Back to Journals » OncoTargets and Therapy » Volume 12
High Tiam1 expression predicts positive lymphatic metastasis and worse survival in patients with malignant solid tumors: a systematic review and meta-analysis
Authors Yang C, Ma C, Li Y, Mo P, Yang Y
Received 20 October 2018
Accepted for publication 10 May 2019
Published 25 July 2019 Volume 2019:12 Pages 5925—5936
DOI https://doi.org/10.2147/OTT.S191571
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Geoffrey Pietersz
Caixia Yang,1 Chenlin Ma,1 Yingchun Li,1 Peng Mo,1 Yusheng Yang2
1Department of Stomatology, Qinghai province people’s Hospital, Qinghai, People’s Republic of China; 2Department of Pathology, Ninbo Yinzhou No. 2 Hospital, Ninbo, People’s Republic of China
Background: Many studies have explored the prognostic value of T-cell lymphoma invasion and metastasis inducing factor 1 (Tiam1) and its association with lymphatic metastasis in malignant solid tumors, but the conclusions remain controversial. Therefore, we performed a meta-analysis to systematically assess the prognostic value of Tiam1 expression and its association with lymphatic metastasis in malignant solid tumors.
Methods: We searched eligible studies in PubMed, Web of Science and EMBASE databases (from inception up to October 2018). The combined HR with 95% CI was used to estimate the prognostic value of Tiam1 expression. The correlation between Tiam1 expression and lymphatic metastasis was assessed using the combined odds ratio (OR) with 95% CI.
Results: A total of 17 studies with 2,228 patients with solid tumors were included in this meta-analysis. The overall estimated results showed that high Tiam1 expression was significantly associated with shorter overall survival (HR= 2.08, 95% CI: 1.62–2.68, P<0.01), and disease-free survival (HR = 1.86, 95% CI: 1.49–2.32, P<0.01). Besides, we also found that there was a close relationship between high Tiam1 expression and positive lymphatic metastasis (OR=2.63; 95% CI: 1.79–3.84, P<0.01).
Conclusion: High Tiam1 expression was significantly associated with shorter survival and positive lymphatic metastasis in patients with malignant solid tumors. Therefore, Tiam1 may be a promising prognostic biomarker and an effective therapeutic target for malignant solid tumors.
Keywords: tumor, Tiam1, survival, meta-analysis
Introduction
Cancer has become a leading cause of death and major public health problem worldwide due to its high incidence and mortality1 Although the methods of diagnosis and treatment of cancers have been greatly improved in recent years, long-term survival in some types of cancers remains unsatisfied as a whole1 Tumor biomarkers have values of early detection, prognosis evaluation and drug discovery of cancers, so as to identify specific biomarkers have been attracting many researchers.2 A great plenty of tumor biomarkers have been discovered in recent years, but only a handful of biomarkers could be applied for clinical practice.3 Accordingly, it remains imperative to explore novel sensitive biomarkers that exhibit excellent performances in predicting prognosis in cancers.
T-cell lymphoma invasion and metastasis-inducing factor 1 (Tiam1), a specific guanine nucleotide exchange factor, a member of the Rho GTPase family, was first discovered by Habets et al and identified as an invasion and metastasis-related gene in mice with aggressive T-cell lymphoma.4,5 The TIAM1 gene is located in the q22 band of chromosome 21 and the centromeric end of the AML 21 gene and contains 2 exons (~7.3 kb) separated by 1 intron (14 kb)6 Tiam1 is mainly expressed in normal brain and testis tissues with only minimal or no expressions detected in other normal tissues7 Additionally, Tiam1 is highly expressed in various cancers as well,6,8–23 and its overexpression in cancer cells could contribute to proliferation,24–27 invasion and metastasis,28–31 angiogenesis32 and chemo-resistance of cancer cells33 Of note, Tiam1 expressed in tumor stromal microenvironment also plays a role in regulating tumor invasion, metastasis and chemo-resistance. Cancer-associated fibroblast (CAF) is a major stromal cell in cancer stromal microenvironment.34,35 A recent study by Izumi et al33 showed that CAFs isolated from colorectal cancer (CRC) tissues could induce chemo-resistance of CRC cells when the two kinds of cells were co-cultured, but surprisingly the direct inhibition of Tiam1 in CAFs could result in enhanced chemo-sensitivity of CRC cells33 Considering the multiple functions of Tiam1 in cancer progression, many researchers focused on exploring the prognostic value of Tiam1. However, the conclusions about the prognostic value of Tiam1 in malignant solid tumors remain controversial. Most of studies suggested that high Tiam1 expression was related to shorter survival in many tumors, including hepatocellular carcinoma, pancreatic cancer, gallbladder cancer, prostate cancer, ovarian cancer and breast cancer. On the contrast, a few of studies indicated that low Tiam1 expression was associated with poor prognosis in patients with gastric cancer18 and papillary thyroid cancer12 Considering that most of the single-center studies had the limitations of sample size and methodology, we herein performed a meta-analysis to systematically evaluate the prognostic significance of Tiam1 expression in patients with solid tumor. In addition, Tiam1 is an invasion and metastasis-related gene, so in this meta-analysis, we also performed a pooling analysis to assess the association between Tiam1 expression and lymphatic metastasis.
