Back to Journals » Vascular Health and Risk Management » Volume 17
High Mitral Annulus Calcium Score in Pre-Operative Chest Computerized Tomography and Adverse Outcomes in Mitral Valve Surgery
Authors Kasim A, Elbaz-Greener G , Shalabi A, Kachel E, Grosman-Rimon L, Jerdev M, amir O, Carasso S
Received 17 September 2021
Accepted for publication 3 November 2021
Published 10 December 2021 Volume 2021:17 Pages 801—807
DOI https://doi.org/10.2147/VHRM.S338880
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Harry Struijker-Boudier
Alexandra Kasim,1,* Gabby Elbaz-Greener,2,3,* Amjad Shalabi,4– 6 Erez Kachel,4– 6 Liza Grosman-Rimon,4,5 Michael Jerdev,4 offer amir,2– 5 Shemy Carasso2– 5
1Department of Radiology, B Padeh Medical Center, Poriya, Israel; 2Department of Cardiology, Hadassah Medical Center, Jerusalem, Israel; 3Faculty of Medicine, Hebrew University of Jerusalem, Jerusalem, Israel; 4Cardiovascular Institute, B Padeh Medical Center, Poriya, Israel; 5The Azrieli Faculty of Medicine in the Galilee, Bar-Ilan University, Safed, Israel; 6Department of Cardiac Surgery, B Padeh Medical Center, Poriya, Israel
*These authors contributed equally to this work
Correspondence: Gabby Elbaz-Greener
Department of Cardiology, Hadassah Medical Center, Room Number 114, Jerusalem, Israel
Tel +97226776564
Fax +97226411028
Email [email protected]
Background: Severe mitral annulus calcification (MAC) is believed to bear high operative and post-operative risk during mitral valve replacement (MVR) surgery, including longer surgery time, post-surgical valvular leaks and increased rate of embolic phenomena. We hypothesized that quantification of mitral calcium in pre-operative chest computerized tomography (CCT), performed to assess aortic root before cross-clamping may help in risk assessment of adverse intraoperative and postoperative outcomes in patients undergoing MVR.
Methods: We included patients who underwent MVR between the years 2015 and 2018 at Poriya medical center. Preoperative CCT was performed using Philips iCT 256 and Agatston mitral annulus calcium score (MACS) was retrospectively calculated using Philips Intellispace portal version 8.0. Patients were divided into MACS quintiles; 1– 3 quintiles were grouped (Low MACS) and compared to the 4– 5 quintiles (High MACS) group for demographic, clinical operative and post-operative parameters.
Results: A total of 66 patients had MVR, out of which 61% were males, with mean age of 64± 9. Concomitant coronary or valvular procedures were done in 60% of patients. The median MACS was 43. High MACS (≥ 854) was not associated with longer bypass or cross clamp times. No differences in the MVR results were found between the groups. There were 6 post-operative embolic events; 1 mesenteric and 5 cerebral, which were not associated with MACS.
Conclusion: MACS did not seem to be related to adverse outcomes in MVR. Due to a low event rate and probable pre-selection of patients without extreme mitral annulus calcifications our results should be confirmed in larger prospective study.
Keywords: mitral annulus calcification, MACS, mitral valve replacement, MVR
Introduction
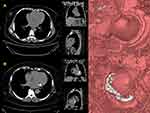
Mitral annulus calcification (MAC) is a chronic, non-inflammatory, degenerative process in the fibrous base of the mitral valve. MAC is most commonly asymptomatic and incidental finding.1 Recently, there has been accumulating evidence that other mechanisms, such as atherosclerosis and abnormal calcium-phosphorus metabolism, also contribute to the development of MAC.1 The mitral annulus (Figure 1), which is typically flexible becomes thicker and less flexible. The posterior annulus is most commonly affected. Calcific masses often extend as far as 3.5 cm into the adjacent myocardium and often project superiorly toward the atrium and centrally into the cavity of the left ventricle.3 Figure 2 shows calcium in the mitral valve, A - Patient without MAC, B - Patient with MAC.
