Back to Journals » Clinical and Experimental Gastroenterology » Volume 14
Hepatectomy with Takasaki’s Technique Using SonaStar Ultrasonic Aspiration System: An Experience from 58 Cases
Authors Ho VL, Pham NH, Nguyen TX , Tran AP, Dang NT, Pham NH
Received 9 May 2021
Accepted for publication 11 June 2021
Published 22 June 2021 Volume 2021:14 Pages 297—302
DOI https://doi.org/10.2147/CEG.S319434
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Anastasios Koulaouzidis
Van Linh Ho,1 Nhu Hien Pham,2 Thanh Xuan Nguyen,2 An Phong Tran,1 Nhu Thanh Dang,3 Nhu Hiep Pham1
1Digestive Surgery Department, Hue Central Hospital, Hue City, Vietnam; 2Department of Abdominal Emergency and Pediatric Surgery, Hue Central Hospital, Hue City, Vietnam; 3Surgery Department, Hue University of Medicine and Pharmacy, Hue City, Vietnam
Correspondence: Thanh Xuan Nguyen
Department of Abdominal Emergency and Pediatric Surgery, Hue Central Hospital, 16 Le Loi Street, Hue City, Vietnam
Tel +84945313999
Email [email protected]
Objective: This study aims to explore the short-term results of hepatectomy with Takasaki’s technique using Sonastar ultrasonic aspiration system.
Materials and Methods: We retrospectively examined data of 58 patients who underwent hepatectomy with Takasaki’s technique using Sonastar ultrasonic aspiration system at Hue Central Hospital from 01/2018 to 02/2021.
Results: The mean age was 60.7 ± 10.5 years (25– 80) and the male/female ratio was 6:1. Patients with solitary tumor accounted for 79%; 68.4% had tumor size greater than 5 cm. Pringle maneuver was used in 57.9%, while selective right or left Glissonean pedicle occlusion was used in 69.0% and 32.8%, respectively. Final transection surface reinforcement was achieved by Surgicel and BioGlue in 78.9% and 21.5% of cases, respectively. Major liver resection accounted for 73.7%. The mean parenchymal transection time was 50 (45– 110) minutes, while mean total operative time was 125 (90– 280) minutes. Mean operative blood loss was 250 (150– 650) mL. Mean post-operative hospital stay was 8 days (7– 23). Post-operative complication rate was 15.9% and mortality rate was 1.7%.
Conclusion: Hepatectomy using Takasaki technique with Sonastar ultrasonic aspiration system is safe, effective, allowing an anatomical resection with sufficient safety margin and resulting in low complication rates (liver failure, biliary leakage) and good survival outcomes.
Keywords: liver tumor, SonaStar, Takasaki’s technique
Background
Hepatectomy is the most popular radical treatment for hepatic malignancies which offers resectable patients better survival rates.1,2 However, hepatectomy is also associated with numerous complications including bleeding, acute liver failure and bile leakage … which can adversely affect survival result and mortality rate.3
Among many Glissonean pedicle approaches, Takasaki’s extrafascial approach provides a safe, quick dissection of Glissonean pedicle compared to intrafascial approach by Lortat–Jacob and Robert4 and transfissural approach by Ton That Tung in Vietnam5 and Tien‐Yu Lin in Taiwan6 as it follows the natural plane between Glisson’s and Laennec's capsules. The Takasaki technique has been widely adopted in anatomical resection for hepatocellular carcinoma as well as other liver tumors.7 Besides a traditional clamp-crush technique, novel parenchymal transection technology of Sonastar (Misonix Inc., Farmingdale, NY, USA) provide precise ultrasonic aspiration with high tissue selectivity and preservation of Glissonean pedicle elements. Furthermore, anatomic liver resection has been demonstrated to provide better recurrence-free survival in hepatocellular carcinoma, as well as better preservation of healthy liver parenchyma and limiting bile leakage by accurate dissection in the intersegmental planes.8
A combination of theses above-mentioned factors could theoretically allow safer and more efficient liver resection. Therefore, we conducted this study to evaluate the short-term postoperative results of hepatectomy with Takasaki’s technique using Sonastar ultrasonic aspiration system (Sonastar).
