Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 13
High Perceived Stigma Among People Living with HIV/AIDS in a Resource Limited Setting in Western Ethiopia: The Effect of Depression and Low Social Support
Authors Turi E , Simegnew D, Fekadu G , Tolossa T , Desalegn M , Bayisa L , Mulisa D , Abajobir A
Received 3 December 2020
Accepted for publication 15 March 2021
Published 1 April 2021 Volume 2021:13 Pages 389—397
DOI https://doi.org/10.2147/HIV.S295110
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bassel Sawaya
Ebisa Turi,1 Dawit Simegnew,2,3 Ginenus Fekadu,4,5 Tadesse Tolossa,1 Markos Desalegn,1 Lami Bayisa,6 Diriba Mulisa,6 Amanuel Abajobir7
1Department of Public Health, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia; 2Vanke School of Public Health, Tsinghua University, Beijing, People’s Republic of China; 3Department of Pharmacy, College of Health and Medical Sciences, Bule Hora University, Bule Hora, Ethiopia; 4Department of Pharmacy, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia; 5School of Pharmacy, Faculty of Medicine, The Chinese University of Hong Kong, Shatin, New Territory, Hong Kong; 6School of Nursing and Midwifery, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia; 7Maternal and Child Wellbeing Unit, African Population and Health Research Centre, Nairobi, Kenya
Correspondence: Ebisa Turi
Department of Public Health, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia
Tel +251 917686021
Fax +251 576617980
Email [email protected]
Background: Antiretroviral therapy (ART) is only one part of a successful range of care among people living with HIV/AIDS (PLWHA). Stigma and low social support are emerging issues worsening the success of ART for PLWHA. This study thus aimed to investigate the level of perceived stigma among PLWHA.
Methods: An institution-based cross-sectional study was conducted in Nekemte, western Ethiopia. A multivariable logistic regression model was used to identify associations between perceived stigma and low social support, depression, and other potential predictor variables using SPSS version 24.0 and adjusted odds ratios (AORs), considering statistical significance at p< 0.05.
Results: A total of 418 study participants were included in the study, with a response rate of 100%. About 48.6% of PLWHA had experienced perceived stigma, and more than two-fifths had poor social support. The following factors were associated with perceived stigma among PLWHA: age (18– 29 years) (AOR=4.88, 95% CI:1.76– 13.5), female sex (AOR=2.10, 95% CI 1.15– 3.82), < 12 months on ART (AOR=2.63, 95% CI 1.09– 6.34), depression (AOR=1.86, 95% CI 1.08– 3.19), social support (poor: AOR=3.45, 95% CI 1.65– 7.23; medium: AOR=2.22, 95% CI 1.09– 4.54), and non-disclosure of HIV status (AOR=2.00, 95% CI 1.11– 3.59).
Conclusion and Recommendation: The magnitude of perceived stigma among PLWHA was high, highlighting the importance of integrating social and mental health support within standard ART for PLWHA.
Keywords: stigma, social support, HIV/AIDS, Nekemte, Ethiopia
Introduction
Globally, more than 74.9 million people have been infected with HIV and 32 million have died of AIDS-related illnesses.1 HIV is among the leading public health challenges in sub-Saharan Africa.2 However, the expansion of antiretroviral therapy (ART) has changed HIV infection into a manageable chronic disease, thereby reducing HIV transmission and reducing the number of people dying from AIDS-related illnesses.3,4 Since 2010, new HIV infections have dropped by 38% and AIDS-related deaths have declined by 49% in the eastern and southern African regions.5
According to UNAIDS, 690,000 people were living with HIV, and 11,000 people had died of AIDS-related illnesses in Ethiopia by 2018. Consequently, the country adopted the UNAIDS 90–90–90 targets, which envision that 90% of people living with HIV would know their HIV status, 90% of people who know their HIV-positive status would be able to access therapy, and 90% of people on treatment would have suppressed viral loads by 2020.6 As such, the UNAIDS Fast Track Strategy has reported 81%, 79%, and 73% success rates for the first, second, and third of the 90–90–90 targets for the country,7 implying that the country needs to have a strong linkage system across HIV/AIDS care continuum to achieve this goal.