Materials and methods
This systematic review and meta-analysis were performed according to PRISMA statement issued in 200936 Besides, this study was approved by Ethics Committee of Qinghai province people’s Hospital.
Literature search strategy
We searched eligible studies in PubMed, Web of Science and EMBASE databases (from inception up to October 2018). The search terms included “cancer,” “tumor,” “carcinoma,” “adenocarcinoma,” “neoplasm,” “malignant,” “malignancy,” “Tiam1,” “T lymphoma invasion and metastasis 1” “T-cell lymphoma invasion and metastasis inducing factor 1”, “survival,” “prognosis,” and “prognostic.” The search strategy used in PubMed was as follows: (((((((((cancer[Title/Abstract]) OR tumor[Title/Abstract]) OR carcinoma[Title/Abstract]) OR adenocarcinoma[Title/Abstract]) OR neoplasm[Title/Abstract]) OR malignant[Title/Abstract]) OR malignancy[Title/Abstract])) AND (((Tiam1[Title/Abstract]) OR (T lymphoma invasion[Title/Abstract] AND metastasis 1[Title/Abstract])) OR (T-cell lymphoma invasion[Title/Abstract] AND metastasis inducing factor 1[Title/Abstract]))) AND (((survival[Title/Abstract]) OR prognosis[Title/Abstract]) OR prognostic[Title/Abstract]). Additionally, we also manually searched eligible studies from the references of the identified articles.
Inclusion and exclusion criteria
The inclusion criteria were as follows: 1) the prognostic value of Tiam1 expression in malignant solid tumor in terms of overall survival (OS), recurrence-free survival (RFS) or disease-free survival (DFS) was explored; 2) the Tiam1 expression was divided into high/positive and low/negative groups; 3) HRs and 95% CIs, which were used to estimate the prognostic value of Tiam1 expression, were reported directly or could be calculated from the Kaplan–Meier curves; 4) the studies were published in English; 5) the studies were published in full text and 6) the study was the most informative report, if the same patient population was enrolled into different studies.
The exclusion criteria were as follows: 1) the studies were duplicated publications, reviews, case reports, conference abstracts, editorials or case reports; 2) the studies were only involved in animal and cell experiments and 3) HRs and CIs could not be extracted.
Data extraction and quality assessment
Two independent authors (Caixia Yang and Chenlin Ma) extracted the information from the included literature using a predefined template based on the reporting checklists of PRISMA36 The following items were extracted: tumor type, the first author’s last name, country, publication year, country, sample number, age, gender, antibody source detection methods, definition of high Tiam1 expression, T stage, TMN stage, distant metastasis, lymph node metastasis, survival outcomes, and HR and its corresponding 95% CI. Software Engauge Digitizer 4.1 (https://markummitchell.github.io/engauge-digitizer/) was used to extract HR and its corresponding 95% CI from Kaplan–Meier curve, if HR and its corresponding 95% CI was not directly reported. The methodological quality of included studies was evaluated using the Newcastle Ottawa scale,37 in which the quality score ranges from 0 to 9. Usually, a study with 6 or more scores is considered to be methodologically sound. With respect to data extraction and quality assessment, any inconsistencies were removed by discussion among all authors.
Statistical analysis
HR with its corresponding 95% CI was used to estimate the prognostic value of Tiam1 expression in patients with malignant solid tumors. HR >1 (low expression as reference) suggested that patients with high Tiam1 expression had shorter survival than those with low expression. The correlation between Tiam1 expression and lymphatic metastasis was assessed using the combined OR with 95% CI, and OR >1 (low expression as reference) indicated that high Tiam1 expression was closely associated with positive lymphatic metastasis. Heterogeneity among the included studies was assessed using Higgin’s I2 statistic. I2>50% signified statistically significant heterogeneity. A fixed-effects or random-effects model was applied to evaluate the prognostic value of Tiam1 expression and its association with lymphatic metastasis. A fixed-effects model was chosen when there was no obvious heterogeneity among studies38 Otherwise, a random-effects model was used. Begg’s test39 and Egger’s test40 were employed to assess the publication bias. Subgroup analysis and meta-regression analysis were performed according to sample size, tumor type, antibody source and quality score to explore the sources of heterogeneity. Sensitivity analysis was conducted by sequentially omitting one study to explore the robustness and reliability of the overall estimated results. All statistical processes were fulfilled using STATA, version 12.0 (Stata Corporation, College Station, TX, USA). All statistical tests were 2-sided, and P p<0.05 was considered as the statistical significance.