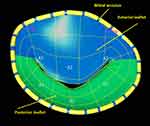 |
Figure 1 Mitral anatomy model. Viewed from the left atrium (Surgeon’s View). Anterior (A), Posterior (P) leaflet scallops numbered from 1–3, from lateral to medial. |
The prevalence of MAC is 8–15%, and significantly increases with advanced age, female sex, in patients with multiple cardiovascular risk factors and with chronic kidney disease (CKD).2–5 Calcification of the mitral annulus increases in situations where there is increased stress on the annulus and the valve.2 Additionally, other conditions contributing to LV hypertrophy, including hypertension and aortic stenosis, and prior chest irradiation in combination with aortic valve disease and restrictive cardiomyopathy are known to be risk factors of MAC.4 Furthermore, several large-scale, community-based cohort studies observed a strong association between the presence of MAC and AF.6 This association is independent of baseline clinical risk factors for AF and of the development of interim myocardial infarction or heart failure.6 MAC might also interrupt the interatrial and intra-atrial conduction processes, leading to conduction system and atrial conduction defects, thus resulting in AF.7
Several clinical implications have been associated with MAC, including cardiovascular disease, mitral valve disease, and arrhythmias. Severe MAC present among quarter of patients referred for mitral valve surgery has implications for the complexity of mitral valve operations.8
According to the current 2021 ESC/EACTS guidelines, a well-established indication of cardiac CT for valvular heart disease includes preoperative assessment of aorta and coronary artery evaluation.9 However, the excellent resolution of cardiac CT is a great benefit in other aspects as evaluation of anatomical structures and geometry. Leaflet calcification and MAC cannot only be visually assessed, but also can be measured quantitatively using Agatston scoring and visualization of its extent and location. Furthermore, cardiac CT has been used for the geometric assessment of the MV apparatus and LV remodeling to help determine the mechanism of functional MR.10
Our objectives were to investigate if quantification of mitral calcium in pre-operative chest computerized tomography (CCT) done to assess aortic root before cross-clamping may help in risk assessment for intraoperative and postoperative adverse outcomes in patients undergoing MVR.
Materials and Methods
This single center retrospective cohort study was approved by the Institutional Research Ethics Board (IRB) at Poriya Medical Center (0099-14-POR). The IRB approved that patients’ consent was not required for this historical retrospective study include only de-identified data.
Patient Selection
We included patients 18 years and older, who underwent MVR between June 2015 and June 2018 at Poriya medical center.
Pre-Operative Chest Computer Tomography
All the CT scans were performed utilizing Brilliance iCT 256-slice scanner, Philips Healthcare. The Ca score scan was acquired in the craniocaudal direction starting at the carina and ending under the diaphragm.
Technical parameters: collimation: 128×0.625 mm; voltage: 120 kV, rotation time 0.36. Scans were reconstructed with an effective section thickness of 1.5 mm. Acquisition was performed during an inspiratory breath-hold while the ECG was recorded simultaneously to allow retrospective gating of the data (Figure 3A and B).
 |
Figure 3 Mitral annulus calcium scoring. (A) Low calcium score. (B) High Calcium Score. |
Outcome Variables
We examined 2 sets of variables: (1) Intraoperative; bypass time, cross-clamp time and (2) Postoperative; thromboembolic events, re-operation, length of stay (LOS), In-hospital mortality, post-operative MR grade and gradients.
Statistical Analysis
Categorical variables were presented as frequency (percentage) and Continuous variables were presented as median, interquartile range (IQR). Patients were divided according to their preoperative MACS, grouping the three lowest quintiles (Low MACS) and the two highest (High MACS). We used the ANOVA Kruskal-Wallis test to compare subgroups pre, intra and post-operative parameters as normal distribution could not be assured. Categorical variables were compared using Fisher’s exact test.
Statistical significance was considered to be two-sided p-values of <0.05. All data were analyzed with MedCalc Statistical Software version 18.11.3 (MedCalc Software Ltd, Ostend, Belgium; https://www.medcalc.org; 2019).
Results
A total number of 66 patients had mitral valve surgery during the study period. Baseline characteristics of the cohort are present in Table 1. In the total cohort, the mean age was 64±9 years and 64% of the patients were males. The majority of patients were hypertensive (77%) and had hyperlipidemia (58%). Concomitant coronary or valvular procedures were done in 79% of patients (Table 1).
 |
Table 1 Patient Characteristics by Mitral Calcium Score |
In the total cohort, MACS ranged between 0 and 14,564. Forty patients had low median MACS (0, [IQR 0–0]), with MACS ranging from 0 to 131 and 26 patients had high median MACS (1024, [IQR 487–2394]), with MACS ranging from 143 to 14,561.