According to the UNAIDS 2015 report, in 35% of countries with available data, over 50% of people report experiencing discriminatory attitudes because of their HIV status.8 Stigma affects multiple domains of people’s lives, and interference with the continuum of care for HIV/AIDS is also rampant. For example, one in eight people living with HIV is denied access to lifelong ART because of enacted stigma and discrimination.9 Research from the USA showed that 89% of people living with HIV/AIDS (PLWHA) reported perceived stigma.10 In Ethiopia, about 15–31.2% of PLWHA reported internalized stigma.11,12
Non-communicable diseases such as mental health problems, stigma, and substance use are emerging issues challenging successful treatment for PLWHA.13 Common mental disorders such as hopelessness, depression, anxiety, suicidal ideation, and substance abuse are more common among PLWHA than the general population.13,14 This suggests the need for an integrated intervention for PLWHA alongside ART. A complex interplay of factors, including low socioeconomic status, non-adherence to ART, and advanced WHO clinical stage III and IV, is associated with stigma (either perceived or enacted) among PLWHA.10,15–18 Moreover, impaired mental health states, such as depression, and perceived stigma are linked with a compromised adherence to ART and poor treatment outcomes,18–20 as well as substance use21 and risky sexual behaviors.22
Understanding the level of perceived stigma and its associated factors will play an important role in successful care for HIV/AIDS patients. However, there is a dearth of research in this regard and limited information on factors that are associated with perceived stigma. This study therefore aims to assess the level of perceived stigma and associated factors among PLWHA attending public health hospitals in Nekemte town in western Ethiopia.
Methods
Study Design, Period, and Area
This study was embedded in a large-scale project on substance use among PLWHA on ART who were followed up at Nekemte public hospitals, western Ethiopia. An institutional-based study design was used, and the study was conducted from February to April 2020. The institutions comprised two health centers and two public hospitals, one specialized hospital and Wllega University Teaching and Referral Hospital. The hospitals provide adult ART and care services; 24-hour emergency, pharmacy, and delivery services; antenatal care; and physiotherapy, inpatient, and psychiatry services to the community.
Source and Study Population
The source population was made up of all ART patients on treatment follow-up at Nekemte public hospitals. The study population comprised sampled ART patients who had treatment follow-up during the study period.
Eligibility Criteria
Patients who were aged above 18 years and those who had enrolled in HIV care within the previous 3 months were eligible.
Exclusion Criteria
Records with incomplete data (baseline clinical and laboratory data, date of HIV diagnosis, date of ART initiation, and outcome not recorded) and transfer in from other institutions with incomplete baseline data were excluded from the study.
Sample Size and Sampling Procedure
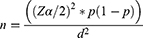
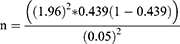
The sample size for this study was calculated by applying a single population proportion formula considering the 95% CI level, 5% margin of error, and 10% contingency rate by taking the proportion (p) of stigma of 43.9% from a previous study, conducted in southern Ethiopia.23
where n is the sample size, the Z value corresponds to the 95% significance level, and P is substance use prevalence, taken from the previous study.23
Therefore, n=380; by adding a 10% non-response rate, the final sample size was estimated to be n=418.
Then, a consecutive sampling technique was used to select study participants based on the inclusion criteria until the required sample size was achieved.
Study Variables
Dependent Variable
The dependent variable was perceived stigma.
Independent Variables
Independent variables included 1) socio-demographic variables, such as residence, age, sex, marital status, educational status, and level of income; 2) HIV/AIDS-related characteristics of the participants, such as time since diagnosis, duration on treatment, and CD4 level; 3) behavior-related characteristics of the patients, such as alcohol use disorder (AUD), smoking, and current khat chewing; 4) level of social support; and 5) disclosure status.
