital had, on average, a higher transvalvular aortic gradient (97.1±36.5 vs 83.3±25 mmHg) in comparison to patients who were discharged alive; however, the difference was not statistically significant. Moderate to severe pulmonary hypertension was associated with higher mortality. No other significant differences existed between the two groups regarding the other echocardiographic parameters. Myocardial infarction/myocardial injury was significantly more frequent in patients who died in hospital in comparison to patients who were discharged alive, and the development of postoperative delirium was also more frequent in those who died in hospital. In logistic multivariate analysis, the number of diseases and values of pulmonary artery pressure were the only independent factors related to mortality (Table 3).
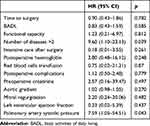 |
Table 3 Multivariate Logistic Analysis |
Comparison Between Patients with Postoperative Course in Intensive Care Unit and in General Ward
Thirty-one patients were followed in an intensive care setting after hip surgery, while the other 35 were referred directly to the general ward. Clinical characteristics and echocardiographic data of the two groups are reported in Tables 4 and 5. Although the average time to surgery was longer in patients referred to the ICU, the percentage of patients treated within 48 hours was identical in the two groups (62% vs 61.9%). No other significant differences were found between the two groups.
 |
Table 4 Clinical Characteristics of Patients Followed in the General Ward or in the Intensive Care Setting |
 |
Table 5 Preoperative Echocardiographic Parameters in Patients Followed in the General Ward or in the Intensive Care Setting |
The incidence of postoperative complications was not significantly different between patients monitored in intensive care after surgery and patients referred to the general ward (Table 6).
 |
Table 6 Postoperative Complications in Parameters in Patients Followed in the General Ward or in the Intensive Care Setting |
Finally, in-hospital mortality (n=3 [8.6%] in the general ward vs n=4 [12.9%] in the ICU) and the length of stay in patients discharged alive (15.9±10.2 days in the general ward and 15.7±8.0 days in patients referred to the ICU) were not significantly different between the two groups.
Discussion
Hip fracture is a common emergency requiring urgent non-cardiac surgery. The incidence of aortic valve stenosis in these patients has been estimated to be between 5% and 10%.1,2 Since, in Italy, hip fracture occurs in more than 100,000 patients every year, at least 4500−9000 will have severe aortic stenosis. This number is probably underestimated since despite SIGN guidelines6 suggesting that echocardiography “should be performed if aortic stenosis is suspected”, to avoid delay in surgery a negligible proportion of patients with hip fracture undergo preoperative echocardiography.10 Guidelines suggest that in patients with severe aortic stenosis urgent non-cardiac procedures should be performed under close haemodynamic monitoring and postoperative observation in the intensive care setting is suggested;6,11,12 however, these indications are not based on randomized or observational studies.8
In the present study, the incidence of severe aortic stenosis (aortic valve area <1 cm2) in patients with hip fracture who underwent careful clinical and echocardiographic evaluation was close to 3%. In-hospital mortality in these patients was 10.6% in comparison to overall mortality, comprising 2–3% of historical samples from our institution.8 In patients who died, diabetes, two or more comorbidities, a low degree of autonomy, heart failure, history of CAD, atrial fibrillation, postoperative delirium and pulmonary hypertension were significantly more frequent than in patients who were discharged alive. In logistic multivariate analysis, however, only the number of diseases and the values of pulmonary artery pressure were independent factors related to mortality. Mortality was not statistically different (12% in patients admietted to ICU vs 9% in patients in general ward). Moreover no differences were found in complications rate between the two groups.