Higher prevalence of female, patients with diabetes mellitus, patients with prior myocardial infarction and previous heart surgery were found in the high MACS group (Table 1). In the low MACS group, there was higher prevalence of patients with chronic obstructive lung disease (COPD), prior cerebro-vascular accident (CVA) and patients with rheumatic heart disease.
Pre-procedure echocardiographic variables were similar between the low and high MACS groups (Table 1).
The main reason for the MVR procedure was MR in both groups, while higher rate of combined valve surgery due to MR and AS was found in the low MACS group (Table 1).
Outcomes and MACS
Intraoperative
There were no differences between the low and high MACS groups in the intraoperative outcomes, as well as bypass time and cross clamp time (Table 2).
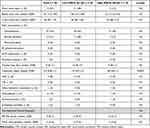 |
Table 2 Outcomes of Mitral Heart Surgery |
Postoperative
In total, there were 6 post-operative confirmed embolic events, 1 mesenteric event and 5 cerebral events. All five cerebral events occurred in the low MACS group (Figure 4).
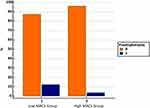 |
Figure 4 Post-operative embolic phenomena. |
There were no statistically significant differences between the groups in the rate of re-operation. Post-operative LOS and in-hospital mortality were similar among the groups (Table 2). Post-operative echocardiography results demonstrated no differences in MR grade and mitral valve gradients between the low vs high MACS groups.
Discussion
In this population-based study of MVR patients, patients were divided according to their preoperative MACS, grouping the three lowest quintiles (Low MACS) and the two highest (High MACS). In this study, out of the total cohort (N = 66), 40 patients were with low MACS, ranging from 0 to 131 and 26 patients were with high median MACS, ranging from 143 to 14,561.
Severe MAC can pose significant challenge to the surgeon undertaking mitral valve replacement or repair. Some of the risks may be cardiac rupture at the atrioventricular junction, rupture of the LV free wall, and in injury to the circumflex artery when debridement of MAC is performed.11,12 MAC was associated with increased intraoperative conversion from valve repair to replacement,8 peri-prosthetic leakage or/and stenosis.13 Manipulation during this procedure may increase thromboembolic events (TEs) by calcium debris, resulting in brain or coronary emboli in patients with severe MAC.14
Perioperative TEs are serious and devastating complications after cardiac surgery, ie, coronary artery bypass grafting and valvular surgery.15 The incidence remained largely unchanged despite advances surgical techniques ranging from 0.8% to 18% in prior studies. The most serious TEs events are cerebrovascular events resulting in higher rate of morbidity and mortality and have been a major limitation for surgery.16
Therefore, it is essential to assess pre-operative TEs risk associated with MVR. Thus, our aim was to examine if quantification of mitral calcium in pre-operative chest computerized tomography done to assess aortic root before cross-clamping may help in risk assessment for TEs adverse outcomes in patients undergoing MVR.
Prior studies found wide risk range of cerebrovascular TEs events following MVR. In our study, there were six (7.6%) post-operative embolic events. One mesenteric event and five cerebral events, which occurred in the low MACS group. Several predictors for TEs were found in prior studies, including older age, female sex, use of intra-aortic balloon pump (IABP), prior coronary artery disease, hypertension and left atrial dimension above 50mm.14 In our study, we found higher prevalence of females and patients with larger left atrial dimension in the high MACS group. However, we could not find a relationship between the MACS levels and the TEs events. The low event number did not allow for a multi-variable analysis of associates of TEs in this study.
Our study should be interpreted in the context of several limitations. First, our study includes a relatively small sample size. Therefore, our findings should be confirmed in larger multicenter studies. Second, our study is retrospective, and the information was based on hospital medical records and as such is susceptible to coding errors. Therefore, we cannot rule out residual confounding of the association we observed. Due to a low event rate and probable pre-selection of patients without extreme mitral annulus calcifications our results should be confirmed in larger prospective study.
Conclusion
MACS in the range found in our study did not seem to be related to adverse outcomes in mitral valve surgery. Yet, due to a low event rate and probable pre-selection of patients without extreme mitral annulus calcifications, our results should be confirmed in larger prospective study. Trials aiming at preventing TEs events should be conducted to reduce morbidity and mortality following MVR.