Measurements
Data on alcohol disorder were collected by adapting a previously validated WHO questionnaire.24 Psychoactive substance use (khat in our case) was also collected by a tool which was adapted from the WHO, ASSIST v3.0. A questionnaire adapted from a tool previously validated in developing countries was used for assessment of the level of depression.25 Data on social support were collected by the Oslo 3-item Social Support Scale (OSS-3).26 The OSS-3 has three categories: “poor support”, 3–8; “moderate support”, 9–11; and “strong support”, 12–14.26 In this study, perceived HIV stigma was measured based up on a tool consisting of nine items which was previously used by Fido et al for measurement purposes; then, individuals who had an attitude score equal to or greater than the mean score of the study population were categorized as having high perceived stigma.27
Data Collection
Data were collected using an interviewer-administered structured questionnaire. A version of the questionnaire in the local language, Afan Oromo, was used to collect the data. The questionnaire covered socio-demographic information and baseline clinical and laboratory data (baseline CD4 count, WHO clinical stage, hemoglobin level, opportunistic infections, WHO functional status, time of HIV diagnosis, time since ART initiation, and comorbidity). In addition, family-related data (disclosure status, partner’s HIV status) and regimen-related data (side effects of drug, time of ART initiation) were included in the checklist.
Data Processing and Statistical Analysis
Each completed questionnaire was coded on a prepared coding sheet by the principal investigator to minimize errors. Data were entered into a computer using the statistical program Epi Info for Windows version 7.0. Data were cleaned and exported to SPSS Windows version 20.0 for further analysis. Descriptive analyses, such as proportions, percentages, frequency distribution, and measures of central tendency, were carried out. Bivariable and multivariable logistic regression models were used. Initially, bivariable analysis was performed between the dependent variable and each of the independent variables, one at a time. Their odds ratios (ORs), 95% confidence intervals (CIs), and p-values were obtained. Then, all variables found to be significant at the bivariable level (p<0.2) were considered as candidates for the multivariable logistic regression model. Violations of regression model assumption were checked by inspection multicollinearity tests and variance inflation factors. Model goodness of fit was tested by the Hosmer–Lemeshow model goodness-of-fit test. A p-value of <0.05 and 95% confidence level was used as a statistically significant difference for the final models.
Ethical Considerations
This study was conducted in accordance with the Declaration of Helsinki. Ethical clearance and permission were obtained from Tsinghua University review board, and permission was secured from Nekemte Specialized Hospital and Wollega University Teaching and Referral Hospital and submitted to ART focal persons in each public health facility. Informed consent was obtained from each respondent before the interview. Study participants were provided with information about the objectives of the study and their right to respond fully or partially to the questionnaire. Confidentiality of individual client information was ensured by using unique identifiers for study participants and limiting access by third parties by storing the completed questionnaires and all documents with participant information in a lockable cabinet. In addition, the phone number and email address of the principal investigator were provided, so that participants could ask questions related to ambiguous or unclear aspects of the study, prior to agreeing to participate. The hard copy of the data, recorded data, and all the interviewers’ notes were kept in a private place, accessible only by the proxy of the principal investigator.
Results
Socio-Demographic Characteristics
A total of 418 PLWHA who were on ART participated in the interview, with a 100% response rate. The predominant ethnicity and religion among the participants were Oromo, 358 (85.6%) and Protestant, 204 (48.8%), respectively. The mean age of the participants was 37.84 (SD=9.54) years, ranging from 20 to 67 years. About one-third of the respondents, 135 (32.3%), fell in the 30–38-year age group. About 274 (65.6%) of them were married and about one-third, 159 (38%), had an educational level of college and above (Table 1).
 |
Table 1 Socio-Demographic Characteristics of the Study Participants |
HIV/AIDS-Related Characteristics of the Participants
From a total of 418 participants, more than half had experienced adverse drug reactions after initiating the treatment. The majority of the study participants, 350 (83.7%), had a history of opportunistic infections. About two-thirds, 277 (66.3%), had disclosed their HIV status, while about two-fifths of the participants had missed their ART and practiced risky sexual behavior due to substance use (Table 2).
 |
Table 2 HIV/AIDS-Related Characteristics of the Participants |
Social Support and Perceived Stigma for HIV/AIDS Patients on ART Follow-Up in Nekemte Town
About one-third of the participants, 138 (33.01%), had poor social support, whereas 8% had strong social support. Analysis of the study data revealed that most of the study participants who experienced high perceived stigma were those who had poor social support (Figure 1).