Results
Literature selection
The flowchart of literature search and selection is shown in Figure 1. A total of 161 publications were retrieved from electronic databases. Further, 74 publications were excluded due to duplicates. Then, the remaining publications were reviewed by the title and abstract, in which 66 publications were excluded owing to unrelated topics, nonclinical studies, reviews and conference abstracts. Next, 4 publications were further excluded after full-text reviewing for lacking available data and enrolling overlapped patients. Finally, a total of 17 studies were included in our meta-analysis.6,8–23
 |
Figure 1 Flow diagram of selecting eligible studies. |
Basic characteristics of included studies
A total of 17 studies enrolling 2,228 patients with malignant solid tumors were included in this meta-analysis. The included studies were published from 2006 to 2018. A total of 16 studies assessed the prognostic value of Tiam1 for OS6,8–10,12–23 and 6 studies for DFS.11,14,16,19,21,22 Besides, 15 studies reported the association between Tiam1 expression and lymph node metastasis.6,8–10,12–15,17–23 All the included studies detected the Tiam1 expression in protein level. More details about the main characteristics of the included studies were presented in Tables 1 and 2.
 |
Table 1 The main characteristics of the included studies |
 |
Table 2 The main characteristics of the included studies |
Pooling analysis
A total of 16 studies with 2,168 patients explored the correlation between Tiam1 expression and OS. The random-effects model was employed to pool HRs and their 95% CIs due to the significant heterogeneity among these studies (I2=68.2%, p<0.01). The result showed that patients with high Tiam1 expression had shorter OS than those with low expression (HR=2.08, 95% CI: 1.62–2.68, p<0.01; Figure 2). Six studies with 845 patients reported the relationship between Tiam1 expression and DFS. Because of no significant heterogeneity (I2=48.2%, p=0.08), the fixed effect model was used to pooling data. The result showed that patients with high Tiam1 expression also had shorter OS than those with low expression (HR=1.86, 95% CI: 1.49–2.32, p<0.01; Figure 3).
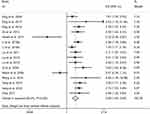 |
Figure 2 Forest plot of pooled HR for the association between high Tiam1 expression and poor overall survival (OS). |
 |
Figure 3 Forest plot of pooled HR for the association between high Tiam1 expression and poor disease-free survival (DFS). |
Besides, a total of 15 studies with 1,951 patients investigated the relationship between Tiam1 expression and lymph node metastasis. Because of significant heterogeneity (I2=61.1%, p<0.01, we pool data on lymphatic metastasis using the random-effect model and found that high Tiam1 expression predicted a higher proportion of lymphatic metastasis (OR=2.63, 95% CI: 1.79–3.84, p<0.05; Figure 4).
 |
Figure 4 Forest plot of pooled HR for the association between high Tiam1 expression and positive lymph node metastasis. |
Subgroup and meta-regression analyses
The subgroup and meta-regression analyses were conducted according to sample size, tumor type, antibody source, definition of high Tiam1 expression and quality score to explore the sources of the heterogeneity in the meta-analyses of the association of Tiam1 expression with OS and lymphatic metastasis. The results of subgroup analysis showed that the significant heterogeneity for OS and lymphatic metastasis still existed in subgroup analysis by any factor (Table 3). However, the results of meta-regression analysis showed that antibody source might explain the major heterogeneity in the meta-analyses of the association of Tiam1 expression with OS (p<0.01) (Table 4). Additionally, we found that high Tiam1 expression was associated with shorter OS and positive lymphatic metastasis in all subgroups, only with the exception of subgroup of the other antibody sources, suggesting that our overall estimated results were stable and reliable as a whole.
 |
Table 3 The prognostic role of Tiam1 expression in different subgroups |
 |
Table 4 The potential source of heterogeneity evaluated by meta-regression |
Sensitivity analysis and publication bias
We conducted sensitivity analysis by sequentially omitting one study to further explore the robustness and reliability of the overall estimated results about OS and lymphatic metastasis. The results showed that our pooled results about OS (Figure 5A) and lymphatic metastasis (Figure 5B) did not change significantly when any one of the included studies was omitted, thereby confirming the robustness of the overall estimated results.
 |
Figure 5 Sensitivity analysis for OS (A) and lymph node metastasis (B). Begg`s funnel plot of publication bias assessment for OS (C) and lymph node metastasis (D). |
The Begg’s and Egger’s tests were conducted to assess the publication bias for OS and lymphatic metastasis. The results showed that the Begg’s funnel plots for OS (Figure 5C) and lymphatic metastasis (Figure 5D) were symmetric, and the p-values of Egger’s tests for OS (p=0.804) and lymphatic metastasis (p=0.388) were >0.05, suggesting that there was no significant publication bias. Due to the limited number of eligible studies about DFS, publication bias assessment was not performed in this analysis.