Materials and Methods
A retrospective study was conducted on 58 patients who underwent hepatectomy with Takasaki’s technique using Sonastar in Hue Central Hospital from 01/2018 to 02/2021. The recorded information included (1) general information: age, gender, history of liver diseases and past liver-directed therapy; (2) laboratory tests: hepatic function was classified using Child-Pugh classification; (3) tumor characteristics: site, size, number, and Barcelona Clinic Liver Cancer (BCLC) staging; (4) technical characteristics and complications.
Using the International Study Group of Liver Disease (ISGLS) criteria, bile leakage was defined as a bilirubin concentration in the drain fluid at least three times the serum bilirubin concentration measured at the same time) from postoperative day 3 onwards or the need for re-intervention (radiologic or surgical) for biliary collections or peritonitis. Similarly, posthepatectomy liver failure was defined as an increased international normalized ratio and concomitant hyperbilirubinemia on or after postoperative day 5.
Surgical Procedure
Step 1: Patients were all placed in supine position with both arms tucked alongside the body. A J-shaped incision was used. After placement of Kent retractor, the abdomen was carefully explored for any contraindications for a curative resection (eg unresectable local invasion, distant metastasis). Liver mobilization was performed based on which type of hepatectomy was planned. Cholecystectomy was routinely performed to facilitate hilar dissection.
Step 2: A combination of blunt and sharp dissection allowed us to enter the avascular plane between Glisson’s and Laennec capsules. The bifurcation was first lower from the inferior surface of segment 4. Left and right pedicle could then be easily encircled and taped using right angle dissector. Further dissection of the right anterior and posterior sections could also be proceeded based on the types of hepatectomy. Pringle maneuver can be selectively used during this step. Dissection of higher level Glissonean pedicles usually required an intrahepatic approach after localisation by intraoperative ultrasound.
Step 3: The Glisonnean pedicle supplying the to-be-resected segment was clamped and the demarcation line was marked with electrocautery. Sonastar system was then used for parenchymal transection. The rapid forward and backward movement of the tip of the handpiece would create a cavitation effect resulting in fragmentation of tissue with higher water content (eg hepatocytes) and preservation of fibrous tissue (biliary tracts and blood vessels). All biliary and vascular elements were then clipped or suture – ligated before division. Sonastar was also equipped with aspiration and electrocautery components, which further facilitated a bloodless and safe transection.
Step 4: Final inspection was performed to identify sites of bile leak or hemorrhage from the transection surface, which were then reinforced by suture. Surgicel or BioGlue was then placed on the transection surface. An abdominal drain was placed under the liver and exteriorized on the right flank.
Step 5: Abdominal closure.
Data Analysis
Dаtа were analyzed using SPSS 16.0 (IBM, Chicago, IL, USA). All descriptive Descriptive data were presented as means and standard deviations (SDs) and percentages.
Results
Patient Characteristics
Fifty-eight patients (50 men and 8 women) underwent hepatectomy with Takasaki’s technique using Sonastar. The mean age was 60.7 ± 10.5 (25–80) years. There were 57 (98.3%) patients with a medical history of hepatitis B or C (51 hepatitis B). Most patients were classified as Child-Pugh Stage A and Performance Status (PS) 0. All patients had platelet counts over 100.000/mm3 and normal coagulation panel. The mean of serum AFP level was 379 ± 110.7 (11.5–1660) ng/mL.
Tumor Characteristics
The majority of patients had solitary tumor (79.3%), tumor that is more than 5cm in size (68.4%), and distinct tumor capsule (89.5%) (Table 1).
 |
Table 1 Tumor Characteristics |
Technical Characteristics
Pringle maneuver was used in 11 patients (19%), while selective right and left Glissonean pedicles occlusion was used in 40 (69%) and 19 (32.8%), respectively. Surgicel was used to reinforce the transection surface in 49 (84.5%), and Bioglue was used in 21.5% of cases. Anatomical liver resection was performed in 51 patients (87.9%). Major liver resection (≥3 segments) was done in 74.1% of cases (Table 2). The mean of liver parenchyma transection time was 50 (45–110) minutes. The mean operative time was 125 (90–280) minutes. The amount of blood lost during operation was 250 (150–650) mL.
 |
Table 2 Characteristics of Liver Resection Technique |
Surgical results and Early Outcomes
Postoperative characteristics were listed in Table 3. Most patients experienced an uneventful postoperative course. In the majority of patients, liver function tests showed slight disturbances during the first 5 postoperative days and gradually normalized from day 5 onwards.