 |
Figure 1 Social support and perceived stigma among PLWHA. |
Factors Associated with Perceived Stigma Among PLWHA
Based on bivariable logistic regression analyses, socio-demographic variables such as age (18–19 years; COR=3.85, 95% CI 1.98−7.5), sex (female; COR=0.96, 95% CI 0.64–1.46), residence (rural; COR=0.66, 95% CI 0.43–1.01), marital status (single; COR=1.8, 95% CI 0.815–3.99), educational status (no formal education; COR=0.74, 95% CI 0.42–1.307), and income level (<500 Ethiopian birr; COR=1.67, 95% CI 1.04–2.68), as well as clinically related factors such as time of diagnosis (<24 months; COR=1.95, 95% CI 1.12–2.38) and duration of treatment (<12 months; COR=4.61, 95% CI 2.13–9.98), and behavior-related factors such as current smoking (COR=2.57, 95% CI 1.64–4.03), khat chewing (COR=1.50, 95% CI 0.97–2.35), AUD (COR=2.54, 95% CI 1.56–4.12), social support (poor social support; COR=3.04, 95% CI 1.64–5.64), and disclosure status (COR=2.48, 95% CI 1.49–3.94) were associated with high perceived stigma. On multivariable logistic regression, participants being aged 18–29 years (AOR=4.88, 95% CI 1.76–13.5), being female (AOR=2.10, 95% CI 1.15–3.82), less than 12 months’ treatment duration (AOR=2.63, 95% CI 1.09–6.34), current smoking (AOR=2.42, 95% CI 1.19–4.9), reported depression (AOR=1.86; 95% CI 1.08–3.19), poor social support (AOR=3.45, 95% CI 1.65–7.23), medium social support (AOR=2.22, 95% CI 1.09–4.54), and not disclosing HIV status (AOR=2.00, 95% CI 1.11–3.59) were significantly associated with high perceived stigma (Table 3).
 |
Table 3 Factors Associated with Perceived Stigma Among HIV/AIDS Patients on Antiretroviral Therapy in Nekemte Town |
Discussion
In PLWHA, the provision of ART is found to improve the lifespan of the patients. However, this prolonged lifespan is compromised by discrimination and a high burden of HIV/AIDS-related stigma, which is triggered by socio-demographic, psychosocial, behavioral, and clinical factors. In this study, high perceived HIV-related stigma was significantly associated with poor social support. This is due to the fact that higher levels of social support give a patient a sense of belongingand a feeling of love and affection, so the patient can cope psychologically better with the disease compared to people with lower levels of social support and self-esteem.28,29 Moreover, social support and care are the most important factors impacting the quality of life of PLWHA.30
In this study, younger age groups were more stigmatized than older PLWHA. This finding is in line with other findings from a cross-sectional study.31 This could be explained by both cognitive (e.g., fear of aging or getting sick) and social issues (e.g., fear of separation/divorce, family stress, and career transition) that could affect how stigma is anticipated. Most of these experiences are likely to wield less influence as they tend to stabilize with older age. As people grow older they may become more comfortable with their HIV status as they are likely to have more counselling as long as they stay in HIV/AIDS continuum of care.31
The odds of perceived HIV-related stigma among females with HIV were about two times higher than in their male counterparts. This is consistent with other literature finding that women living with HIV are vulnerable to enacted, anticipated, and internalized stigma.10,17,32 Stigma is highly related to depression, which affects more women than men as women are more vulnerable to HIV-related stigma. Moreover, women in developing countries are less powerful in decision-making regarding their sexual and other life matters. These underlying gender-based inequalities are compounded and exacerbated by HIV status. As a result, women living with HIV often experience an interwoven and overlapping jigsaw of stigma due to their HIV status and being female. Biological factors are another problem that increases the susceptibility of females to HIV infection, favored by socio-behavioral practices and socioeconomic differences, which in turn lead to HIV-related stigma.17 However, this result contradicts a study from India in which males were more stigmatized than females. This is because in India, but not in our set-up, males were the breadwinners.15,29,33,34
Not disclosing their HIV status was positively associated with HIV-related stigma among PLWHA. The same result was reported in other studies.32,35–37 This can be explained as stigma appearing to interfere in the relationship between misconception and willingness to disclose HIV status in the event of infections. For both sexes of PLWHA, misconception is associated with stigma, which in turn is negatively associated with willingness to disclose.38