Previous investigations are heterogeneous regarding the degree of aortic valve stenosis, type of anaesthesia (neuraxial vs general) and perioperative monitoring. McBrien et al13 reported a 10% mortality at 30 days in patients with severe aortic stenosis who underwent hip fracture surgery in comparison to 6.25% in patients with moderate valve disease. Most patients, 67%, had general anaesthesia and continuous haemodynamic monitoring. Time to surgery was on average 5.5 days from injury. In their case-control study, Keswani et al3 reported a higher 30-day mortality in the group with aortic stenosis in comparison to controls (14.7% vs 4.2%). However, an analysis of subgroups (moderate vs severe aortic stenosis) was not performed. In their study, prognosis was not affected by the type (general vs regional) of anaesthesia. A twofold higher in-hospital mortality after hip fracture surgery in aortic stenosis, with an average aortic valve area of 0.97 cm2, in comparison to patients without aortic stenosis was reported by Adunsky et al.1 The CURRENT AS study14 reported an overall 4.3% mortality at 30 days in patients with severe aortic stenosis who underwent non-cardiac surgery (71% treated under general anaesthesia). Although hip fracture accounted for 61 out of 187 enrolled patients, outcome was not evaluated separately. Four of the overall eight deaths, however, occurred after hip surgery. All published studies, with few exceptions,7,15 suggest that severe aortic stenosis is related to higher mortality in patients undergoing hip fracture surgery, in agreement with the results of the present investigation. Nevertheless, in previous studies characterization of haemodynamic characteristics was generally poor and, when comparable, a less severe impairment was found in comparison to our patients (for example, in CURRENT AS study, peak aortic gradient was 55±22 mmHg and only 10% had pulmonary hypertension, in comparison to a peak gradient of 84±26 mmHg and 37% with pulmonary hypertension reported in the present investigation). A more severe haemodynamic impairment in patients included in our study is supported by the observation that pulmonary hypertension was independently related to in-hospital mortality. Further postoperative haemodynamic impairment may account for the higher incidence of delirium in patients who died (6/7 vs 15/59, p<0.003). All had signs of myocardial injury/infarction and three showed rapidly worsening heart failure.
Balloon aortic valvuloplasty has been demonstrated to decrease the risk of perioperative complications in patients with severe aortic stenosis,16,17 although it leads to a significant surgical delay. A multicentre study may be needed to assess its usefulness in very high-risk patients.
Although guidelines suggest monitoring in an intensive setting patients with severe aortic stenosis after hip surgery, we did not find any randomized or observational study in the literature supporting this recommendation.8 Owing to the limited intensive care resources in our hospital, the availability of intensive monitoring was not considered a reason to delay surgery. Therefore, in the period under investigation, we had, by chance, two comparable groups of patients with or without monitoring in the intensive setting. We did not find any significant difference in terms of mortality, complications or length of stay in patients who underwent postoperative monitoring in the intensive care setting in comparison to those who directly returned to the general ward. This observation may be interesting in terms of resource allocation, suggesting that the costs related to intensive monitoring in the postoperative setting in patients with hip fracture and severe aortic stenosis may be spared. This affirmation, however, must be taken with caution. In general, multidisciplinary management of hip fracture is associated with an early and long-term improvement in outcomes,18,19 and the results reported in the present study may be related to the organizational model of our hospital, in which the ward is attended by an internal medicine specialist/geriatrician, 24 hours, 7 days a week.
Limitations
The main limitations of the study are its retrospective design and the overall small number of patients included. However, to our knowledge, this is the largest series reporting outcomes in patients with severe aortic stenosis who need surgery for hip fracture. The comparison between patients monitored in the ICU setting and those returned to the general ward did not follow formal randomization and was the result of chance owing the limited intensive care resources. Nevertheless, the characteristics of the two resulting groups were comparable, allowing a sufficiently accurate analysis.
Conclusion
In patients who need urgent/emergency non-cardiac surgery, aortic stenosis is often undiagnosed and only preoperative echocardiographic evaluation may reveal its presence and severity. After hip surgery, the mortality rate in patients with severe aortic stenosis is about 10%. Two or more comorbidities and pulmonary hypertension are the only independent predictive factors of mortality. Postoperative monitoring in the intensive care setting does not add significant risk reduction in an advanced model with a medical ward under daily 24-hour supervision.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Adunsky A, Kaplan A, Arad M, Mizrahi EH, Gottlieb S. Aortic stenosis in elderly hip fractured patients. Arch Gerontol Geriatr. 2008;46(3):401–408. doi:10.1016/j.archger.2007.05.013
2. Rostagno C, Ranalli C, Polidori G, Cartei A, Boccaccini A, Peris A. Outcome in elderly patients with aortic stenosis undergoing Hip fracture surgery. Results may suggest a different postoperative strategy? Trauma Surg Acute Care Open. 2019;4(1):e000218. doi:10.1136/tsaco-2018-000218
3. Keswani A, Lovy A, Khalid M, et al. The effect of aortic stenosis on elderly hip fracture outcomes: a case control study. Injury. 2016;47(2):413–418. doi:10.1016/j.Injury.2015.10.015
4. Chen X, Ma Y, Deng Z, Li Q, Liao J, Zheng Q. Prediction of early postoperative major cardiac events and in-hospital mortality in elderly hip fracture patients: the role of different types of preoperative cardiac abnormalities on echocardiography report. Clin Interv Aging. 2020;15:755–762. doi:10.2147/CIA.S250620
5. Ahmed T, Safdar A. The management dilemma: concomitant acute hip fracture and severe asymptomatic aortic stenosis. Cureus. 2020;12(4):e7527. doi:10.7759/cureus.7527
6. Scottish Intercollegiate Guidelines Network. Management of hip fracture in older people: a national clinical guideline. sign.ac.uk/pdf/sign111.pdf. 2009.