Discussion
Many studies have explored the prognostic value of T-cell lymphoma invasion and metastasis inducing factor 1 (Tiam1) and its association with lymphatic metastasis in malignant solid tumors, but the conclusions remain controversial. Therefore, we performed a meta-analysis to systematically assess the prognostic value of Tiam1 expression and its association with lymphatic metastasis in malignant solid tumors.
To our best knowledge, this study is the first meta-analysis to systematically assess the prognostic value of Tiam1 expression and its association with lymphatic metastasis in patients with malignant solid tumors. A total of 17 studies with 2,228 patients with solid tumors were included in this meta-analysis. The combined results showed that high Tiam1 expression was significantly associated with shorter overall survival (OS; HR = 2.08, 95% CI: 1.62–2.68, P<0.01), and disease-free survival (DFS; HR = 1.86, 95% CI: 1.49–2.32, P<0.01). Besides, we also found that there was a close relationship between high Tiam1 expression and positive lymphatic metastasis (OR=2.63; 95% CI: 1.79–3.84, P<0.01). Furthermore, our subgroup, meta-regression, and sensitivity analyses showed that the overall estimated results were reliable and stable.
Multiple cellular functions of Tiam1 in tumor progression have been elaborated, which may account for the inverse association between Tiam1 expression and survival of cancer patients. First, metastasis is an essential hall marker of cancer and always leads to poor survival.41–43 Numerous studies suggested that Tiam1 contributed to invasion and metastasis in various cancers, including osteosarcoma,44 retinoblastoma,45 gastric cancer,46 CRC,47–51 hepatocellular carcinoma,25,52 breast cancer,53 cholangiocarcinoma,54 cervical cancer,20 ovarian cancer,55 nasopharyngeal cancer,8,16 laryngeal cancer,56 thyroid carcinoma,57 nom-small cell lung cancer,48 pancreatic cancer6,58,59 and oral squamous cell carcinoma27 Malliri et al reported that Tiam1 could facilitate E-cadherin-based adhesions between cancer cells in mouse intestinal tumors and human colon tumors, resulting in invasion and metastasis60 Epithelial–mesenchymal transition (EMT) is a key process of enhancing cancer cell migration, invasion and metastasis.28–31 Liu et al reported that Tiam1 overexpression could promote invasiveness and metastasis of thyroid carcinoma in vitro and in vivo by activating Wnt/EMT pathway57 Similarly, Ding6 and Yang et al20 also demonstrated that Tiam1 overexpression could also boost invasion and metastasis of pancreatic cancer and cervical cancer by inducing EMT. Current evidence shows that angiogenesis is also involved in tumor metastasis.61–63 A study by Yang et al suggested that depletion of Tiam1 could significantly suppress cervical cancer cell angiogenesis through inhibiting microtubule formation, blood vessels formation, as well as VEGF and VEGFA expression20 Additionally, a recent study by Zhu et al also showed that Tiam1 overexpression could accelerate progression of lung adenocarcinoma by enhancing angiogenesis32 Second, Tiam1 also has a role in regulating chemo-resistance of malignant cells. For instance, Hofbauer et al24 reported that Tiam1/Rac1 signal transduction could contribute to chemoresistance of chronic lymphocytic leukemia cells. In a recent study, Izumi et al33 found that Tiam1 was overexpressed in CRC patients who did not respond to chemotherapy and demonstrated that upregulation of Tiam1 could induce chemo-resistance by enhancing stemness of CRC cells. Third, several studies also suggested that Tiam1 overexpression could promote the in vitro proliferation of malignant cells and in vivo growth of tumor.24–27 As above, it can be easily deduced that Tiam1 expression in cancer cells is required for facilitating tumor growth, invasion, metastasis and chemo-resistance, which supports the prognostic value of Tiam1. Therefore, Tiam1 in tumor cells may be an attractive therapeutic target. Fourth, increasing evidence showed that the stromal microenvironment within cancers is a pivotal factor of regulating the growth, invasiveness, and metastasis and chemo-sensitivity of cancer cells,64–68 and Tiam1 expressed in tumor stromal microenvironment also plays a role in regulating tumor invasion, metastasis and chemo-resistance. CAF is a major stromal cell in cancer stromal microenvironment.34,35 Izumi et al33 found that CAFs isolated from CRC tissues could induce chemo-resistance of CRC cells when the two kinds of cells were co-cultured, but surprisingly the direct inhibition of Tiam1 in CAFs could result in enhanced chemo-sensitivity of CRC cells33 Thus, targeting Tiam1 in tumor stromal may be an ideal way to boost the effectiveness of chemotherapy. However, it was also reported that Tiam1 in tumor-associated fibroblasts had a role in modulating tumor invasion and metastasis, and knockout of Tiam1 in tumor-associated fibroblasts facilitated tumor invasion and metastasis.69,70 Therefore, more studies are warranted to fully elucidate the functions of Tiam1 in tumor stromal and to assess the integrated effects of Tiam1 in tumor epithelial cells and stromal.