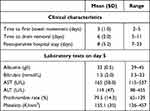 |
Table 3 Postoperative Characteristics |
Postoperative complications occurred in 5 patients (8.5%) (Table 4). One patient (1.7%) experienced bile leakage which lead to bile peritonitis requiring second operation in the fifth day postoperatively. The patient was dead in the two days after the second operation cause of nonrecoverable septic shock. The posthepatectomy liver failure was reported in 1/58 patient (1.7%), which was treated conservatively with fresh frozen plasma and human albumin transfusion.
 |
Table 4 Post-Operative Complications |
The overall 24-month survival rates were 31% (18/58 patients). 15.3% (9/58 patients) patients had recurrences and were treated by ultrasound guided percutaneous Radiofrequency Ablation (RFA), all of whom were still alive still the end of the study period (Table 5)
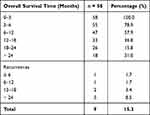 |
Table 5 Survival Prognosis |
Discussions
Surgical Technique
The Takasaki’s technique helps reduce bleeding in hepatic parenchyma transection as well as easily detect the anatomical boundaries of hepatic segments. Therefore, it help minimize the ischemia of remnant hepatic parenchyma and avoid the spread of malignant cells to the adjacent liver segments.
The application of Sonastar ultrasonic aspiration system in the liver parenchymal transection provides many significant advantages including preservation of small blood vessels and bile ducts at the transection surface which then be subsequently controlled by clipping or ligation to prevent hemorrhage and bile leak. It also facilitate dissection close to important vascular and biliary structures when the tumor is nearby. On the other hand, the maximal preservation of healthy liver parenchymal help ensure sufficient remnant liver volume to prevent postoperative liver failure.
Morbidity and Mortality
The overall morbidity rate was 8.5%. Our study reported one case (1.7%) with postoperative bile leak which lead to bile peritonitis requiring second operation on day 5. The patient was dead on the second day after the second operation due to nonrecoverable septic shock. The postoperative hepatic failure was reported in only 1/58 patient (1.7%), which was treated conservatively with fresh frozen plasma and human albumin transfusion. Two patients (3.4%) had ascites and were treated human albumin transfusion and diuretic (furosemide 40 mg per day). All other patients recovered after 7–10 days postoperatively. Patients with residual abscess complication were treated with ultrasound guided drainage and broad-spectrum antibiotics.
Recent improvements in anesthesia and intensive care along with updated techniques and tools help reduce the morbidity and mortality rates significantly. According to recent studies, hepatectomy complications accounted for 25% to 50%,9 with common complications related to surgery including bleeding, bile leakage, prolonged abdominal distention, hepatic dysfunction, prolonged pleural effusion and abscess below the diaphragm. Mild and severe bleeding and the need of blood transfusion were the factors that increased the rate of morbidity and mortality.10,11 Retrospective study and multivariate analysis in major liver resections revealed that Pringle maneuver technique and blood transfusion were risk factors for patients, especially those with chronic comorbidities. Moreover, blood transfusion was the independent risk factor of postoperative mortality12. Liver failure was associated closely with preoperative hepatic functions, extent of liver resection and future liver remnant volume (FLRV). Hepatic failure was the main cause of postoperative mortality. Right portal vein embolization (PVE) was a procedure that induces regrowth on left liver to accomplish the required FLRV.
Postoperative Survivals
The survival rates of liver resection in patients with tumor more than 5 cm in diameter was approximately 68.4%. In fact, the tumor size, in most case, did not result in significant difficulty intraoperatively. Studies showed that the overall survival was dependent on the tumor size and the stage of disease as well as the preoperative hepatic function. Patients with less-than-5cm tumors had the 5-years survival rate was about 70%, meanwhile, patients with hepatocellular carcinoma and hepatitis, the 5-years survival rate after hepatectomy was just 60%, and the rate of mortality related to surgery was about 2 to 3%.13
The recurrence rate in the current study was 15.3%. However, because only 18 patients in our study were followed longer than 24 months, longer follow-up time is required to accurately reflect the survival prognosis. In the current literature, recurrence rate in 5-year follow-up was about 50 to 80%. Despite of the application of updated techniques and supported tools, there was not much improvement in limiting recurrence.14 Therefore, a multidisciplinary approach to recurrence is important to prolong posthepatectomy survival.15
This is only a retrospective observation of short-term outcomes of the current technique of hepatectomy on a limited number of patients. A longer follow-up time and a control group is required in future study to clarify the potential benefits of Sonastar system and Takasaki technique.