7. Pellikka PA, Sarano ME, Nishimura RA, et al. Outcomes of 622 adults with asymptomatic, hemodynamically significant aortic stenosis during prolonged follow-up. Circulation. 2005;111:3290–3295. doi:10.1161/CIRCULATIONAHA.104.495903
8. Sorrentino R, Santoro C, Bardi L, Rigolin V, Gentile F. Non-cardiac surgery in patients with valvular heart disease. Heart. 2021. doi:10.1136/heartjnl-2021-319160
9. Rostagno C, Buzzi R, Campanacci D, et al. In hospital and 3-month mortality and functional recovery rate in patients treated for hip fracture by a multidisciplinary team. PLoS One. 2016;11(7):e0158607. doi:10.1371/journal.pone.0158607
10. Loxdale SJ, Sneyd JR, Donovan A, Werrett G, Viira DJ. The role of routine pre-operative bedside echocardiography in detecting aortic stenosis in patients with a Hip fracture. Anaesthesia. 2012;67:51–54. doi:10.1111/j.1365-2044.2011.06942.x
11. Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guidelines on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/ American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014;64:2372–2405. doi:10.1016/j.jacc.2014.07.945
12. The Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). 2014 ESC/ESA guidelines on non-cardiac surgery: cardiovascular assessment and management. Eur Heart J. 2014;35:2383–2431. doi:10.1093/eurheartj/ehu282
13. McBrien ME, Heyburn G, Stevenson M, et al. Previously undiagnosed aortic stenosis revealed by auscultation in the Hip fracture population–echocardiographic findings, management and outcome. Anaesthesia. 2009;64(8):863–870. doi:10.1111/j.1365-2044.2009.05960
14. Taniguchi T, Morimoto T, Shiomi H, et al.; CURRENT AS Registry Investigators. Elective non-cardiac surgery in patients with severe aortic stenosis - observations from the CURRENT AS registry. Circ J. 2020;84(7):1173–1182. doi:10.1253/circj.CJ-20-0026
15. Leibowitz D, Rivkin G, Schiffman J, et al. Effect of severe aortic stenosis on the outcome in elderly patients undergoing repair of hip fracture. Gerontology. 2009;55(3):303–306. doi:10.1159/000209245
16. Ferré F, Viarnes M, Martin C, et al. Is preoperative balloon aortic valvuloplasty of interest for severe aortic stenosis in Hip fracture surgery? Injury. 2021;52(6):1438–1444. doi:10.1016/j.injury.2020.09.048
17. Rostagno C, Cartei A, Di Cristo A, Buzzi R, Santoro G. Aortic ballon valvuloplasty is still a valuable option for high risk patients with severe aortic stenosis before surgery for Hip fracture. Int J Cardiovasc Res. 2015;4:5. doi:10.4172/2324-8602.1000222
18. Patel JN, Klein DS, Sreekumar S, Liporace FA, Yoon RS. Outcomes in multidisciplinary team-based approach in geriatric hip fracture care: a systematic review. J Am Acad Orthop Surg. 2020;28(3):128–133. doi:10.5435/JAAOS-D-18-00425
19. Khasraghi FA, Christmas C, Lee EJ, Mears SC, Wenz JF. Effectiveness of a multidisciplinary team approach to hip fracture management. J Surg Orthop Adv. 2005;14(1):27–31.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