There were some limitations in this meta-analysis. We should cautiously consider when interpreting the results of pooling analysis. First, only studies published in English were included in this meta-analysis, which probably introduced bias. Second, some of the included studies did not directly provide HRs and 95% CIs, and thereby we estimated HRs from the Kaplan–Meier curve using Engage Digitizer 4.1. Inevitably, manually extracting data from Kaplan–Meier curve will cause some calculation errors. Third, there was significant heterogeneity in this meta-analysis. We conducted subgroup and meta-regression analyses based on some factors and identified the antibody source as one of the main sources. In fact, many other factors including age, tumor size, gender, TNM stage, distant metastasis and follow-up time may also cause heterogeneity. However, we failed to conduct subgroup and meta-regression analyses based on these factors due to lacking relevant data in the included studies. Fourth, among all the 17 included studies, only 2 studies with a few patients were from Germany and the rest were all from China, and so it remains unclear whether our findings could be generalized to other populations, especially Caucasian and Africans.
Conclusion
High Tiam1 expression was significantly associated with poor survival and positive lymphatic metastasis in patients with solid tumors. Therefore, Tiam1 may be a promising prognostic biomarker and an effective therapeutic target for solid tumors.
Acknowledgments
This study was not supported by grants from any funding sources.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7–30. doi:10.3322/caac.21442
2. Kalia M. Biomarkers for personalized oncology: recent advances and future challenges. Metabolism. 2015;64(3 Suppl 1):S16–S21. doi:10.1016/j.metabol.2014.10.027
3. Kulasingam V, Prassas I, Diamandis EP. Towards personalized tumor markers. NPJ Precis Oncol. 2017;1(1):17. doi:10.1038/s41698-017-0021-2
4. Habets GG, Scholtes EH, Zuydgeest D, et al. Identification of an invasion-inducing gene, Tiam-1, that encodes a protein with homology to GDP-GTP exchangers for Rho-like proteins. Cell. 1994;77(4):537–549.
5. Mertens AE, Roovers RC, Collard JG. Regulation of Tiam1-Rac signalling. FEBS Lett. 2003;546(1):11–16.
6. Ding M, Li Y, Yang Y, et al. Elevated expression of Tiam1 is associated with poor prognosis and promotes tumor progression in pancreatic cancer. Onco Targets Ther. 2018;11:4367–4375. doi:10.2147/OTT.S171425
7. Boissier P, Huynh-Do U. The guanine nucleotide exchange factor Tiam1: a Janus-faced molecule in cellular signaling. Cell Signal. 2014;26(3):483–491.
8. Ding Y, Chen B, Huang J, et al. Overexpression of Tiam1 is associated with malignant phenotypes of nasopharyngeal carcinoma. Oncol Rep. 2014;32(2):607–618.
9. Ding Y, Chen B, Wang S, et al. Overexpression of Tiam1 in hepatocellular carcinomas predicts poor prognosis of HCC patients. Int J Cancer. 2009;124(3):653–658.