Acknowledgments
The corresponding author affirms that he has listed everyone who contributed significantly to the work. The authors had access to all the study data, and were responsible for the accuracy of the analysis, and had authority over manuscript preparation and the decision to submit the manuscript for publication. The corresponding author confirms that all authors read and approve the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Birudaraju D, Cherukuri L, Pranesh S, Budoff MJ. Current methods to assess mitral annular calcification and its risk factors. Expert Rev Cardiovasc Ther. 2021;19(9):787–800. doi:10.1080/14779072.2021.1964361
2. Abramowitz Y, Jilaihawi H, Chakravarty T, Mack MJ, Makkar RR. Mitral annulus calcification. J Am Coll Cardiol. 2015;66(17):1934–1941. doi:10.1016/j.jacc.2015.08.872
3. Fertman MH, Wolff L. Calcification of the mitral valve. Am Heart J. 1946;31:580–589. doi:10.1016/0002-8703(46)90004-X
4. Kanjanauthai S, Nasir K, Katz R, et al. Relationships of mitral annular calcification to cardiovascular risk factors: the Multi-Ethnic Study of Atherosclerosis (Mesa). Atherosclerosis. 2010;213:558–562. doi:10.1016/j.atherosclerosis.2010.08.072
5. Asselbergs FW, Mozaffarian D, Katz R, et al. Association of renal function with cardiac calcifications in older adults: the cardiovascular health study. Nephrol Dial Transplant. 2009;24:834–840. doi:10.1093/ndt/gfn544
6. Foley PW, Hamaad A, El-Gendi H, Leyva F. Incidental cardiac findings on computed tomography imaging of the thorax. BMC Res Notes. 2010;3:326. doi:10.1186/1756-0500-3-326
7. O’Neal WT, Efird JT, Nazarian S, Alonso A, Heckbert SR, Soliman EZ. Mitral annular calcification and incident atrial fibrillation in the Multi-Ethnic Study of Atherosclerosis. Europace. 2015;17:358–363. doi:10.1093/europace/euu265
8. Pekdemir H, Cansel M, Yagmur J, et al. Assessment of atrial conduction time by tissue Doppler echocardiography and P-wave dispersion in patients with mitral annulus calcification. J Electrocardiol. 2010;43:339–343. doi:10.1016/j.jelectrocard.2010.02.013
9. Vahanian A, Beyersdorf F, Praz F, et al. ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2021;2021. doi:10.1093/eurheartj/ehab395.
10. Suh YJ, Lee S, Chang BC, et al. Utility of cardiac CT for preoperative evaluation of mitral regurgitation: morphological evaluation of mitral valve and prediction of valve replacement. Korean J Radiol. 2019;20:352–363. doi:10.3348/kjr.2018.0350
11. Fusini L, Ghulam Ali S, Tamborini G, et al. Prevalence of calcification of the mitral valve annulus in patients undergoing surgical repair of mitral valve prolapse. Am J Cardiol. 2014;113(11):1867–1873. doi:10.1016/j.amjcard.2014.03.013
12. Carpentier AF, Pellerin M, Fuzellier JF, Relland JY. Extensive calcification of the mitral valve anulus: pathology and surgical management. J Thorac Cardiovasc Surg. 1996;111:
13. Okada Y. Surgical management of mitral annular calcification. Gen Thorac Cardiovasc Surg. 2013;61(11):619–625. doi:10.1007/s11748-013-0207-7
14. Maisano F, Caldarola A, Blasio A, De Bonis M, La Canna G, Alfieri O. Midterm results of edge-to-edge mitral valve repair without annuloplasty. J Thorac Cardiovasc Surg. 2003;126(6):1987–1997. doi:10.1016/S0022-5223(03)01291-1
15. Russo A, Grigioni F, Avierinos JF, et al. Thromboembolic complications after surgical correction of mitral regurgitation incidence, predictors, and clinical implications. J Am Coll Cardiol. 2008;51:1203–1211. doi:10.1016/j.jacc.2007.10.058
16. Gaudino M, Rahouma M, Di Mauro M, et al. Early versus delayed stroke after cardiac surgery: a systematic review and meta-analysis. J Am Heart Assoc. 2019;8:e012447. doi:10.1161/JAHA.119.012447
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.