HIV patients with depression were about two times more likely to experience perceived stigma than those who were not depressed. This result is in line with the study findings from another part of Ethiopia23 and a systematic review.39 The possible explanation for this could be people that with HIV are seen as immoral or unsafe, which is associated with stigmatizing beliefs. Being an HIV patient, by itself, is associated with the likelihood of depression,39 in which poor psychosocial functioning, the presence of opportunistic infections, poor immune status, and fear of dying from a chronic illness could explain the existence of depression and HIV-related stigma, as well as their association with each other.40
The findings of this study should, be interpreted with caution, owing to the following limitations. First, the cross-sectional design of this study only allows the development of hypotheses and cannot establish cause–effect relationships. No randomization or power calculations were performed. Even though our interviewers were well trained, some participants could be vulnerable to giving socially desirable answers rather than expressing their genuine feelings, and this could lead to a bias in understanding the real burden of HIV-related stigma in PLWHA. In addition, the findings from limited public health institutions in Nekemte cannot fully show the true picture either in Ethiopia or in sub-Saharan Africa. Moreover, our findings only indicate the associated factors of HIV-related stigma among registered PLWHA. Hence, it is strongly recommended for future researchers to assess the effects of perceived stigma on ART outcomes. Nevertheless, the findings of this study highlight the importance of integrating social and mental health support within standard ART for PLWHA.
Conclusion and Recommendation
The magnitude of perceived stigma among PLWHA was high, highlighting the importance of integrating social and mental health support within standard antiretroviral therapy for PLWHA.
Abbreviations
AOR, adjusted odds ratio; ART, antiretroviral therapy; AUD, alcohol use disorder; COR, crude odds ratio; PLWHA, people living with HIV/AIDS.
Data Sharing Statement
Data will be available upon request from the corresponding authors.
Ethical Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki. Ethical clearance and permission was obtained from Tsinghua University review board, and permission was secured from Nekemte Specialized Hospital and Wollega University Teaching and Referral Hospital, and submitted to each public health facility HIV/AIDS focal person. Written informed consent was obtained from each respondent before the interview.
Acknowledgments
We extend our warm thanks to all supervisors, data collectors, and study participants for their cooperation and support during the study period. The authors are also grateful to all health facility heads for their cooperation and to Wollega University for material support.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. WHO. HIV/AIDS [fact sheet]; 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/hiv-aids.
2. World Health Organization. Key facts on HIV/AIDS. Available from: https//www.who.int/topics/substance_abuse/en/2019.
3. Smith MK, Westreich D, Liu H, et al. Treatment to prevent HIV transmission in serodiscordant couples in Henan, China, 2006 to 2012. Clin Infect Dis. 2015;61(1):111–119. doi:10.1093/cid/civ200
4. Zhao Y, Wu Z, McGoogan JM, et al. Immediate antiretroviral therapy decreases mortality among patients with high CD4 counts in China: a nationwide, retrospective cohort study. Clin Infect Dis. 2018;66(5):727–734. doi:10.1093/cid/cix878
5. UNAIDS. Advancing towards the three zeros. 2020. Available from: https://www.unaids.org/sites/default/files/media_asset/2020_aids-data-book_en.pdf.
6. Hapco F. HIV/AIDS Strategic Plan 2015–2020 in an Investment Case Approach. Addis Ababa: Federal HIV/AIDS Prevention and Control Office, Ethiopia; 2014.
7. Gesesew HA, Ward P, Woldemichael K, Mwanri L. HIV care continuum outcomes: can Ethiopia meet the UNAIDS 90- 90-90Targets? Ethiop J Health Sci. 2020;30(2):179. doi:10.4314/ejhs.v30i2.5
8. Joint United Nations Programme on HIV/AIDS. On the Fast-Track to End AIDS by 2030: Focus on Location and Population. Geneva: UNAIDS; 2015:2030.