10. Du X, Wang S, Lu J, et al. Clinical value of Tiam1-Rac1 signaling in primary gallbladder carcinoma. Med Oncol. 2012;29(3):1873–1878. doi:10.1007/s12032-011-0046-2
11. Engers R, Mueller M, Walter A, Collard JG, Willers R, Gabbert HE. Prognostic relevance of Tiam1 protein expression in prostate carcinomas. Br J Cancer. 2006;95(8):1081–1086. doi:10.1038/sj.bjc.6603385
12. Hsueh C, Lin JD, Yang CF, et al. Prognostic significance of Tiam1 expression in papillary thyroid carcinoma. Virchows Arch. 2011;459(6):587–593. doi:10.1007/s00428-011-1164-0
13. Li H, Cui X, Chen D, et al. Clinical implication of Tiam1 overexpression in the prognosis of patients with serous ovarian carcinoma. Oncol Lett. 2016;12(5):3492–3498. doi:10.3892/ol.2016.5091
14. Li Z, Liu Q, Piao J, et al. Clinicopathological implications of Tiam1 overexpression in invasive ductal carcinoma of the breast. BMC Cancer. 2016;16(1):681. doi:10.1186/s12885-016-2724-0
15. Liu H, Shi G, Liu X, Wu H, Fan Q, Wang X. Overexpression of Tiam1 predicts poor prognosis in patients with esophageal squamous cell carcinoma. Oncol Rep. 2011;25(3):841–848. doi:10.3892/or.2010.1122
16. Liu N, Tang LL, Sun Y, et al. MiR-29c suppresses invasion and metastasis by targeting TIAM1 in nasopharyngeal carcinoma. Cancer Lett. 2013;329(2):181–188. doi:10.1016/j.canlet.2012.10.032
17. Liu S, Li Y, Qi W, et al. Expression of Tiam1 predicts lymph node metastasis and poor survival of lung adenocarcinoma patients. Diagn Pathol. 2014;9:69. doi:10.1186/1746-1596-9-69
18. Walch A, Seidl S, Hermannstadter C, et al. Combined analysis of Rac1, IQGAP1, Tiam1 and E-cadherin expression in gastric cancer. Mod Pathol. 2008;21(5):544–552. doi:10.1038/modpathol.2008.3
19. Yang H, Cai YC, Cao Y, et al. The prognostic value of Tiam1 protein expression in head and neck squamous cell carcinoma: a retrospective study. Chin J Cancer. 2015;34(12):614–621. doi:10.1186/s40880-015-0053-3
20. Yang Y, Wu Q, Li N, et al. Upregulation of Tiam1 contributes to cervical cancer disease progression and indicates poor survival outcome. Hum Pathol. 2018;75:179–188. doi:10.1016/j.humpath.2018.02.006
21. Wang S, Li S, Yang X, et al. Elevated expression of T-lymphoma invasion and metastasis inducing factor 1 in squamous-cell carcinoma of the head and neck and its clinical significance. Eur J Cancer. 2014;50(2):379–387. doi:10.1016/j.ejca.2013.10.003
22. Qi Y, Huang B, Yu L, Wang Q, Lan G, Zhang Q. Prognostic value of Tiam1 and Rac1 overexpression in nasopharyngeal carcinoma. ORL J Otorhinolaryngol Relat Spec. 2009;71(3):163–171. doi:10.1159/000223440
23. Zhao L, Liu Y, Sun X, He M, Ding Y. Overexpression of T lymphoma invasion and metastasis 1 predict renal cell carcinoma metastasis and overall patient survival. J Cancer Res Clin Oncol. 2011;137(3):393–398. doi:10.1007/s00432-010-0895-7
24. Hofbauer SW, Krenn PW, Ganghammer S, et al. Tiam1/Rac1 signals contribute to the proliferation and chemoresistance, but not motility, of chronic lymphocytic leukemia cells. Blood. 2014;123(14):2181–2188. doi:10.1182/blood-2013-08-523563
25. Chen G, Lu L, Liu C, Shan L, Yuan D. MicroRNA-377 suppresses cell proliferation and invasion by inhibiting TIAM1 expression in hepatocellular carcinoma. PLoS One. 2015;10(3):e0117714. doi:10.1371/journal.pone.0117714
26. Liu Y, Wang X, Jiang X, et al. Tumor-suppressive microRNA-10a inhibits cell proliferation and metastasis by targeting Tiam1 in esophageal squamous cell carcinoma. J Cell Biochem. 2018. doi:10.1002/jcb.28059
27. Zhou H, Kann MG, Mallory EK, et al. Recruitment of Tiam1 to semaphorin 4D activates rac and enhances proliferation, invasion, and metastasis in oral squamous cell carcinoma. Neoplasia. 2017;19(2):65–74.