Conclusions
Hepatectomy using Takasaki technique with Sonastar ultrasonic aspiration system is safe, effective, allowing an anatomical resection with sufficient safety margin and resulting in low complication rates (liver failure, biliary leakage) and good survival outcomes.
Ethics Approval and Consent to Participate
This study has been reviewed by the Ethics Committee of Hue Central Hospital; all procedures performed in studies involving human participants were conducted according to the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent for Publication
Written informed consent for publication of the clinical details were obtained from each patient.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests.
References
1. Andel D, Dassen MG, Reinders-Hut MTM, et al. Surgical outcomes of major hepatectomy following “radiation lobectomy” for hepatic malignancies and insufficiently functional future liver remnant: initial experience. Br J Surg. 2020;107(12):e609–e610. doi:10.1002/bjs.11828
2. Lu WP, Dong JH. Hepatectomy for hepatocellular carcinoma in the era of liver transplantation. World J Gastroenterol. 2014;20(28):9237–9244. doi:10.3748/wjg.v20.i28.9237
3. Ishii M, Mizuguchi T, Harada K, et al. Comprehensive review of post-liver resection surgical complications and a new universal classification and grading system. World J Hepatol. 2014;6(10):745–751. doi:10.4254/wjh.v6.i10.745
4. Lortat-Jacob JL, Robert HG. [Well defined technic for right hepatectomy]. Presse Med. 1952;60(26):549–551. Noewegian.
5. Tung T, Quang N. A new technique for operating on the liver. Lancet. 1963;26(7274):192–193. doi:10.1016/S0140-6736(63)91210-8
6. Lin TY, Chen KM, Liu TK. Total right hepatic lobectomy for primary hepatoma. Surgery. 1960;48:1048–1060.
7. Takasaki K. Glissonean pedicle transection method for hepatic resection: a new concept of liver segmentation. J Hepatobiliary Pancreat Surg. 1998;5(3):286–291. doi:10.1007/s005340050047
8. Orcutt ST, Anaya DA. Liver resection and surgical strategies for management of primary liver cancer. Cancer Control. 2018;25(1):1073274817744621. doi:10.1177/1073274817744621
9. Fong Y, Sun RL, Jarnagin W, Blumgart LH. An analysis of 412 cases of hepatocellular carcinoma at a Western center. Ann Surg. 1999;229(6):790–799;discussion 799–800. doi:10.1097/00000658-199906000-00005
10. Makuuchi M, Takayama T, Gunven P, Kosuge T, Yamazaki S, Hasegawa H. Restrictive versus liberal blood transfusion policy for hepatectomies in cirrhotic patients. World J Surg. 1989;13(5):644–648. doi:10.1007/BF01658893
11. Shirabe K, Shimada M, Gion T, et al. Postoperative liver failure after major hepatic resection for hepatocellular carcinoma in the modern era with special reference to remnant liver volume. J Am Coll Surg. 1999;188(3):304–309. doi:10.1016/S1072-7515(98)00301-9
12. Wei AC, Tung-Ping Poon R, Fan ST, Wong J. Risk factors for perioperative morbidity and mortality after extended hepatectomy for hepatocellular carcinoma. Br J Surg. 2003;90(1):33–41. doi:10.1002/bjs.4018
13. European Association for Study of L, European Organisation for R, Treatment of C. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. Eur J Cancer. 2012;48(5):599–641.
14. Bruix J, Sherman M, American Association for the Study of Liver D. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53(3):1020–1022. doi:10.1002/hep.24199
15. Matsumata T, Kanematsu T, Takenaka K, Yoshida Y, Nishizaki T, Sugimachi K. Patterns of intrahepatic recurrence after curative resection of hepatocellular carcinoma. Hepatology. 1989;9(3):457–460. doi:10.1002/hep.1840090320
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