9. Avert: Global information and education on HIV and AIDS. HIV stigma and discrimination Available from: www.avert.org.
10. Swendeman D, Rotheram-Borus MJ, Comulada S, Weiss R, Ramos ME. Predictors of HIV-related stigma among young people living with HIV. Health Psychol. 2006;25(4):501. doi:10.1037/0278-6133.25.4.501
11. Parcesepe A, Tymejczyk O, Remien R, et al. HIV-related stigma, social support, and psychological distress among individuals initiating ART in Ethiopia. AIDS Behav. 2018;22(12):3815–3825. doi:10.1007/s10461-018-2059-8
12. Abaynew Y, Deribew A, Deribe K. Factors associated with late presentation to HIV/AIDS care in South Wollo ZoneEthiopia: a case-control study. AIDS Res Ther. 2011;8(1):8. doi:10.1186/1742-6405-8-8
13. Padilla M, Frazier EL, Carree T, Luke Shouse R, Fagan J. Mental health, substance use and HIV risk behaviors among HIV-positive adults who experienced homelessness in the United States - Medical Monitoring Project, 2009–2015. AIDS Care. 2020;32(5):594–599. doi:10.1080/09540121.2019.1683808
14. Da W, Li X, Qiao S, Zhou Y, Shen Z. Antiretroviral therapy and mental health among people living with HIV/AIDS in China. Psychol Health Med. 2020;25(1):45–52. doi:10.1080/13548506.2019.1616101
15. Ramlagan S, Sifunda S, Peltzer K, Jean J, Ruiter RA. Correlates of perceived HIV-related stigma among HIV-positive pregnant women in rural Mpumalanga province, South Africa. J Psychol Afr. 2019;29(2):141–148. doi:10.1080/14330237.2019.1603022
16. Endeshaw M, Walson J, Rawlins S, et al. Stigma in Ethiopia: association with depressive symptoms in people with HIV. AIDS Care. 2014;26(8):935–939. doi:10.1080/09540121.2013.869537
17. Ajong AB, Njotang PN, Nghoniji NE, et al. Quantification and factors associated with HIV-related stigma among persons living with HIV/AIDS on antiretroviral therapy at the HIV-day care unit of the Bamenda Regional Hospital, North West Region of Cameroon. Global Health. 2018;14. doi:10.1186/s12992-018-0374-5
18. Rueda S, Mitra S, Chen S, et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ Open. 2016;6(7):e011453. doi:10.1136/bmjopen-2016-011453
19. Martinez J, Harper G, Carleton RA, et al. The impact of stigma on medication adherence among HIV-positive adolescent and young adult females and the moderating effects of coping and satisfaction with health care. AIDS Patient Care STDS. 2012;26(2):108–115. doi:10.1089/apc.2011.0178
20. Katz IT, Ryu AE, Onuegbu AG, et al. Impact of HIV‐related stigma on treatment adherence: systematic review and meta‐synthesis. J Int AIDS Soc. 2013;16(3 Suppl 2):16. doi:10.7448/IAS.16.3.18640
21. Felker-Kantor EA, Wallace ME, Madkour AS, Duncan DT, Andrinopoulos K, Theall K. HIV stigma, mental health, and alcohol use disorders among people living with HIV/AIDS in New Orleans. J Urban Health. 2019;96(6):878–888. doi:10.1007/s11524-019-00390-0
22. Agnew-Brune CB, Balaji AB, Mustanski B, et al. Mental health, social support, and HIV-related sexual risk behaviors among HIV-negative adolescent sexual minority males: three U.S. cities, 2015. AIDS Behav. 2019;23(12):3419–3426. doi:10.1007/s10461-019-02525-5
23. Duko B, Geja E, Zewude M, Mekonen S. Prevalence and associated factors of depression among patients with HIV/AIDS in Hawassa, Ethiopia, cross-sectional study. Ann Gen Psychiatry. 2018;17(45). doi:10.1186/s12991-018-0215-1
24. Soboka M, Tesfaye M, Feyissa GT, Hanlon C. Alcohol use disorders and associated factors among people living with HIV who are attending services in south west Ethiopia. BMC Res Notes. 2014;7(1):828. doi:10.1186/1756-0500-7-828