28. Liao TT, Yang MH. Revisiting epithelial-mesenchymal transition in cancer metastasis: the connection between epithelial plasticity and stemness. Mol Oncol. 2017;11(7):792–804. doi:10.1002/1878-0261.12096
29. Shi C, Chen Y, Chen Y, Yang Y, Bing W, Qi J. CD4(+) CD25(+) regulatory T cells promote hepatocellular carcinoma invasion via TGF-beta1-induced epithelial-mesenchymal transition. Onco Targets Ther. 2019;12:279–289. doi:10.2147/OTT.S172417
30. Sun R, Lu X, Gong L, Jin F. TCTP promotes epithelial-mesenchymal transition in lung adenocarcinoma. Onco Targets Ther. 2019;12:1641–1653. doi:10.2147/OTT.S184555
31. Wang J, Li H, Xia C, et al. Downregulation of CENPK suppresses hepatocellular carcinoma malignant progression through regulating YAP1. Onco Targets Ther. 2019;12:869–882. doi:10.2147/OTT.S190061
32. Zhu G, Zhang Y, Wang Q, et al. The prognostic value of Tiam1 correlates with its roles in epithelial-mesenchymal transition progression and angiogenesis in lung adenocarcinoma. Cancer Manag Res. 2019;11:1741–1752. doi:10.2147/CMAR.S195093
33. Izumi D, Toden S, Ureta E, Ishimoto T, Baba H, Goel A. TIAM1 promotes chemoresistance and tumor invasiveness in colorectal cancer. Cell Death Dis. 2019;10(4):267. doi:10.1038/s41419-019-1300-3
34. Choe C, Shin YS, Kim C, et al. Crosstalk with cancer-associated fibroblasts induces resistance of non-small cell lung cancer cells to epidermal growth factor receptor tyrosine kinase inhibition. Onco Targets Ther. 2015;8:3665–3678. doi:10.2147/OTT.S89659
35. Hu G, Zhong K, Chen W, Wang S, Huang L. Podoplanin-positive cancer-associated fibroblasts predict poor prognosis in lung cancer patients. Onco Targets Ther. 2018;11:5607–5619. doi:10.2147/OTT.S175566
36. Knobloch K, Yoon U, Vogt PM. Preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and publication bias. J Craniomaxillofac Surg. 2011;39(2):91–92. doi:10.1016/j.jcms.2010.11.001
37. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. doi:10.1007/s10654-010-9491-z
38. Dai K, Quan J, Yan F, et al. lncRNAs as potential molecular biomarkers in the clinicopathology and prognosis of cholangiocarcinoma: a systematic review and meta-analysis. Onco Targets Ther. 2019;12:1905–1915. doi:10.2147/OTT.S188134
39. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101.
40. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi:10.1136/bmj.315.7109.629
41. Gao XL, Zhang M, Tang YL, Liang XH. Cancer cell dormancy: mechanisms and implications of cancer recurrence and metastasis. Onco Targets Ther. 2017;10:5219–5228. doi:10.2147/OTT.S140854
42. Wei C, Wang Y, Li X. The role of Hippo signal pathway in breast cancer metastasis. Onco Targets Ther. 2018;11:2185–2193. doi:10.2147/OTT.S157058
43. Xue JY, Huang C, Wang W, Li HB, Sun M, Xie M. HOXA11-AS: a novel regulator in human cancer proliferation and metastasis. Onco Targets Ther. 2018;11:4387–4393. doi:10.2147/OTT.S166961
44. Jin J, Cai L, Liu ZM, Zhou XS. miRNA-218 inhibits osteosarcoma cell migration and invasion by down-regulating of TIAM1, MMP2 and MMP9. Asian Pac J Cancer Prev. 2013;14(6):3681–3684.
45. Subramanian N, Navaneethakrishnan S, Biswas J, Kanwar RK, Kanwar JR, Krishnakumar S. RNAi mediated Tiam1 gene knockdown inhibits invasion of retinoblastoma. PLoS One. 2013;8(8):e70422. doi:10.1371/journal.pone.0070422
46. Li Z, Yu X, Wang Y, et al. By downregulating TIAM1 expression, microRNA-329 suppresses gastric cancer invasion and growth. Oncotarget. 2015;6(19):17559–17569. doi:10.18632/oncotarget.2755
47. Poudel KR, Roh-Johnson M, Su A, et al. Competition between TIAM1 and membranes balances endophilin A3 activity in cancer metastasis. Dev Cell. 2018;45(6):738–752 e736. doi:10.1016/j.devcel.2018.05.021
48. Zhu G, Fan Z, Ding M, et al. An EGFR/PI3K/AKT axis promotes accumulation of the Rac1-GEF Tiam1 that is critical in EGFR-driven tumorigenesis. Oncogene. 2015;34(49):5971–5982. doi:10.1038/onc.2015.45
49. Wang B, Li W, Liu H, et al. miR-29b suppresses tumor growth and metastasis in colorectal cancer via downregulating Tiam1 expression and inhibiting epithelial-mesenchymal transition. Cell Death Dis. 2014;5:e1335. doi:10.1038/cddis.2014.304
50. Minard ME, Ellis LM, Gallick GE. Tiam1 regulates cell adhesion, migration and apoptosis in colon tumor cells. Clin Exp Metastasis. 2006;23(5–6):301–313. doi:10.1007/s10585-006-9040-z
51. Minard ME, Herynk MH, Collard JG, Gallick GE. The guanine nucleotide exchange factor Tiam1 increases colon carcinoma growth at metastatic sites in an orthotopic nude mouse model. Oncogene. 2005;24(15):2568–2573. doi:10.1038/sj.onc.1208503
52. Liu Y, Ding Y, Huang J, et al. MiR-141 suppresses the migration and invasion of HCC cells by targeting Tiam1. PLoS One. 2014;9(2):e88393. doi:10.1371/journal.pone.0088393
53. Minard ME, Kim LS, Price JE, Gallick GE. The role of the guanine nucleotide exchange factor Tiam1 in cellular migration, invasion, adhesion and tumor progression. Breast Cancer Res Treat. 2004;84(1):21–32. doi:10.1023/B:BREA.0000018421.31632.e6
54. Cheng W, Liu Y, Zuo Z, et al. Biological effects of RNAi targeted inhibiting Tiam1 gene expression on cholangiocarcinoma cells. Int J Clin Exp Pathol. 2015;8(12):15511–15526.
55. Li J, Liang S, Jin H, Xu C, Ma D, Lu X. Tiam1, negatively regulated by miR-22, miR-183 and miR-31, is involved in migration, invasion and viability of ovarian cancer cells. Oncol Rep. 2012;27(6):1835–1842. doi:10.3892/or.2012.1744
56. Wang S, Li S, Tang Q, et al. Overexpression of Tiam1 promotes the progression of laryngeal squamous cell carcinoma. Oncol Rep. 2015;33(4):1807–1814. doi:10.3892/or.2015.3785
57. Liu L, Wu B, Cai H, et al. Tiam1 promotes thyroid carcinoma metastasis by modulating EMT via Wnt/beta-catenin signaling. Exp Cell Res. 2018;362(2):532–540. doi:10.1016/j.yexcr.2017.12.019
58. Guo X, Wang M, Jiang J, et al. Balanced Tiam1-rac1 and RhoA drives proliferation and invasion of pancreatic cancer cells. Mol Cancer Res. 2013;11(3):230–239. doi:10.1158/1541-7786.MCR-12-0632
59. Cruz-Monserrate Z, O’Connor KL. Integrin alpha 6 beta 4 promotes migration, invasion through Tiam1 upregulation, and subsequent Rac activation. Neoplasia. 2008;10(5):408–417.
60. Malliri A, Rygiel TP, van der Kammen RA, et al. The rac activator Tiam1 is a Wnt-responsive gene that modifies intestinal tumor development. J Biol Chem. 2006;281(1):543–548. doi:10.1074/jbc.M507582200
61. Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000;100(1):57–70.
62. Bai ZG, Zhang ZT. A systematic review and meta-analysis on the effect of angiogenesis blockade for the treatment of gastric cancer. Onco Targets Ther. 2018;11:7077–7087. doi:10.2147/OTT.S169484
63. Peng T, Li Z, Li D, Wang S. MACC1 promotes angiogenesis in cholangiocarcinoma by upregulating VEGFA. Onco Targets Ther. 2019;12:1893–1903. doi:10.2147/OTT.S197319
64. Guerra L, Odorisio T, Zambruno G, Castiglia D. Stromal microenvironment in type VII collagen-deficient skin: the ground for squamous cell carcinoma development. Matrix Biol. 2017;63:1–10. doi:10.1016/j.matbio.2017.01.002
65. Vail ME, Murone C, Tan A, et al. Targeting EphA3 inhibits cancer growth by disrupting the tumor stromal microenvironment. Cancer Res. 2014;74(16):4470–4481. doi:10.1158/0008-5472.CAN-14-0218
66. Quail DF, Joyce JA. Microenvironmental regulation of tumor progression and metastasis. Nat Med. 2013;19(11):1423–1437.
67. Achyut BR, Arbab AS. Myeloid cell signatures in tumor microenvironment predicts therapeutic response in cancer. Onco Targets Ther. 2016;9:1047–1055.
68. Wang L, Yang X, Li D, et al. The elevated glutaminolysis of bladder cancer and T cells in a simulated tumor microenvironment contributes to the up-regulation of PD-L1 expression by interferon-gamma. Onco Targets Ther. 2018;11:7229–7243.
69. Xu K, Rajagopal S, Klebba I, et al. The role of fibroblast Tiam1 in tumor cell invasion and metastasis. Oncogene. 2010;29(50):6533–6542.
70. Xu K, Tian X, Oh SY, et al. The fibroblast Tiam1-osteopontin pathway modulates breast cancer invasion and metastasis. Breast Cancer Res. 2016;18(1):14.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