25. Gelaye B, Williams MA, Lemma S, et al. Validity of the patient health questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. 2013;210(2):653–661. doi:10.1016/j.psychres.2013.07.015
26. Dalgard OS, Dowrick C, Lehtinen V, et al. Negative life events, social support and gender difference in depression. Soc Psychiatry Psychiatr Epidemiol. 2006;41(6):444–451. doi:10.1007/s00127-006-0051-5
27. Fido NN, Aman M, Brihnu Z. HIV stigma and associated factors among antiretroviral treatment clients in Jimma town, Southwest Ethiopia. HIV/AIDS. 2016;8:183–193. doi:10.2147/HIV.S114177
28. Wani MA, Bhat SA. Social support, self-esteem and quality of life among people living with HIV/AIDS in Jammu & Kashmir India. Anales De Psicología. 2020;36(2):232–241. doi:10.6018/analesps.351111
29. Matsumoto S, Yamaoka K, Takahashi K, et al. Social support as a key protective factor against depression in HIV-infected patients: report from large HIV clinics in Hanoi, Vietnam. Sci Rep. 2017;7(1):1–12. doi:10.1038/s41598-017-15768-w
30. Li X, Yuan X, Wang J, Zhang W, Zhou Y, Liu G. Evaluation of impact of social support and care on HIV‐positive and AIDS individuals’ quality of life: a nonrandomised community trial. J Clin Nurs. 2017;26(3–4):369–378. doi:10.1111/jocn.13377
31. Emlet CA, Brennan DJ, Brennenstuhl S, Rueda S, Hart TA, Rourke SB. The impact of HIV-related stigma on older and younger adults living with HIV disease: does age matter? AIDS Care. 2015;27(4):520–528.
32. Adane B, Yalew M, Damtie Y, Kefale B. Perceived stigma and associated factors among people living with HIV attending ART clinics in public health facilities of Dessie City, Ethiopia. HIV/AIDS - Research and Palliative Care. 2020;12:551–557. doi:10.2147/HIV.S274019
33. Nyamathi A, Ekstrand M, Zolt-Gilburne J, et al. Correlates of stigma among rural Indian women living with HIV/AIDS. AIDS Behav. 2013;17(1):329–339. doi:10.1007/s10461-011-0041-9
34. Kumar N, Unnikrishnan B, Thapar R, et al. Stigmatization and discrimination toward people living with HIV/AIDS in a coastal city of South India. J Int Assoc Provid AIDS Care. 2017;16(3):226–232. doi:10.1177/2325957415569309
35. Pearson C, Micek M, Pfeiffer J, et al. One year after ART initiation: psychosocial factors associated with stigma among HIV-positive mozambicans. AIDS Behav. 2009;13(6):1189. doi:10.1007/s10461-009-9596-0
36. Vanable PA, Carey MP, Blair DC, Ra L. Impact of HIV-related stigma on health behaviors and psychological adjustment among HIV-positive men and women. AIDS Behav. 2006;10(5):473–482. doi:10.1007/s10461-006-9099-1
37. Wolfe WR, Weiser S, Bangsberg D, et al. Effects of HIV-related stigma among an early sample of patients receiving antiretroviral therapy in Botswana. AIDS Care. 2006;18(8):931–933. doi:10.1080/09540120500333558
38. Yang H, Li X, Stanton B, Fang X, Lin D, Naar-King S. HIV-related knowledge, stigma, and willingness to disclose: a mediation analysis. AIDS Care. 2006;18(7):717–724. doi:10.1080/09540120500303403
39. Lowther K, Selman L, Harding R, Ij H. Experience of persistent psychological symptoms and perceived stigma among people with HIV on antiretroviral therapy (ART): a systematic review. Int J Nurs Stud. 2014;51(8):1171–1189. doi:10.1016/j.ijnurstu.2014.01.015
40. Akena D, Musisi S, Joska J, Stein DJ, Cameron DW. The association between aids related stigma and major depressive disorder among HIV-positive individuals in Uganda. PLoS One. 2012;7(11):11. doi:10.1371/journal.pone.0048671
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.